Abstract
Objectives. We examined associations between macrolevel economic factors hypothesized to drive changes in distributions of weight and body mass index (BMI) in a representative sample of 200 796 men and women from 40 low- and middle-income countries.
Methods. We used meta-regressions to describe ecological associations between macrolevel factors and mean BMIs across countries. Multilevel regression was used to assess the relation between macrolevel economic characteristics and individual odds of underweight and overweight relative to normal weight.
Results. In multilevel analyses adjusting for individual-level characteristics, a 1–standard-deviation increase in trade liberalization was associated with 13% (95% confidence interval [CI] = 0.76, 0.99), 17% (95% CI = 0.71, 0.96), 13% (95% CI = 0.76, 1.00), and 14% (95% CI = 0.75, 0.99) lower odds of underweight relative to normal weight among rural men, rural women, urban men, and urban women, respectively. Economic development was consistently associated with higher odds of overweight relative to normal weight. Among rural men, a 1–standard-deviation increase in foreign direct investment was associated with 17% (95% CI = 1.02, 1.35) higher odds of overweight relative to normal weight.
Conclusions. Macrolevel economic factors may be implicated in global shifts in epidemiological patterns of weight.
Cardiovascular diseases are among the leading causes of death in low- and middle-income countries (LMICs),1 where mortality from such diseases has been increasing and is expected to continue doing so until 2030.2 In parallel to this trend, there has been an increase in average body mass index (BMI; defined as weight in kilograms divided by the square of height in meters) in most regions of the world.3 With population-based studies indicating a U- or J-shaped relation between BMI and cardiovascular disease mortality,4,5 these shifts in BMI may increase the proportion of the population at greatest risk for cardiovascular diseases. As such, increases in BMI may contribute to escalating cardiovascular disease mortality in LMICs,6 highlighting the need for understanding BMI patterns and predictors.
Comparative longitudinal data that can be used to monitor BMI changes (often expressed according to prevalence of underweight, overweight, and obesity) across LMICs are scant; however, existing data suggest that the prevalence of underweight has decreased, the prevalence of overweight and obesity has increased, and, in general, there is a greater burden of overweight than underweight in most LMICs, particularly in urban areas.7–9 Shifts in the key determinants of weight, including diet and physical activity, are hypothesized to influence these patterns.3 Major changes in global dietary consumption have increased per capita food intake in LMICs, as well as the proportion of people’s daily diet derived from energy-dense and fatty foods.3,10–12 Although cross-national and longitudinal data on physical activity are limited, available evidence suggests that forms of transportation, employment, and leisure activities have become more sedentary and may contribute to changing patterns of weight at the population level.13,14
Macrolevel economic factors, including economic development, urbanization, foreign investment, and trade liberalization, are hypothesized to drive shifting patterns of dietary composition, physical activity, and other determinants of nutritional outcomes.3,15 Economic growth and attendant increases in per capita income, for example, are associated with increased consumption of energy-dense foods,16 and recent cross-national analyses suggest that economic development is associated with a faster rate of growth in the prevalence of overweight among lower-income groups in LMICs.17,18 Urbanization is hypothesized to increase access to processed diets, reduce opportunities for physical activity, and expose residents to food marketing, thereby promoting a more sedentary lifestyle associated with less energy expenditure and greater caloric intake.15
The influx of foreign direct investment (FDI), defined as investments by an enterprise in one country intended to acquire a lasting management interest in an enterprise operating in a foreign economy, represents one mechanism through which transnational corporations enter into new markets. FDI inflows are, along with greater openness to trade,19 hypothesized to be a key element in reshaping the global market for food, particularly in LMICs, by threatening traditional modes of agricultural production and facilitating the processing, distribution, and marketing of lower-cost, energy-dense food.20,21
Despite the potential role that these macrolevel economic factors may play in shaping the epidemiological pattern of diet, behavior, and weight in LMICs, few empirical studies have investigated the relation between contextual factors and individual weight. A limited number of ecological studies have been conducted,9,22 but their results cannot be used to draw inferences about health at the individual level. Furthermore, the social patterning of diet and physical activity according to area of residence (urban or rural) and gender suggests that the macrolevel factors posited to drive changes in weight may have distinct implications for particular groups of individuals,23,24 and ecological studies cannot assess whether associations between macrolevel economic characteristics and weight vary according to such individual-level characteristics.
We used data from a sample of approximately 200 000 adults from 40 LMICs to describe the ecological associations between macrolevel economic factors hypothesized to drive changes in determinants of weight (i.e., economic development, urbanization, FDI, trade liberalization) and average BMIs across countries and examine the association between macrolevel characteristics and the probability at the individual level of underweight and overweight or obesity relative to normal weight. We also assessed cross-level interactions of macrolevel factors with gender and area of residence.
METHODS
The World Health Survey (WHS) was carried out in 2002–2003 in 70 countries across all continents and levels of development to provide comparable cross-national measures of population health, health services, and other health system activities. The sampling frame for these nationally representative surveys included 100% of the eligible population in each surveyed country. A probability sampling design was used to select individual respondents. In most countries, multistage cluster sampling was used to randomly select private households for interviews. Resident adults aged 18 years or older were eligible to be interviewed; a Kish table was used to select a respondent from each household to complete the individual interview. The WHS has been used extensively for making cross-national comparisons of population health, including weight.25–29 Further details are available elsewhere.30,31
We used the World Bank income classifications for low- and middle-income countries (those with gross national incomes of $12 195 or below) to identify 43 LMICs from the 70 WHS countries; we excluded 3 countries with missing information on the macrolevel characteristics of interest or missing probability of selection weights for all respondents. The average response rate across the 39 countries with available data on response rate (these data were not reported for Bosnia and Herzegovina) was 96.09%. We restricted our analyses to adults between the ages of 18 and 65 years.
Measures
We used self-reported height and weight to calculate BMI and weight status. BMI was used to classify respondents as underweight (BMI < 18.5), normal weight (BMI = 18.5–24.9), or overweight–obese (BMI ≥25.0; hereafter referred to as “overweight”) according to the World Health Organization’s classification system.32
Data were collected on respondents’ demographic characteristics (e.g., sex, age, marital status), and interviewers recorded information on area of residence (urban or rural) at the time of the assessment. We measured socioeconomic status (SES) according to respondents’ years of educational attainment, split into country-specific tertiles for our analysis. We used the approach developed by Ferguson et al.33 to estimate country-specific household permanent income; this approach assumes that SES is a latent variable that can be estimated on the basis of ownership of assets (e.g., radios, televisions, cars), access to services (e.g., electricity, running water, sewerage), and known predictors of income (e.g., age and education), in this case via a dichotomous hierarchical ordered probit model. This method has been used in prior WHS analyses34,35 as well as other investigations,36 and validation studies show moderate to high correlations between estimated income and reported household income.33 We split household permanent income into country-specific quartiles for our analysis.
Measures of health status included overall self-rated health (categorized as good to excellent, moderate, or bad to very bad) and the extent to which respondents reported difficulty moving around in the preceding 30 days (categorized as no to mild difficulty, moderate difficulty, or severe to extreme difficulty). We measured whether the respondent was a current smoker of any tobacco products.
At the country level, we used information from the World Bank’s World Development Indicators database for the year 2000 to measure levels of economic development, urbanization, and FDI.37 We assessed economic development according to per capita gross domestic product (GDP), converted to international dollars (via purchasing power parity rates) and mean centered for our multivariable analyses. Urbanization was measured according to the percentage of a country’s population living in urban areas, as defined by national statistical offices; this variable was also mean centered for our analyses. We measured FDI inflows as a percentage of GDP, a common measure of level of FDI penetration,19,38 and standardized these data as z scores so that higher values reflected greater FDI.
Trade liberalization was measured according to countries’ mean tariff percentage averaged over the years 1990 to 1999, a common measure of openness to trade; these data were based on calculations by Wacziarg and Welch39 and derived from the United Nations Conference on Trade and Development, the World Bank, and the World Trade Organization. The average tariff was unavailable for 5 countries, and in these cases we substituted the mean tariff for the year most proximate to 1995 from the World Development Indicators database.37 Mean tariffs were standardized as z scores and reverse coded so that higher values reflected greater openness to trade.
Statistical Analyses
Approximately 38% of the participants were missing data on at least one individual-level covariate, raising concerns that a complete-case analysis would introduce selection bias. We used multiple imputation, which has been demonstrated to reduce bias and improve efficiency relative to listwise deletion, for these missing data.40,41 Imputation was carried out in Amelia II, which imputes data via a bootstrapping-based expectation maximization algorithm under the assumptions that data are missing at random and complete data are in multivariate normal form.42,43 We used available information on health and sociodemographic covariates to produce 10 imputed data sets.
We calculated country-specific mean BMIs for men and women and used random effects meta-regression analyses to assess the unadjusted ecological associations between macrolevel factors and male and female mean BMIs across countries. These models, run via the Metafor package in R,44 were weighted by the inverse of the standard error of the gender-specific mean BMI for each country.
We used multinomial regression models with a logit link function to assess the adjusted multilevel relations between our individual- and country-level covariates of interest and the odds of underweight and overweight relative to normal weight within each of the 4 strata defined by gender (male–female) and residence (urban–rural). We included a random intercept to account for within-country clustering. All analyses were weighted by the WHS individual probability of selection weights. The Mplus statistical software package (Muthén and Muthén, Los Angeles, CA) was used to estimate multilevel models.
RESULTS
Table 1 shows, for each country, weighted mean BMIs for the overall sample and for men and women. There were substantial variations in weight status across LMICs. Mean BMIs were lowest among Asian countries, with India having the lowest mean BMI (20.24). Conversely, average BMIs were highest in countries in Europe and Central Asia, Latin America, and the Caribbean. Sample characteristics are shown in Table 2. Across countries, the mean GDP per capita (in current international dollars) was $3448 (SD = 2711.49), the mean percentage of the population residing in urban areas was 43.68 (SD = 19.26), the mean FDI as a percentage of GDP was 2.83 (SD = 2.01), and the mean tariff percentage was 18.94 (SD = 11.17).
TABLE 1—
Response Rate, Sample Size, and Weighted Mean Body Mass Index by Region and Country: 40 Low- and Middle-Income Countries Included in the World Health Survey, 2002–2003
| Region and Country | Response Rate, %a | Sample Size, No. | Total, Weighted Mean BMI (SE) | Men, Weighted Mean BMI (SE) | Women, Weighted Mean BMI (SE) |
| Africa | |||||
| Burkina Faso | 98.75 | 4538 | 20.87 (0.12) | 21.00 (0.15) | 20.76 (0.18) |
| Chad | 97.20 | 4305 | 24.07 (0.12) | 24.00 (0.15) | 24.14 (0.16) |
| Congo | 98.18 | 2376 | 23.46 (0.17) | 23.23 (0.21) | 23.68 (0.24) |
| Cote D’Ivoire | 99.22 | 3023 | 23.17 (0.09) | 23.06 (0.11) | 23.33 (0.15) |
| Ethiopia | 98.92 | 4645 | 21.01 (0.10) | 21.01 (0.11) | 21.01 (0.16) |
| Ghana | 96.70 | 3541 | 22.72 (0.09) | 22.18 (0.12) | 23.24 (0.13) |
| Kenya | 95.85 | 4009 | 22.59 (0.13) | 21.79 (0.17) | 23.36 (0.18) |
| Malawi | 96.06 | 4866 | 23.56 (0.08) | 23.78 (0.12) | 23.35 (0.10) |
| Mali | 84.80 | 3485 | 20.67 (0.14) | 20.71 (0.17) | 20.64 (0.21) |
| Mauritania | 98.74 | 3527 | 23.48 (0.13) | 22.69 (0.19) | 24.22 (0.17) |
| Mauritius | 98.08 | 3538 | 23.63 (0.10) | 23.52 (0.12) | 23.75 (0.14) |
| Namibia | 98.65 | 3911 | 23.06 (0.12) | 22.94 (0.18) | 23.16 (0.16) |
| Senegal | 90.06 | 2812 | 22.72 (0.15) | 22.22 (0.17) | 23.19 (0.23) |
| South Africa | 90.02 | 2241 | 24.14 (0.16) | 24.07 (0.19) | 24.22 (0.22) |
| Swaziland | 98.26 | 2816 | 25.82 (0.16) | 25.57 (0.25) | 26.02 (0.22) |
| Zambia | 93.92 | 3586 | 22.29 (0.11) | 22.23 (0.17) | 22.36 (0.16) |
| East Asia and the Pacific | |||||
| China | 99.97 | 3487 | 21.93 (0.07) | 22.08 (0.10) | 21.79 (0.11) |
| Lao People’s Democratic Republic | 91.42 | 4628 | 21.36 (0.05) | 21.47 (0.07) | 21.24 (0.07) |
| Malaysia | 99.08 | 5602 | 23.64 (0.08) | 23.56 (0.12) | 23.72 (0.11) |
| Philippines | 99.95 | 9458 | 21.95 (0.05) | 21.98 (0.08) | 21.92 (0.08) |
| Europe and Central Asia | |||||
| Bosnia and Herzegovina | … | 839 | 24.58 (0.16) | 24.84 (0.25) | 24.33 (0.21) |
| Georgia | 98.92 | 2108 | 25.06 (0.10) | 25.46 (0.14) | 24.70 (0.15) |
| Kazakhstan | 99.93 | 4250 | 24.62 (0.11) | 24.53 (0.18) | 24.70 (0.13) |
| Latvia | 93.96 | 630 | 25.26 (0.21) | 25.07 (0.27) | 25.43 (0.30) |
| Russia | 99.91 | 3229 | 25.46 (0.17) | 25.16 (0.18) | 25.64 (0.25) |
| Turkey | 97.46 | 10 035 | 24.90 (0.07) | 24.89 (0.09) | 24.91 (0.10) |
| Ukraine | 89.19 | 2025 | 25.13 (0.14) | 24.96 (0.19) | 25.28 (0.19) |
| Latin America and the Caribbean | |||||
| Brazil | 100.00 | 4475 | 24.36 (0.08) | 24.56 (0.10) | 24.17 (0.11) |
| Dominican Republic | 94.33 | 4031 | 24.60 (0.12) | 24.72 (0.16) | 24.47 (0.17) |
| Ecuador | 82.20 | 4167 | 24.43 (0.11) | 24.43 (0.15) | 24.43 (0.14) |
| Mexico | 99.67 | 34 501 | 25.31 (0.04) | 25.18 (0.06) | 25.43 (0.06) |
| Paraguay | 97.21 | 4668 | 24.56 (0.08) | 24.87 (0.10) | 24.25 (0.12) |
| Uruguay | 99.73 | 2494 | 25.03 (0.10) | 25.48 (0.13) | 24.59 (0.16) |
| Middle East and North Africa | |||||
| Morocco | 89.44 | 4099 | 23.73 (0.13) | 23.23 (0.17) | 24.22 (0.19) |
| Tunisia | 99.04 | 4436 | 23.96 (0.08) | 23.73 (0.09) | 24.19 (0.12) |
| South Asia | |||||
| Bangladesh | 93.67 | 5225 | 21.86 (0.09) | 21.57 (0.12) | 22.16 (0.17) |
| India | 97.06 | 9158 | 20.24 (0.07) | 20.38 (0.09) | 20.10 (0.11) |
| Nepal | 98.51 | 8057 | 21.81 (0.08) | 21.50 (0.10) | 22.13 (0.13) |
| Pakistan | 94.28 | 5808 | 22.98 (0.10) | 22.94 (0.13) | 23.02 (0.16) |
| Sri Lanka | 99.07 | 6169 | 21.12 (0.08) | 21.18 (0.10) | 21.06 (0.12) |
Note. BMI = body mass index. The sample size was n = 200 796.
Number of individual interviews completed or partially completed divided by number of individuals selected.
TABLE 2—
Sample Characteristics by Area of Residence and Gender: 40 Low- and Middle-Income Countries Included in the World Health Survey, 2002–2003
| Characteristic | Total (n = 200 796), Mean ±SE or % (SE) | Urban Men (n = 44 253), Mean ±SE or % (SE) | Urban Women (n = 56 201), Mean ±SE or % (SE) | Rural Men (n = 45 914), Mean ±SE or % (SE) | Rural Women (n = 54 427), Mean ±SE or % (SE) |
| Age, y | 35.63 ±0.07 | 35.43 ±0.12 | 36.22 ±0.12 | 35.25 ±0.13 | 35.70 ±0.14 |
| Years of educational attainment | 6.56 ±0.03 | 8.91 ±0.05 | 8.09 ±0.05 | 5.89 ±0.07 | 4.03 ±0.05 |
| Continuous household permanent income value | −0.4 ±0.00 | 0.25 ±0.01 | 0.23 ±0.01 | −0.24 ±0.01 | −0.28 ±0.01 |
| Marital status | |||||
| Currently married | 61.52 (0.11) | 56.66 (0.24) | 55.37 (0.22) | 67.19 (0.23) | 67.03 (0.21) |
| Never married | 20.92 (0.09) | 29.12 (0.23) | 20.03 (0.17) | 23.07 (0.21) | 13.35 (0.16) |
| Othera | 17.56 (0.09) | 14.22 (0.18) | 24.60 (0.19) | 9.74 (0.14) | 19.62 (0.18) |
| Self-rated health status | |||||
| Good or excellent | 65.15 (0.11) | 70.86 (0.22) | 60.79 (0.21) | 69.12 (0.22) | 61.64 (0.21) |
| Moderate | 27.62 (0.10) | 24.37 (0.21) | 31.68 (0.20) | 24.46 (0.20) | 28.74 (0.20) |
| Bad or very bad | 7.23 (0.06) | 4.77 (0.10) | 7.53 (0.11) | 6.41 (0.12) | 9.62 (0.13) |
| Level of difficulty moving around in past 30 d | |||||
| No or mild difficulty | 86.43 (0.08) | 90.76 (0.14) | 85.96 (0.15) | 87.62 (0.15) | 82.39 (0.16) |
| Moderate difficulty | 9.30 (0.07) | 6.85 (0.12) | 9.80 (0.13) | 8.35 (0.13) | 11.59 (0.14) |
| Extreme or severe difficulty | 4.27 (0.05) | 2.40 (0.07) | 4.24 (0.09) | 4.03 (0.09) | 6.02 (0.10) |
| Currently smokes any tobacco products | |||||
| No | 75.21 (0.10) | 60.35 (0.24) | 87.58 (0.14) | 58.16 (0.23) | 88.89 (0.14) |
| Yes | 24.29 (0.10) | 39.04 (0.23) | 12.10 (0.14) | 41.16 (0.23) | 10.68 (0.13) |
Note. Distributions were weighted by probability of selection weights.
Separated, divorced, widowed, or cohabiting.
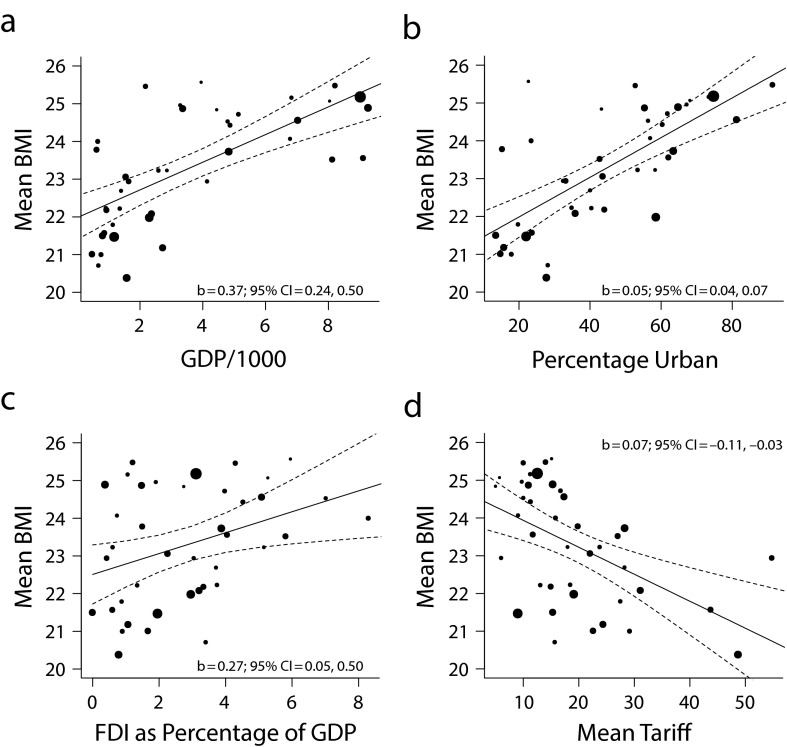
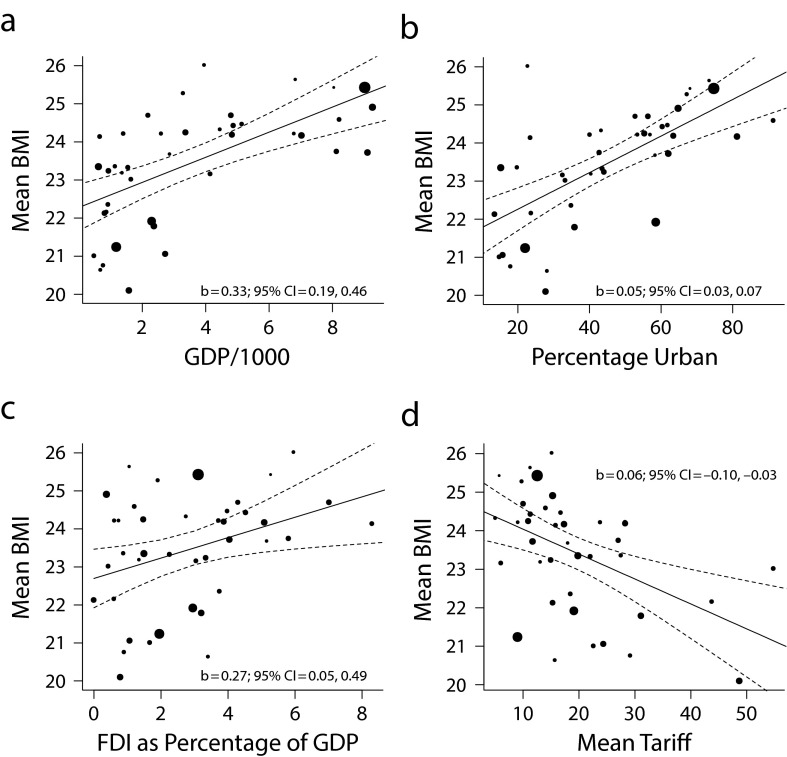
Results from our meta-regression analyses (Figure 1) suggested that mean BMIs for men increased by 0.37 units for every $1000 increase in per capita GDP (95% confidence interval [CI] = 0.24, 0.50), 0.05 units for every 1–percentage-point increase in the proportion of urban residents (95% CI = 0.04, 0.07), 0.27 units per 1–percentage-point increase in FDI as a percentage of GDP (95% CI = 0.05, 0.50), and 0.07 units per 1–percentage-point decrease in the mean tariff (95% CI = 0.03, 0.11). Associations between macrolevel characteristics and mean BMIs for women were similar (Figure 2).
FIGURE 1—
Ecological associations between mean BMI among men and macrolevel characteristics (a) per capita GDP, (b) percentage of urban residents, (c) FDI as a percentage of GDP, and (d) mean tariff: 40 low- and middle-income countries included in the World Health Survey, 2002–2003.
Note. BMI = body mass index; CI = confidence interval; FDI = foreign direct investment; GDP = gross domestic product. Results are derived from bivariate random-effects meta-regression models weighted by the inverse of the standard error of the mean BMI for men in each country. The sample size was n = 90 167.
FIGURE 2—
Ecological associations between mean BMI among women and macrolevel characteristics (a) per capita GDP, (b) percentage of urban residents, (c) FDI as a percentage of GDP, and (d) mean tariff: 40 low- and middle-income countries included in the World Health Survey, 2002–2003.
Note. BMI = body mass index; CI = confidence interval; FDI = foreign direct investment; GDP = gross domestic product. Results are derived from bivariate random-effects meta-regression models weighted by the inverse of the standard error of the mean BMI for women in each country. The sample size was n = 110 628.
Multilevel associations between individual- and country-level characteristics and the odds of underweight and overweight relative to normal weight for urban and rural respondents, stratified by gender, are shown in Tables 3 and 4, respectively. At the individual level, never-married (vs currently married) status was positively associated with underweight and negatively associated with overweight. Higher incomes were associated with lower odds of underweight relative to normal weight and higher odds of overweight relative to normal weight. Worse health, measured according to poorer self-rated health and more difficulty moving around, was positively associated with both underweight and overweight relative to normal weight for some groups. For example, bad or very bad (vs good or excellent) self-rated health was positively associated with underweight relative to normal weight among men and with overweight relative to normal weight among urban women.
TABLE 3—
Multilevel Regression Model Results Showing Associations Between Individual- and Country-Level Characteristics and Odds of Underweight and Overweight Relative to Normal Weight Among Urban Men and Women: 40 Low- and Middle-Income Countries Included in the World Health Survey, 2002–2003
| Urban Men |
Urban Women |
|||
| Underweight vs Normal Weight, OR (95% CI) | Overweight vs Normal Weight, OR (95% CI) | Underweight vs Normal Weight, OR (95% CI) | Overweight vs Normal Weight, OR (95% CI) | |
| Individual-level characteristics | ||||
| Agea | 0.88 (0.83, 0.93) | 1.23 (1.16, 1.30) | 0.85 (0.81, 0.91) | 1.28 (1.21, 1.34) |
| Marital status | ||||
| Currently married (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Never married | 1.42 (1.23, 1.65) | 0.63 (0.56, 0.70) | 1.44 (1.26, 1.63) | 0.68 (0.61, 0.76) |
| Otherb | 0.92 (0.72, 1.19) | 0.97 (0.86, 1.09) | 1.09 (0.92, 1.30) | 0.94 (0.86, 1.03) |
| Educational attainment tertile | ||||
| Lowest (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Middle | 0.98 (0.82, 1.18) | 1.14 (1.00, 1.30) | 0.95 (0.81, 1.11) | 1.02 (0.92, 1.12) |
| Highest | 0.88 (0.71, 1.08) | 1.08 (0.96, 1.22) | 0.86 (0.73, 1.03) | 0.86 (0.75, 0.99) |
| Household permanent income quartile | ||||
| 1 (lowest; Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 0.96 (0.81, 1.15) | 1.16 (1.02, 1.31) | 1.00 (0.86, 1.16) | 1.16 (1.08, 1.24) |
| 3 | 0.92 (0.75, 1.14) | 1.30 (1.13, 1.49) | 0.96 (0.81, 1.14) | 1.17 (1.07, 1.28) |
| 4 (highest) | 0.76 (0.57, 1.01) | 1.49 (1.33, 1.67) | 0.83 (0.70, 0.98) | 1.28 (1.15, 1.43) |
| Self-rated health status | ||||
| Good or excellent (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Moderate | 1.17 (0.98, 1.39) | 1.01 (0.90, 1.14) | 1.15 (1.03, 1.30) | 1.20 (1.11, 1.30) |
| Bad or very bad | 1.58 (1.18, 2.11) | 1.19 (0.97, 1.46) | 1.26 (0.93, 1.69) | 1.20 (1.03, 1.40) |
| Level of difficulty moving around in past 30 d | ||||
| No or mild difficulty (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Moderate difficulty | 1.29 (1.06, 1.56) | 0.89 (0.75, 1.04) | 1.26 (1.04, 1.52) | 1.07 (0.93, 1.22) |
| Extreme or severe difficulty | 1.29 (0.90, 1.84) | 0.95 (0.76, 1.18) | 1.08 (0.82, 1.42) | 1.18 (1.01, 1.38) |
| Currently smokes any tobacco products | ||||
| No (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.18 (1.05, 1.33) | 0.77 (0.71, 0.84) | 1.40 (1.21, 1.61) | 0.83 (0.69, 1.01) |
| Country-level characteristics | ||||
| Per capita GDPc | 1.00 (0.90, 1.10) | 1.09 (1.02, 1.16) | 0.96 (0.87, 1.07) | 1.08 (1.01, 1.15) |
| Population in urban areas, %d | 0.85 (0.75, 0.96) | 1.15 (0.95, 1.17) | 0.92 (0.80, 1.06) | 1.00 (0.90, 1.10) |
| Foreign direct investment, % of GDPe | 1.00 (0.86, 1.16) | 0.99 (0.89, 1.10) | 0.95 (0.85, 1.06) | 0.96 (0.87, 1.05) |
| Mean tarifff | 0.87 (0.76, 1.00) | 1.11 (0.93, 1.33) | 0.86 (0.75, 0.99) | 1.10 (0.96, 1.26) |
Note. CI = confidence interval; GDP = gross domestic product; OR = odds ratio. The sample size was n = 100 454.
Centered at 18 years of age and divided into 10-year groups.
Separated, divorced, widowed, or cohabiting.
Mean centered and divided by $1000.
Mean centered and divided by 10%.
Standardized as a z score, with higher values reflecting greater foreign direct investment.
Standardized as a z score and reverse coded, with higher values reflecting greater openness to trade.
TABLE 4—
Multilevel Regression Model Results Showing Associations Between Individual- and Country-Level Characteristics and Odds of Underweight and Overweight Relative to Normal Weight Among Rural Men and Women: 40 Low- and Middle-Income Countries Included in the World Health Survey, 2002–2003
| Rural Men |
Rural Women |
|||
| Underweight vs Normal Weight, OR (95% CI) | Overweight vs Normal Weight, OR (95% CI) | Underweight vs Normal Weight, OR (95% CI) | Overweight vs Normal Weight, OR (95% CI) | |
| Individual-level characteristics | ||||
| Agea | 0.96 (0.91, 1.01) | 1.16 (1.09, 1.25) | 0.94 (0.89, 0.99) | 1.16 (1.09, 1.23) |
| Marital status | ||||
| Currently married (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Never married | 1.37 (1.18, 1.59) | 0.74 (0.61, 0.90) | 1.33 (1.17, 1.50) | 0.72 (0.59, 0.87) |
| Otherb | 1.00 (0.81, 1.25) | 1.11 (0.98, 1.27) | 0.98 (0.84, 1.15) | 0.96 (0.87, 1.05) |
| Educational attainment tertile | ||||
| Lowest (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Middle | 0.95 (0.81, 1.10) | 1.05 (0.92, 1.19) | 1.00 (0.87, 1.14) | 1.02 (0.89, 1.16) |
| Highest | 0.87 (0.75, 1.00) | 1.05 (0.92, 1.20) | 1.10 (0.94, 1.28) | 0.93 (0.80, 1.08) |
| Household permanent income quartile | ||||
| 1 (lowest; Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 0.95 (0.87, 1,02) | 1.14 (1.00, 1.29) | 0.92 (0.84, 1.01) | 1.12 (1.04, 1.21) |
| 3 | 0.84 (0.75, 0.95) | 1.16 (1.00, 1.35) | 0.84 (0.76, 0.93) | 1.22 (1.11, 1.33) |
| 4 (highest) | 0.76 (0.64, 0.90) | 1.46 (1.27, 1.69) | 0.69 (0.61, 0.80) | 1.30 (1.14, 1.50) |
| Self-rated health status | ||||
| Good or excellent (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Moderate | 1.13 (1.00, 1.27) | 1.03 (0.93, 1.15) | 1.07 (0.99, 1.16) | 1.06 (0.96, 1.16) |
| Bad or very bad | 1.33 (1.05, 1.68) | 1.10 (0.86, 1.41) | 1.13 (0.93, 1.36) | 1.13 (0.92, 1.39) |
| Level of difficulty moving around in past 30 d | ||||
| No or mild difficulty (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Moderate difficulty | 1.07 (0.92, 1.25) | 1.05 (0.88, 1.25) | 1.16 (0.99, 1.37) | 1.08 (0.93, 1.24) |
| Extreme or severe difficulty | 1.19 (0.96, 1.47) | 1.18 (0.94, 1.48) | 1.16 (0.94, 1.43) | 1.28 (1.07, 1.54) |
| Currently smokes any tobacco products | ||||
| No (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.13 (0.98, 1.31) | 0.76 (0.67, 0.87) | 1.23 (1.06, 1.44) | 0.76 (0.66, 0.88) |
| Country-level characteristics | ||||
| GDP per capitac | 0.97 (0.88, 1.08) | 1.10 (1.02, 1.18) | 1.01 (0.92, 1.10) | 1.12 (1.04, 1.19) |
| Population in urban areas, %d | 0.82 (0.74, 0.91) | 1.05 (0.91, 1.20) | 0.84 (0.73, 0.96) | 1.01 (0.88, 1.15) |
| Foreign direct investment, % of GDPe | 0.94 (0.81, 1.09) | 1.17 (1.02, 1.35) | 0.93 (0.83, 1.04) | 1.10 (0.95, 1.26) |
| Mean tarifff | 0.87 (0.76, 0.99) | 1.09 (0.87, 1.36) | 0.83 (0.71, 0.96) | 1.08 (0.87, 1.34) |
Note. CI = confidence interval; GDP = gross domestic product; OR = odds ratio. The sample size was n = 100 341.
Centered at 18 years of age and divided into 10-year groups.
Separated, divorced, widowed, or cohabiting.
Mean centered and divided by $1000.
Mean centered and divided by 10%.
Standardized as a z score, with higher values reflecting greater foreign direct investment.
Standardized as a z score and reverse coded, with higher values reflecting greater openness to trade.
At the country level, urbanization and trade liberalization were associated with lower odds of underweight relative to normal weight among adults living in urban and rural areas. For example, each 10–percentage-point increase in the proportion of urban residents per country was associated with 15% (95% CI = 0.75, 0.96) and 18% (95% CI = 0.74, 0.91) lower odds of underweight relative to normal weight among men in urban and rural areas, respectively. Similarly, a 1–standard-deviation increase in trade liberalization was associated with 14% (95% CI = 0.75, 0.99) and 17% (95% CI = 0.71, 0.96) lower odds of underweight relative to normal weight among women in urban and rural areas, respectively.
Per capita GDP was consistently associated with higher odds of overweight relative to normal weight among both urban and rural men and women, with the increased odds associated with a $1000 increase in GDP per capita ranging from 8% (95% CI = 1.01, 1.15) among urban women to 12% (95% CI = 1.04, 1.19) among rural women. In addition, a 1–standard-deviation increase in net FDI inflow as a percentage of GDP was associated with 17% (95% CI = 1.02, 1.35) higher odds of overweight relative to normal weight among rural men.
DISCUSSION
We used data from a sample of approximately 200 000 adults in 40 LMICs to test the associations between macrolevel economic characteristics hypothesized to drive changes in global patterns of diet and physical activity (i.e., economic development, urbanization, FDI, trade liberalization) and individual weight status. At the ecological level, economic development, urbanization, FDI, and trade liberalization were associated with higher mean BMIs among both men and women. After accounting for individual-level characteristics and measured compositional differences between countries in our multilevel regression models, we found that greater urbanization and trade openness were associated with a lower probability of underweight relative to normal weight, whereas economic development and FDI were associated with a higher probability of overweight.
Macrolevel Determinants of Weight Status
Neoliberal policies encouraging FDI and reduced barriers to trade are hypothesized to drive rapid transformations of the global food environment, particularly growth in unhealthy food and beverage commodities in LMICs and the attendant changes in nutritional status documented over the past 10 to 15 years.20,21,45,46 There is preliminary support for this hypothesis. Transnational food and drink companies have penetrated markets in middle-income countries.20,45 In addition, Stuckler et al. recently showed that the growth of per capita consumption of processed foods in LMICs has outpaced that of higher-income countries since 1997; furthermore, FDI was correlated with greater exposure to unhealthy food commodities in LMICs.20 Neoliberal policies may also have important influences on unemployment, wages, and poverty that in turn affect diet and physical activity patterns, although these effects are poorly understood and warrant further research.47
Nonetheless, few studies have considered whether macrolevel exposures, particularly those related to neoliberalization and greater market integration, are associated with variations in nutritional outcomes such as weight status. Consistent with prior ecological work,9,22 the results of our meta-regression analyses showed that levels of economic development and urbanization were positively associated with mean BMIs across countries. Our results also showed that average BMIs were higher in countries with greater FDI and fewer barriers to trade.
To assess whether macrolevel factors were related to individual weight status independently of compositional characteristics, we used multilevel regression models that controlled for country- and individual-level covariates. Our findings showed that macrolevel factors were associated with nutritional status variations in LMICs. Higher levels of urbanization and trade liberalization were associated with lower odds of underweight relative to normal weight among both urban and rural men and women. We corroborated previous findings17,18 by showing that economic development was associated with higher odds of overweight relative to normal weight. In addition, FDI was positively associated with the odds of overweight relative to normal weight among rural men, providing preliminary evidence that regulatory environments facilitating investments by foreign companies may adversely affect nutritional status in LMICs.
It is unclear why FDI was associated with overweight among rural but not urban residents. FDI may have a detrimental impact on rural residents because the influx of cheaper foods into a food system may endanger farming practices and alter patterns of consumption among rural residents.20 For example, qualitative evidence from Gambia suggests that the emergence of a “remittance economy” has driven the increase in obesity in rural areas by altering the goods sold at village shops and increasing the sale of vegetable oils, in particular, suggesting that FDI may influence patterns of consumption in rural areas.48
Longitudinal work assessing whether changes in economic development, urbanization, and FDI influence distributions of weight within countries is needed to identify causal effects of macrolevel factors on nutritional status. Furthermore, country-specific evidence suggests that the effects of macro-economic factors may vary across contexts. For instance, a shift in nutritional outcomes characterized by receding underweight and increasing overweight has not been observed in India, despite rapid economic growth,49 suggesting that the association between economic development and overweight or obesity is not universal. In addition, although research suggests that the North American Free Trade Agreement transformed food systems in Mexico, the growing presence of transnational food companies in the Brazilian market has, in part because of government legislation, not completely displaced traditional food systems.45,50
Individual-Level Determinants of Weight Status
Our multilevel regression models showed that marital, socioeconomic, and health status were the most important individual-level correlates of weight. Relative to being currently married, never having been married was positively associated with underweight and negatively associated with overweight relative to normal weight among men and women. These patterns may reflect sociocultural factors, including norms favoring a larger body size as a marker of health, beauty, or affluence; alternatively, they may reflect the absence of stigmatization of obesity51 or unmeasured marriage-related characteristics that are associated with weight.
With respect to SES, the seminal work of Sobal and Stunkard showed that, by contrast with high-income countries, the relation between SES and obesity in LMICs was positive for men and women.52 Recent work indicates that the burden of obesity may be shifting toward socioeconomically disadvantaged groups, although higher SES is still associated with overweight in the majority of LMICs.8,17,18 Consistent with recent cross-national evidence,53 we found that household income was associated with lower odds of underweight and higher odds of overweight relative to normal weight. The association between income and weight may reflect ownership of material goods and attendant behavioral changes (e.g., car ownership and reduced energy expenditures). However, it may also point to stress associated with culture change, long implicated as an important health determinant,54 as a contributor to body composition patterns in LMICs.55
By contrast with income, education was not associated with weight in our analyses, potentially reflecting the relatively more important role of the economic or material dimension of class in lower-income settings.56 However, income may mediate the effect of education on weight, and adjusting for both variables simultaneously may attenuate the direct effect of education. Our analyses showed nonlinearity in the association between health and weight. A U-shaped association between health status, disability, and body weight could reflect the reciprocal relation between health status and weight (i.e., decreased body weights are related to existing disease and increased disability and health problems among the overweight).57
Limitations
There were limitations to our analyses. First, we relied on self-reported height and weight. Prior research in developing contexts has shown minor deviations between self-reported and measured weights and concluded that self-reports are acceptably valid.58 Despite similar conclusions in the context of developed countries,59 other studies indicate underreporting of weight and overreporting of height.60 We found that our estimates of the prevalence of overweight were similar to measured estimates for some countries49,61 but that rates were potentially underestimated in others,62 although direct comparisons are complicated by differences in sampling, time periods, and sampling variability. Differential misclassification of weight status by levels of development, urbanization, FDI, or trade may have biased our estimates of the effects of macrolevel characteristics on patterns of underweight and overweight.
Second, we assumed that control for country- and individual-level compositional characteristics was sufficient to control for confounding between macrolevel economic characteristics and individual-level weight. However, important unmeasured characteristics could have biased our results. Third, one macrolevel characteristic may mediate the effect of another, and such temporal relations cannot be clarified with cross-sectional data. Longitudinal analyses are needed to identify the effects of a particular characteristic independently of other secular trends.
Conclusions
Our results suggest that multilevel economic factors, including SES and levels of trade liberalization, may be implicated in global shifts in epidemiological patterns of weight. Macro-economic factors may act as a double-edged sword, improving health in some situations and threatening it in others. Longitudinal investigations focusing on specific policies related to diet, physical activity, and weight represent a potentially fruitful area for future work.
Acknowledgments
We thank the Institute for Health Metrics and Evaluation for the estimates of permanent income used in our analyses.
Human Participant Protection
This study was approved by the institutional review board of McGill University; the study was based on secondary use of unidentifiable data.
References
- 1.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. 2006;84(2):289–298. doi: 10.1093/ajcn/84.1.289. [DOI] [PubMed] [Google Scholar]
- 4.Zheng W, McLerran DF, Rolland B et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364(8):719–729. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whitlock G, Lewington S, Sherliker P et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Popkin BM. The nutrition transition and its health implications in lower-income countries. Public Health Nutr. 1998;1(1):5–21. doi: 10.1079/phn19980004. [DOI] [PubMed] [Google Scholar]
- 7.Subramanyam MA, Kawachi I, Berkman LF, Subramanian SV. Socioeconomic inequalities in childhood undernutrition in India: analyzing trends between 1992 and 2005. PLoS One. 2010;5(6):e11392. doi: 10.1371/journal.pone.0011392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monteiro CA, Conde WL, Popkin BM. Income-specific trends in obesity in Brazil: 1975–2003. Am J Public Health. 2007;97(10):1808–1812. doi: 10.2105/AJPH.2006.099630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mendez MA, Monteiro CA, Popkin BM. Overweight exceeds underweight among women in most developing countries. Am J Clin Nutr. 2005;81(3):714–721. doi: 10.1093/ajcn/81.3.714. [DOI] [PubMed] [Google Scholar]
- 10.Kearney J. Food consumption trends and drivers. Philos Trans R Soc Lond B Biol Sci. 2010;365(1554):2793–2807. doi: 10.1098/rstb.2010.0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alexandratos N, editor. World Agriculture: Towards 2030/2050. Rome, Italy: United Nations Food and Agriculture Organization; 2006. [Google Scholar]
- 12.Wang Z, Zhai F, Zhang B, Popkin BM. Trends in Chinese snacking behaviors and patterns and the social-demographic role between 1991 and 2009. Asia Pac J Clin Nutr. 2012;21(2):253–262. [PMC free article] [PubMed] [Google Scholar]
- 13.Bell AC, Ge K, Popkin BM. The road to obesity or the path to prevention: motorized transportation and obesity in China. Obes Res. 2002;10(4):277–283. doi: 10.1038/oby.2002.38. [DOI] [PubMed] [Google Scholar]
- 14.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012;13(8):659–680. doi: 10.1111/j.1467-789X.2011.00982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93(suppl 1):S9–S30. doi: 10.1210/jc.2008-1595. [DOI] [PubMed] [Google Scholar]
- 16.Zhai F, Wang H, Du S et al. Lifespan nutrition and changing socio-economic conditions in China. Asia Pac J Clin Nutr. 2007;16(suppl 1):374–382. [PubMed] [Google Scholar]
- 17.Jones-Smith JC, Gordon-Larsen P, Siddiqi A, Popkin BM. Cross-national comparisons of time trends in overweight inequality by socioeconomic status among women using repeated cross-sectional surveys from 37 developing countries, 1989–2007. Am J Epidemiol. 2011;173(6):667–675. doi: 10.1093/aje/kwq428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones-Smith JC, Gordon-Larsen P, Siddiqi A, Popkin BM. Is the burden of overweight shifting to the poor across the globe? Time trends among women in 39 low- and middle-income countries (1991–2008) Int J Obes (Lond) 2012;36(8):1114–1120. doi: 10.1038/ijo.2011.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hawkes C. The role of foreign direct investment in the nutrition transition. Public Health Nutr. 2005;8(4):357–365. doi: 10.1079/phn2004706. [DOI] [PubMed] [Google Scholar]
- 20.Stuckler D, McKee M, Ebrahim S, Basu S. Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med. 2012;9(6):e1001235. doi: 10.1371/journal.pmed.1001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ezzati M, Vander Hoorn S, Lawes CM et al. Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med. 2005;2(5):e133. doi: 10.1371/journal.pmed.0020133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cassels S. Overweight in the Pacific: links between foreign dependence, global food trade, and obesity in the Federated States of Micronesia. Global Health. 2006;2:10. doi: 10.1186/1744-8603-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fleischer NL, Diez Roux AV, Alazraqui M, Spinelli H, De Maio F. Socioeconomic gradients in chronic disease risk factors in middle-income countries: evidence of effect modification by urbanicity in Argentina. Am J Public Health. 2011;101(2):294–301. doi: 10.2105/AJPH.2009.190165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guthold R, Ono T, Strong KL, Chatterji S, Morabia A. Worldwide variability in physical inactivity: a 51-country survey. Am J Prev Med. 2008;34(6):486–494. doi: 10.1016/j.amepre.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 26.Moore S, Hall JN, Harper S, Lynch JW. Global and national socioeconomic disparities in obesity, overweight, and underweight status. J Obes. 2010;2010:514674. doi: 10.1155/2010/514674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 28.Liu L, Yin X, Morrissey S. Global variability in diabetes mellitus and its association with body weight and primary healthcare support in 49 low- and middle-income developing countries. Diabet Med. 2012;29(8):995–1002. doi: 10.1111/j.1464-5491.2011.03549.x. [DOI] [PubMed] [Google Scholar]
- 29.Ayuso-Mateos JL, Nuevo R, Verdes E, Naidoo N, Chatterji S. From depressive symptoms to depressive disorders: the relevance of thresholds. Br J Psychiatry. 2010;196(5):365–371. doi: 10.1192/bjp.bp.109.071191. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization. Health statistics and health information systems: World Health Survey. Available at: http://www.who.int/healthinfo/survey/en. Accessed September 18, 2013.
- 31.Ustun B, Chatterji S, Mechbal A, Murray CJ. The World Health Surveys. In: Murray CJ, Evans DB, editors. Health Systems Performance Assessment: Debates, Methods and Empiricism. Geneva, Switzerland: World Health Organization; 2003. pp. 797–808. [Google Scholar]
- 32.World Health Organization. Global database on body mass index: BMI classification. Available at: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed September 18, 2013.
- 33.Ferguson BD, Tandon A, Gakidou E, Murray CJ. Estimating permanent income using indicator variables. In: Murray CJ, Evans DB, editors. Health Systems Performance Assessment: Debates, Methods and Empiricism. Geneva, Switzerland: World Health Organization; 2003. pp. 747–760. [Google Scholar]
- 34.Harper S, McKinnon B. Global socioeconomic inequalities in tobacco use: internationally comparable estimates from the World Health Surveys. Cancer Causes Control. 2012;23(suppl 1):11–25. doi: 10.1007/s10552-012-9901-5. [DOI] [PubMed] [Google Scholar]
- 35.McKinnon B, Harper S, Moore S. Decomposing income-related inequality in cervical screening in 67 countries. Int J Public Health. 2011;56(2):139–152. doi: 10.1007/s00038-010-0224-6. [DOI] [PubMed] [Google Scholar]
- 36.Gakidou E, Oza S, Vidal Fuertes C et al. Improving child survival through environmental and nutritional interventions: the importance of targeting interventions toward the poor. JAMA. 2007;298(16):1876–1887. doi: 10.1001/jama.298.16.1876. [DOI] [PubMed] [Google Scholar]
- 37.World Bank. World development indicators. Available at: http://data.worldbank.org/data-catalog/world-development-indicators. Accessed September 18, 2013.
- 38.Borensztein E, De Gregorio J, Lee J- W. How does foreign direct investment affect economic growth? J Int Econ. 1998;45(1):115–135. [Google Scholar]
- 39.Wacziarg R, Welch KH. Trade liberalization and growth: new evidence. World Bank Econ Rev. 2008;22(2):187–231. [Google Scholar]
- 40.Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- 41.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- 42.Honaker J, King G. What to do about missing values in time-series cross-section data. Am J Pol Sci. 2010;54(2):561–581. [Google Scholar]
- 43.Honaker J, King G, Blackwell M. Amelia II: a program for missing data. Available at: http://www.jstatsoft.org/v45/i07/paper. Accessed September 18, 2013.
- 44.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1–48. [Google Scholar]
- 45.Monteiro CA, Cannon G. The impact of transnational “big food” companies on the South: a view from Brazil. PLoS Med. 2012;9(7):e1001252. doi: 10.1371/journal.pmed.1001252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hawkes C. Uneven dietary development: linking the policies and processes of globalization with the nutrition transition, obesity and diet-related chronic diseases. Global Health. 2006;2:4. doi: 10.1186/1744-8603-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Winters LA, McCulloch N, McKay A. Trade liberalization and poverty: the evidence so far. J Econ Lit. 2004;42(1):72–115. [Google Scholar]
- 48.Prentice AM. The emerging epidemic of obesity in developing countries. Int J Epidemiol. 2006;35(1):93–99. doi: 10.1093/ije/dyi272. [DOI] [PubMed] [Google Scholar]
- 49.Subramanian SV, Perkins JM, Khan KT. Do burdens of underweight and overweight coexist among lower socioeconomic groups in India? Am J Clin Nutr. 2009;90(2):369–376. doi: 10.3945/ajcn.2009.27487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Clark SE, Hawkes C, Murphy SM, Hansen-Kuhn KA, Wallinga D. Exporting obesity: US farm and trade policy and the transformation of the Mexican consumer food environment. Int J Occup Environ Health. 2012;18(1):53–65. doi: 10.1179/1077352512Z.0000000007. [DOI] [PubMed] [Google Scholar]
- 51.Siervo M, Grey P, Nyan OA, Prentice AM. A pilot study on body image, attractiveness and body size in Gambians living in an urban community. Eat Weight Disord. 2006;11(2):100–109. doi: 10.1007/BF03327758. [DOI] [PubMed] [Google Scholar]
- 52.Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989;105(2):260–275. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- 53.Subramanian SV, Perkins JM, Ozaltin E, Davey Smith G. Weight of nations: a socioeconomic analysis of women in low- to middle-income countries. Am J Clin Nutr. 2011;93(2):413–421. doi: 10.3945/ajcn.110.004820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cassel JC, Patrick R, Jenkins D. Epidemiological analysis of the health consequences of culture change. Ann N Y Acad Sci. 1960;84:938–949. doi: 10.1111/j.1749-6632.1960.tb39126.x. [DOI] [PubMed] [Google Scholar]
- 55.Reyes-Garcia V, Gravlee CC, McDade TW, Huanca T, Leonard WR, Tanner S. Cultural consonance and body morphology: estimates with longitudinal data from an Amazonian society. Am J Phys Anthropol. 2010;143(2):167–174. doi: 10.1002/ajpa.21303. [DOI] [PubMed] [Google Scholar]
- 56.McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29(1):29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- 57.Mansson NO, Eriksson KF, Israelsson B, Ranstam J, Melander A, Rastam L. Body mass index and disability pension in middle-aged men—non-linear relations. Int J Epidemiol. 1996;25(1):80–85. doi: 10.1093/ije/25.1.80. [DOI] [PubMed] [Google Scholar]
- 58.Avila-Funes JA, Gutierrez-Robledo LM, Ponce De Leon Rosales S. Validity of height and weight self-report in Mexican adults: results from the National Health and Aging Study. J Nutr Health Aging. 2004;8(5):355–361. [PubMed] [Google Scholar]
- 59.Lee DH, Shin A, Kim J, Yoo KY, Sung J. Validity of self-reported height and weight in a Korean population. J Epidemiol. 2011;21(1):30–36. doi: 10.2188/jea.JE20100058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gorber SC, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8(4):307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 61.Ismail MN, Chee SS, Nawawi H, Yusoff K, Lim TO, James WP. Obesity in Malaysia. Obes Rev. 2002;3(3):203–208. doi: 10.1046/j.1467-789x.2002.00074.x. [DOI] [PubMed] [Google Scholar]
- 62.Jahns L, Baturin A, Popkin BM. Obesity, diet, and poverty: trends in the Russian transition to market economy. Eur J Clin Nutr. 2003;57(10):1295–1302. doi: 10.1038/sj.ejcn.1601691. [DOI] [PubMed] [Google Scholar]