Abstract
Didelphic uterus with obstructed hemivagina and ipsilateral renal agenesis is a rare condition. It usually presents with pelvic pain following the menarche, dysmenorrhoea, and an increase in abdominal volume or a palpable mass due to unilateral haematocolpos. We present the case of a 13-year-old girl who referred with recurrent pelvic pain, mainly at the time of menses, and irregular menstrual cycle complaints in this report. The patient underwent ultrasonography and magnetic resonance (MR) imaging of the pelvis was performed. The diagnosis was uterus didelphys with obstructed hemivagina and ipsilateral renal agenesia. Laparotomy was performed for diagnosis and treatment purposes. Two separated hemiuteri and two cervices with hematometra and hematocolpos on the right side and ipsilateral renal agenesis were detected. The vaginal septum was excised completely and Strassman metroplasty was performed. Her complaints were resolved and she was absolutely asymptomatic after surgery. Diagnosis and management of this congenital anomaly is challenging due to the complexity of the anatomic structures, nonspecific complaints, and heterogenic presentation. These anomalies must always be considered while working-up female patients presenting with episodic abdominal pain and abdominopelvic mass.
Keywords: Uterus didelphys, vaginoplasty, metroplasty, Müllerian anomalies, renal agenesis
Özet
Tek taraflı kapalı vajen ve aynı tarafta böbrek agenezisi ile birlikte didelfik uterus nadir görülen bir durumdur. Genellikle menarj sonrasında görülen pelvik ağrı, dismenore, karın hacminde artış veya tek taraflı hematokolposa bağlı olarak ele gelen kitle şeklinde ortaya çıkar. Bu yazıda özellikle adet sırasında ortaya çıkan pelvik ağrı ve düzensiz adet kanaması şikayetleri ile başvuran 13 yaşındaki bir kız çocuğunun olgusunu sunduk. Hastaya pelvik ultrasonografi ve manyetik rezonans (MR) incelemesi yapıldı. Tek taraflı kapalı vajen ve aynı tarafta böbrek agenezisi ile birlikte didelfik uterus tanısı konuldu. Tanı ve tedavi amaçlı laparotomi yapıldı. İki ayrı hemiuterus, iki serviks ve sağ tarafta hematometra ve hematokolpos ile aynı tarafta böbrek agenezi tesbit edildi. Vaginal septum tamamen çıkartıldı ve Strassmann metroplastisi yapıldı. Ameliyat sonrasında hastanın bütün şikayetleri geçti ve bulguları tamamen kayboldu. Anatomik yapılardaki farklılığa, şikayetlerin özgün olmamasına ve değişik şekillerde ortaya çıkmasına bağlı olarak bu konjenital anomalinin tanısı ve tedavisi güçtür. Dönemsel karın ağrısı ve abdominopelvik kitle ile başvuran bir kadında mutlaka bu bozuklukların da olabileceği düşünülmelidir.
Introduction
Müllerian duct anomalies consist of a set of structural malformations resulting from abnormal development of the paramesonephric or Müllerian ducts. The prevalence of these anomalies ranges from 0.001 to 10% in the general population and from 8–10% in women with an adverse reproductive history (1, 2).
A wide variety of malformations can occur when this system is disrupted. They range from uterine and vaginal agenesis to duplication of the uterus and vagina to minor uterine cavity abnormalities.
Uterine malformations result from a failure in organogenesis or from fusion or reabsorption of the Müllerian ducts. Approximately 11% of uterine malformations are didelphys uterus (3). Didelphic uterus is associated with unilateral anomalies, i.e., obstructed hemivagina and ipsilateral renal agenesis in 15%–30% of cases, establishing a well-known symptomatic complex (hematocolpos, piocolpos, hematometra, hematosalpinx) that needs an in-depth diagnostic approach as well as surgical treatment with definite anatomic confirmation of the defect type and side (4). This manifestation has been referred to in the literature as the Herlyn-Werner-Wunderlich syndrome (HWWS) as well as the obstructed hemivagina and ipsilateral renal anomaly syndrome (OHVIRA) (5, 6). It is a rare condition and occurs as result of an embryologic arrest simultaneously affecting the Müllerian and metanephric ducts at about 8 weeks gestation.
Clinical presentations are variable, depending on the degree of obstruction and the existence of an opening. The most common presenting symptoms are the onset of dysmenorrhoea within the first years after menarche and progressive pelvic pain. Marked rectal pain and constipation secondary to haematocolpos impingement have also been reported as presenting symptoms (7).
In this report, we present a case of a 13-year-old girl who was referred with recurrent pelvic pain, mainly at the time of menses, and irregular menstrual cycles and was diagnosed with uterus didelphys associated with unilateral vagina obstructed by a transverse septum with ipsilateral renal agenesis.
Case Report
A 13-year-old girl presented with recurrent pelvic pain, mainly at the time of menses, and irregular menstrual cycles. The patient’s menarche occurred at the age of 11 years. She complained of severe abdominal pain that occurred during each of her menses. An ultrasound examination revealed the existence of two distinct hemiuteruses. The left one was of normal length and the cavity was empty; the right one formed an angle of about 90 degrees with the contralateral and contained fluid in its cavity (haematometra). A cystic mass along the right lateral wall in the upper part of the vagina also was found (haematocolpos). Ultrasound examination of the abdomen confirmed the presence of a single left kidney. Magnetic resonance (MR) imaging of the pelvis was recommended and performed to enable further evaluation. Subsequent computed tomographic examination verified the gynaecologic findings of ultrasound examination and also revealed the accompanying anomalies of ipsilateral renal agenesis (Figure 1).
Figure 1.
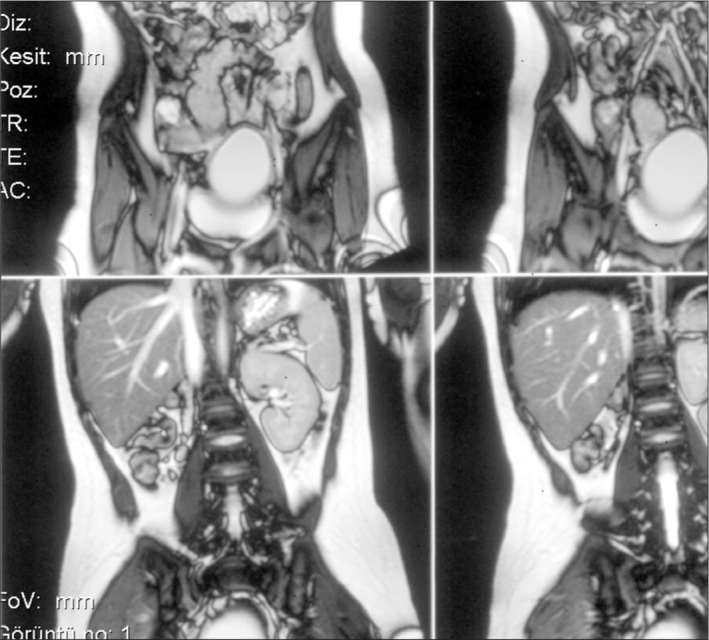
MR image
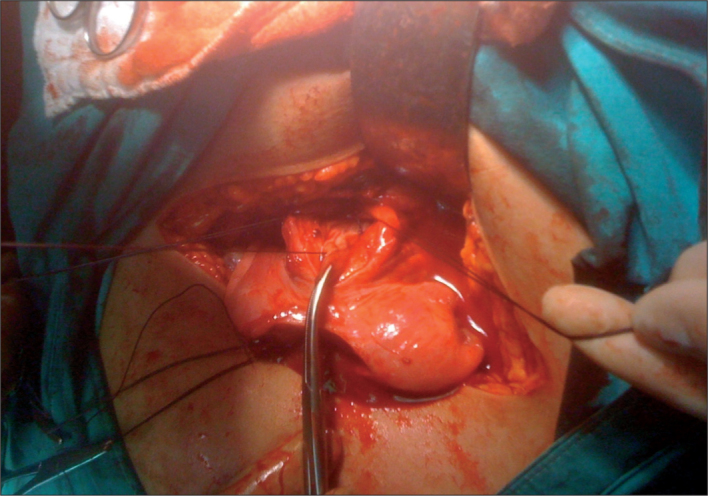
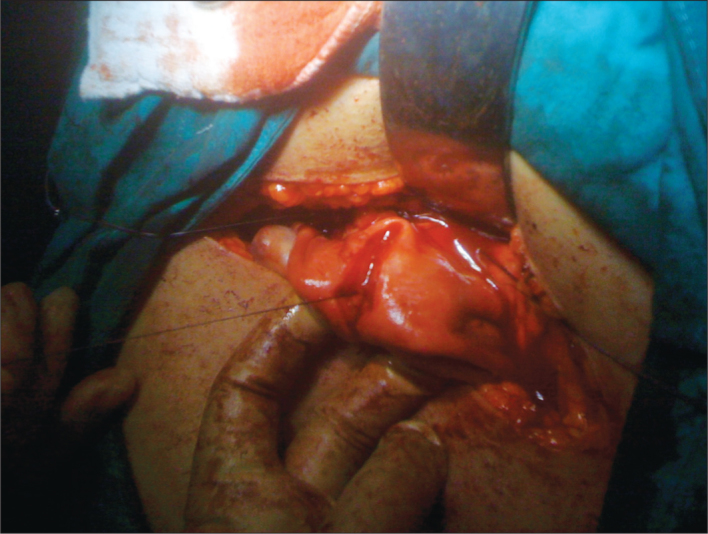
A diagnostic laparotomy was performed to evaluate the mass and its peripheral extensions with regard to the pelvic anatomy in detail. Laparotomic observation confirmed the diagnosis. We detected two separated hemiuteri and two cervices with haematometra and haematocolpos on the right side and ipsilateral renal genesis (Figure 2). After an incision on the vaginal septum, a large amount of chocolate-coloured fluid was drained, and the dimensions of the right uterus were diminished after the procedure (Figure 3). Then, the vaginal septum was excised completely and the edges of the septum were marsupialised (Figure 4). As two hemiuteri were hypoplastic, we decided to perform metroplasty by Strassman’s method (Figure 5). We made a wedge-shaped incision, deep enough to enter the endometrial cavity on the medial aspect of each uterine horn. The incision extended from the superior aspect of each horn, near the interstitial region of the fallopian tubes, to the inferior aspect of the uterus. Apposition of the opposing myometrium was achieved using interrupted vertical figure-8 sutures along the posterior and anterior uterine walls. The final layer was closed using continuous subserosal sutures, without exposing any suture material to the peritoneal cavity.
Figure 2.
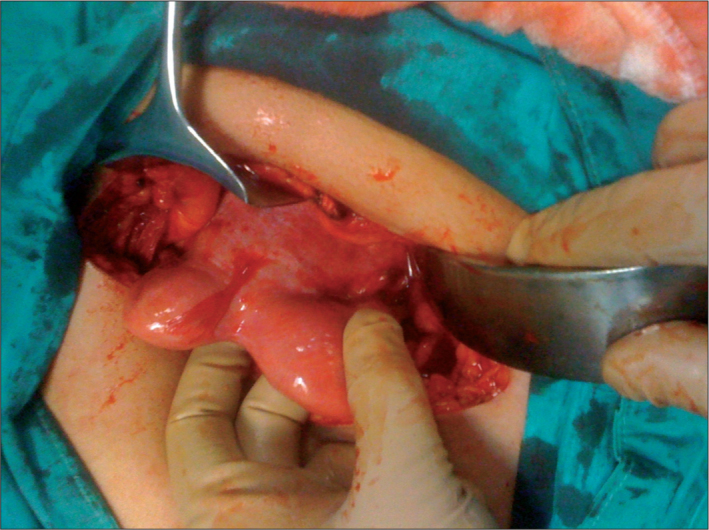
Two distinct hemiuteruses
Figure 3.
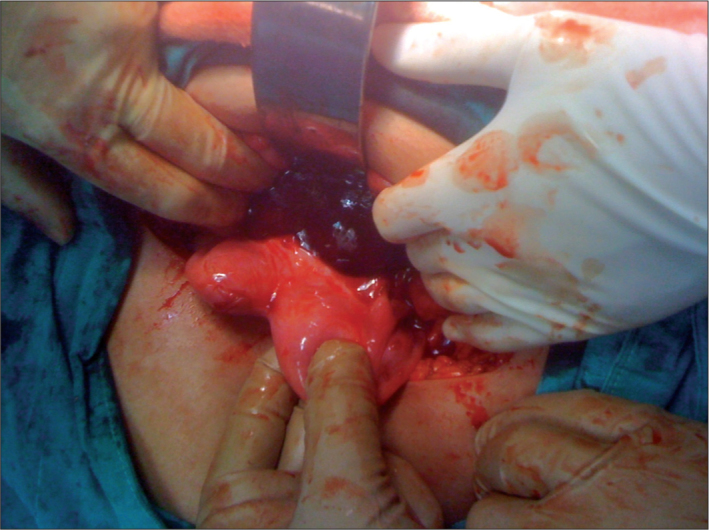
After an incision on the vaginal septum, a large amount of chocolate-colored fluid was drained
Figure 4.
The vaginal septum was excised completely and the edges of the septum were marsupialized
Figure 5.
Metroplasty by Strassman’s method
The patient was comfortable in the postoperative period. She was followed-up regularly, and she was completely asymptomatic after surgery.
Discussion
Congenital Müllerian defects are a fascinating clinical problem, the true incidence of which is hard to determine as most data are derived from studies of patients presenting with reproductive problems, and an accurate diagnosis and complete assessment of the uterine morphology has not always been performed. In many patients, uterine congenital anomalies have been related to infertility, recurrent pregnancy loss, prematurity and other obstetric complications. Although uterine malformations are common, complex malformations are rare. Complex malformations of the female genital tract are often incorrectly identified, treated and reported.
Failure of fusion of the Müllerian ducts can result in a uterine didelphys in some cases, and failure of canalisation or resorption in the uterovaginal canal or urogenital sinus can lead to a vaginal septum (8). OHVIRA is a variant of the broad spectrum of Müllerian anomalies that is being more frequently diagnosed and reported with increasing awareness and advances in radiological imaging.
Diagnosis of this syndrome is a challenge as the complaints are nonspecific and presentations are heterogenic. Patients with this syndrome are frequently asymptomatic, and are often missed in routine gynaecological examinations. A history of pelvic pain following the menarche, dysmenorrhoea and an increase in abdominal volume are complaints that are suggestive of uterine anomalies. Primary amenorrhoea and changes to menstrual flows may also be present (9). Usually, on examination, a unilateral pelvic mass is detected, with the right side affected nearly twice as frequently as the left side (10). Our case showed the right-sided involvement as well.
Ultrasonography, conventional and sonohysterosalpingography, magnetic resonance imaging and three-dimensional computed tomography angiography are useful tools for diagnosing complex Müllerian anomalies. However, haematocolpos frequently distorts the anatomy, leading to radiologic imaging of variable utility. Laparoscopy and laparotomy may be appropriate to aid in the definition of anatomy, and to treat the anomalies and concomitant conditions such as adhesions or endometriosis (11, 12).
Management of this complex congenital anomaly of the female reproductive tract requires careful anatomic consideration. Surgical reconstruction of the internal genitalia with restoration of menses and maintenance of a patent genital tract is challenging. Full excision and marsupialisation of the vaginal septum are the preferred surgical approaches for the treatment of uterine didelphys with obstructed unilateral vagina (13). This can be challenging as haematocolpos causes distortion of the adjacent anatomic structures and there is chronic inflammation. Also, the vagina of many adolescent girls is narrow. Definition of the anatomic structures in detail is a crucial step as sepsis and death have been reported in cervical agenesis cases where vaginoplasty was performed (14, 15).
In this case, we excised and marsupialised the vaginal septum to relieve the obstruction. Also, we performed Strassman metroplasty to preserve future fertility and to prevent obstetric complications such as preterm delivery and recurrent abortus as the size of the two hemiuteri were hypoplastic. Resection of the septum to the level of the cervix that is in close proximity to the uterine vascular supply is a technical challenge while operating on these patients as anatomic variation can lead to ectopic vasculature, especially in the case of asymmetric bicollis. Therefore, careful examination and imaging needs to be performed before surgery to avoid possible haemorrhage in a constricted difficult-to-visualise surgical fields.
In conclusion, a high index of suspicion is necessary to diagnose these disorders, and adequate work-up, careful exam and imaging, as well as careful surgical planning is essential in the management of these anomalies.
Footnotes
Ethics Committee Approval: N/A
Informed Consent: Informed consent was received from the participant of this case.
Peer-review: Externally peer-reviewed.
Author contributions: All authors contributed equally during the preparation of this manuscript.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Pui MH. Imaging diagnosis of congenital uterine malformation. Comput Med Imaging Graph. 2004;28:425–33. doi: 10.1016/j.compmedimag.2004.05.008. http://dx.doi.org/10.1016/j.compmedimag.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 2.Propst AM, Hill JA., 3rd Anatomic factors associated with recurrent pregnancy loss. Semin Reprod Med. 2000;18:341–50. doi: 10.1055/s-2000-13723. http://dx.doi.org/10.1055/s-2000-13723. [DOI] [PubMed] [Google Scholar]
- 3.Nahum GG. Uterine anomalies. How common are they, and what is their distribution among subtypes? J Reprod Med. 1998;43:877–87. [PubMed] [Google Scholar]
- 4.Heinonen PK. Clinical implications of the didelphic uterus: long term follow-up of 49 cases. Eur J Obstet Reprod Biol. 2000;91:183–90. doi: 10.1016/s0301-2115(99)00259-6. http://dx.doi.org/10.1016/S0301-2115(99)00259-6. [DOI] [PubMed] [Google Scholar]
- 5.Smith NA, Laufer MR. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertil Steril. 2007;87:918–22. doi: 10.1016/j.fertnstert.2006.11.015. http://dx.doi.org/10.1016/j.fertnstert.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Gholoum S, Puligandla P, Hui T, Su W, Quiros E, Laberge J. Management and outcome of patients with combined vaginal septum, bifid uterus, and ipsilateral renal agenesis (Herlyn-Werner-Wunderlich syndrome) J Pediatr Surg. 2006;41:987–92. doi: 10.1016/j.jpedsurg.2006.01.021. http://dx.doi.org/10.1016/j.jpedsurg.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 7.Pieroni C, Rosenfeld DL, Mokrzycki ML. Uterus didelphys with obstructed hemivagina and ipsilateral renal agenesis. A case report. J Reprod Med. 2001;46:133–6. [PubMed] [Google Scholar]
- 8.Laufer MR, Goldstein DP, Hendren WH. Structural abnormalities of the female reproductive tract. In: Emans SJ, Laufer MR, Goldstein DP, editors. Pediatric and Adolescent Gynecology. 2d ed. Vol. 334. Philadelphia: Lippincott Williams & Wilkins; p. 2005.p. 416. [Google Scholar]
- 9.Fedele L, Bianchi S, Frontino G. Septums and synechiae: approaches to surgical correction. Clin Obstet Gynecol. 2006;49:767–88. doi: 10.1097/01.grf.0000211948.36465.a6. http://dx.doi.org/10.1097/01.grf.0000211948.36465.a6. [DOI] [PubMed] [Google Scholar]
- 10.Vercellini P, Daguati R, Somigliana E, Viganò P, Lanzani A, Fedele L. Asymmetric lateral distribution of obstructed hemivagina and renal agenesis in women with uterus didelphys: institutional case series and a systematic literature review. Fertil Steril. 2007;87:719–24. doi: 10.1016/j.fertnstert.2007.01.173. http://dx.doi.org/10.1016/j.fertnstert.2007.01.173. [DOI] [PubMed] [Google Scholar]
- 11.Burgis J. Obstructive Müllerian anomalies: case report, diagnosis, and management. Am J Obstet Gynecol. 2001;185:338–44. doi: 10.1067/mob.2001.116738. http://dx.doi.org/10.1067/mob.2001.116738. [DOI] [PubMed] [Google Scholar]
- 12.Takeuchi H, Sato Y, Shimanuki H, Kikuchi I, Kumakiri J, Kitade M, et al. Accurate preoperative diagnosis and laparoscopic removal of the cavitated non-communicated uterine horn for obstructive müllerian anomalies. J Obstet Gynaecol Res. 2006;32:74–9. doi: 10.1111/j.1447-0756.2006.00354.x. http://dx.doi.org/10.1111/j.1447-0756.2006.00354.x. [DOI] [PubMed] [Google Scholar]
- 13.Stassart JP, Nagel TC, Prem KA, Phipps WR. Uterus didelphys, obstructed hemivagina, and ipsilateral renal agenesis: the University of Minnesota experience. Fertil Steril. 1992;57:756–61. doi: 10.1016/s0015-0282(16)54955-3. [DOI] [PubMed] [Google Scholar]
- 14.Casey CC, Laufer MR. Cervical agenesis: septic death after surgery. Obstet Gynecol. 1997;90:706–7. doi: 10.1016/s0029-7844(97)00391-8. http://dx.doi.org/10.1016/S0029-7844(97)00391-8. [DOI] [PubMed] [Google Scholar]
- 15.Fujimoto MD, Miller JH, Klein NA, Soules MR. Congenital cervical atresia: report of seven cases and review of the literature. Am J Obstet Gynecol. 1997;177:1419–25. doi: 10.1016/s0002-9378(97)70085-1. http://dx.doi.org/10.1016/S0002-9378(97)70085-1. [DOI] [PubMed] [Google Scholar]


