Abstract
Background: Aggregation of metabolic risk factors—i.e., elevated plasma triglyceride (TG), reduced high-density lipoprotein cholesterol (HDL-C), elevated blood pressure, and raised plasma glucose—convey increased risk for atherosclerotic cardiovascular disease and type 2 diabetes.
Methods: This study was carried out to determine the association of waist girth, ethnicity, and gender with susceptibility for metabolic risk. Included were 1671 adult women (50.7% black) and 1339 men (46.5% black) enrolled in the Dallas Heart Study. Subjects were stratified into three categories by waist girth—low, intermediate, and high, corresponding to BMI ranges of <25 kg/m2, 25–29.9 kg/m2, and ≥30 kg/m2.
Results: Risk factor prevalence rose progressively through each waist-girth category. However, even among those with high waist-girth, prevalence of three or more risk factors was less than 50%. Several differences among the ethnic groups were noted; for example, Hispanic men had a higher prevalence of elevated TG compared to whites; black men, on the other hand, had a lower frequency of high TG. There were also fewer black men with low HDL-C than in the other groups. Black and Hispanic men had a higher prevalence of elevated glucose and updated homeostasis model assessment of insulin resistance (HOMA2-IR) than whites. More black men had elevated blood pressure than other groups. These differences were less pronounced among ethnic groups of women.
Conclusion: Although ethnic and gender differences in risk factor prevalence may exist, it is notable that the majority of subjects, even when obese, did not have elevated risk factors. This finding points to the need to focus largely on subjects with metabolic risk factors when implementing therapeutic interventions.
Introduction
The metabolic syndrome is an aggregation of several metabolic risk factors, including elevated plasma triglyceride (TG), reduced high-density lipoprotein cholesterol (HDL-C), elevated blood pressure, and raised plasma glucose.1,2 This aggregation is recognized as a multiplex risk factor for atherosclerotic cardiovascular disease (ASCVD) and type 2 diabetes mellitus (T2DM).1–3 Metabolic risk factors are more common in obese individuals. For this reason, obesity is commonly included in the clinical definition of metabolic syndrome. Even so, obesity is more of a susceptibility factor for the syndrome than a direct cause of ASCVD or diabetes. The metabolic syndrome is variably expressed in the general population.4–6 In this study, we examined variable manifestations of the components of the syndrome in white, black, and Hispanic men and women of the Dallas Heart Study (DHS).7 Categorical risk factors were plotted as a function of waist circumference (WC), which is the usual measure of obesity employed to identify the syndrome. The purpose was to determine differences in susceptibilities for metabolic risk factors.
Methods
Among all the subjects of the DHS,7 the current sample contained 1671 women (50.7% black, 31.3% white, 18.1% Hispanic) and 1339 men (46.5% black, 37.3% white, 16.3% Hispanic). DHS study participants of other ethnicities were excluded from the study. All participants consented to participate in an Institutional Review Board–approved study.
Risk factor measurements
Height, weight, waist circumference, blood pressure, fasting plasma lipids, glucose, and insulin, were measured as described.7 Insulin sensitivity was estimated with the updated homeostasis model assessment of insulin resistance (HOMA2-IR) computer model (HOMA Calculator version 2.2).8 Abnormal homeostasis assessment (HOMA2-IR) values were defined as above 1.63, which was the 75th percentile for HOMA derived from the 1169 subjects of this study who had a BMI less than 30 kg/m2. The large Bruneck study reported similar results.9
Categorical metabolic risk factors were defined as elevated fasting TG ≥150 mg/dL; reduced HDL-C <40 mg/dL in men and <50 mg/dL in women; fasting glucose ≥100 mg/dL; and systolic blood pressure (SBP) ≥130 mmHg or on hypertensive medication. These factors are those listed in consensus recommendations. The presence of three or more metabolic risk factors was defined as a high metabolic risk.10 Individuals who were treated for hypertension (7.3% of men and 8.9% of women) were included in the “at risk” category. None of the subjects included were taking statins and non were reported to have T2DM.
Waist girths
Three categories of waist girth were defined for this study—low, intermediate, and high. They were defined to correspond to body mass indexes (BMIs) of <25 kg/m2, 25–29.9 kg/m2, and ≥30 kg/m2. Values for waist girth were derived in two ways that were congruent. First, Zhu et al.11 defined these cut-points based on National Health and Nutrition Examination Survey III (NHANES III) data; and second, we found essentially the same cut-points from regressions of DHS data. Low waist girth corresponded to <90 cm in men and <80 cm in women; intermediate waist girths were 90–101 cm in men and 80–89 cm in women; and high waist girths were ≥102 cm in men and ≥90 cm in women.
Statistics
Data are summarized as means±standard deviation (SD or standard error (SE) for metabolic parameters. Comparisons of means of metabolic risk factors among ethnic groups within each gender were done using analysis of variance (ANOVA) with Bonferroni adjustments as needed (P<0.02) or without Bonferroni adjustments in selected cases but using a post hoc Fisher test (P<0.05). Comparisons of percentages with metabolic risks within each gender and ethnic group was done by using a difference in proportions test, provided that the samples satisfied the standard binomial requirement for the product of sample size. A SAS version of StatView (version 5.1.26) was employed for the analyses.
Results
Table 1 shows the characteristics for DHS subjects. There was a high prevalence of obesity as shown by relatively high BMI values. Hispanic men and women were about 5 years younger on average than whites; blacks were the same age as whites. Black men and women had lower TG levels than the other groups; black men, but not black women, also had higher HDL-C levels than the two other groups. White men and women had lower fasting glucose levels compared to men and women of the other groups; the same differences were noted for HOMA2-IR (Table 1). Black men and women on average had higher SBP values than men and women of the other ethnic groups; the same table shows that black men had a lower mean non-HDL-C than white and Hispanic men, but there were no differences in non-HDL-C levels among the three groups of women.
Table 1.
Subject Demography and Metabolic Factors
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Black | White | Hispanic | Black | White | Hispanic | |
| Mean±SD | Mean±SD | |||||
| Number | 653 | 469 | 217 | 887 | 489 | 295 |
| Age (years) | 46±10 | 45±9 | 41±9a | 45±10 | 46±10 | 41±9a |
| Body mass index (kg/m2) | 29.5±6.8 | 28.9±5.5 | 29.4±4.6 | 33.6±8.7b | 29.2±7.6 | 31.4±7.9a |
| Waist circumference (cm) | 100.6±16.8 | 102.5±14.2 | 99.2±11.0a | 102.1±17.7b | 92.9±17.1 | 95.5±16.9d |
| Triglyceride mg/dL* | 90 (72)b | 119 (106) | 131 (111)d | 81 (55)b | 102 (78) | 110 (77)d |
| HDL-C | 50±15b | 42±10 | 42±10 | 54±15 | 54±17 | 49±12a |
| Non-HDL-C | 128±43b | 142±39 | 145±42 | 126±43 | 129±39 | 128±38 |
| Glucose | 108±52 | 98±29c | 104±34 | 104±47 | 97±34c | 108±48 |
| Insulin μU/mL* | 12.2 (14.9) | 10.8 (11.9) | 13.1 (11.9) | 15.3 ( 13.5) | 9.8 (10.8)e | 14.8 (14.5) |
| HOMA2-IR* | 1.63 (1.93) | 1.42 (1.51) | 1.72 (1.57)d | 2.01 (1.77) | 1.28 (1.42)e | 1.93 (2.01) |
| Systolic blood pressure | 132±18 | 127±13c | 124±13a | 130±19b | 121±15 | 119±16 |
Median (interquartile).
Significantly different from white and black; P<0.001.
Significantly different from white and Hispanic (P<0.001).
Significantly different from black (P<0.001).
Significantly different from white [analysis of variance (ANOVA) with post hoc Fisher protected least significant difference (PLSD) (P<0.05)].
Significantly different from black and Hispanics (P<0.001).
ANOVA with Bonferroni adjustments (P≤0.0167).
SD, standard deviation; HDL-C, high-density lipoprotein cholesterol; HOMA2-IR, updated homeostasis model assessment of insulin resistance.
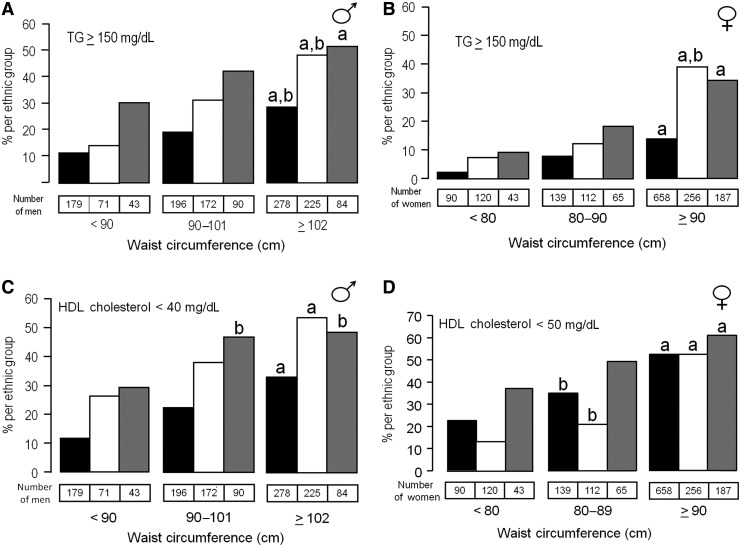
Among individual risk factors, the prevalence of elevated TG was strongly dependent on waist girth in all ethnic groups (Fig. 1). The same pattern was noted for reduced HDL-C. Persons with intermediate waist girth were more likely to have both elevated TG and reduced HDL-C levels than were those with low waist girth. Of note, the majority of persons with intermediate waist circumferences did not have either elevated TG or reduced HDL-C levels. In those with high waist girth, frequencies of abnormalities in TG and HDL-C varied between 25% and 50%. An exception was in obese, African American women, who had a low prevalence of elevated TG levels.
FIG. 1.
Percent of men (A) and women (B) of three ethnic origins black (black bars), white (white bars), Hispanic (gray bars) with high triglyceride (TG) levels (TG ≥150 mg/dL) as a function of obesity. Classification according to waist girth was made as follows: nonobese (<90 cm for men and <80 cm for women), overweight (90–101 cm for men and 80–89 cm for women), and obese (≥102 cm for men and ≥90 cm for women). The prevalence of high-risk TG increased with increasing waist girth in black (black bars) and white (white bars) men (a,bP<0.05) (A). A high prevalence of at-risk TG was present in the Hispanic group at any waist girth, although the prevalence was not significantly different between the overweight and obese groups but only between the nonobese and obese groups (aP<0.05) (A). In women (B), significantly higher prevalences of high-risk TG were noted in obese compared to overweight in each of the three ethnic groups (aP<0.05). In white women, the prevalence of high-risk TG was also significantly higher in obese compared with nonobese (bP<0.05). High-risk prevalence of high-density lipoprotein cholesterol (HDL-C) is summarized for men (C) and women (D). Obese black and white men and women had a higher prevalence of low HDL-C compared with overweight and nonobese (aP<0.05) (C and D); obese and overweight Hispanic men had higher prevalence of low HDL-C than nonobese (cP<0.05); but overweight and obese men had similar prevalences of low HDL-C. In contrast, Hispanic obese women had a higher prevalence of low HDL-C than overweight or nonobese (aP<0.05) (D).
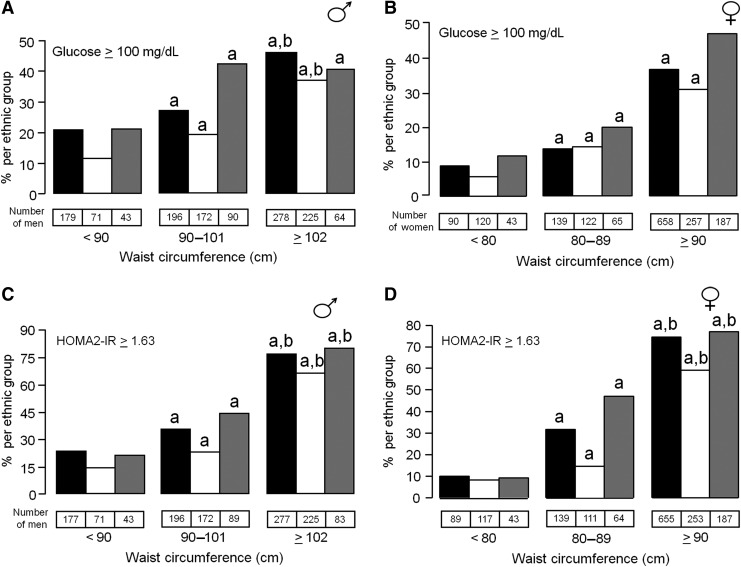
The prevalence of elevated glucose levels was consistently higher in all groups with intermediate waist girth compared to low waist girth, and the prevalence generally rose even higher at high waist girth (Fig. 2). Fasting glucose levels generally were lower in whites than in blacks or Hispanics at all waist-girth categories. The prevalence of IR, as reflected by HOMA2-IR, rose strikingly with increasing obesity. In those with high waist girth, 60%–70% had elevated HOMA2-IR. The frequency was substantially lower in subjects with intermediate waist girth, although the frequency was higher than in the group with low waist girth. Still, the majority of subjects with intermediate waist girth did not manifest an elevated HOMA2-IR. In blacks and Hispanics, percentages with elevated HOMA-IR were numerically higher than those for whites; this was true for both men and women.
FIG. 2.
Black (black bars), white (white bars), Hispanic (gray bars). The prevalence of increased fasting blood glucose in blacks and whites increases (a P<0.05) with increases in waist girth in men (A) and women (B). The prevalence was also higher in obese compared to overweight men and women of the same ethnic groups (bP<0.05). Overweight and obese Hispanics men (A) also had a high prevalence of high-risk fasting glucose (aP<0.05) compared with nonobese. Prevalence of high updated homeostasis model assessment of insulin resistance (HOMA2-IR) values was high in obese and overweight men of each ethnic group compared with nonobese (aP<0.05) (C). In addition, obese men also had a higher prevalence of increased HOMA2-IR values compared to overweight men. Similar observations were made in women (D).
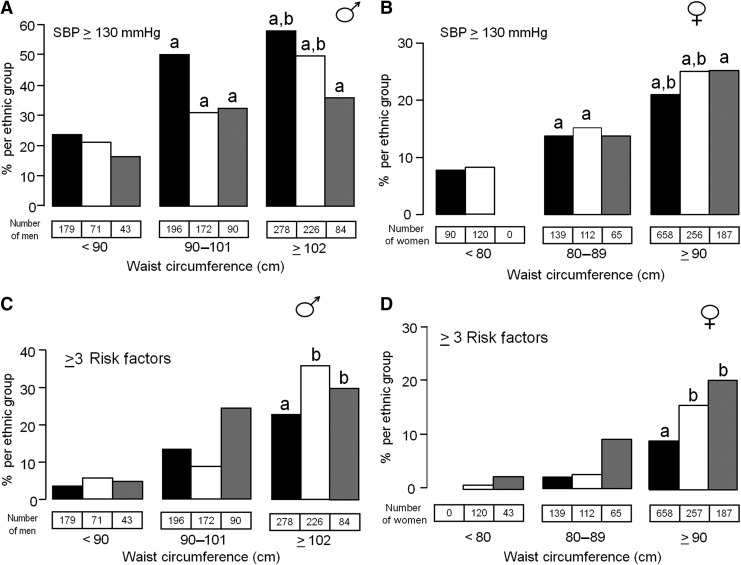
Elevations in blood pressure occurred stepwise from low to intermediate to high waist girths (Fig. 3). Compared to the other ethnicities, black men, but not women, had a greater frequency of elevated SBP with increasing waist girth category. At higher waist girths, black men appeared to be extremely susceptible to elevated blood pressure compared to other ethnicities.
FIG. 3.
Black (black bars), white (white bars), Hispanic (gray bars). The percent of men with high risk systolic blood pressure (SBP) was significantly higher in obese and overweight men compared to nonobese for each ethnic group (aP<0.05) (A). Obese black men had a higher percentage of subjects with three or more risk factors compared with nonobese (aP<0.05) and overweight (bP<0.05), whereas obese white and Hispanic men had significantly higher percentage of subjects with three or more risk factors compared to overweight (bP<0.05) (C). Similar trends were noted in women (B and D).
The frequency of multiple metabolic risk factors in men rose sharply at intermediate waist girth, but was still higher at high waist girth (Fig. 3). In women, occurrence of three or more risk factors was only modestly elevated in those with waist girth in the intermediate range, but was even greater in those in the high waist-girth category. But even with high waist girth, the frequency of three or more risk factors in women was less than 20%.
Discussion
This study showed that increasing waist girth is associated with a rise in all metabolic risk factors in black, white, and Hispanic men and women. The metabolic risk factors accompanying increased adipose tissue are believed to be related to abnormal production by adipose tissue of nonesterified fatty acids (NEFA) and other adipokines, such as adiponectin and inflammatory cytokines.12 But an important observation in the current study was that among those with high waist girth, or what is called abdominal obesity in the United States,2 only about one-half or less had categorical metabolic risk factors. Conversely, in all ethnic groups, a sizable portion with high waist girths were resistant to the development of risk factors. Moreover, less than a third of men and less than a fifth of women with high waist girths had three or four metabolic risk factors. These findings do not minimize the impact of abdominal obesity on metabolic risk factors for the population as a whole, but they do show the importance of individual variability in susceptibility for their development.
In other regions of the world, the threshold for abdominal obesity is set at a lower level, typically being 90–94 cm in men and 80 cm in women.2 In the current study, we defined intermediate waist girth to be in the range of 90–101 cm in men and 80–90 cm in women. These ranges correspond closely to a BMI range of 25–29.9 kg/m2. In this intermediate category, metabolic risk factors were more common than in those with low waist girths, but, on the whole, they were less prevalent than in subjects with high waist girths. These findings nonetheless add support for including intermediate waist girth in the definition of abdominal obesity, as advocated by some investigators.2 Yet such a definition must be made with an understanding that susceptibility for developing metabolic risk factors with intermediate waist girths is lower than in those with high waist girths.
The prevalence of elevated TG rose stepwise with increasing waist girth in all ethnic groups; HDL-C levels fell in parallel with greater waist girths. Presumably a higher prevalence of elevated TG associated with increasing waist girth was due to higher NEFA levels accompanying a greater pool of adipose tissue,13 as well as to secondary IR in muscle.14 The mechanisms whereby obesity lowers HDL-C are not fully understood, but may be related to at least two factors: (1) Exchange of cholesterol in HDL for TG in very-low-density lipoprotein (VLDL),15 and (2) reduced adiponectin levels.16 Regardless of mechanism, it must be noted that majority of persons with intermediate and high waist circumferences did not have either elevated TG or reduced HDL-C.
Increasing obesity is known to be accompanied by greater IR. This relationship was reflected in the frequency of elevated HOMA2-IR in different waist-girth categories. In the high waist circumference category, the majority of subjects in all groups had elevated HOMA2-IR. Although elevated HOMA2-IR was less common in the intermediate waist-girth category, it nonetheless exceeded that of the low waist girth. Even so, the majority of subjects with intermediate waist girth did not have elevated HOMA2-IR. There appeared to be differences in the proportions with elevated HOMA2-IR among the three groups. Blacks appeared to have more IR than whites. This difference has been reported previously.17,18 A similar difference was noted between Hispanics and whites.17 The reasons for these ethnic differences have not been determined.
The frequencies of elevated fasting glucose rose with increasing waist girth, but were less common than were elevations in HOMA2-IR. Moreover, ethnic and gender elevations in glucose were less pronounced than for HOMA2-IR. Glucose elevations are the result of the combination of IR and decreased insulin secretion. This combination of abnormalities seemingly is less common than increases of elevated HOMA2-IR alone. T2DM has been reported to be more common in backs and Hispanics than in whites.19,20 These differences in diabetes rates may be foreshadowed by the somewhat greater frequencies of elevated glucose levels in blacks and Hispanics, compared to whites, both in intermediate and high waist-girth categories.
The observation that elevations in blood pressure rose progressively from low to intermediate to high waist girths strongly implies that elevations of SBP are due in part to metabolic abnormality. How obesity affects blood pressure is not fully understood. Current evidence suggests that multiple factors play a role.21 Some investigators22 recommend that obesity-related hypertension be recognized as a specific disease phenotype requiring special attention to management through weight-reduction strategies. A finding of interest was that blood pressure in black men appeared to be more sensitive to moderate obesity (intermediate waist girth) than were black women and white and Hispanic men. This finding undoubtedly has important public health implications for detection of hypertension in black men.
Multiple metabolic risk factors are indicative of high metabolic risk,23 or the metabolic syndrome.1 In the current study, a high metabolic risk was relatively uncommon at intermediate waist girth except in Hispanic men. At high waist girth, three three or more metabolic risk factors averaged about 30% in men and less than 20% in women. This study raises the question of whether obesity should be considered more of a susceptibility factor for metabolic syndrome than as a component of it.10 If not, obesity could be one of several factors, such as gender and ethnicity, as underlying susceptibility factors for the metabolic syndrome.
In summary, this study contains several features of interest. First, variability in susceptibility to metabolic risk factors among waist girths, gender, and ethnicities is considerable although poorly understood. Whether these differences can be explained by genetic influences, environmental factors, or both remains to be elucidated. Second, this study provides a reasonable argument for including intermediate waist girth in the definition of abdominal obesity; on the other hand, metabolic risk factors are consistently higher in those with a high waist girth. Any definition of abdominal obesity thus depends on arbitrary considerations. Third, women in general are less prone to metabolic risk factors than are men. This observation may well contribute to the earlier onset of ASCVD in men compared to women. Although frequencies of elevated HOMA2-IR were similar in men and women, the prevalence of T2DM likewise has been reported to be lower in women than in men.24 Fourth, blacks are less susceptible to elevations of TG and reductions of HDL-C than are other ethnicities at every level of waist girth; but apparently these “benefits” are not sufficient to offset a greater susceptibility for hypertension and hyperglycemia in overall ASCVD risk. Significantly increasing waist girth had a marked effect on the susceptibility of blacks for hypertension. The major susceptibility in Hispanics was in IR, which undoubtedly predisposes to T2DM; otherwise, their metabolic characteristics appeared to resemble those of whites.
Finally, this study raises the question whether clinical criteria for the metabolic syndrome should be based on easily measured metabolic risk factors, with the exception that obesity should be considered a susceptibility factor for the syndrome rather than an integral part of the definition. Because the majority of obese individuals do not have multiple metabolic risk factors, clinical resources might better be directed toward obese persons who are at high metabolic risk. Of course, obese persons without metabolic risk factors must be monitored more closely long term than nonobese persons because they likely are more susceptible to developing these risk factors over time.
Acknowledgments
The authors express appreciation to the Dallas Heart Study investigators and research staff for data management and continued support of data analysis.
Grant support for the Dallas Heart Study was provided by the Donald W. Reynolds Foundation and by US Public Health Service General Clinical Research Center grant M01-RR00633. This work was supported by award number T32HL007360 from the National Heart, Lung, and Blood Institute to Dr. Neeland, by grants UL1DE019584 and PL1DK081182 from the National Institutes of Health, and by a Clinical and Translational Science Award, UL1TR000451 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Author Disclosure Statement
No competing financial interests exist. The authors have no disclosures to make in relation to the content of this manuscript.
References
- 1.Grundy SM, Cleeman JI, Daniels SR, et al. ; American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735–2752 [DOI] [PubMed] [Google Scholar]
- 2.Alberti KG, Eckel RH, Grundy SM, et al. ; International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120:1640–1645 [DOI] [PubMed] [Google Scholar]
- 3.Grundy SM. Metabolic syndrome: A multiplex cardiovascular risk factor. J Clin Endocrinol Metab 2007;92:399–404 [DOI] [PubMed] [Google Scholar]
- 4.Agarwal S, Jacobs DR, Jr, Vaidya D, et al. . metabolic syndrome derived from principal component analysis and incident cardiovascular events: The Multi Ethnic Study of Atherosclerosis (MESA) and Health, Aging, and Body Composition (Health ABC). Cardiol Res Pract 2012;919425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ukegbu UJ, Castillo DC, Knight MG, et al. . Metabolic syndrome does not detect metabolic risk in African men living in the U.S. Diabetes Care 2011;34:2297–2299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jordan HT, Tabaei BP, Nash D, et al. . Metabolic syndrome among adults in New York City, 2004 New York City Health and Nutrition Examination Survey. Prev Chronic Dis 2012;9:E04. [PMC free article] [PubMed] [Google Scholar]
- 7.Victor RG, Haley RW, Willett DL, et al. ; Dallas Heart Study Investigators. The Dallas Heart Study: A population-based probability sample for the multidisciplinary study of ethnic differences in cardiovascular health. Am J Cardiol 2004;93:1473–1480 [DOI] [PubMed] [Google Scholar]
- 8.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care 2004;27:1487–1495 [DOI] [PubMed] [Google Scholar]
- 9.Bonora E, Kiechl S, Willeit J, et al. . Population-based incidence rates and risk factors for type 2 diabetes in white individuals: The Bruneck study. Diabetes 2004;53:1782–1789 [DOI] [PubMed] [Google Scholar]
- 10.Vega GL, Barlow CE, Grundy SM. Prevalence of the metabolic syndrome as influenced by the measure of obesity employed. Am J Cardiol 2010;105:1306–1312 [DOI] [PubMed] [Google Scholar]
- 11.Zhu S, Heymsfield SB, Toyoshima H, et al. . Race-ethnicity-specific waist circumference cutoffs for identifying cardiovascular disease risk factors. Am J Clin Nutr 2005;81:409–415 [DOI] [PubMed] [Google Scholar]
- 12.Eckel RH, Alberti KG, Grundy SM, et al. . The metabolic syndrome. Lancet 2010;375:181–183 [DOI] [PubMed] [Google Scholar]
- 13.Nestel PJ, Whyte HM. Plasma free fatty acid and triglyceride turnover in obesity. Metabolism 1968;17:1122–1128 [DOI] [PubMed] [Google Scholar]
- 14.Flannery C, Dufour S, Rabøl R, et al. . Skeletal muscle insulin resistance promotes increased hepatic de novo lipogenesis, hyperlipidemia, and hepatic steatosis in the elderly. Diabetes 2012;61:2711–1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eisenberg S, Gavish D, Oschry Y, et al. . Abnormalities in very low, low and high density lipoproteins in hypertriglyceridemia. Reversaltoward normal with bezafibrate treatment. J Clin Invest 1984;74:470–482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park SH, Kim JY, Lee JH, et al. . Association between plasma adiponectin and high-density lipoprotein cholesterol in postmenopausal women. Clin Biochem 2010;43:1069–1073 [DOI] [PubMed] [Google Scholar]
- 17.Haffner SM, D'Agostino R, Jr, Saad MF, et al. . Increased insulin resistance and insulin secretion in nondiabetic African-Americans and Hispanics compared with non-Hispanic whites. The Insulin Resistance Atherosclerosis Study. Diabetes 1996;45:742–748 [DOI] [PubMed] [Google Scholar]
- 18.Osei K, Schuster DP. Ethnic differences in secretion, sensitivity, and hepatic extraction of insulin in black and white Americans. Diabet Med 1994;11:755–762 [DOI] [PubMed] [Google Scholar]
- 19.Harris MI. Epidemiological correlates of NIDDM in Hispanics, whites, and blacks in the U.S. population. Diabetes Care 1991;14:639–648 [DOI] [PubMed] [Google Scholar]
- 20.Harris MI, Flegal KM, Cowie CC, et al. . Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in US adults. Diabetes Care 1998;21:518–524 [DOI] [PubMed] [Google Scholar]
- 21.Hall JE, Louis K. Dahl Memorial Lecture. Renal and cardiovascular mechanisms of hypertension in obesity. Hypertension 1994;23:381–394 [DOI] [PubMed] [Google Scholar]
- 22.Dorresteijn JA, Visseren FL, Spiering W. Mechanisms linking obesity to hypertension. Obes Rev 2012;13:17–26 [DOI] [PubMed] [Google Scholar]
- 23.Rosenzweig JL, Ferrannini E, Grundy SM, et al. ; Endocrine Society. Primary prevention of cardiovascular disease and type 2 diabetes in patients at metabolic risk: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2008;93:3671–3689 [DOI] [PubMed] [Google Scholar]
- 24.Goodarz Danaeil G, Friedman AB, Shefali O, et al. . Diabetes prevalence and diagnosis in US states: Analysis of health survey. Population Health Metrics 2009;7:16. [DOI] [PMC free article] [PubMed] [Google Scholar]