Abstract
Objectives. To inform public health efforts to promote independent functioning among older adults, we have provided new national estimates of late-life disability that explicitly recognize behavioral adaptations.
Methods. We analyzed the 2011 National Health and Aging Trends Study, a study of Medicare enrollees aged 65 years and older (n = 8077). For 7 mobility and self-care activities we identified 5 hierarchical stages—fully able, successful accommodation with devices, activity reduction, difficulty despite accommodations, and receipt of help—and explored disparities and associations with quality of life measures.
Results. Among older adults, 31% were fully able to complete self-care and mobility activities. The remaining groups successfully accommodated with devices (25%), reduced their activities (6%), reported difficulty despite accommodations (18%), or received help (21%). With successive stages, physical and cognitive capacity decreased and symptoms and multimorbidity increased. Successful accommodation was associated with maintaining participation in valued activities and high well-being, but substantial disparities by race, ethnicity, and income existed.
Conclusions. Increased public health attention to behavioral adaptations to functional change can promote independence for older adults and may enhance quality of life.
An unprecedented number of adults in the United States will reach late life over the next few decades. The US Census Bureau projects that by 2030 the number of older Americans will exceed 70 million (20% of the population),1 and the vast majority of these individuals will be living with multiple chronic conditions.2 The risks of disability increase markedly with age and chronic illness, which in turn has consequences for older adults’ quality of life.3 Although late-life disability prevalence declined over the past quarter century, recent studies suggest such improvements have paused and may reverse course as the baby boom generation enters old age.4–6 Significantly higher rates among disadvantaged groups also remain a concern.7
Consequently, late-life disability remains a prominent public health matter8 and maintaining the ability of older adults to function independently in the community an important goal.9 Self-care and mobility activities—although not the only targets of functional preservation—have long been recognized as essential to older adults’ well-being and to their continued social and community participation and thus are of particular interest. Public health professionals play a unique role in addressing late-life disability by setting and monitoring population-level goals, designing needs assessments for communities, developing programs and policies to maximize functioning, providing information to older adults and their caregivers, and focusing on gaps for high-risk groups (e.g., minority, low-income populations).10
With respect to public health monitoring, for example, Healthy People 2020 has targeted a 10% reduction nationally (from a baseline level of 29%) in the proportion of older adults with moderate to severe limitations in daily functioning. The Federal Interagency Forum on Aging Statistics and the Centers for Disease and Control and Prevention also track late-life disability (the latter at the state level), and community needs assessments to promote aging preparedness have included such measures (at the local level).11–13 Specific measurement approaches vary. Healthy People 2020, for instance, tracks the proportion of older adults who report having difficulty by themselves and without special equipment performing basic activities of daily living (bathing or showering, dressing, eating, getting in or out of bed or chairs, walking, or using the toilet). The Centers for Disease and Control and Prevention tracks those who either are limited in their activities or use special equipment because of a health problem. Other programs focus on needing help from another person with daily activities.
A common feature of these monitoring efforts is that they do not permit distinctions according to how older adults carry out daily activities. For instance, the approaches do not allow identification of individuals who have successfully accommodated difficulties by using aids such as walkers and grab bars, which older adults are increasingly adopting to foster independent functioning.14,15 They also miss altogether individuals who adjust their behavior without recognizing difficulty, for instance by dressing or walking less often (so-called preclinical disability16,17), an at-risk group for whom intervention may delay or deter the need for hands-on care. Hence, current efforts overlook valuable opportunities for assessing public health needs and evaluating program impacts related to independent functioning.
To better address the extent to which public health efforts can improve the lives of older adults, a fuller spectrum of functional assessment is needed. Using a new national survey of Medicare beneficiaries, we have introduced a 5-category hierarchy of late-life mobility and self-care limitations. We have identified those who
are fully able;
have successfully accommodated declines by using assistive technology or environmental features;
have reduced their activity frequency but report no difficulty;
report difficulty doing activities by themselves, even when using any accommodations they have in place; and
receive assistance from another person.
We demonstrate how underlying physical and cognitive capacity and reports of multimorbidity vary by each successive category and provide estimates of disparities for key demographic groups. Finally, recognizing the importance of integrating measures of participation and quality of life into studies of disability,18 we examine connections of the new hierarchy we have developed to 2 such indicators: participation restrictions and subjective well-being. We focus our discussion on the implications of our findings for public health practice and for tracking population-level care needs.
METHODS
Data are from the first (2011) round of the National Health and Aging Trends Study (NHATS). The NHATS drew a sample of adults aged 65 years and older from individuals in the Medicare enrollment file living in the contiguous United States on September 30, 2010, with oversamples by age and for Black, non-Hispanic individuals. The enrollment file represents 96% of all older adults in the United States; the 4% not represented include individuals who were born in another country and never qualified for benefits and those who remain on employment-related benefits (most of whom are aged 65–69 years).
The NHATS conducted interviews from May through November 2011 (71% response rate). The sample size for this analysis was 8077 persons, of whom 468 were nursing home residents. Analytic weights adjusted for differential nonresponse and produced national prevalence estimates.19 We generated Medicare population estimates (totaling 38.1 million) by applying estimates of age-specific prevalence to enrollment file totals by age when the sample was drawn.
In-person interviews, conducted in settings other than nursing homes (n = 7609), collected detailed self-reported information on participants’ physical capacity, how participants carry out activities of daily life, and their social, physical, and technological environment. Physical and cognitive performance batteries provided complementary measures of participants’ capacity, and additional survey questions elicited self-reported information on various topics including chronic health conditions, economic status, participation restrictions, and subjective well-being. The NHATS interviewed proxy respondents when the sample person could not respond (n = 583).20
Mobility and Self-Care Disability
The NHATS reengineered the classic activities of daily living measures.21 For each activity (going outside, getting around inside, getting out of bed, eating, getting cleaned up, using the toilet, and dressing), participants first reported their use of devices or environmental modifications (canes, walkers, wheelchairs, scooters, grab bars, bath or shower seat, eating and dressing devices) and help from another person during the previous month. Respondents who ever performed the activity without help then reported about difficulty they had in the last month when doing the activity alone (with the particular devices or environmental features named earlier, if used). For activities other than getting out of bed, toileting, and eating, participants also reported about changes in the last year in the frequency with which they performed the activity.
From these measures we created 5 hierarchical categories for each activity:
no device use, reduction in activities, difficulty, or assistance (fully able);
device use but no reduction in activities, difficulty, or assistance (successful accommodation);
reductions in activities but no difficulty or assistance (reduced activities);
difficulty performing activities (by oneself, when using devices, if used) but no assistance (difficulty); and
assistance from another person or, rarely, not doing the particular activity (assistance).
We created a summary measure indicating the lowest level of functioning across all 7 activities. For the summary measure, we combined nursing home residents with the assistance group and considered only nonmissing cases (99.6% or more for each activity). All 7 activities have statistical properties that suggest they belong in the scale (α = 0.93), and a validation study demonstrated that similar hierarchies have acceptable test–retest reliability over a 2- to 4-week period.22
Physical and Cognitive Capacity Measures and Multimorbidity
The NHATS Physical Capacity Scale (0–12; α = 0.88) builds on the traditional Nagi framework but measures greater as well as more limited functioning.23 Questions assessed ability in the last month to carry out the following validated pairs of activities without devices or help from another person: walk 6 blocks and 3 blocks, walk up 20 stairs and 10 stairs, lift and carry 20 pounds and 10 pounds, kneel down and bend over (without holding on to anyone or anything), put a heavy object on a shelf overhead and reach up over head, and open a sealed jar using hands only and grasp small objects.23 Participants who reported they were able to do the first (more difficult) activity in each pair skipped the follow-up item. We gave participants 1 point if they could carry out only the easier task and 2 points for the more challenging task.
We also developed a self-reported symptom scale (0–12; α = 0.81) that measured pain; exhaustion; breathing problems; limited strength or movement in shoulders, arms, or hands; limited strength or movement in hips, legs, knees, or feet; and balance or coordination problems.3 Individuals received 1 point if they experienced the symptom in the last month and 2 points if it limited their activities.
The NHATS also included several established physical performance measures: a 3-meter usual walking speed test, 5 balance tests, rapid chair stands, grip strength using a handheld dynamometer, and peak airflow. Following prior studies,24 we combined usual walking speed, balance tests, and rapid chair stands into the Short Physical Performance Battery (SPPB; range = 0–12). For each test, we used quartiles to assign values 1 to 4, and we assigned 0 to individuals meeting exclusion criteria related to functioning, unable to complete a test, or not attempting it for safety reasons. We followed similar procedures for coding grip strength (range = 0–4) and peak airflow (range = 0–4).25
We imputed missing scores for the physical performance measures (5%–10% for components and 13% for the SPPB) multiple times (K = 10) based on age, gender, race/ethnicity, proxy status, place of residence, physical capacity, and symptom scores.26 The means we have reported by disability level are nearly identical to those with missing cases omitted. The regression-based t test, establishing the hierarchy of the disability spectrum, took into account both sampling variation and imputation uncertainty.
The NHATS measured memory through a 10-word recall test. Interviewers read a randomly assigned list of nouns to respondents at 2-second intervals.27 They then asked participants to recall as many words as possible, in any order, in up to 2 minutes (immediate recall) and again after a brief interval (delayed recall). For the 7% of participants with missing cognition scores, we performed multiple imputations using the strategy we have described for physical performance measures.
We created a count of chronic conditions (0–13) to reflect multimorbidity. We included history of a heart attack, heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, stroke, Alzheimer’s disease or dementia, cancer (excluding skin), a broken or fractured hip, and current symptoms of depression and generalized anxiety (from the validated Patient Health Questionnaire-428,29).
Race/Ethnicity and Income
The NHATS confirmed age and gender with participants. Respondents or proxies reported race using 8 categories (White, Black, American Indian, Alaskan Native, Asian, Native Hawaiian, Pacific Islander, and other); those giving multiple responses also identified a primary race. The NHATS also asked whether participants considered themselves Hispanic or Latino. We classified responses into White non-Hispanic, Black non-Hispanic, Hispanic, and all other (including unknown). The last category consists mainly of respondents identifying as Asian.
The NHATS obtained information about the income that the sampled person (and spouse or partner, if applicable) received from major sources including Social Security; Supplemental Security Income; Veteran’s Administration income; pension plans; earned income; interest or dividend income from mutual funds or stocks, bonds, bank accounts, or CDs (certificates of deposit); and retirement account withdrawals. After determining which sources of income the respondent (and spouse or partner) had, interviewers asked respondents to report amounts, offering bracketed ranges to those who did not know or refused. A final item asked about total income from all sources with a bracketed range again offered as needed. We used the imputed total income value provided on the NHATS public use file, which filled in missing values for 13% of individuals within a reported bracketed value and 31% within an imputed bracketed value.30 We constructed quartiles with cutpoints at $15 000, $30 000, and $60 000.
Participation Restrictions and Subjective Well-Being
We constructed a dichotomous indicator of participation restrictions that takes into account individual preferences for different types of activities. For visiting in person with friends or family; attending religious services; participating in clubs, classes, or other organized activities; and going out for enjoyment, if the sample persons valued the activity (a lot or somewhat) and their health or functioning kept them from doing the activity in the last month, we considered them to have a participation restriction. We also considered those who reported that their health or functioning kept them from working, volunteering, or carrying out their favorite activity to have a restriction.
For self-respondents (n = 7026) we created a scale of subjective well-being (0–22; α = 0.74) from 4 items reflecting positive and negative emotions (frequency from every day to never in the last month of feeling cheerful, bored, full of life, or upset) and 3 reflecting self-realization (extent of disagreement with statements about purpose in life, self-acceptance, and environmental mastery).31 Factor analysis confirmed that these items formed 1 factor with loadings 0.47 or higher. (An additional item about personal growth did not scale with the others, and we therefore omitted it.) We imputed cases with missing values (< 2%) according to the procedure we have described and reverse-coded items as necessary so that 0 indicated low well-being.
RESULTS
Among the 38.1 million older adults enrolled in Medicare, only 12.0 million (31.0%) were fully able (without accommodation, difficulty, or help) to carry out all self-care and mobility activities (Table 1). More than 9.0 million (24.5%) had successfully accommodated and another 9.1 million either had reduced their activity level but did not report difficulty (2.1 million; 5.6%) or had difficulty carrying out activities alone (7.0 million; 18.4%). The remaining 7.7 million (20.5%) had received assistance in the last month with at least 1 task (including 1.1 million nursing home residents).
TABLE 1—
Percentage and Number of Medicare Beneficiaries in Each Stage of the Late-Life Disability Spectrum and Percentage by Activity: National Health and Aging Trends Study, United States, 2011
| Summary Across Activities |
|||||||||
| Level | % (95% CI) | No. (in Millions) | Going Outside, % (95% CI) | Getting Around Inside, % (95% CI) | Getting out of Bed, % (95% CI) | Eating, % (95% CI) | Bathing, % (95% CI) | Toileting, % (95% CI) | Dressing, % (95% CI) |
| Fully able | 31.0 (29.9, 32.1) | 12.0 | 64.1 (62.8, 65.4) | 69.0 (67.9, 70.0) | 74.2 (73.1, 75.3) | 90.0 (89.3, 90.7) | 53.8 (52.5, 55.1) | 57.2 (55.8, 58.5) | 77.5 (76.5, 78.5) |
| Successful accommodation | 24.5 (23.5, 25.5) | 9.3 | 6.8 (6.2, 7.4) | 7.2 (6.6, 7.9) | 3.8 (3.2, 4.3) | 0.3 (0.2, 0.4) | 25.4 (24.3, 26.6) | 31.0 (29.5, 32.6) | 1.0 (0.8, 1.2) |
| Activity reduction | 5.6 (5.0, 6.3) | 2.1 | 7.0 (6.3, 7.9) | 2.8 (2.4, 3.2) | … | … | 2.4 (2.0, 2.9) | … | 1.2 (1.0, 1.6) |
| Difficulty (by oneself, with accommodations, if used) | 18.4 (17.4, 19.5) | 7.0 | 7.7 (6.9, 8.5) | 10.9 (10.2, 11.6) | 14.0 (13.3, 14.9) | 2.7 (2.3, 3.1) | 7.5 (6.8, 8.2) | 5.4 (4.8, 6.0) | 7.2 (6.6, 7.8) |
| Assistance from others | 20.5 (19.6, 21.4) | 7.7 | 11.3 (10.5, 12.1) | 6.7 (6.2, 7.4) | 4.8 (4.4, 5.4) | 4.0 (3.5, 4.5) | 7.6 (7.0, 8.2) | 3.1 (2.7, 3.6) | 9.9 (9.4, 10.6) |
| Nursing home | … | … | 3.0 (2.7, 3.3) | 3.0 (2.7, 3.3) | 3.0 (2.7, 3.3) | 3.0 (2.7, 3.3) | 3.0 (2.7, 3.3) | 3.0 (2.7, 3.3) | 3.0 (2.7, 3.3) |
| Missing | … | … | 0.1 (0.0, 0.2) | 0.4 (0.3, 0.6) | 0.2 (0.1, 0.3) | 0.0 (0.0, 0.2) | 0.3 (0.2, 0.5) | 0.3 (0.2, 0.6) | 0.2 (0.0, 0.3) |
| Total | 100.0 | 38.1 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
Note. CI = confidence interval. The sample (n = 8077) represents the aged Medicare population.
The distribution of older adults across this spectrum varied by activity (Table 1). For instance, 90.0% of older adults were fully able to eat by themselves, whereas only 53.8% of older adults were fully able to bathe by themselves. Successful accommodation was highest for bathing and toileting (most often using grab bars, bath seats, and raised toilet seats; data not shown) and lowest for eating and dressing. Having reduced activity was most common for going outside (7.0%), whereas difficulty was highest for getting out of bed (14.0%) and assistance most common for going outside (11.3%) and dressing (9.9%).
The categories in the proposed spectrum were hierarchical and largely distinct (Table 2). Mean mobility performance (SPPB) scores, for instance, fell progressively with each successive category, ranging from 8.6 (of 12.0) for those in the fully able category to less than 3.0 for the group who received assistance. SPPB components followed this pattern, as did grip strength, peak airflow, memory tests, and self-reported measures of physical capacity, symptoms, and multimorbidity. Within the intermediate categories, distinctions were statistically significant for the SPPB, walking speed, and self-reported measures. Moreover, those who limited their activities had similar balance and chair rise scores to those who successfully accommodated, and similar strength and cognitive capacity scores to those who reported difficulty, suggesting the category was appropriately placed.
TABLE 2—
Physical and Cognitive Capacity Scores and Number of Chronic Conditions by Stage in the Late-Life Disability Spectrum: National Health and Aging Trends Study, United States, 2011
| Test or Scale (Range) |
||||||||||||
| Level | SPPB (0–12), Mean | Usual Walking Speed (0–4), Mean | Rapid Chair Stands (0–4), Mean | Balance Stands (0–4), Mean | Grip Strength (0–4), Mean | Peak Airflow (0–4), Mean | Immediate Word Recall (0–10), Mean | Delayed Word Recall (0–10), Mean | Physical Capacity (0–12), Mean | Symptoms (12–0), Mean | Chronic Conditions (0–13), Mean | |
| Fully able | 8.6* | 2.9* | 2.7* | 3.0* | 2.8* | 2.8* | 5.2* | 3.9* | 11.3* | 1.5* | 1.9* | |
| Successful accommodation | 7.2* | 2.5* | 2.2 | 2.5 | 2.3* | 2.5* | 5.0* | 3.6* | 10.1* | 2.2* | 2.4* | |
| Activity reduction | 6.7* | 2.2* | 2.1* | 2.4* | 2.1 | 2.2 | 4.6 | 3.1 | 9.2* | 3.3* | 2.7* | |
| Difficulty (by oneself, with accommodations, if used) | 5.6* | 2.0* | 1.5* | 2.1* | 1.9* | 2.2* | 4.6* | 3.3* | 7.9* | 5.3* | 3.2* | |
| Assistance from others | 2.7 | 1.0 | 0.7 | 1.0 | 1.3 | 1.6 | 3.2 | 2.2 | 4.2 | 6.5 | 4.1 | |
Note. SPPB = Short Physical Performance Battery. The sample (n = 7609) represents the aged non–nursing home-based Medicare population.
*P < .01 for test of difference from next (lower) functioning group.
The proportion of the population that fell into each stage of the spectrum shifted dramatically with age (Table 3; χ2 = 876.5; P < .001). For instance, about 44.6% of individuals aged 65 to 69 years were fully able to carry out mobility and self-care activities independently, whereas only 4.0% of those aged 90 years or older did so, consistent with a linear decline. By contrast, the percentage who received assistance increased exponentially from 11.0% among those aged 65 to 69 years to nearly 61.7% among those aged 90 years or older. Two of the intermediate groups showed a pattern of gradual increase with age, peaking among those aged 75 to 84 years for successful accommodation and among those aged 80 to 84 years for difficulty despite accommodations, before declining at older ages. Reductions in activity were relatively rare across all age groups (4.5%–7.0%).
TABLE 3—
Stage in the Late-Life Disability Spectrum by Age, Gender, Race, and Income Quartiles: National Health and Aging Trends Study, United States, 2011
| Characteristic | No. | Fully Able | Successful Accommodation | Activity Reduction | Difficulty (by Oneself, With Accommodations if Used) | Assistance From Others | Total | χ2, P |
| Age, y | 876.5, < .001 | |||||||
| 65–69 | 1417 | 44.6 | 22.4 | 4.9 | 17.1 | 11.0 | 100.0 | |
| 70–74 | 1610 | 39.0 | 24.4 | 6.0 | 17.7 | 12.9 | 100.0 | |
| 75–79 | 1569 | 27.4 | 29.2 | 6.2 | 19.1 | 18.1 | 100.0 | |
| 80–84 | 1590 | 19.7 | 27.1 | 5.3 | 21.8 | 26.1 | 100.0 | |
| 85–89 | 1067 | 10.2 | 21.8 | 7.0 | 19.2 | 41.8 | 100.0 | |
| ≥ 90 | 824 | 4.0 | 15.2 | 4.5 | 14.6 | 61.7 | 100.0 | |
| Gender | 271.9, < .001 | |||||||
| Male | 3285 | 40.0 | 22.5 | 4.8 | 18.0 | 14.7 | 100.0 | |
| Female | 4792 | 24.3 | 26.0 | 6.2 | 18.7 | 24.8 | 100.0 | |
| Race/ethnicity | 146.5, < .001 | |||||||
| White, non-Hispanic | 5498 | 31.4 | 26.4 | 5.1 | 18.3 | 18.9 | 100.0 | |
| Black, non-Hispanic | 1788 | 27.0 | 17.7 | 7.4 | 20.8 | 27.2 | 100.0 | |
| Hispanic | 471 | 27.3 | 13.0 | 9.2 | 18.0 | 32.5 | 100.0 | |
| Other | 320 | 37.3 | 20.5 | 6.3 | 16.9 | 19.0 | 100.0 | |
| Income quartile, $ | 581.8, < .001 | |||||||
| Lowest (< 15 000) | 2229 | 22.6 | 19.2 | 7.4 | 20.8 | 30.1 | 100.0 | |
| Second (15 000– < 30 000) | 1968 | 25.2 | 23.4 | 7.4 | 22.5 | 21.6 | 100.0 | |
| Third (30 000– < 60 000) | 1891 | 34.2 | 29.4 | 5.0 | 18.6 | 12.8 | 100.0 | |
| Highest (≥ 60 000) | 1521 | 45.0 | 28.3 | 3.7 | 14.3 | 8.8 | 100.0 |
Note. The sample for age, gender, and race/ethnicity (n = 8077) represents the aged Medicare population, and the sample for income quartiles (n = 7609) represents the aged non–nursing home-based Medicare population.
Only 24.3% of older women, compared with 40.0% of men, were fully able to carry out activities. They were also more likely than were men both to receive assistance (24.8% vs 14.7%) and to successfully accommodate (26.0% vs 22.5%). Blacks and Hispanics, but not other minorities (who are mostly Asian), and those in the 2 lowest income quartiles were much less likely than were others to be fully able or to successfully accommodate but were more likely to reduce their activity level, report difficulty (Blacks), and receive assistance.
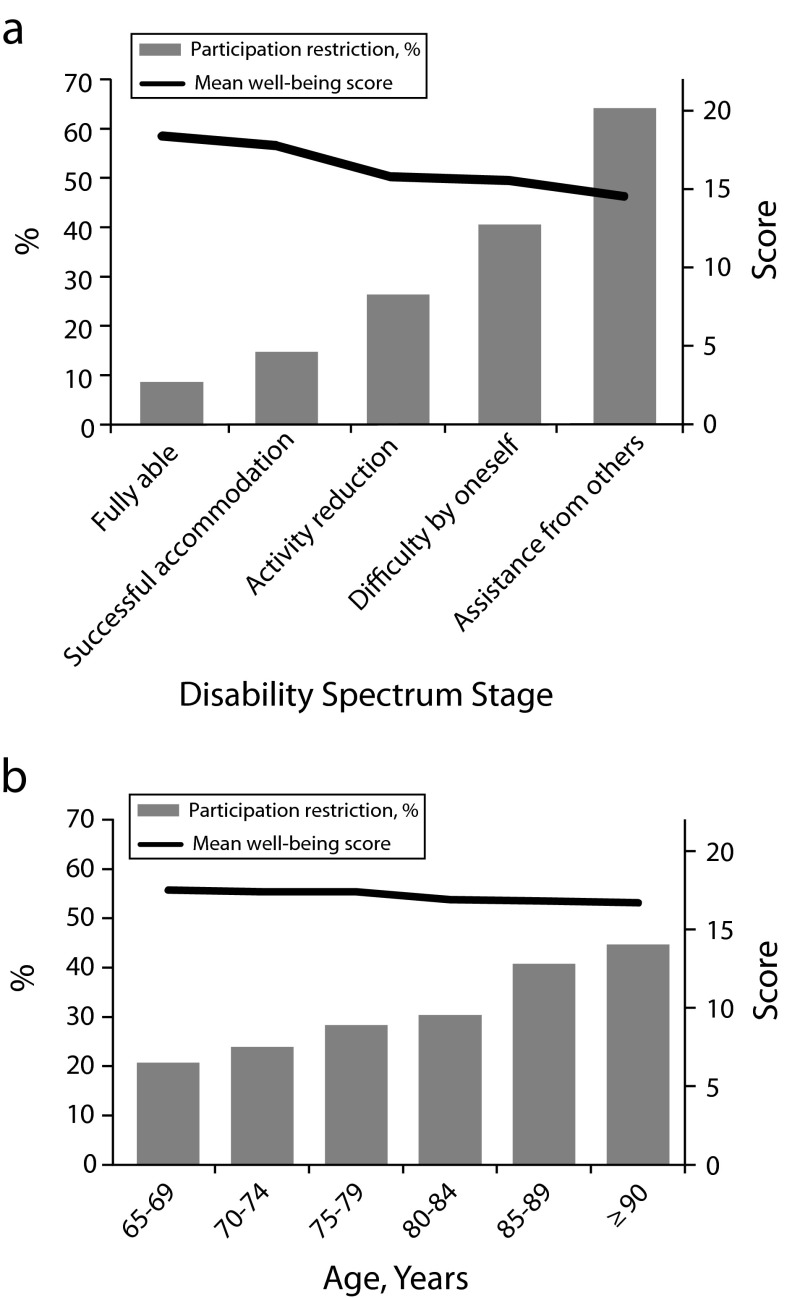
As shown in Figure 1a, the proposed spectrum had a strong relationship with both participation restrictions (bars; P < .001) and mean well-being (line; P < .001) scores. For instance, only 9% of those fully able to carry out mobility and self-care activities had a participation restriction, and at the other end of the spectrum, 64% of those who received help with such tasks were restricted. These relationships did not simply reflect age; to the contrary, patterns were much flatter when examined by 5-year age groups (Figure 1b). Moreover, models including both limitation and age categories (not shown) demonstrated significant relationships with these outcomes only for limitations.
FIGURE 1—
Percentage of older adults with participation restrictions and mean well-being scores by (a) stage in the late-life disability spectrum and (b) age: National Health and Aging Trends Study, United States, 2011.
Note that those who had successfully accommodated reported only modestly higher rates of participation restrictions than did those who were fully able (14.7% vs 8.7%) and similar well-being scores (18.0 vs 18.4).
DISCUSSION
We have provided new national estimates of self-care and mobility limitations among older adults along a spectrum that incorporates adaptation to functional decline. Our findings suggest that one third of the population aged 65 years and older are fully able to carry out self-care and mobility activities, half are managing without assistance to varying degrees of success, and the remaining fifth receive assistance from another person with mobility or some aspect of self-care. Importantly, for the first time, to our knowledge, with national data we have been able to distinguish 3 groups—amounting to nearly half the older population—who are not fully able but are managing without assistance. Previous national studies,4 which yield estimates of difficulty without help or special equipment of 20% to 27% for older adults living in the community and up to 29% if the institutional population is included appear to miss a substantial fraction of this group. Moreover, we have demonstrated associations with participation and well-being that are independent of age.
A limitation of our study is its cross-sectional perspective. However, as future rounds of the NHATS become available, the investigation of individual pathways through the proposed spectrum as well as determinants and consequences of distinct pathways will be possible. In addition, although we have demonstrated descriptive associations among disability, participation restrictions, and subjective well-being, further investigation into the extent and nature of causal connections is needed.
Nevertheless, the proposed hierarchy may be helpful for developing, targeting, and evaluating the effectiveness of public health policies and programs to curb disability and its negative consequences in late life. Two groups not previously discernible may be especially important targets for public health interventions—the 7.0 million older adults who have difficulty carrying out activities alone with whatever accommodations they have already made and the additional 2.1 million who have reduced their activity level but do not experience or acknowledge difficulty. Identification of these individuals opens up the possibility of intervening to fortify individuals’ capacity to carry out these basic activities (e.g., through strength or endurance programs designed to avert deconditioning) and, in cases where restoration of capacity is not possible, to encourage safe and independent use of accommodations (e.g., through home environment or assistive technology programs).
The 9 million older individuals identified as successfully accommodating mobility or self-care activities are also a new group of special interest. Among the activities included here, toileting and bathing were most often successfully accommodated, typically through the use of grab bars and other simple environmental features such as raised toilet seats and bath or shower seats. Such features may accommodate underlying declines in capacity and also prevent progression if they avert, for example, debilitating falls.
Findings suggest that those who are Black or Hispanic and have a low income may be most important to target with interventions promoting successful accommodation. Communities where minority and low-income groups are prevalent may be especially fruitful targets for programs that promote home modification and identification of assistive devices suited to the individual’s needs and capacities. Notably the use of technological approaches to address functional decline is not associated with substantially reduced quality of life; to the contrary, adults who successfully accommodate seem on average to have levels of participation and subjective well-being close to those of persons who are fully able. Future research should investigate whether interventions that foster successful accommodation, particularly among minority groups and past the peak ages of 75 to 84 years, yield payoff not only for independent functioning but also for continued participation and well-being into very late life.
Finally, our analysis has implications for tracking and interpreting population-level trends in late-life disability prevalence. After many years of steady decline, the United States has experienced a plateau in late-life disability prevalence, and recent studies portend a possible reversal in direction.4–6 Medical and public health advances are thought to be partly responsible for declines before 2000,32 but researchers have not been able to discern whether more older adults are reaching late life fully able to carry out daily activities or are better able to accommodate deficits in capacity. Reasons for the recent leveling off are equally unclear. As the NHATS continues to track the self-care and mobility limitation spectrum we have introduced, more nuanced investigations of factors driving trends can be undertaken and projections accordingly fine-tuned. Indeed, better characterizing the care needs of the growing older population is a critical step in maximizing functioning—and quality of life—for all older adults.
Acknowledgments
This research was funded through a cooperative agreement with the National Institute on Aging (grant U01-AG032947).
An earlier version of this article was presented at the annual meeting of the Population Association of America; April 11–13, 2013; New Orleans, LA.
Note. The views expressed in this work are those of the authors alone and do not necessarily represent the views of the authors’ employers or the funding agency.
Human Participant Protection
The Johns Hopkins Bloomberg School of Public Health institutional review board approved this study.
References
- 1. US Census Bureau. Table 2. Projections of the population by selected age groups and sex for the United States: 2015 to 2060. 2012. Available at: http://www.census.gov/population/projections/data/national/2012/summarytables.html. Accessed September 15, 2013.
- 2.Centers for Medicare and Medicaid Services. Chronic Conditions Among Medicare Beneficiaries, Chart Book. Baltimore, MD: 2011. [Google Scholar]
- 3.Freedman VA, Stafford F, Schwarz N, Conrad F, Cornman J. Disability, participation, and subjective wellbeing among older couples. Soc Sci Med. 2012;74(4):588–596. doi: 10.1016/j.socscimed.2011.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freedman VA, Spillman BC, Andreski PM et al. Trends in late-life activity limitations in the United States: an update from five national surveys. Demography. 2013;50(2):661–671. doi: 10.1007/s13524-012-0167-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin SF, Beck AN, Finch BK, Hummer RA, Master RK. Trends in US older adult disability: exploring age, period, and cohort effects. Am J Public Health. 2012;102(11):2157–2163. doi: 10.2105/AJPH.2011.300602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaye HS. Disability rates for working-age adults and for the elderly have stabilized, but trends for each mean different results for costs. Health Aff (Millwood) 2013;32(1):127–134. doi: 10.1377/hlthaff.2012.0533. [DOI] [PubMed] [Google Scholar]
- 7.Schoeni RF, Martin LG, Andreski PM, Freedman VA. Persistent and growing socioeconomic disparities in disability among the elderly: 1982–2002. Am J Public Health. 2005;95(11):2065–2070. doi: 10.2105/AJPH.2004.048744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson LA, Goodman RA, Holtzman D, Posner SF, Northridge ME. Aging in the United States: opportunities and challenges for public health. Am J Public Health. 2012;102(3):393–395. doi: 10.2105/AJPH.2011.300617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guralnik JM, Fried LP, Salive ME. Disability as a public health outcome in the aging population. Annu Rev Public Health. 1996;17:25–46. doi: 10.1146/annurev.pu.17.050196.000325. [DOI] [PubMed] [Google Scholar]
- 10.Albert SA, Freedman VA. Public Health and Aging: Maximizing Functioning and Wellbeing. 2nd ed. New York, NY: Springer; 2010. [Google Scholar]
- 11.Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key Indicators of Well-Being. Washington, DC: US Government Printing Office; 2012. [Google Scholar]
- 12.Centers for Disease Control and Prevention. The State of Aging and Health in America 2007. Whitehouse Station, NJ: Merck Company Foundation; 2007. [Google Scholar]
- 13.Feldman PH, Oberlink M. The AdvantAge Initiative: developing community indicators to promote the health and well-being of older people. Family Community Health J. 2003;26(4):268–274. doi: 10.1097/00003727-200310000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Freedman VA, Agree E, Martin LG, Cornman J. Trends in the use of assistive technology and personal care for late-life disability, 1992–2001. Gerontologist. 2006;46(1):124–127. doi: 10.1093/geront/46.1.124. [DOI] [PubMed] [Google Scholar]
- 15.Wolff JL, Agree EM, Kasper JD. Wheelchairs, walkers, and canes: what does Medicare pay for, and who benefits? Health Aff (Millwood) 2005;24(4):1140–1149. doi: 10.1377/hlthaff.24.4.1140. [DOI] [PubMed] [Google Scholar]
- 16.Fried LP, Young Y, Rubin G, Bandeen-Roche K. WHAS II Collaborative Research Group. Self-reported preclinical disability identifies older women with early declines in performance and early disease. J Clin Epidemiol. 2001;54(9):889–901. doi: 10.1016/s0895-4356(01)00357-2. [DOI] [PubMed] [Google Scholar]
- 17.Whetstone LM, Fozard JL, Metter EJ et al. The physical functioning inventory: a procedure for assessing physical function in adults. J Aging Health. 2001;13(4):467–493. doi: 10.1177/089826430101300402. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine. The Future of Disability in America. Washington, DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- 19.Montaquila J, Freedman VA, Spillman BC, Kasper JD. National Health and Aging Trends Study Development of Round 1 Survey Weights. Baltimore, MD: Johns Hopkins University School of Public Health; 2012. [Google Scholar]
- 20.Kasper J, Freedman VA. National Health and Aging Trends Study Round 1 User Guide: Final Release. Baltimore, MD: Johns Hopkins University School of Public Health; 2012. [Google Scholar]
- 21.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The Index of ADL, a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 22.Freedman VA, Agree EM, Cornman JC, Spillman BC, Kasper JD. Reliability and validity of self-care and mobility accommodations measures in the National Health and Aging Trends Study. Gerontologist. 2013 doi: 10.1093/geront/gnt104. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freedman VA, Kasper J, Cornman J et al. Validation of new measures of disability and functioning in the National Health and Aging Trends Study. J of Gerontol B Soc Psy Sci. 2011;66(9):1013–1021. doi: 10.1093/gerona/glr087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guralnik JM, Simonsick EM, Ferrucci L et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 25.Kasper JD, Freedman VA, Niefeld MR. Construction of Performance-Based Summary Measures of Physical Capacity in the National Health and Aging Trends Study. Baltimore, MD: Johns Hopkins University School of Public Health; 2012. [Google Scholar]
- 26.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: Wiley; 1987. [Google Scholar]
- 27. Ofstedal MB, Fisher GG, Herzog AR. HRS/AHEAD documentation report: documentation of cognitive functioning measures in the Health and Retirement Study. 2005. Available at: http://hrsonline.isr.umich.edu/sitedocs/userg/dr-006.pdf. Accessed July 1, 2013.
- 28.Kroenke K, Spitzer RL, Williams JBW, Lowe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 29.Lowe B, Wahl I, Rose M et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2009;122(1–2):86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 30.Montaquila J, Freedman VA, Kasper JD. National Health and Aging Trends Study. Round 1: Income Imputation. Baltimore, MD: Johns Hopkins University School of Public Health; 2012. NHATS technical paper 3. [Google Scholar]
- 31.Ryff C. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57(6):1069–1081. [Google Scholar]
- 32.Schoeni RF, Freedman VA, Martin LG. Why is late-life disability declining? Milbank Mem Q. 2008;86(1):47–89. doi: 10.1111/j.1468-0009.2007.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]