Abstract
Objective: To investigate which clinical characteristics will influence the pregnancy rate and live birth rate after myomectomy.
Subjects and Methods: Data of clinical characteristics and reproductive outcome from 471 patients who wished to conceive and who underwent abdominal or laparoscopic myomectomy in the Obstetrics and Gynecology Hospital of Fudan University from January 2008 to June 2012 were retrospectively analyzed.
Results: Average age in the pregnancy group (30.0±3.7 years) and the nonpregnancy group (31.2±4.1 years) was statistically different (P=.000). The diameter of the biggest myoma had a positive relationship with the pregnancy rate when it was <10 cm (rs=0.095, P=.039). Abortions before myomectomy, operation type, number, location, and classification of myomas, uterine cavity penetration, and uterine volume seemed not to influence the pregnancy rate (P>.05). The location of the myoma may influence the live birth rate after myomectomy (rs=0.198, P=.002). Anterior and posterior myomas were associated with higher live birth rates than other locations (P=.001). The average interval between myomectomy and pregnancy was 16.0±8.7 months, and there was no difference between the abdominal (17.2±8.6 months) and laparoscopic (15.2±8.8 months) groups (P=.102). The interval in the live birth group was 15.0±8.4 months, and that in the non–live birth group was 18.9±9.3 months; the difference was significant (P=.005).
Conclusions: Patients' age, myoma size and location, and interval between myomectomy and pregnancy may influence the pregnancy rate and live birth rate after myomectomy.
Introduction
As the most common benign solid tumor of the genital system of females, uterine myoma is diagnosed in 25%–30% of females during their lives.1 Uterine myomas are speculated to be the sole cause of infertility in 1%–3% of women and may contribute to infertility in 5%–10% of women.2 Myomas are also estimated to be the cause of approximately 7% of recurrent spontaneous abortions.3
As a uterus-preserving surgery, myomectomy performed either through the abdomen (laparotomy) or laparoscopically is most popular among young women who want to conceive after the operation. Although occurrence is rare, the possibility of uterine rupture during pregnancy or delivery after myomectomy exists.4 Uterine rupture is one of the most severe complications, which can cause both maternal and fetal death. The overall uterine rupture rate in women with previous myomectomy is very low. It was 0.2% in abdominal myomectomy5 and 0.26% in laparoscopic removal.6 As well, it was reported that 53% of patients will present with new myomas in 5 years after myomectomy.7 An appropriate time interval between myomectomy and pregnancy is important. According to our past experience, there should be a 2-year interval between myomectomy and pregnancy. That was considered to be improved because a 3-month contraception time after myomectomy was reported by others.8
It is not clear whether clinical characteristics such as patient age, abortion times before myomectomy, operation type, number, location, and classification of myomas, uterine cavity penetration, and uterine volume could affect the pregnancy and live birth rate after myomectomy. The aim of the present study was to investigate which clinical characteristic can influence the pregnancy rate and live birth rate after myomectomy and to find a proper interval between myomectomy and pregnancy from our experience.
Subjects and Methods
Four hundred seventy-one patients who wanted to conceive after myomectomy were retrospectively investigated in the Obstetrics and Gynecology Hospital of Fudan University from January 2008 to June 2012. Patients with any plausible infertility factor and whose partner's semen analysis was abnormal were excluded. Clinical characteristics including patient age, abortions before myomectomy, operation, myoma number, diameter of biggest myoma, location and classification of myoma, uterine cavity penetration, and uterine volume were investigated and analyzed. Reproductive outcomes including pregnancy rate and live birth rate were investigated. The diagnosis of myomas was reached after pelvic examination and transvaginal ultrasound. Follow-up data regarding fertility and pregnancy outcomes were collected from hospital records or by telephone interview. Myomas were classified into three types: intramural, subserosa, and submucous. The uterine volume was calculated by the formula V=πab2/6 (where a is the long diameter and b is the short diameter). This study was approved by the Ethics Committee of the Obstetrics and Gynecology Hospital of Fudan University. Written informed consents were obtained from all patients.
According to our experience and reported literature, abdominal myomectomy is suitable for patients with large or multiple myomas and for patients with severe adhesions not suitable for the laparoscopic technique. Laparoscopic myomectomy, with less blood loss, shorter hospitalization, faster recovery, and fewer adhesions, is suitable for patients without the above limitations. However, a residual may be left in laparoscopic myomectomy because the surgeon cannot palpate the uterus under laparoscopy. A double layer of sutures using monofilament absorbable suture material (Maxon™; Covidien, Mansfield, MA) was used in either abdominal or laparoscopic myomectomy for intramural myomas. In our study, surgeons told the patients about both kinds of myomectomies, and the patients chose the type of operation by themselves. The same group of surgeons was involved in either the laparoscopic or abdominal myomectomy procedure.
Patients were discharged from the hospital after ambulation without postoperative fever. All patients were examined at the outpatient clinic 1 month later and then every 6 months after that. It was recommended that patients wait for an interval of 6–24 months before trying to conceive.
Statistical analysis was performed using SPSS version 16.0 software (SPSS Inc., Chicago, IL). Continuous data were expressed as mean±standard deviation values. Nonparametric variables were expressed as median and interquartile range. Student's t test and nonparametric tests were used as appropriate. The chi-squared test and Fisher's exact test were used for cross-tabulated comparison. The correlation was assessed with Spearman correlation coefficients. Differences were considered to be significant at P<.05.
Results
Of the 471 patients who successfully finished the investigation, 237 patients subsequently conceived, and 156 patients had a live birth after myomectomy. The median length of follow-up was 31 months (range, 6–47 months). The pregnancy rate was 50.3%, the live birth rate was 33.1%, the relapse rate was 5.5%, and there were no uterine ruptures.
The clinical characteristics of the pregnancy and nonpregnancy groups are given in Table 1. There were no statistically significant differences in abortions before myomectomy, operation, number, location, or classification of myomas, uterine cavity penetration, and uterine volume in the two groups (P>.05). Patients' age in the pregnancy group was 30.0±3.7 years, and that in the nonpregnancy group was 31.2±4.1 years; the difference was significant (P=.000). The diameter of the biggest myoma was larger in the pregnancy group than in the nonpregnancy group when it was <10 cm (P<.05).
Table 1.
Comparison of Clinical Characteristics of Pregnancy and Nonpregnancy Groups
| Characteristic | Pregnancy (n=237) | No pregnancy (n=234) | P value |
|---|---|---|---|
| Age (years) | 30.0±3.7 | 31.2±4.1 | .000 |
| Abortions before myomectomya | 0 (1) | 0 (1) | .996 |
| Operation (laparoscopy/abdominal) | 139/98 | 141/93 | .778 |
| Myoma numbera | 2 (2) | 1 (2) | .283 |
| Diameter of biggest myoma | 6.3±1.9 | 5.8±1.6 | .002 |
| ≤5 cm | 4.8±0.6 | 4.4±0.9 | .001 |
| 5–10 cm | 7.2±1.3 | 6.8±1.1 | .003 |
| >10 cm | 11.9±0.4 | 11.5±0.7 | .286 |
| Location of myomas | rs=0.064 | .163 | |
| Classification of myomas | rs=0.011 | .811 | |
| Intramural (%) | 50.1% (214/427) | ||
| Subserosa (%) | 55% (22/40) | ||
| Submucous (%) | 25% (1/4) | ||
| Uterine cavity penetration (n) | 19 | 18 | 1.000 |
| Uterine volume | rs=0.082 | .075 |
Data are mean±standard deviation values unless indicated otherwise.
Median (interquartile range) values.
The differences between the live birth and non–live birth groups are explained in Table 2. There were no statistically significant differences in age, abortions before myomectomy, operation, myoma number, diameter of biggest myoma, classification of myomas, uterine cavity penetration, and uterine volume between the two groups (P>.05). A different location of the myomas can influence the live birth rate (rs=0.198, P=.001), with a 34.0% pregnancy rate for anterior myomas, 44.2% for posterior myomas, and 21.8% for others. The interval between myomectomy and pregnancy in the live birth group was 15.0±8.4 months, and that in the non–live birth group was 18.9±9.3 months; the difference was significant (P=.005).
Table 2.
Comparison of Clinical Characteristics of Live Birth and Non–Live Birth Groups
| Characteristic | Live birth (n=156) | Non–live birth (n=81) | P value |
|---|---|---|---|
| Age (years) | 29.9±3.9 | 29.0±3.2 | .094 |
| Abortions before myomectomya | 0 (1) | 0 (1) | .424 |
| Operation (laparoscopy/abdominal) | 93/63 | 46/35 | .679 |
| Myoma numbera | 1 (2) | 1 (2) | .693 |
| Diameter (cm) of biggest myoma | 6.4±2.0 | 6.3±1.8 | .829 |
| Location of myomas | rs=0.198 | .002 | |
| Anterior (%) | 34.0% (53/156) | ||
| Posterior (%) | 44.2% (69/156) | .001 | |
| Others (%) | 21.8% (34/156) | ||
| Classification of myomas | rs=0.087 | .184 | |
| Uterine cavity penetration (n) | 14 | 5 | .615 |
| Uterine volume | rs=0.097 | .137 | |
| Interval (months) | 15.0±8.4 | 18.9±9.3 | .005 |
Data are mean±standard deviation values unless indicated otherwise.
Median (interquartile range) values.
The comparison of laparoscopic and abdominal myomectomy is given in Table 3. The pregnancy rate was 49.6% in the laparoscopic group and 51.3% in the abdominal group; the difference was not significant (P=.397). The live-birth rate was 33.2% in the laparoscopic group and 33.0% in the abdominal group; the difference was not significant (P=.520). In our results, the hospital stay was significantly shorter in the laparoscopic group than in the abdominal group (P<.05). The operation time in the laparoscopic group was longer than in the abdominal group (P<.05). There was no difference in uterine rupture, blood loss, and relapse in the two groups (P>.05). The average interval between myomectomy and pregnancy was 16.0±8.7 months, and there was no difference between the abdominal (17.2±8.6 months) and laparoscopic (15.2±8.8 months) groups (P=.102).
Table 3.
Comparison of Laparoscopic and Abdominal Myomectomy
| Characteristic | Laparoscopic (n=280) | Abdominal (n=191) | P value |
|---|---|---|---|
| Pregnancy rate (%) | 49.6% (139/280) | 51.3% (98/191) | .397 |
| Live birth rate (%) | 33.2% (93/280) | 33.0% (63/191) | .520 |
| Interval (months) | 15.2±8.8 | 17.2±8.6 | .102 |
| Uterine rupture (n) | 0 | 0 | — |
| Operation time (minutes) | 93.2±37.9 | 71.0±24.8 | .001 |
| Blood loss (mL) | 100.9±72.1 | 142.8±141.9 | .107 |
| Hospitalization (days) | 6.5±1.8 | 7.4±2.0 | .024 |
| Relapse (n/total) | 11/280 | 15/191 | .053 |
Data are mean±standard deviation values unless indicated otherwise.
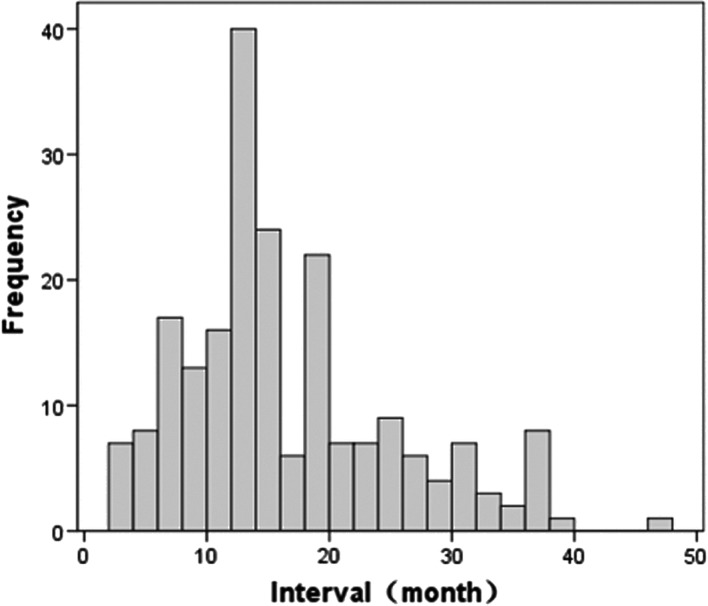
A 12-month interval between myomectomy and pregnancy occurred with the highest frequency in all pregnant patients (Fig. 1).
FIG. 1.
Interval between myomectomy and pregnancy for all pregnant patients. The interval with the highest frequency was 12 months.
Discussion
In this retrospective study, patients chose the type of myomectomy following a description of the procedures by surgeons themselves. Studies suggested that in selected patients, the pregnancy rate was about 50%–60% with both the laparoscopic and abdominal approaches.9 In our results, the pregnancy rate in the abdominal group was 51.3%, a little bit lower than the 57% reported by Vercellini et al.10 Younger people have a higher pregnancy rate, as the average age (30.0±3.7 years) in the pregnancy group was statistically younger than in the nonpregnancy group (31.2±4.1 years).
Several hypotheses have been proposed to explain the mechanisms of how myomas can induce infertility11: myomas can cause uterine contraction, which can interfere with sperm migration and ovum transport, or myomas may enlarge the anatomical uterine cavity and secrete inflammatory and vasoactive substances, which may cause implantation failure.
As well, different classifications of myomas have different impacts on reproductive outcomes.12 Submucosal myomas can decrease pregnancy and live births rate,13 and intramural myomas may impair fertility,14 whereas subserosal myomas may not impair fertility or pregnancy loss. In our study, there were 427 cases of intramural myomas, 40 subserosal myomas, and only 4 submucosal myomas. The pregnancy rate was similar in the intramural and subserosal groups, and they were higher than in the submucosal group, although the difference was not statistically meaningful.
In our result, the sizes of myomas also impact fertility or pregnancy loss: the diameter of the biggest myoma was larger in the pregnancy group than in the nonpregnancy group, when it was <10 cm. This may be explained by the reasoning that the bigger the myoma, the easier it can be diagnosed and the earlier it can be operated on to yield a better outcome. Different locations of myomas can influence the live birth rate; we measured rates of 34.0% in anterior myomas, 44.2% in posterior myomas, and 21.8% in others.
Abdominal myomectomy was first introduced by Boney in 1931, as summarized elsewhere.15 It has been the standard approach of conservative treatment of uterine myomas for years. It is suitable for women with large or multiple myomas, for those with myomas located at very special points, or when suspected in cases of severe adhesions in the pelvic. Laparoscopic myomectomy was first introduced by Semm in 1979 for subserous myomas.16 In the beginning of the 1990s, the procedure began to be performed in intramural myomas. Now it is one of the most common surgical procedures in infertile patients. Laparoscopic myomectomy is noted by less blood loss, fewer adhesions after operation, faster recovery, and shorter hospitalization compared with abdominal myomectomy.9,17 In our results, the hospital stay was significantly shorter in the laparoscopic group than in the abdominal group. As well, there was no difference in pregnancy rate and live birth rate between the two groups.
Laparoscopic myomectomy has the shortcoming of difficulty in diagnosing small and multiple myomas without palpation of the uterine; hence small myomas may be missed. It has been reported that the recurrence rate of myomas was higher in laparoscopic myomectomy compared with laparotomy.18 In our results, the relapse rate in the two groups was not statistically different; it might because the observation time was limited. In our results, the operation time in the laparoscopic group was obviously longer than in the abdominal group. The difference was because of the difficulty with morcellation and removal and that the technical requirements for manipulation of needles and suture make the laparoscopic procedure difficult to perform.19
Uterine rupture during pregnancy and delivery is one of the most severe complications after myomectomy. It may be associated with intracorporeal tissue damage from electrocoagulation and incomplete wound formation due to the difficulty of suturing.18,20 A study of uterine wound healing using magnetic resonance imaging demonstrated that the uterine healing process was complete at 12 weeks after abdominal myomectomy in the absence of hematoma or edema formation in the myometrium.21 Another factor that affects uterine rupture is the time interval between myomectomy and first pregnancy. According to our previous experiences, most surgeons in our hospital recommended 6–24 months of contraception use after myomectomy. In this study, the average interval between myomectomy and pregnancy was 16.0±8.7 months, and there was no difference between the abdominal and laparoscopic groups. However, the average interval in the live birth group was much shorter than in the non–live birth group. This indicates that a shorter interval may have better reproductive outcomes. From Figure 1, we can conclude that a 12-month interval was suitable after myomectomy in this study. However, we should shorten the interval between myomectomy and pregnancy in appropriate cases.
In conclusion, patients' age, myoma size and location, and interval between myomectomy and pregnancy may influence the pregnancy rate and live birth rate after myomectomy. Laparoscopic myomectomy performed by an experienced surgeon on appropriate patients can be considered as a safe and attractive alternative to abdominal myomectomy with similar reproductive outcomes.
Acknowledgments
The authors thank colleagues in the Medical Record Department for providing data and Xiao Ju Lu for performing the telephone interviews.
Disclosure Statement
No competing financial interests exist.
References
- 1.Mettler L, Schollmeyer T, Tinelli A, Malvasi A, Alkatout I. Complications of uterine fibroids and their management, surgical management of fibroids, laparoscopy and hysteroscopy versus hysterectomy, haemorrhage, adhesions, and complications. Obstet Gynecol Int 2012;2012:791248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kolankaya A, Arici A. Myomas and assisted reproductive technologies: When and how to act? Obstet Gynecol Clin North Am 2006;33:145–152 [DOI] [PubMed] [Google Scholar]
- 3.Khaund A, Lumsden MA. Impact of fibroids on reproductive function. Best Pract Res Clin Obstet Gynaecol 2008;22:749–760 [DOI] [PubMed] [Google Scholar]
- 4.Myomas and reproductive function. Fertil Steril 2008;90(5 Suppl):S125–S130 [DOI] [PubMed] [Google Scholar]
- 5.Parker WH, Einarsson J, Istre O, Dubuisson JB. Risk factors for uterine rupture after laparoscopic myomectomy. J Minim Invasive Gynecol 2010;17:551–554 [DOI] [PubMed] [Google Scholar]
- 6.Sizzi O, Rossetti A, Malzoni M, Minelli L, La Grotta F, Soranna L, et al. Italian multicenter study on complications of laparoscopic myomectomy. J Minim Invasive Gynecol 2007;14:453–462 [DOI] [PubMed] [Google Scholar]
- 7.Yoo EH, Lee PI, Huh CY, Kim DH, Lee BS, Lee JK, et al. Predictors of leiomyoma recurrence after laparoscopic myomectomy. J Minim Invasive Gynecol 2007;14:690–697 [DOI] [PubMed] [Google Scholar]
- 8.Palomba S, Zupi E, Falbo A, Russo T, Marconi D, Tolino A, et al. A multicenter randomized, controlled study comparing laparoscopic versus minilaparotomic myomectomy: Reproductive outcomes. Fertil Steril 2007;88:933–941 [DOI] [PubMed] [Google Scholar]
- 9.Malzoni M, Tinelli R, Cosentino F, Iuzzolino D, Surico D, Reich H. Laparoscopy versus minilaparotomy in women with symptomatic uterine myomas: Short-term and fertility results. Fertil Steril 2010;93:2368–2373 [DOI] [PubMed] [Google Scholar]
- 10.Vercellini P, Maddalena S, De Giorgi O, Aimi G, Crosignani PG. Abdominal myomectomy for infertility: A comprehensive review. Hum Reprod 1998;13:873–879 [DOI] [PubMed] [Google Scholar]
- 11.Goldberg J, Pereira L. Pregnancy outcomes following treatment for fibroids: Uterine fibroid embolization versus laparoscopic myomectomy. Curr Opin Obstet Gynecol 2006;18:402–406 [DOI] [PubMed] [Google Scholar]
- 12.Pritts EA, Parker WH, Olive DL. Fibroids and infertility: An updated systematic review of the evidence. Fertil Steril 2009;91:1215–1223 [DOI] [PubMed] [Google Scholar]
- 13.Jayakrishnan K, Menon V, Nambiar D. Submucous fibroids and infertility: Effect of hysteroscopic myomectomy and factors influencing outcome. J Hum Reprod Sci 2013;6:35–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brady PC, Stanic AK, Styer AK. Uterine fibroids and subfertility: An update on the role of myomectomy. Curr Opin Obstet Gynecol. 2013;25:255–259 [DOI] [PubMed] [Google Scholar]
- 15.Kalogiannidis I, Prapas N, Xiromeritis P, Prapas Y. Laparoscopically assisted myomectomy versus abdominal myomectomy in short-term outcomes: A prospective study. Arch Gynecol Obstet 2010;281:865–870 [DOI] [PubMed] [Google Scholar]
- 16.Semm K. New methods of pelviscopy (gynecologic laparoscopy) for myomectomy, ovariectomy, tubectomy and adnectomy. Endoscopy 1979;11:85–93 [DOI] [PubMed] [Google Scholar]
- 17.Kumakiri J, Kikuchi I, Kitade M, Matsuoka S, Kono A, Ozaki R, et al. Association between uterine repair at laparoscopic myomectomy and postoperative adhesions. Acta Obstet Gynecol Scand 2012;91:331–337 [DOI] [PubMed] [Google Scholar]
- 18.Desai P, Patel P. Fibroids, infertility and laparoscopic myomectomy. J Gynecol Endosc Surg 2011;2:36–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Munro MG. Uterine leiomyomas, current concepts: Pathogenesis, impact on reproductive health, and medical, procedural, and surgical management. Obstet Gynecol Clin North Am 2011;38:703–731 [DOI] [PubMed] [Google Scholar]
- 20.Darwish AM, Nasr AM, El-Nashar DA. Evaluation of postmyomectomy uterine scar. J Clin Ultrasound 2005;33:181–186 [DOI] [PubMed] [Google Scholar]
- 21.Tsuji S, Takahashi K, Imaoka I, Sugimura K, Miyazaki K, Noda Y. MRI evaluation of the uterine structure after myomectomy. Gynecol Obstet Invest 2006;61:106–110 [DOI] [PubMed] [Google Scholar]