Abstract
Objective
The purpose of this study was to determine if placental location is associated with adverse pregnancy outcome and to assess whether any association exists between different blood groups and location of the placenta.
Material and Methods
Medical records of women were reviewed retrospectively and placental position as documented in the case notes at routine antenatal (20–38 weeks) ultrasonography was identified. Placental position was categorised as anterior, posterior and fundal. Association of placental location with foeto-maternal outcome and different blood groups was noted.
Results
A total 474 case notes of women were analysed for placental location, feto-maternal outcome and blood groups. Anterior placenta was found to have a relation with a greater risk of pregnancy-induced hypertension, gestational diabetes mellitus and placental abruption (p<0.001), while posterior placenta had a significant association with preterm labour (p<0.001). Regarding foetal outcome, an anterior placenta was significantly associated with intrauterine growth retardation and intrauterine foetal death (p<0.001). The majority (54%) of women with an anterior placenta were O-positive blood group, while 46% of women in the posterior placenta group were A-positive blood group (p<0.001).
Conclusion
Anterior placental implantation is associated with an increased risk of pregnancy-induced hypertension, gestational diabetes mellitus, placental abruption, intrauterine growth retardation and intrauterine foetal death. Posterior placenta has a significant association with preterm labour and A-positive blood group. Anterior placenta is common in women with O-positive blood group. Placental location may be an important determinant of pregnancy outcome.
Keywords: Placental location, pregnancy outcome, neonatal outcome, antenatal complications
Özet
Amaç
Bu çalışmanın amacı, plasenta konumunun olumsuz gebelik sonuçları ile ilişkili olup olmadığını belirlemek ve farklı kan grupları ve plasenta konumu arasında herhangi bir ilişki olup olmadığını değerlendirmektir.
Gereç ve Yöntemler
Kadınların tıbbi kayıtları retrospektif olarak incelendi ve rutin doğum öncesi (20–38 hafta) ultrasonografide olgu notlarında dokümante edilen plasental pozisyon tanımlandı. Plasental pozisyon anterior, posterior ve fundal olarak kategorize edildi. Feto-maternal akıbet ve farklı kan grupları ile plasental konum ilişkisi not edildi.
Bulgular
Kadınlar toplam 474 vaka notu, plasental konum, feto-maternal akıbet ve kan grupları açısından analiz edildi. Posterior plasenta erken doğum ile anlamlı ilişkili (p<0.001) iken anterior plasenta; gebeliğe bağlı hipertansiyon, gestasyonel diabetes mellitus ve plasenta dekolmanı açısından daha büyük bir risk ile ilişkili bulundu (p<0.001). Fetal akıbet gözönüne alındığında bir anterior plasenta intrauterin gelişme geriliği ve intrauterin fetal ölüm ile belirgin ilişkili bulundu (p<0.001). Posterior plasenta grubunda kadınların %46’sının kan grubu A pozitif iken anterior plasentalı kadınların çoğunluğunun (% 54) kan grubu O-pozitif idi (p<0.001).
Sonuç
Anterior plasental yerleşim gebeliğe bağlı hipertansiyon, gestasyonel diabetes mellitus, plasenta dekolmanı, intrauterin gelişme geriliği ve intrauterin fetal ölüm riskinde artış ile ilişkilidir. Posterior plasenta erken doğum ve A pozitif kan grubu ile anlamlı bir ilişkiye sahiptir. Anterior plasenta O-pozitif kan grubuna sahip kadınlarda sık görülür. Plasentanın konumu gebelik sonucunun önemli bir belirleyicisi olabilir.
Introduction
In Saudi Arabia, screening ultrasonography (USG) of a large proportion of pregnant women is undertaken and they generally receive at least one obstetric USG for gestational age, amniotic fluid volume, foetal anatomic survey and placental location. Are these implantation sites predictive of an adverse pregnancy outcome? Only a limited number of investigators have dealt with placental implantation site and pregnancy outcome (1–3). Uterine blood supply is not uniformly distributed. The site of implantation and resultant location of the placenta within the uterus are likely important determinants of placental blood flow and therefore pregnancy success (4). There has been extensive research on low placental implantation because of the importance of detecting placenta previa. Only a few studies have been undertaken on other aspects of placental position and possible impact on pregnancy outcome. These studies reported that placental location might have implications for poor pregnancy outcome including preterm birth (5), small for gestational age (SGA) (4), foetal malposition, malpresentation and the development of pre-eclampsia (1, 6). In theory, lateral placental location could contribute a higher risk of foetal intrauterine growth retardation (IUGR). A case-control trial conducted in the USA revealed that women with their placenta located in the fundus carry an increased risk of premature rupture of membranes with all the consequential adverse sequelae (5). Reports on an association between IUGR and placental locations (other than placenta previa) have been conflicting (1, 7, 8).
This study was designed to investigate:
The association between placental location and foeto-maternal outcome of pregnancy.
The relationship of different maternal blood groups with placental location.
Material and Methods
This retrospective study was conducted at a Abha General Hospital, Abha, KSA. Our study group included women with singleton pregnancy, delivered vaginally after 28 weeks of gestation, who had prior documentation of placental location on the basis of antenatal USG. The study outcome was the relationship of different placental locations with antenatal foeto-maternal complications, like pregnancy-induced hypertension (PIH), gestational diabetes mellitus (GDM), placental abruption, bad obstetric history (BOH), preterm delivery, intrauterine growth retardation (IUGR), intrauterine foetal death (IUFD) and neonatal outcome. The records of 500 subjects were ascertained. It is our departmental policy to offer a routine scan at 18–20 weeks or later if the booking is late. The details of placental locations are recorded apart from other parameters. We categorised each placenta as anterior, posterior and fundal. Placentas occupying the left or right region of the anterior and posterior uterine walls were considered anterior and posterior, respectively. The following data were collected - maternal age, gravidity, parity, number of miscarriages, gestational age at delivery, maternal blood group, birth weight (BW) of the baby, and 1 minute and 5 minute Apgar scores. The data were analysed using SPSS version 17. The results have been expressed in terms of probability (p) value. A chi squared test was used for categorical data and unpaired t test for continuous data. A p-value <0.05 was considered statistically significant. The study was approved by our Institutional Research and Ethics Committee.
Results
The study group consisted of 500 cases who delivered vaginally, during November and December 2012. Of these, 10 cases who delivered before 28 weeks, 10 women who came fully dilated without prior documented placental location by USG and six cases that had multiple pregnancies were excluded, leaving a total of 474 women. Table 1 describes the characteristics of the pregnant women according to placental location. There were no differences between baseline characteristics among three placental location categories. Fundal location was noted in 46%, anterior in 28% and posterior in 26% women (Figure 1). Neonatal outcome according to placental locations are shown in Table 2. There was no significant difference in gestational age at birth, mean BW and Apgar scores. Table 3 shows the association of different maternal blood groups with placental location. The commonest blood groups were O-positive (49%, n=236) and A-positive (36%, n=173). The majority (54%, n=72) of women with O-positive blood group had anterior placenta (p<0.001), while A-positive blood group was associated with posterior placenta in the majority of cases (46%, n=57, p<0.001)
Table 1.
Relationship between placental location and maternal characteristics
| Characteristic | Fundal N=218 | Anterior N=133 | Posterior N=123 | p value |
|---|---|---|---|---|
| Past history | ||||
| Gravidity (Mean±SD) | 5.4±2.2 | 5.03±1.7 | 5.5±2.6 | 0.55 |
| Parity (Mean±SD) | 3.8±1.9 | 3.54±1.6 | 3.8±2.1 | 0.54 |
| Miscarriage (Mean±SD) | 0.83±1.5 | 0.63±2.0 | 0.9±1.0 | 0.48 |
| Bad obstetric history (%) | 2(0.9) | 2(1.5) | 0 | <0.001 |
| Present age & complications | ||||
| Maternal age (Mean±SD) | 32.9±5.1 | 31.8±5.2 | 31.9±4.9 | 2.45 |
| PIH (%)† | 7(3.2) | 5(3.7) | 2(1.6) | <0.001 |
| GDM (%)‡ | 6(2.7) | 8(6.0) | 2(1.6) | <0.001 |
| Placental abruption (%) | 5(2.3) | 5(3.7) | 0 | <0.001 |
| PTL (%)¥ | 0 | 0 | 3(2.4) | <0.001 |
SD: standard deviation;
PIH -pregnancy induced hypertension;
GDM - gestational diabetes mellitus;
PTL - pre-term labour
Figure 1.
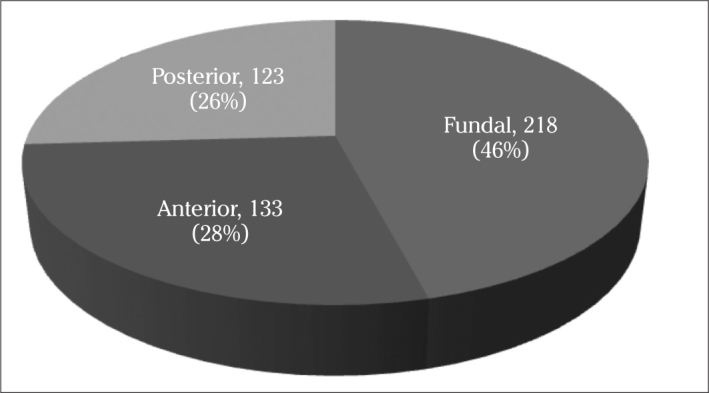
Location of placenta in 474 women
Table 2.
Relationship of foetal outcome with placental location
| Variable | Fundal N=218 | Anterior N=133 | Posterior N=123 | p value |
|---|---|---|---|---|
| Gestational age (Mean±SD) | 37.9±1.5 | 37.2±2 | 37.8±1.4 | 2.45 |
| Foetal weight, grams (Mean±SD) | 2857±493.4 | 2808±658.3 | 2842±503 | |
| APGAR score (mean) | ||||
| 1 min | 6.2 | 6.1 | 6.2 | 2.48 |
| 5 min | 8.7 | 8.4 | 8.8 | 3.55 |
| IUGR (%)† | 0 | 4 (3) | 0 | <0.001 |
| Congenital anomalies (%) | 3 (1.4) | 0 | 0 | <0.001 |
| IUFD (%)‡ | 3 (1.4) | 2 (1.5) | 0 | <0.001 |
SD: standard deviation;
IUGR- intrauterine growth retardation;
IUFD- intrauterine foetal death
Table 3.
Association of placental location with blood groups
| Blood group N=(474) | Fundal N=218(%) | Anterior N=133(%) | Posterior N=123(%) | p value |
|---|---|---|---|---|
| O-positive | 108 (49.5) | 72 (54) | 56 (45.5) | <0.001 |
| O-negative | 14 (6.4) | 4 (3) | 0 | <0.001 |
| A-positive | 70 (32) | 46 (34.5) | 57 (46.3) | <0.001 |
| A-negative | 6 (2.7) | 2 (1.5) | 0 | 0.56 |
| B-positive | 14 (6.4) | 9 (6.7) | 10 (8.1) | 0.56 |
| B-negative | 2 (0.9) | 0 | 0 | 0.005 |
| AB-positive | 0 | 0 | 0 | 0 |
| AB-negative | 4 (1.8) | 0 | 0 | 0.005 |
Discussion
The blood supply of the uterus is not uniformly distributed and placental location is an important determinant of placental blood flow, as measured by uterine artery Doppler velocimetery (7, 9, 10). There are limited data on the association between placental location, pregnancy complications and perinatal outcome. Some researchers have described that placental location has implications for poor pregnancy outcomes, including preterm birth (5) and small for gestational age (SGA) (4). This study showed a significant association between posterior placenta and preterm labour. In contrast, we did not find any association with SGA. Our finding is consistent with another report (11). Hadley et al. (5) reported that a placenta located in the fundus carries a significantly higher risk of premature rupture of the membrane. They presumed that fundal location of the placenta places the weakest point of the membrane over the cervical os and thus predisposes the women to premature rupture of membrane with all of the consequential adverse sequelae. Contrarily, we found a significant association of posterior placenta with preterm labour. This is probably because placenta located on the posterior uterine wall may be somehow less efficient due to the anatomy of that wall (12). As a result of uneven uterine blood supply (4), the posterior wall of the pregnant uterus is longer (13) and somewhat thicker (14). Each of these factors may affect uterine blood supply, especially as the uterus expands to accommodate the pregnancy. Janewarland et al. (12), in a case-control study, reported that posterior placenta is statistically more likely to result in a still birth. They described that its exact cause is not clear but they put forward three possible hypotheses: the structure of posterior uterine wall is somehow at fault, there may be associated intrauterine factors with the posterior-located placenta, or the pregnant woman’s sleeping position is the problem. However, we did not observe such relation. Rather, this study found a significant correlation between fundal and anterior placenta with IUFD (Table 2). The present study showed a statistically significant association of anterior placenta with an increased incidence of PIH, GDM, BOH, placental abruption, IUGR and IUFD. One of the explanations may be non-uniform uterine blood supply or it might be by chance due to the small sample size; further research is needed to verify these findings. In line with Karthika et al. (15), we did not observe a significant difference in mean BW among different placental location groups. The current study showed that IUGR pregnancies had a significant association with anterior placentas. Although the mean BW of anteriorly placed placental pregnancies is low, it is not significant because the number of IUGR pregnancies is only four out of 133 cases. However, Lucy et al. (4) described a positive correlation between IUGR and lateral placentas, rather than anterior and posterior. Kofinas et al. (7) reported that unilateral placentas are more common than central (anterior and posterior) ones in pregnancies with IUGR and/or pre-eclampsia. Consistent with our findings, Booth et al. (16) reported a significant association between fundal placentation and PIH. The present study revealed a significant association of fundal and anterior placentas with PIH and IUGR. In contrast, a recent population-based case-control study of more than 3000 pregnancies (10) reported that the risk of having a foetus with IUGR was not increased by the site of placental implantation. However, that study grouped placental locations in three broad categories (low, high lateral and high fundal) which did not differentiate central (anterior or posterior) placenta. The observation that most of the placentas in this study were located in fundus is not consistent with prior reports (16–18). At least in theory, a placenta which is primarily implanted near the uterine and/or ovarian arteries might receive more blood than one implanted centrally, whether anterior or posterior, and this could account for poor pregnancy outcome with anterior placenta, as seen in our study. In the three groups of placental location (fundal, anterior and posterior), the mean gestational age and BW were found to be almost the same; however, some have reported the negative impact of fundal location of placenta on these findings. Kalanithi et al. (4) studied the possible influence of placental location on the Apgar scores of newborns. They described the location of the placenta as either fundal, uterine body or lower uterine segment. They found no case of low Apgar score (<4) in the lower uterine segment group, whereas they found that the higher the placenta was situated in the uterus, the greater the incidence of an Apgar score <4 (i.e. 0.6% in the uterine body group and 2.4% in the fundal group). Our study showed no correlation between low Apgar score and placental location. We found no case with Apgar score <4.
We observed that anterior placenta have a strong association with O-positive blood group and posterior placenta with A-positive blood group. Therefore, O-positive blood group women are more prone to antenatal complications, which are commoner in anterior placenta women. To the best of our knowledge, either no work or only small studies have been performed in this regard. Large scale studies are required to confirm these findings. The retrospective nature of this study is a limitation, chiefly because of “observer variation” as a result of different sonographers locating the placental position with variable reporting styles and experience. Nevertheless, a large prospective study, where the placental positions are determined by only one experienced sonographer, would be useful to confirm the findings of this study.
In summary, pregnancies with anterior placenta are complicated by PIH, GDM, placental abruption, IUGR and IUFD as compared to fundal or posterior ones. Anterior placenta is common in O-positive and posterior placenta in A-positive blood group. Women with posterior placenta have a greater risk of premature delivery. This study supports the hypothesis that the location of the placenta is associated with pregnancy success. Therefore, placental location may be an important determinant of pregnancy outcome. Additional research is needed to confirm this observation and to determine whether pregnancies with anterior placenta may benefit from more intensive monitoring.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for the study.
Informed Consent: N/A
Peer-review: Externally peer-reviewed.
Conflict of Interest: No conflict of interest was declared by the author.
Financial Disclosure: The author declared that this study received no financial support.
References
- 1.Magann EF, Doherty DA, Turner K, Lanneau GS, Jr, Morrison JC, Newnham JP. Second trimester placental location as a predictor of an adverse pregnancy outcome. J Perinatol. 2007;27:9–14. doi: 10.1038/sj.jp.7211621. http://dx.doi.org/10.1038/sj.jp.7211621. [DOI] [PubMed] [Google Scholar]
- 2.Leiberman JR, Fraser D, Kasis A, Mazor M. Reduced frequency of hypertensive disorders in placenta previa. Obstet Gynecol. 1991;77:836–9. [PubMed] [Google Scholar]
- 3.Newton ER, Barass V, Cetrulo CL. The epidemiology and clinical history of asymptomatic midtrimester placenta previa. Am J Obstet Gynecol. 1984;148:743–8. doi: 10.1016/0002-9378(84)90559-3. http://dx.doi.org/10.1016/0002-9378(84)90559-3. [DOI] [PubMed] [Google Scholar]
- 4.Kalanithi LE, Illuzzi JL, Nossov VB, Frisbaek Y, Abdel-Razeq S, Copel JA, et al. Intrauterine growth restriction and placental location. J Ultrasound Med. 2007;26:1481–9. doi: 10.7863/jum.2007.26.11.1481. [DOI] [PubMed] [Google Scholar]
- 5.Hadley CB, Main DM, Gabbe SG. Risk factors for premature rupture of the fetal membranes. Am J Perinatol. 1990;7:374–9. doi: 10.1055/s-2007-999527. http://dx.doi.org/10.1055/s-2007-999527. [DOI] [PubMed] [Google Scholar]
- 6.Hoogland HJ, de Haan J. Ultrasonographic placental localization with respect to fetal position in utero. Eur J Obstet Gynecol Reprod Biol. 1980;11:9–15. doi: 10.1016/0028-2243(80)90047-7. http://dx.doi.org/10.1016/0028-2243(80)90047-7. [DOI] [PubMed] [Google Scholar]
- 7.Kofinas AD, Penry M, Swain M, Hatjis CG. Effect of placental laterality on uterine artery resistance and development of preeclampsia and intrauterine growth retardation. Am J Obstet Gynecol. 1989;161:1536–9. doi: 10.1016/0002-9378(89)90920-4. http://dx.doi.org/10.1016/0002-9378(89)90920-4. [DOI] [PubMed] [Google Scholar]
- 8.Vaillant P, Best MC, Cynober E, Devulder G. Pathological Doppler uterine readings when the placenta is laterally situated. J Gynecol Obstet Biol Reprod (Paris) 1993;22:301–7. [PubMed] [Google Scholar]
- 9.Kofinas AD, Penry M, Greiss FC, Jr, Meis PJ, Nelson LH. The effect of placental location on uterine artery flow velocity waveforms. Am J Obstet Gynecol. 1988;159:1504–8. doi: 10.1016/0002-9378(88)90584-4. http://dx.doi.org/10.1016/0002-9378(88)90584-4. [DOI] [PubMed] [Google Scholar]
- 10.Ito Y, Shono H, Shono M, Muro M, Uchiyama A, Sugimori H. Resistance index of uterine artery and placental location in intrauterine growth retardation. Acta Obstet Gynecol Scand. 1998;77:385–90. http://dx.doi.org/10.1034/j.1600-0412.1998.770405.x. [PubMed] [Google Scholar]
- 11.Cho JY, Lee YH, Moon MH, Lee JH. Difference in migration of placenta according to the location and type of placenta previa. J Clin Ultrasound. 2008;36:79–84. doi: 10.1002/jcu.20427. http://dx.doi.org/10.1002/jcu.20427. [DOI] [PubMed] [Google Scholar]
- 12.Warland J, McCutcheon H, Baghurst P. Placental position and stillbirth: a case-control study. Journal of Clinical Nursing. 2009;18:1602–6. doi: 10.1111/j.1365-2702.2008.02779.x. http://dx.doi.org/10.1111/j.1365-2702.2008.02779.x. [DOI] [PubMed] [Google Scholar]
- 13.Andersen KV, Munck O, Larsen JF, Kjeldsen H. Placental flow index in posterior wall placentas measured with 99 mtechnecium-labelled human serum albumen. Clinical Physiology. 1983;17:577–80. doi: 10.1111/j.1475-097x.1983.tb00867.x. http://dx.doi.org/10.1111/j.1475-097X.1983.tb00867.x. [DOI] [PubMed] [Google Scholar]
- 14.Degani S, Leibovitz Z, Shapiro I, Gonen R, Ohel G. Myometrial thickness in pregnancy: Longitudinal sonographic study. J Ultrasound Med. 1998;17:661–5. doi: 10.7863/jum.1998.17.10.661. [DOI] [PubMed] [Google Scholar]
- 15.Devarajan K, Kives S, Ray JG. Placental location and newborn weight. J Obstet Gynaecol Can. 2012;34:325–9. doi: 10.1016/S1701-2163(16)35212-4. [DOI] [PubMed] [Google Scholar]
- 16.Booth RT, Wood C, Beard RW, Gibson JR, Pinkerton JH. Significance of site of placental attachment in uterus. Br Med J. 1962;5294:1732–4. doi: 10.1136/bmj.1.5294.1732. http://dx.doi.org/10.1136/bmj.1.5294.1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fried AM. Distribution of the bulk of the normal placenta: review and classification of 800 cases by ultrasonography. Am J Obstet Gynecol. 1978;132:675–80. doi: 10.1016/0002-9378(78)90863-3. [DOI] [PubMed] [Google Scholar]
- 18.Magann EF, Evans SF, Newnham JP. Placental implantation at 18 weeks and migration throughout pregnancy. South Med J. 1998;91:1025–7. doi: 10.1097/00007611-199811000-00006. http://dx.doi.org/10.1097/00007611-199811000-00006. [DOI] [PubMed] [Google Scholar]


