Abstract
Advanced ovarian pregnancy is a quite rare condition. Due to the high maternal and neonatal mortality rates, early and accurate diagnosis is vital. Lack of sufficient data led us to search the literature and compile available data on the topic. A 33-year-old woman presented with acute abdomen at 34 weeks of gestation. She underwent laparotomy, which revealed a live foetus surrounded by an intact amnion membrane located in the left adnexal area. The patient delivered a live female infant. Heavy bleeding from the placenta necessitated salpingo oophorectomy. Histological examination of the removed tissue confirmed the ovarian pregnancy. Because of the substantial risk of adverse outcomes, this condition should be borne in mind, especially in cases presenting with acute abdomen during pregnancy.
Keywords: Abdominal pregnancy, ectopic pregnancy, ovarian pregnancy
Özet
İkinci ve üçüncü trimester over gebeliği oldukça nadir bir durumdur. Yüksek maternal ve neonatal mortalite oranları nedeniyle erken ve doğru tanı konulması hayat kurtarıcıdır. Karşılaştığımız ender rastlanan olgu ve konu ile ilgili yeterli bilginin bulunmayışı bizi ikinci ve üçüncü trimester over gebeliği hakkındaki literatürü irdelemeye yöneltti. Otuz üç yaşında kadın hasta, gebeliğin otuz dördüncü haftasında akut abdomen bulgularıyla kliniğimize başvurdu. Laparatomide sol adneksial alanda intakt amniotik membran ile çevrili, içinde canlı fetusun bulunduğu ekstrauterin gebelik tespit edildi. Canlı bir kız bebek doğurtuldu. Plasental alandaki şiddetli kanama nedeniyle salpingo ooferektomi yapıldı. Histopatolojik sonuç over gebeliğiyle uyumlu bulundu. Özellikle ilk trimesterden sonra akut batın bulgularıyla başvuran hastalarda, ayırıcı tanıda over gebeliği akılda tutulmalıdır.
Introduction
Ovarian pregnancy is a specific type of non-tubal ectopic pregnancy, presenting with the same symptomatology. The condition is inherently problematic and challenging. First, it is very rare, which makes it hard to be taken into account during differential diagnosis. Second, reaching an accurate diagnosis is not easy and requires a series of exhaustive procedures ending with surgery in the majority of cases. In situations where routine antenatal follow-up cannot be done during the first and second trimester, the diagnosis of ovarian pregnancy is usually missed. Consequently, presumably a rather high, but unfortunately unknown percent of cases remain undiagnosed. These cases are classified under various other terms such as abdominal, rudimanter horn, cornual pregnancy etc. Third, maternal mortality and perinatal mortality rates are considered to be rather high, although there have only been a few figures published specific to the condition due to the facts described above. As a consequence, the overall reflection of all these to our current literature is the scarcity of data on the subject.
Hence, early and accurate diagnosis is vital to prevent serious outcomes and to overcome severe complications. Here, we report a case with a live 34-week ovarian pregnancy occurring after spontaneous conception and presenting as an acute emergency. Based on our case, we carried out a literature search and evaluated the risk factors, incidence, symptoms, sonographic findings and management strategy of ovarian pregnancy.
Case Report
A 33-year-old woman gravida 3, para 1 presented to the emergency department with severe abdominal pain, nausea and vomiting. The pregnant patient was of low socio-economic status and had not visited any obstetrician for prenatal care. Her past medical history included one ectopic pregnancy and one caesarean section with a healthy birth. There was no history of pelvic inflammatory disease, ovulatory induction or intra uterine device (IUD) use.
On physical examination, the abdomen revealed generalised tenderness to palpation in both lower quadrants with guarding and rebound. The foetus was found to be lying in oblique position. Pelvic examination showed a retroverted cervix without dilatation. Her blood pressure was 96/55 mmHg, with a heart rate of 100 bpm. Her complete blood cell count showed a low haemoglobin level of 9.3 g/dL, a slightly elevated white blood cell count of 13.8×103/μL, and a normal platelet count.
The patient was immediately taken for ultrasonographic examination and a 34-week old pregnancy in the abdominal cavity was noted away from the uterus. The patient underwent a laparotomy, which revealed a live foetus surrounded by an intact amnion membrane located in the left adnexal area next to the uterus. The uterus was larger than the normal size, the right ovary and tuba were normal in appearance and there was about 500 mL of haemoperitoneum in the abdominal cavity.
The patient delivered a girl weighing 1920 gr. The newborn’s Apgar scores were 4 and 6 at one and five minutes, respectively. She was in the 25–50th percentile, and was intubated immediately after delivery. The baby developed respiratory distress despite the administration of endotracheal surfactant and was followed in intensive care.
The placenta was adherent to the left ovary, uterus, left abdominal sidewall and omentum. The left tuba was elongated, the left ovary was large and oedematous and bleeding was seen in some areas. There was significant bleeding from detached portions of the placenta and the attached ovary, and we had to remove the placenta via salpingo oophorectomy in order to provide haemostasis. The patient was transfused with two units of blood during the operation and she was taken to the recovery room in a stable condition. The postoperative period was uneventful; she was discharged on the 5th postoperative day. The newborn died on the 4th day in the intensive care unit because of respiratory insufficiency and no other congenital malformation was found on autopsy except for pulmonary hypoplasia. Histological examination of the removed tissue confirmed the ovarian pregnancy.
Discussion
The present case is a rare example of an advanced ovarian pregnancy occurring after spontaneous conception.
Although the focus of this review is ovarian pregnancy, some of the figures given below are related to other types of abdominal pregnancies. Due to the scarcity of data specific to ovarian pregnancy, and because all different types present with same symptoms and require the same treatment approach, we believe that these figures could be of help in reaching an overall impression on ovarian pregnancy also.
Ectopic pregnancy represents about 1–2% of all pregnancies with 95% occurring in the fallopian tube. Abdominal pregnancies represent just 1% of ectopic pregnancies; ovarian pregnancy accounts for 0.5–3% of all ectopic pregnancies. The overall incidence ranges from 1 in 2100 to 1 in 7000 pregnancies (1–3). To the best of our knowledge, only 11 cases of advanced ovarian pregnancy have been previously reported based on a literature search carried out on PUBMED for the period from 1948 to 2013 (4–14).
The pathogenic mechanism is thought to be fertilisation occurring outside the tube, followed by implantation within the ovary or the failure of follicular extrusion (15, 16). Due to the extreme rarity of ovarian pregnancy, the risk factors are not as well established as in tubal pregnancy. Possible risk factors in the literature include previous ectopic pregnancy, pelvic inflammatory disease, IUD use, endometriosis, previous abdominal surgery, uterine anomalies and assisted reproductive techniques (ART) (15–19).
In a series of 49 cases where ovarian pregnancy was confirmed, the most common risk factors were found to be previous abdominal surgery for 19 cases and endometriosis for 16 cases. Four patients had a history of pelvic inflammatory disease, and only 2 patients had used an IUD. Huge uterine myoma was found in 2 cases, bicornuate uterus was found in 1 case, and arcuate uterus was found in 1 case (20). Our patient had ectopic pregnancy and caesarean section as risk factors. According to the above-mentioned study the most common complaints are abdominal pain (42.9%) and vaginal bleeding (28.6%) (20). The pain is generally nonspecific during early gestation and becomes worse as the pregnancy advances, sometimes culminating in cases of acute abdomen due to rupture of the gestational sac and placental disruption, resulting in haemoperitoneum. In the same study, interestingly, five asymptomatic patients were incidentally discovered to have an ovarian pregnancy during post-in vitro fertilisation (IVF) monitoring. The relation with ART was later supported by Ngu et al. (21), who reported that 28.5% of ovarian pregnancies were associated with IVF, indicating the high risk of ovarian pregnancy among women who undergo ART.
The diagnosis of advanced ovarian pregnancy is very challenging. History and physical examination are inconclusive. It is easier to reach a diagnosis during the first trimester using high resolution transvaginal ultrasound, making quantitative measurements of b-human chorionic gonadotropin (HCG) levels and performing laparoscopy; hence, an early diagnosis of an ovarian pregnancy is proposed to be more feasible, as Dr. Huang also concluded in his case report (4). However, as the pregnancy grows, without any suspicion and meticulous examination, a diagnosis of advanced ovarian pregnancy probably can be missed easily. Some authors even argue that ovarian pregnancy is unlikely to be diagnosed preoperatively due to its rarity, a lack of typical presenting symptoms, and a lack of known risk factors (20).
Ultrasonography is the most often used non-invasive diagnostic imaging method in pregnancy. Echographic evidence of a non-gravid uterus alongside a foetus is diagnostic in extrauterine pregnancy. Actually, a preoperative diagnosis of advanced abdominal pregnancy is usually missed, with only 45% of cases being diagnosed preoperatively (22). Observing the entire uterine wall encapsulating the pregnancy and placenta confirms the intrauterine pregnancy. If ultrasonography shows no uterine wall surrounding the foetus, and if foetal parts are very close to the abdominal wall, then the suspected diagnosis would be extrauterine pregnancy. The possibility of extrauterine pregnancy should be strongly suspected, especially in cases of bleeding or non-labour abdominal pain during the third trimester. In addition to these, painful foetal movements, abnormal foetal lie, foetal demise, abdominal mass palpated apart from the foetus, an unusual echographic appearance of placenta, oligohydramnios, the presence of maternal intraperitoneal fluid, and induction failure are all suggestive of abdominal pregnancy; however, neither is accepted to be pathognomonic for ovarian pregnancy (22, 23). Laparotomy findings being at hand, the diagnosis of ovarian pregnancy needs to be confirmed through histopathological work up. Histopathological diagnosis is based upon the worldwide accepted criteria proposed by Spiegelberg, which are as follows: fallopian tubes including fimbria must be intact and separate from the ovary; the pregnancy must occupy the normal position of the ovary; the ovary must be attached to the uterus through the utero-ovarian ligament and there must be ovarian tissue attached to the pregnancy in the specimen. In our case, the final histopathological diagnosis was based on the Spiegelberg criteria (Figure 1).
Figure 1.
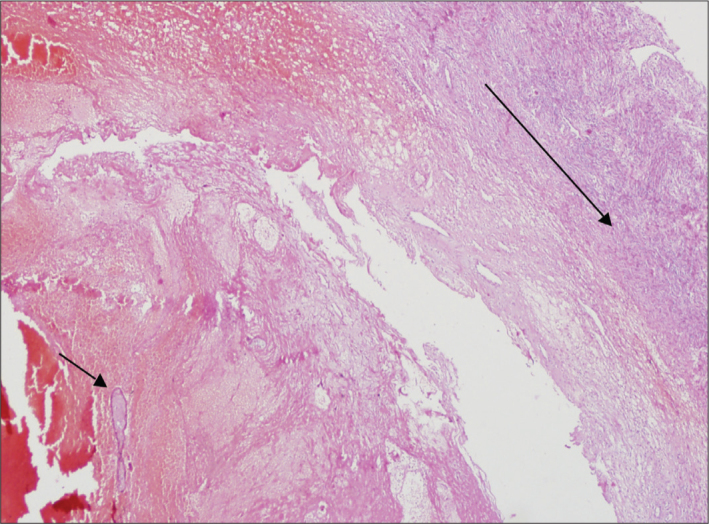
Haemorrhage and chorion villus (small arrow) within ovarian stroma (large arrow) (H&Ex20)
Once the diagnosis is made, the subsequent steps also continue to be challenging with advanced ovarian/abdominal pregnancy. No absolute consensus exists with regard to the management of abdominal pregnancies. In view of the high maternal mortality and foetal mortality and morbidity, progressive oligohydramnios, a high incidence of malformations, and foetal growth restriction due to placental insufficiency, the majority of investigators agree that abdominal pregnancy should be terminated as soon as it is diagnosed and that the procedure should include complete removal of the foetus and placenta. On the other hand, there are numerous reports of advanced extrauterine pregnancies ending with a viable foetus and a healthy mother. Since the diagnosis is frequently missed preoperatively and adverse foetal and maternal outcomes do not necessarily occur in association with the continuation of pregnancy, one could argue that the termination of an advanced extrauterine pregnancy upon antenatal diagnosis might not be warranted. However, these cases should be followed-up very carefully in order to prevent adverse outcomes (24).
In fact, advanced ovarian pregnancy is diagnosed upon laparotomy in the majority of the cases. The most life-threatening complication of operation is bleeding from the implantation site of the placenta. The most controversial issue in advanced ovarian/abdominal pregnancy during laparotomy is whether or not to remove the placenta. Blood supply to the abnormally implanted placenta is diffuse and the origin is often unidentifiable; consequently, attempts to remove the placenta can provoke bleeding. A placenta left in situ might be resorbed spontaneously, but if it does not, the risk of infection, necrosis, and the need for a second surgery is considerable. Most authors agree that the placenta should be removed provided its blood supply is identified and can be ligated without damaging other organs (22). In cases where placental implantation has occurred in vascular areas such as the mesentery and vital organs, it has been recommended that the placenta should be left in situ, as surgical excision can result in uncontrollable and life-threatening haemorrhage. If the blood supply cannot be identified, the placenta should be left in place and the patient should be followed-up for paralytic ileus, peritonitis, sepsis, or the formation of abscesses and pre-eclampsia (25). Methotrexate treatment has been proven to be of little value in cases of advanced abdominal pregnancies. When destruction occurs too quickly upon methotrexate treatment, the risk of sepsis and death ensues due to the formation of large amounts of necrotic tissue. This might be avoided by using methotrexate judiciously with the administration of lower doses with less frequent intervals; thereby allowing the slow resorption of the placenta left in the abdominal cavity (26). In the present case, emergency laparotomy was performed because of acute abdomen. The foetus was delivered, and the placenta had to be removed via salpingo-oophorectomy due to heavy bleeding.
For the newborn, it is important to rule out congenital malformations. Foetal malformations associated with advanced abdominal pregnancy are as high as 40% and only 50% of these babies survive up to one week post-delivery (23, 27). Pulmonary hypoplasia, pressure deformities, and foetal growth restriction due to placental insufficiency are the most eminent causes leading to neonatal complications. Typical deformities include limb defects, facial and cranial asymmetry, joint abnormalities and central nervous malformation (28). These pregnancies usually do not extend to 37 weeks and usually end up with foetal loss (29). In our case, the newborn died of severe respiratory insufficiency, and pulmonary hypoplasia was found on autopsy.
Our case presented as acute abdomen. All of the subsequent procedures were performed under emergency conditions and we were not able to take any ultrasound or intraoperative pictures. This is a weak point of our study.
The diagnosis of advanced ovarian pregnancy is difficult, and treatment is based on surgical approaches. This review describes a very rare case of advanced ovarian pregnancy in a patient with intra-abdominal haemorrhage and acute abdomen resulting in a live birth, together with a literature review of the topic. In patients with advanced gestational age and abnormal foetus lie, it is important to bear in mind that this may be an abdominal/ovarian pregnancy and the surgeon should be prepared to face various complications during the surgery, such as massive haemorrhage, disseminated intravascular coagulation, pulmonary oedema, bowel perforation, and sepsis. Considerable adverse outcomes are also relevant for the newborn baby. Therefore, the aim of this review was for clinicians to consider abdominal ovarian pregnancy as a differential diagnosis and prepare to manage the patient with a multidisciplinary surgical team, along with the assurance of sufficient blood, and the presence of a newborn intensive care unit; these factors would reduce the high maternal and neonatal mortality rate.
Acknowledgements
We are grateful to the patient for giving consent for her medical records to be published.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Acıbadem University.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author contributions: Concept – Y.G., E.M., E.Z.; Design – E.M., S.K.E., P.K.; Supervision – E.M., S.K.E., P.K.; Resource – E.Z., Ş.Ö., S.K.E.; Materials – E.Z., Ş.Ö., S.K.E.; Data Collection&/or Processing – E.M., E.Z., S.K.E.; Analysis&/or Interpretation – Y.G., Ş.Ö., P.K.; Literature Search – E.M., E.Z., S.K.E.; Writing – E.M., Ş.Ö., P.K.; Critical Reviews - Y.G., E.M., S.K.E.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: No financial disclosure was declared by the authors.
References
- 1.Nwobodo EI. Abdominal pregnancy. A case report. Ann Afr Med. 2004;3:195–6. doi: 10.4103/1596-3519.55653. [DOI] [PubMed] [Google Scholar]
- 2.Bouyer J, Coste J, Fernandez H, Pouly JL, Job-Spira N. Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Hum Reprod. 2002;17:3224–30. doi: 10.1093/humrep/17.12.3224. [DOI] [PubMed] [Google Scholar]
- 3.Hage PS, Arnouk IF, Zarou DM, Kim BH, Wehbeh HA. Laparoscopic management of ovarian ectopic pregnancy. J Am Assoc Gynecol Laparosc. 1994;1:283–5. doi: 10.1016/s1074-3804(05)81025-4. [DOI] [PubMed] [Google Scholar]
- 4.Huang J, Jing X, Fan S, Fufan Z, Yiling D, Pixiang P, et al. Primary unruptured full term ovarian pregnancy with live female infant: case report. Arch Gynecol Obstet. 2011;283( Suppl 1):31–3. doi: 10.1007/s00404-010-1755-z. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal S, Gahlot D. An advanced primary ovarian pregnancy. J Obstet Gynaecol. 2000;20:542. doi: 10.1080/014436100434866. [DOI] [PubMed] [Google Scholar]
- 6.Kosovski I, Schopova P, Skotschev S. A case of full term ovarian pregnancy. Zentralbl Gynakol. 1992;114:316–7. [PubMed] [Google Scholar]
- 7.Ogunniyi SO, Faleyimu BL, Odesanmi WO, Fasubaa OB. Ovarian pregnancy causing obstructed labor at term in a heterotopic gestation. Int J Gynaecol Obstet. 1990;31:283–5. doi: 10.1016/0020-7292(90)91024-k. [DOI] [PubMed] [Google Scholar]
- 8.Fernandez H, De Ziegler D, Imbert MC, Cambet B, Frydman R, Papiernik E. Advanced combined intra-uterine and ovarian gestations: case report. Eur J Obstet Gynecol Reprod Biol. 1990;37:293–6. doi: 10.1016/0028-2243(90)90038-3. [DOI] [PubMed] [Google Scholar]
- 9.Schander K, Pediaditakis D, Stille A, Bartz KO. The course and treatment of an ovarian pregnancy in the 3rd trimester. Geburtshilfe Frauenheilkd. 1989;49:198–200. doi: 10.1055/s-2008-1026578. [DOI] [PubMed] [Google Scholar]
- 10.Shindo N, Takeuchi N, Tamamoto F, Sumi Y, Katayama H, Takada M, et al. A case of advanced ovarian pregnancy--usefulness of preoperative angiography. Rinsho Hoshasen. 1988;33:841–4. [PubMed] [Google Scholar]
- 11.Mofid M, Rhee MW, Lankerani M. Ovarian pregnancy with delivery of a live baby. Obstet Gynecol. 1976;47:5S–8S. [PubMed] [Google Scholar]
- 12.Malonzo AA, Boronow RC. Sigmoid-amniotic fistula in advanced ovarian pregnancy: use of preliminary colostomy. South Med J. 1970;63:557–9. doi: 10.1097/00007611-197005000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Aitken G. Advanced ovarian pregnancy. Aust N Z J Obstet Gynaecol. 1964;40:26–31. doi: 10.1111/j.1479-828x.1964.tb00247.x. [DOI] [PubMed] [Google Scholar]
- 14.Walker A. Advanced ovarian pregnancy. Proc R Soc Med. 1948;41:677. [PMC free article] [PubMed] [Google Scholar]
- 15.Bontis J, Grimbizis G, Tarlatzis BC, Miliaras D, Bili H. Intrafollicular ovarian pregnancy after ovulation induction/intrauterine insemination: pathophysiological aspects and diagnostic problems. Hum Reprod. 1997;12:376–8. doi: 10.1093/humrep/12.2.376. [DOI] [PubMed] [Google Scholar]
- 16.Marret H, Hamamah S, Alonso AM, Pierre F. Case report and review of the literature: primary twin ovarian pregnancy. Hum Reprod. 1997;12:1813–5. doi: 10.1093/humrep/12.8.1813. [DOI] [PubMed] [Google Scholar]
- 17.Comstock C, Huston K, Lee W. The ultrasonographic appearance of ovarian ectopic pregnancies. Obstet Gynecol. 2005;105:42–5. doi: 10.1097/01.AOG.0000148271.27446.30. [DOI] [PubMed] [Google Scholar]
- 18.Einenkel J, Baier D, Horn LC, Alexander H. Laparoscopic therapy of an intact primary ovarian pregnancy with ovarian hyperstimulation syndrome: case report. Hum Reprod. 2000;15:2037–40. doi: 10.1093/humrep/15.9.2037. [DOI] [PubMed] [Google Scholar]
- 19.Ghi T, Banfi A, Marconi R, Iaco PD, Pilu G, Aloysio DD, et al. Three-dimensional sonographic diagnosis of ovarian pregnancy. Ultrasound Obstet Gynecol. 2005;26:102–4. doi: 10.1002/uog.1933. [DOI] [PubMed] [Google Scholar]
- 20.Choi HJ, Im KS, Jung HJ, Lim KT, Mok JE, Kwon YS. Clinical analysis of ovarian pregnancy: a report of 49 cases. Eur J Obstet Gynecol Reprod Biol. 2011;158:87–9. doi: 10.1016/j.ejogrb.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 21.Ngu SF, Cheung VY. Non-tubal ectopic pregnancy. Int J Gynaecol Obstet. 2011;115:295–7. doi: 10.1016/j.ijgo.2011.07.032. [DOI] [PubMed] [Google Scholar]
- 22.Nkusu Nunyalulendho D, Einterz EM. Advanced abdominal pregnancy: case report and review of 163 cases reported since 1946. Rural Remote Health. 2008;8:1087. [PubMed] [Google Scholar]
- 23.Kun KY, Wong PY, Ho MW, Tai CM, Ng TK. Abdominal pregnancy presenting as a missed abortion at 16 weeks’ gestation. Hong Kong Med J. 2000;6:425–7. [PubMed] [Google Scholar]
- 24.Dahab AA, Aburass R, Shawkat W, Babgi R, Essa O, Mujallid RH. Full-term extrauterine abdominal pregnancy: a case report. J Med Case Reports. 2011;5:531. doi: 10.1186/1752-1947-5-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stovall TG, Elkins TE. Twin abdominal pregnancy. A case report. J Reprod Med. 1985;30:784–6. [PubMed] [Google Scholar]
- 26.Rahaman J, Berkowitz R, Mitty H, Gaddipati S, Brown B, Nezhat F. Minimally invasive management of an advanced abdominal pregnancy. Obstet Gynecol. 2004;103:1064–8. doi: 10.1097/01.AOG.0000127946.14387.48. [DOI] [PubMed] [Google Scholar]
- 27.Teng H, Kumar G, Ramili N. A viable secondary intra-abdominal pregnancy resulting from rupture of uterine scar: role of MRI. Br J Radiol. 2007;80:e134–6. doi: 10.1259/bjr/67136731. [DOI] [PubMed] [Google Scholar]
- 28.Stevens CA. Malformations and deformations in abdominal pregnancy. Am J Med Genet. 1993;47:1189–95. doi: 10.1002/ajmg.1320470812. [DOI] [PubMed] [Google Scholar]
- 29.Baffoe P, Fofie C, Gandau BN. Term abdominal pregnancy with healthy newborn: a case report. Ghana Med J. 2011;45:81–3. doi: 10.4314/gmj.v45i2.68933. [DOI] [PMC free article] [PubMed] [Google Scholar]


