Summary
Aim
A partial edentulous area was restored with a tooth to implant fixed partial denture and a rigid connection between the two elements. Maintenance recalls were performed over a 19-year period of observation on a yearly basis.
Methods
The following parameters were collected during each examination over the entire period of observation: PD around the implant and natural tooth abutment, gingival index, modified gingival index, plaque index, modified plaque index, occlusal assessment, marginal bone loss. Radiographic assessment of peri-implant bone remodeling was performed in a retrospective way. The following reference points were assessed on each image: fixture-abutment junction, threads, first contact of the crestal bone with the implant on both mesial and distal side. This made possible, with the known values for implant diameter and length, to make linear measurements of remaining peri-implant bone measured from the mesial and distal marginal bone levels and the fixture-abutment junction. The amount of bone change over the baseline to a 19 years follow-up observation time was calculated for both the implant and the natural tooth.
Results
Clinical parameters showed healthy values over the entire period of observation with slight isolated positive bleeding on probing. Bone remodeling values were constant over the entire period with slight higher values around the tooth. Peri-apical radiographs did not show any intrusion of the tooth.
Conclusions
The present case report showed the complete functionality and stability of a tooth to implant rigidly connected FPD over a period of 19 years.
Keywords: dental implants, natural tooth, rigid connection, follow-up
Introduction
The incorporation of natural teeth as abutments in implant-supported restorations is sometimes necessary to reach chewing comfort. However, the survival rates of both implants and reconstructions in combined tooth-implant supported fixed partial dentures (FPDs) are lower than those reported for solely implant supported FPDs (1). In addition, the convenience of connecting tooth to implant is a very discussed issue since an implant does not feature the same anatomical and physiological aspects of a tooth. In fact, while the tooth is provided with periodontal ligament that functions as an hydraulic system, a dental implant does not feature any periodontal ligament and is directly connected with the surrounding bone. Teeth with healthy periodontal ligament show mobility of 50–200 μm upon displacement of the crown with a force of 01. N (2, 3) while dental implants demonstrate values less than 10 μm (4). Moreover, tactile perception of natural tooth abutments was shown to be significantly higher than that demonstrated for implant abutments. Sensory feedback due to periodontal mechanoreceptors located in the periodontal ligament are extremely sensitive to external stimuli. These receptors have thresholds of about 20 μm of thickness in between antagonistic teeth and 1–2 g upon tooth loading. After extraction of teeth the periodontal ligament and its receptors disappear.
Following the placement of dental implants detection thresholds are increased to at least 50–100 μm of thickness and 50–100 g upon tooth loading. The underlying mechanism of the so-called ‘bone-perception’ phenomenon remains a matter of debate, but it is assumed that mechanoreceptors in the 4 peri-implant bone and neighbouring periosteum may be activated by implant loading (5). In order to compensate the different intrusion behaviours of teeth and implants in a tooth to implant FPD, a stress disposer has been suggested (6). In this experimental study it was noted that the value of resorption around the implant rigidly attached with the natural tooth did not jeopardize implant integration. Additionally it was observed that the rigid connection is more favourable than the connection with disposer because it is able to attenuate the intrusion of natural tooth. Finally, in this study it was recommended to design pontic as short as possible to prevent the phenomenon of intrusion and more straight as possible to prevent lateral displacement of the natural abutment. Other researchers have evaluated the biomechanical stress of perimplant bone in tooth to implant FPDs (7). Specific factors that positively reduced the stress were the rigid connection, the number of splinted teeth and the direction of the prosthetic loading. This in vitro research was performed using 3-D finite element analysis. The three variables were compared to the value of the stress on the bone and mobility of teeth involved. The results showed that load direction and tooth mobility were the main elements affecting stress value on bone tissue. The occlusal stress as cause of teeth lateral movement in FPDs has been investigated in another study (8). This experiment was carried out with the non-linear finite element analysis and computed tomography. One-piece and two-piece implants splinted to natural teeth were used and the quality of periodontal support was varied. The analytical results showed as oblique load caused greater stress on the bone tissue than axial stresses. One-piece implant absorbed occlusal forces better than two-piece one while the degree of periodontal support and the number of splinted teeth according to these authors slightly affected the transmission of stress on the bone around FPDs (9). The purpose of the present study was to evaluate on a long follow-up time (19 years) the peri-implant bone remodeling, the periodontal and peri-implant health and the success rate of a combined tooth to implant FPD supported by a plasma sprayed (TPS) implant rigidly splinted to a natural tooth abutment.
Materials and methods
Treatment plan, implant surgery and prosthetic restoration
On January 1994 a 53 years old, healthy patient (G.L.R.), was visited in the Unit of Prosthodontics and Implant Dentistry, School of Dentistry, “Sapienza” University of Rome. The patient reported as his chief complaint the need to restore a distal edentulous area in the left lower jaw. The patient also reported severe hypersensitivity on tooth # 28. The clinical assessment confirmed that teeth # 30 and 31 were missing and a deep gingival recession was observed on the buccal aspect of tooth # 2.89 (A.D.A. Classification). No additional dental treatments were required. Peri-apical radiographs and clinical examination revealed optimal periodontal status on teeth # 28 and 29 and sufficient bone to place standard dental implants in the area of teeth # 30 and 31 (Fig. 1) Several treatment modalities were proposed to the patient and because of financial reasons he opted for a tooth to implant FPD with the placement of a dental implant in position 31 while involving tooth 29 as mesial abutment. The FPD was planned with a rigid connection between the two prosthetic elements. A gold ceramic crown was also planned on tooth # 30. The patient adopted an antimicrobial prophylaxis with a mouthwash of 0.12% chlorexidine (Dentosan 0.12%, Pfiezer, New Brunswick, NJ, USA) rinsing for 1 minute prior to surgery and three times a day for the following 10 days. Systemic antibiotics were prescribed (Zimox® 1gr, Pfiezer, New Brunswick, NJ, USA; 3 gr for day; amoxicillin for 6 days starting 1 hour before surgery). Local anesthesia was induced by infiltration with articaine/epinephrine (Ecocain ® 20 mg/ml, Molteni Dental, Italy). A full thickness, crestal incision was made and the bone site exposed. The implant placement was performed following the instructions of the implant manufacturer under abundant saline solution irrigation. A TPS cylindrical hollow-basket design implant was inserted (ITI Bonefit®, Straumann, Switzerland) (4.1 mm diameter × 12 mm length) (Fig. 2). The patient was instructed to maintain a liquid or semiliquid diet for the first three days and then gradually return to a normal diet. Painkiller medications (Aulin®, nimesulide 100 mg, Roche, Italy) were prescribed and adopted by patient when needed. A two-stages surgery was adopted and the implant healed completely covered and uneventfully. The surgical uncovering of the implant was performed 4 months later and an healing abutment was connected to the implant. Fifteen days after the suture removal an impression was taken and a temporary methacrylate resin FPD connecting the implant and the tooth # 29 was delivered. Five months following the implant placement a pick-up impression with polivinylsiloxane material (Optosil ® and Xantopren®, Bayer, Germany) was performed. A single casting with a proper design to achieve a reduced occlusal surface and avoid excessive deflecting stress was made. In order to prevent premature contacts on the implant occlusal surface and consequent excessive stress to the abutment natural tooth a “group” occlusal model was made. In this type of occlusal model, the residual teeth had the first occlusal contact. A gold-ceramic FPD was finally delivered and cemented. Although the patient was thoroughly informed about the need of a strict periodontal and implant maintenance therapy, he did not show up at the first control visit that was planned 6 months after the prosthetic loading. The first supportive visit was carried out after one year; when the temporary crown on tooth # 28 was removed and a definitive gold alloy and ceramic crown was fixed (Figs. 3, 4). After wards, a supportive therapy program was performed on a regular basis (every 4 to 6 months). The final clinical and radiographic assessment was made on March 2012.
Figure 1.
Baseline X-ray showing the absence of 2.8, 2.9 natural teeth.
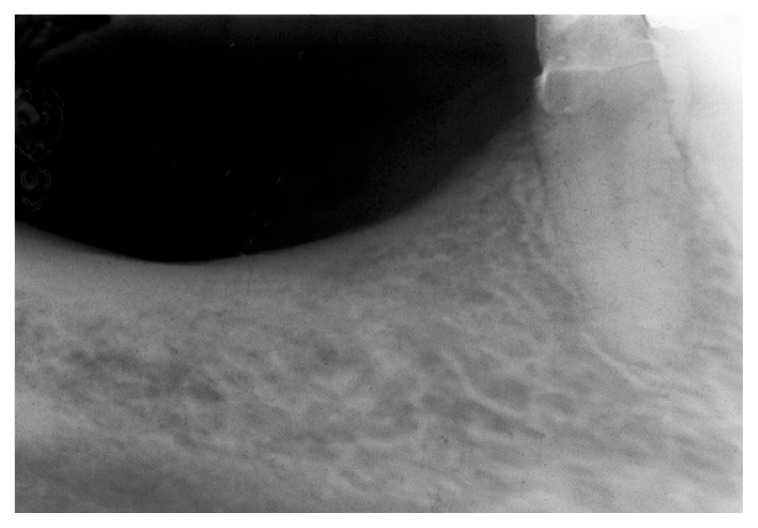
Figure 2.
Periapical X-ray performed following implant placement.
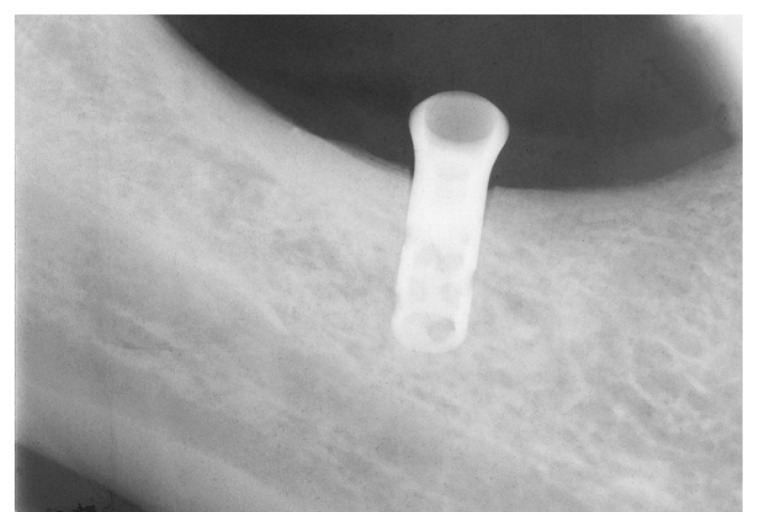
Figure 3.
The fixed partial is rigidly connected between the natural tooth and the dental implant.
Figure 4.
Periapical X-ray performed after fixed partial denture and single crown delivery.
Clinical evaluation
Over the entire period of observation, the following parameters were collected during each examination:
PD around the implant and natural tooth abutment;
gingival index (GI) and modified gingival index (mGI) (10, 11);
occlusal assessment;
marginal bone loss.
Probing depth was recorded at four aspects for both the implant and the natural tooth (mesio and disto buccal, buccal, lingual). Plaque and gingival indices for the natural tooth and modified plaque index (mPI) and gingival index (mGI) for the implant respectively were used. The patient was instructed about proper daily oral hygiene procedures to perform 3 times a day through the use of medium hardness dental brush, interdental brushes, and mouth washes.
Radiographic assessment
Radiographic assessment of peri-implant bone remodeling was performed in a retrospective way according to two previously published papers (14, 15). Briefly, standardized peri-apical radiographs were taken using a Rinn XCP Ring positioner (Dentsply, Constanz, Germany) and a beam guiding rod to allow parallelization between the x-ray tube and the film and standardize all the radiographs. The radiographs were performed with a dental x-ray machine (Dentsply, Constanz, Germany) equipped with a long tube that operated at 70Kw/7.5mA and were developed in an automatic developer under standardized conditions. The radiographs, set on a cephalometric unit in a dark room, were acquired and converted in digital images with a camera, and saved into a computer memory in TIFF format. Later each image was processed with specific software (Scion Image Beta 4.03 for Windows XP, Scion LTD USA) and displayed on a high resolution monitor. A computer assisted calibration was made on mesial and distal side of each implant measuring the known distance between 2 threads. This calibration allowed a correct measurement even if there was a slight deviation of the central beam and a consequent magnification of the image. The following reference points were assessed on each image: fixture-abutment junction, threads, first contact of the crestal bone with the implant on both mesial and distal side. This made possible, with the known values for implant diameter and length, to make linear measurements of remaining peri-implant bone measured from the mesial and distal marginal bone levels and the fixture-abutment junction. The linear measurements were made by a trackball driven cursor on a 10 times magnified digitized image of the implant on the monitor. The amount of bone change over the baseline to a 19 years follow-up observation time was calculated for both the implant and the natural tooth.
Results
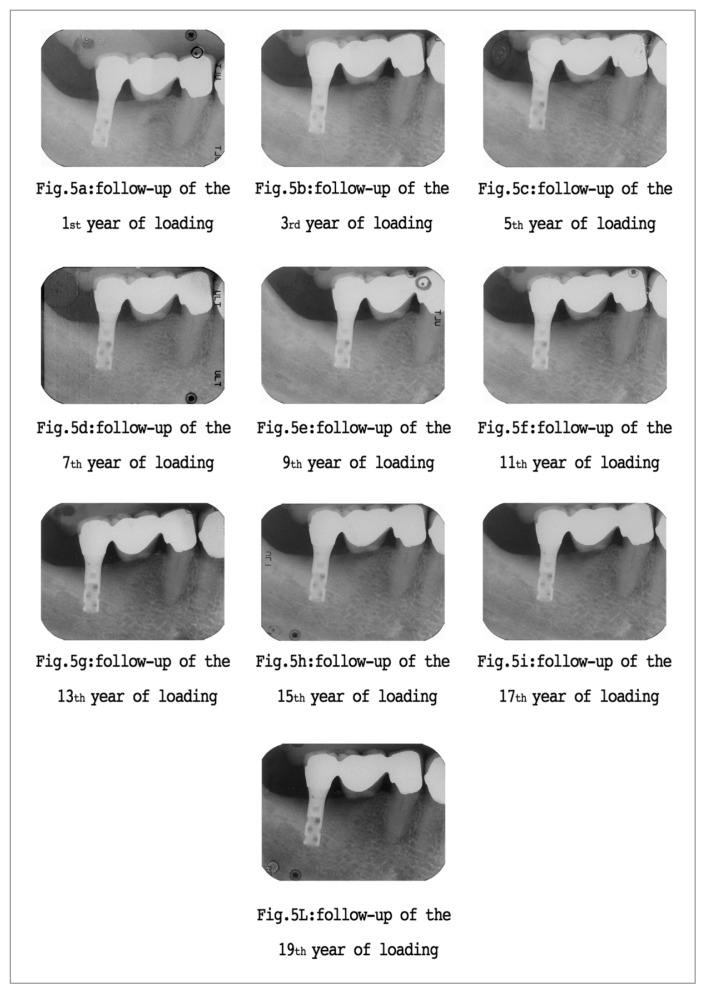
All the clinical and radiographic parameters collected over the entire period of follow-up are reported in Table 1. The values of GI and PI for natural tooth and mGI and mPI for the implant showed a minimal increase over time with a slight increase around the natural tooth during the seventeenth year when the presence of bleeding on probing and calculus was observed. No peri-implant and periodontal pockets were observed during all the follow-up period. No prosthetic complications as discementation, abutment loosening, ceramic or metallic fracture were observed. Peri-apical radiographs did not show any intrusion, even minimal, of the tooth abutment (Fig. 5). Bone remodeling around the two abutments is showed in Table 2. Constant values over the time with slight higher values around the tooth were observed.
Table I.
Clinical parameters during 19-years follow-up.
| Follow-up period | IPD mesio facial | IPD facial | IPD disto facial | IPD lingual | mPI | mGI | TPD mesio facial | TPD facial | TPD disto facial | TPD lingual | PI | GI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 1 year | 2.5 | 2.0 | 2.5 | 2.5 | 0 | 0 | 2.0 | 1.5 | 2.0 | 2.0 | 0 | 0 |
| 3 years | 2.5 | 2.0 | 2.0 | 2.5 | 0 | 0 | 2.0 | 1.5 | 2.0 | 2.0 | 0 | 0 |
| 5 years | 3.0 | 2.0 | 2.5 | 3.0 | 0 | 0 | 2.0 | 2.0 | 2.5 | 2.0 | 0 | 0 |
| 7 years | 3.0 | 2.0 | 2.5 | 3.0 | 1 | 0 | 2.0 | 2.0 | 2.5 | 2.0 | 0 | 0 |
| 9 years | 3.5 | 3.0 | 3.0 | 3.0 | 1 | 1 | 2.5 | 2.0 | 2.5 | 2.5 | 1 | 1 |
| 11 years | 3.5 | 3.0 | 3.0 | 3.0 | 1 | 1 | 2.5 | 2.0 | 3.0 | 2.5 | 1 | 1 |
| 13 years | 3.5 | 3.0 | 3.5 | 3.0 | 1 | 1 | 2.5 | 2.5 | 3.0 | 3.0 | 1 | 1 |
| 15 years | 3.5 | 3.0 | 3.5 | 3.5 | 1 | 1 | 2.5 | 2.5 | 3.0 | 3.0 | 1 | 2 |
| 17 years | 4 | 3.0 | 4.0 | 3.5 | 2 | 1 | 3.0 | 2.5 | 3.0 | 3.0 | 2 | 2 |
| 19 years | 4 | 3.0 | 4.0 | 4.0 | 2 | 2 | 3.0 | 2.5 | 3.5 | 4.0 | 2 | 2 |
| Mean | 3.3 | 2.6 | 3.05 | 3.01 | 0.9 | 0.7 | 2.4 | 2.1 | 2.7 | 2.6 | 0.8 | 0.9 |
NA: Not Assessed
Figure 5.
Periapical X-rays made during the maintenance therapy performed on a two year basis.
Table II.
Peri-implant bone remodeling during 19-years follow-up.
| Follow-up | BIO-OS-TPS IMPLANT | NATURAL TOOTH |
|---|---|---|
| Baseline | 0 | 0 |
| 1st Year following Prosthetic Loading | 0.29 | 0.40 |
| 3rd Year following Prosthetic Loading | 0.31 | 0.41 |
| 5th Year following Prosthetic Loading | 0.21 | 0.45 |
| 7th Year following Prosthetic Loading | 0.18 | 0.47 |
| 9th Year following Prosthetic Loading | 0.29 | 0.48 |
| 11th Year following Prosthetic Loading | 0.31 | 0.46 |
| 13th Year following Prosthetic Loading | 0.30 | 0.49 |
| 15th Year following Prosthetic Loading | 0.21 | 0.47 |
| 17th Year following Prosthetic Loading | 0.30 | 0.48 |
| 19th Year following Prosthetic Loading | 0.20 | 0.45 |
| Total mm | 2.6 | 3.10 |
Discussion and conclusion
Tooth to implant FPDs are characterized by the presence of supporting elements (teeth and implants) that feature a different viscoelastic deformation. This may determine tooth intrusion and the possibility of lateral movement followed by a fast viscoelastic return. Implants have very reduced movements compared to natural teeth. For these reasons, tooth to implant FPDs should be planned and made after a very careful evaluation. In order to correctly select the natural abutment the following parameters should be considered: periodontal status and bone support around the natural tooth. Teeth with clinical mobility should not be used as prosthetic abutments (16). The tooth to implant distance is another key factor. An increased tooth to implant distance may increase shock and cause peri-implant bone remodeling (17). Moreover, the presence of a long intermediate pontic between the implant and the tooth and any axial force applied to the restoration may determine a bending moment of the bridge. This may subject the entire framework to flexion and significantly dislocate the tooth in the apical direction. It is important to emphasize that, although in a different way, dental implants allow modulation of functional occlusal loads similarly to teeth. To better understand the behavior of perimplant bone, which is able of activating a continuous dynamic remodeling in order to adapt to the variations of occlusal loads, it has been introduced the concept of “bone-perception” (17). Some researchers published recommendations that should be considered during the treatment planning of a tooth to implant rehabilitation. Firstly, it is essential to assess the morphology of the natural abutment roots and it is better to use curved or oval-section roots. Secondly, the connection between anterior teeth and implants should be avoided because anterior teeth have a greater horizontal clinical mobility (90–108 μm) compared to implants (18). From the clinical point of view, in order to ensure predictability of the tooth and implant supported restoration, it is appropriate not to splint periodontally compromised dental elements with high mobility since this causes a cantilever with excessive stress on implants with massive loss of peri-implant bone tissue as final result. Some Authors suggested the use of rigid connection to avoid the intrusion of teeth in tooth to implant FPDS (19). Other Authors reviewed the incidence of intrusion in tooth-implant connection and concluded that rigid connections seem to produce the greatest stress on the natural tooth, periodontal ligament and perimplant bone tissue while the non-rigid connections reduce stress on the bone while increasing it on the prosthetic restoration. These Authors observed that FPDs with rigid connection had an higher success rate than non-rigid one (20). Another study carried out on 876 implants in 244 partially edentulous patients rehabilitated with fixed prostheses anchored on implants rigidly connected to the natural elements showed as after 15 years of functioning just one single implant failed while all the remaining implants did not show any functional or stability loss (21). Similar results were published in a review in which a total of 25 papers were included. The Authors concluded that the use of rigid connectors produce clinical results more favorable compared to interlock or to heat sinks of the occlusal load with evident predictability in the long term and reducing severe biological and prosthetic complications as intrusion of natural tooth abutment (22). The TPS screw is a commercially pure titanium implant with a plasma-sprayed surface that was originally described by Ledermann (23). In recent years most of dental implant manufacturers do not produce TPS implants anymore. As a matter of fact, these surfaces were replaced by sandblasted and etched ones (SLA) because it has been shown that medium rough surfaces may increase the bone-implant contact (BIC) in both the early (3 months from healing) and late (12 months) stages of osseointegration process (24). However, different studies did not register any differences in bone covering between the TPS and SLA surfaces (25). We are, of course, aware of the limits of the present case-report and we do think that longitudinal studies about the success and survival rates of tooth to implant restorations are urgently needed. However, in the present case report it was possible to observe the complete functionality and stability of a tooth to implant rigidly connected FPD over a period of 19 years. This paper described the case of a fixed tooth to implant partial denture that has been observed for 19 years. Although a case report manuscript does not feature the highest level of scientific evidence, the present paper describes the successful restoration of an edentulous area with a fixed tooth to implant rehabilitation. The long term success of this case was possible because a very careful treatment planning has been developed. In fact, evaluation of the root morphology of the natural tooth abutment, the adoption of a rigid connection and the design of the pontic are the main key factors for the long term successful restoration of this type of implant prosthetic rehabilitation.
References
- 1.Lang NP, Pjetursson BE, Tan K, Brägger U, Egger M, Zwahlen M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. II. Combined tooth--implant-supported FPDs. Clin Oral Implants Res. 2004;15:643–53. doi: 10.1111/j.1600-0501.2004.01118.x. [DOI] [PubMed] [Google Scholar]
- 2.Muhleman HR. Die physiologische und pathologische Zahnbeweglichkeit. Schweizer Monatsschrift für Zahnheilkunde. 1951:1–71. [PubMed] [Google Scholar]
- 3.Muhleman HR. Periodontometry, a method for measuring tooth mobility. Oral Surgery. 1951;4:1220–1223. doi: 10.1016/0030-4220(51)90080-1. [DOI] [PubMed] [Google Scholar]
- 4.Cohen SR, Orenstein JH. The use of attachments in combination implant and natural tooth fixed partial dentures: a technical report. Int J Oral Maxillofac Implants. 1994;9:230–234. [PubMed] [Google Scholar]
- 5.Jacobs R. Periodontal tactile perception and Peri-implant Osseoperception. In Lindhe J. Clinical Periodontology and Implant Dentistry. Blackwell Munksagaard; 2008. pp. 122–23. [Google Scholar]
- 6.Naert IE, Duyck JA, Hosny MM, et al. Freestanding and tooth-implant connected prostheses in the treatment of partially edentulous patients. Part I: An up to 15-years clinical evaluation. Clin Oral Implants Res. 2001;12:237–44. doi: 10.1034/j.1600-0501.2001.012003237.x. [DOI] [PubMed] [Google Scholar]
- 7.Lin CL, Wang JC, Chang WJ. Biomechanical interactions in tooth-implant-supported fixed partial dentures with variations in the number of splinted teeth and connector type: a finite element analysis. Clin Oral Implants Res. 2008;19:107–17. doi: 10.1111/j.1600-0501.2007.01363.x. [DOI] [PubMed] [Google Scholar]
- 8.Lin CL, Wang JC, Chang SH, et al. Evaluation of stress induced by implant type, number of splinted teeth, and variations in periodontal support in tooth-implant-supported fixed partial dentures: a non-linear finite element analysis. J Periodontol. 2010;81:121–30. doi: 10.1902/jop.2009.090331. [DOI] [PubMed] [Google Scholar]
- 9.Silness J, Loe H. Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 10.Loe H, Silness I. Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–551. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 11.Mombelli A, van Oosten MA, Schurch E, Jr, Land NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987;2:145–51. doi: 10.1111/j.1399-302x.1987.tb00298.x. [DOI] [PubMed] [Google Scholar]
- 12.Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998;17:63–76. doi: 10.1111/j.1600-0757.1998.tb00124.x. [DOI] [PubMed] [Google Scholar]
- 13.Danza M, Tortora P, Quaranta A, et al. Randomised study for the 1-year crestal bone maintenance around modified diameter implants with different loading protocols: a radiographic evaluation. Clin Oral Investig. 2010;14:417–26. doi: 10.1007/s00784-009-0314-0. [DOI] [PubMed] [Google Scholar]
- 14.Quaranta A, Cicconetti A, Battaglia L, Piemontese M, Pompa G, Vozza I. Crestal bone remodeling around platform switched immediately loaded implants placed in sites of previous failures. Eur J Infl. 2012;10:115–122. [Google Scholar]
- 15.Lulic M, Brägger U, Lang NP, et al. Ante’s (1926) law revisited: a systematic review on survival rates and complications of fixed dental prostheses (FDPs) on severely reduced periodontal tissue support. Clin Oral Implants Res. 2007;18:63–72. doi: 10.1111/j.1600-0501.2007.01438.x. [DOI] [PubMed] [Google Scholar]
- 16.Baron M, Haas R, Baron W, et al. Peri-implant bone loss as a function of tooth-implant distance. Int J Prosthodont. 2005;18:427–33. [PubMed] [Google Scholar]
- 17.Klineberg I, Murray G. Osseoperception: sensory function and proprioception. Adv Dent Res. 1999;13:120–9. doi: 10.1177/08959374990130010101. [DOI] [PubMed] [Google Scholar]
- 18.Misch CE, Bidez MW. Implant-protected occlusion: a biomechanical rationale. Compendium. 1994;15:1330, 1332. 1334 passim; quiz 1344. [PubMed] [Google Scholar]
- 19.Sheets CG, Earthman JC. Tooth intrusion in implant-assisted prostheses. J Prosthet Dent. 1997;77:39–45. doi: 10.1016/s0022-3913(97)70205-1. [DOI] [PubMed] [Google Scholar]
- 20.Hita-Carrillo C, Hernández-Aliaga M, Calvo-Guirado JL. Tooth-implant connection: a bibliographic review. Med Oral Patol Oral Cir Bucal. 2010 Mar 1;15(2):e387–94. doi: 10.4317/medoral.15.e387. [DOI] [PubMed] [Google Scholar]
- 21.Jemt T, Lekholm U, Adell R. Osseointegrated implants in the treatment of partially edentulous patients: a preliminary study on 876 consecutively placed fixtures. Int J Oral Maxillofac Implants. 1989;4(3):211–7. [PubMed] [Google Scholar]
- 22.Hoffmann O, Zafiropoulos GG. Tooth-implant connection: a review. J Oral Implantol. 2012;38(2):194–200. doi: 10.1563/AAID-JOI-D-10-00071. [DOI] [PubMed] [Google Scholar]
- 23.Ledermann Ph. Vollprotetische Versorgung des Zahnlosen Problemunterkiefers mit Hilfe von 4 titan-plasmabeschichteten PDL-schraubenimplantaten. Schweiz Mschr Zahnheilk. 1979;89:137–145. [PubMed] [Google Scholar]
- 24.Albrektsson T, Wennerberg A. Oral implant surfaces: Part 2--review focusing on clinical knowledge of different surfaces. Int J Prosthodont. 2004;17(5):544–64. [PubMed] [Google Scholar]
- 25.Cochran DL, Schenk RK, Lussi A, et al. Bone response to unloaded and loaded titanium implants with a sandblasted and acid-etched surface: a histometric study in the canine mandible. J Biomed Mater Res. 1998;40(1):1–11. doi: 10.1002/(sici)1097-4636(199804)40:1<1::aid-jbm1>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]