Abstract
Objectives. We investigated the roles of House membership and the influence of social and sexual network members on the sexual risk behavior of men in the Los Angeles House and Ball community.
Methods. From February 2009 to January 2010, male participants (n = 233) completed interviewer-assisted surveys during a House meeting or Ball event. We used logistic regression to model the effects of sexual network size, influence of sexual network members, House membership status, and their interactions on high-risk sex.
Results. Significant predictors of high-risk sex included number of sexual partners in the nominated social network, multiethnicity, and previous diagnosis of sexually transmitted infection. House membership was protective against high-risk sex. Additionally, a 3-way interaction emerged between number of sexual partners in the network, influence, and network members’ House membership.
Conclusions. Future research should assess network members’ attitudes and behavior in detail to provide a greater understanding of the dynamics of social influence and to identify additional avenues for intervention.
African American men who have sex with men (MSM) have disproportionately high rates of HIV. African American MSM are being diagnosed with HIV or AIDS at more than twice the rate of White or Hispanic MSM,1 yet the individual-level risk behaviors of African American MSM do not explain the disparities in infection rates.2–4 It is important to examine the social context of African American MSM to help explain these disparities and to develop appropriate preventive interventions.
One particularly noteworthy avenue for approaching HIV prevention among African American MSM is the context of the House and Ball communities. Houses and Balls have a long history in the African American community.5 Presently, “Balls” can be characterized as underground social events that reward individuals who win competitions focused on dance, athletics, and gender expression. “Houses” are structured groups of individuals, led by a “mother,” “father,” or both, that compete against each other during Balls.6 Balls and Houses function as different entities yet work together in forming the vibrant community often known as the “Ballroom” or “Ball scene.”
House and Ball communities are present in cities such as Los Angeles and Oakland, California; Atlanta, Georgia; Chicago, Illinois; Philadelphia, Pennsylvania; Baltimore, Maryland; New York, New York; and Washington, DC.7 Yet relatively little research exists to describe the health and risk behaviors of individuals who participate in Houses and Balls. The few studies reporting HIV prevalence estimates among these communities have suggested that HIV is highly prevalent among House and Ball participants in Baltimore and New York,8 with HIV infection rates in New York potentially as high as 20%.6,9
A connection to the gay community has been well established as an important factor in understanding HIV risk behavior among MSM10; for African American MSM, who may experience rejection from the broader gay community because of their race,11 a connection to similar peers in the House and Ball community may be particularly salient.12 As an underground community, the House and Ball scene serves social as well as entertainment functions. Social support is an integral part of Houses and Balls,7,13 and social networks frequently form among House members, although these networks may vary in composition, size, and organization. Social network members may exert a direct influence on individuals’ behavior and an indirect influence via individuals’ perceptions of their network members’ attitudes and behaviors. For example, lower HIV risk behavior among African American MSM has been associated with perceived social norms that support condom use, even when network members did not use condoms themselves.14 Additionally, strong associations have been shown of self-reported condom use with perceptions of friends talking about condoms, using condoms, and encouraging others to use condoms.15
Social network analyses can help to elucidate such social influence processes on risk and protective behavior,16 and social network approaches have previously been used to understand HIV risk in other populations.17,18 Although the strongest source of influence is generally found between direct ties, including sexual partners, the degree of social influence carried by a network member may also be linked to social roles and in-group status.19 Because in-group members are more influential, their behavior may exert a greater impact on a group member’s health choices than does similar behavior from out-group members.
Because of the importance of social networks in the House and Ball community and the role of social processes, particularly among cohesive in-groups, in determining health behavior, we investigated the interplay between characteristics of community members’ social networks and their own health behavior choices. We examined the roles of relationships, House membership, and perceived influence of social network members on sexual risk behaviors. We hypothesized that House members would be more likely to use condoms to protect their in-group. We further hypothesized that having sexual partners who were House members—and thus, per the first hypothesis, likely to use condoms to protect their in-group—would also protect against sexual risk but only when those sexual partners were reported to be highly influential.
METHODS
Participants were 233 men recruited at House and Ball events in Los Angeles between February 2009 and January 2010 as part of the African American Young Men’s Study.20 House and Ball community members were eligible to participate if they attended an event during the study period and had not previously participated in the research survey. We modeled sampling procedures after the Young Men’s Study, with venue selection and participant recruitment adapted for the target community after extensive community outreach.21 We categorized recruitment venues into 3 types: Balls, House meetings, and community events. Events and venues included in the sampling frame had at least a 2-hour period, with an expected yield of at least 4 House and Ball community members. We created private survey areas at Balls and other events using portable “voting booths” designed for the project. Sampling periods typically occurred during late night or early morning hours. Study staff approached persons who entered the designated venue to assess eligibility. Eligible persons were escorted to the private survey booths to complete the data collection activity. Participants completed a 30- to 45-minute audio, computer-assisted self-interview survey on site. For persons younger than 18 years, we obtained a waiver of parental permission. Participants received a $40 incentive for completing this survey. A full description of the study, including community outreach efforts and sampling and survey procedures, has been previously published.20
We asked participants to report on a variety of demographic variables, including age, race/ethnicity, and multiethnic status (1 = multiethnic, 0 = otherwise). We operationalized current House membership as a binary variable (1 = current House member, 0 = not a current member). An additional binary variable represented a history of sexually transmitted infection (1 = ever diagnosed with any sexually transmitted infection, 0 = never diagnosed with any sexually transmitted infection), and a continuous variable represented total number of sexual partners in the past 3 months.
We asked participants to list up to 10 members of their social networks. Respondents first named up to 5 people who provided emotional support or tangible support (monetary assistance) and with whom they attended Balls; they then named up to 5 additional people with whom they had had sex in the past 3 months and indicated whether any of the social network members they had previously listed were also sexual partners in the past 3 months. We first operationalized main effects of social network variables on the network member level and then aggregated them to the participant level as follows: we contrast-coded (1 = yes, −1 = no) “network sexual partnership,” which represented whether the participant had had sex with the network member within the past 3 months in the network-level data. We then aggregated this variable by mean to the participant level, giving each participant a score representing the percentage of his social network with whom he had recently had sex. We similarly contrast-coded (1 = House member, −1 = nonmember) “network House membership,” which represented whether the network member was a House member and aggregated this by mean to the participant level, giving each participant a score representing the percentage of his social network who were currently House members. “Network influence” was a single measurement of how influential the participant believed each network member was in his life, originally on a 1 (no influence) to 10 (most influential) scale. We first standardized this score (new range = −2.18–0.97) and then aggregated it by mean to the participant level, yielding a mean standardized influence score for each participant that described how influential, on average, that participant’s social network was compared with other participants in the study.
We similarly computed 2- and 3-way interactions between social network variables first at the network level and then aggregated by mean to the participant level. Specifically, we multiplied the contrast codes representing network members’ sexual partnership and House membership by each other and by the continuous influence variable at the network level; we then aggregated these products by mean to the participant level. This yielded three 2-way interaction scores (sexual partnership × House membership, sexual partnership × influence, and House membership × influence) and one 3-way interaction score (sexual partnership × House membership × influence) per participant.
Finally, we asked participants how frequently they had used condoms during vaginal, anal receptive, or anal insertive sex during the past 3 months; response options included never, less than half the time, half the time, more than half the time, and all the time. We operationalized high-risk sex as a binary indicator of inconsistent condom use (1 = inconsistent condom use, defined as any frequency less than all the time; 0 = consistent condom use or no sex) during any penetrative sex act over the past 3 months. We conducted all analyses using IBM SPSS Statistics version 19 (SPSS, Inc, Chicago, IL).
RESULTS
Descriptive statistics for participant demographic, social network, and sexual risk information are summarized in Table 1. We used logistic regression to model the effects of social network sexual partnership, House membership, and influence as well as their interactions on high-risk sex. Because the sample was overwhelmingly African American (83%), we did not include race as a covariate but instead included whether the participant considered himself multiethnic. Participant’s age was not significantly associated with high-risk sex, and we dropped it from the final model. Total number of sexual partners was associated with high-risk sex on the bivariate level (t [71] = 2.282; P < .05) but did not remain significant after controlling for other participant-level and social network variables, and we also removed this from the final model.
TABLE 1—
Descriptive Statistics: African American Young Men’s Study, Los Angeles, CA, February 2009–January 2010
| Variables | No. (%) or Mean ±SD |
| Participant demographics | |
| Age, y (range = 17–53) | 23.56 ±6.03 |
| 17–20 | 70 (30) |
| 21–25 | 119 (51) |
| ≥ 26 | 44 (19) |
| Primary race/ethnicity | |
| Black or African American | 194 (83) |
| Latino or Hispanic | 15 (6) |
| American Indian or Native American | 5 (2) |
| Asian or Pacific Islander | 3 (1) |
| White or Caucasian | 0 (0) |
| Other | 16 (7) |
| Multiethnic | 72 (31) |
| Residential status | |
| Live with family | 92 (40) |
| Own place or apartment | 109 (47) |
| With friends, partner, or House and Ball members | 28 (12) |
| No regular place or other | 4 (2) |
| House membership | |
| Ever a House member | 161 (69) |
| Current House member | 121 (52) |
| Social network variables | |
| No. of members in social network (range = 1–10) | 5.12 ±1.63 |
| No. of sexual partners in social network (range = 0–6) | 1.15 ±1.06 |
| Proportion of social network who are sexual partners | 0.21 ±0.15 |
| No. of House members in social network (range = 0–7) | 1.19 ±1.37 |
| Proportion of social network who are House members | 0.24 ±0.27 |
| Mean influence of social network members (range = 1–10) | 7.27 ±1.91 |
| Sexual risk | |
| Total no. of sexual partners past 3 mo (range = 0–25) | 2.04 ±3.28 |
| Any high-risk sex past 3 mo | 62 (27) |
| Inconsistent condom use during vaginal sex | 11 (5) |
| Inconsistent condom use during anal receptive sex | 46 (20) |
| Inconsistent condom use during anal insertive sex | 50 (22) |
Note. The sample size was n = 233.
The final model predicting high-risk sex, presented in Table 2, displayed good fit (Hosmer and Lemeshow χ2[8] = 10.51, ns) and explained 19.3% of the estimated variance in participants’ engagement in high-risk sexual activity over the prior 3 months. Significant participant-level risk factors for high-risk sex included being multiethnic (odds ratio [OR] = 2.280; 95% confidence interval [CI] = 1.150, 4.519; P < .05) and previous diagnosis with any sexually transmitted infection (OR = 2.334; 95% CI = 1.161, 4.693; P < .05). Current membership in a House was protective against high-risk sex (OR = 0.382; 95% CI = 0.189, 0.771; P < .01).
TABLE 2—
Logistic Regression Model Predicting High-Risk Sex: African American Young Men’s Study, Los Angeles, CA, February 2009–January 2010
| Variables | OR (95% CI) | P |
| Participant variables | ||
| Multiethnic | 2.280 (1.150, 4.519) | .018 |
| Current House member | 0.382 (0.189, 0.771) | .007 |
| Ever diagnosed with an STI | 2.334 (1.161, 4.693) | .017 |
| Main network effects | ||
| No. of sexual partners in network | 4.762 (1.370, 16.547) | .014 |
| No. of House members in network | 1.089 (0.462, 2.566) | .845 |
| Network influence | 1.858 (0.785, 4.399) | .159 |
| 2-way network interactions | ||
| Network sexual partners × influence | 1.255 (0.506, 3.112) | .624 |
| Network House status × influence | 0.654 (0.252, 1.697) | .383 |
| Network sexual partners × House status | 0.764 (0.307, 1.903) | .564 |
| 3-way network interaction: network sexual partners × House status × influence | 0.376 (0.151, 0.936) | .036 |
Note. CI = confidence interval; OR = odds ratio; STI = sexually transmitted infection.
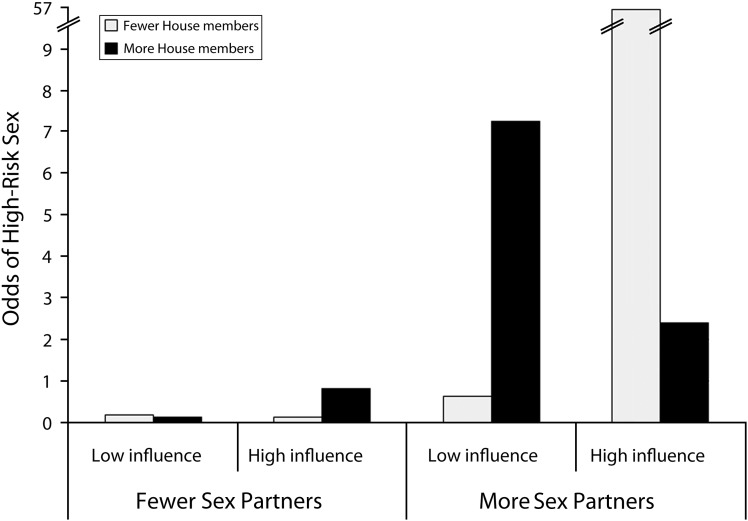
Having more sexual partners in one’s social network was associated with a nearly 5-fold increase in the odds of high-risk sex (OR = 4.76; 95% CI = 1.370, 16.547; P < .05). The number of social network members in Houses was not by itself a significant predictor of high-risk sex, nor was the average influence rating of the network. However, a significant 3-way interaction between network sexual partnership, network House membership, and influence did emerge (OR = 0.376; 95% CI = 0.151, 0.936; P < .05). As depicted in Figure 1, the main effect of network sexual partnership is evident in this 3-way interaction; so having fewer recent sexual partners in one’s social network was associated with lower sexual risk across the other variables. However, among those with more sexual partners in their social networks, who those partners were appeared to matter: the greatest risk was associated with sexual partners who were highly influential but not members of Houses. Comparatively, high-influence House members were associated with less high-risk sex among participants with more sexual partners in their network. Participants whose sexual partners were House members but low influence were also at increased risk for high-risk sex, suggesting that choosing House members as sexual partners is not protective across the board. Rather, the protective effects of partnering with a House member were proportional to the amount of influence that sexual partner exerted.
FIGURE 1—
Three-way interaction between network sexual partnership, network House membership, and network influence on high-risk sex: African American Young Men’s Study, Los Angeles, CA, February 2009–January 2010.
To further understand this effect and check for possible alternative explanations, we conducted a series of supplementary analyses investigating the distribution of sexual partners, House members, and influence among participants’ social networks. Men in the broader House and Ball communities did not appear to be preferentially selecting House members as sexual partners (χ2[1] = 0.166, P = .68). Furthermore, the total number of sexual partners in the past 3 months did not differ by House membership (t [231] = −1.107, P = .27), nor did network members’ influence (t[515] = −0.060, P = .95). Thus, the lower sexual risk associated with influential House members does not appear to be an artifact of more House members in the network or of these members automatically carrying more influence as a result of their involvement in the House and Ball community.
DISCUSSION
We studied a sample of young men in a predominantly African American, MSM community who attended House and Ball events in Los Angles. Consistent with previous research in other communities, a history of sexually transmitted infection and a greater number of sexual partners (particularly inside the social network) were significant risk factors associated with recent high-risk sexual activity. We also found multiethnicity to be an important risk factor for high-risk sex. This result is in line with other research that has found multiethnicity to be a predictor of early sexual debut22; however, little is known about the role of multiple ethnicities in sexual minority populations, and the risk behavior of multiethnic compared with single-ethnic individuals merits further exploration.
Another important finding novel to this sample was the association of current House membership with significantly lower odds of sexual risk taking. Individuals who become House members may be explicitly seeking a safe, supportive social context separate from the larger gay community, which may stigmatize them based on race or ethnicity.11 If so, condom use may reflect House members’ motivation to protect this important community in their lives. Alternately, these results may suggest that Houses have developed an important MSM-focused HIV prevention initiative in their own community. For example, 80% of Los Angeles House and Ball community members reported having been tested for HIV within the past 6 months, and more than a quarter of them reported participating in other HIV prevention–related programming, such as HIV prevention interventions and individual counseling services.23 Further research is warranted to determine whether House membership leads to risk reduction or whether those who are less risky tend to join Houses rather than attending Ball events unaffiliated.
This study also highlights the importance of social networks and social influence in understanding sexual risk behaviors among racial/ethnic minority MSM. An interaction between number of sexual partners in the network, network members’ influence, and House membership illustrated that among men with more sexual partners, having partners who were influential House members was associated with less high-risk sex. By contrast, influential nonmembers were associated with higher odds of engaging in sexual risk behaviors. These findings have potential implications for interventions targeting young MSM who attend House and Ball events: by enhancing the visibility and influence of House members involved in HIV prevention activity, these House members may establish and reinforce social norms of protective behavior in the broader social network of the House and Ball community. Community members have already been receptive to the integration of safer sex and HIV prevention messaging into Ball events.23 Interventions combining HIV prevention with an emphasis on group cohesion, which has been found to be an important mediator of behavior change,24–26 may capitalize on House members’ influence to establish and maintain protective behavioral norms consistent with HIV prevention.
The establishment of protective norms is particularly important considering our finding that participants did not preferentially choose House members as sexual partners. House members may be acting in support of their own health, which automatically carries the benefit of protecting their sexual partners. Interventions that can support influential House members to become ambassadors for HIV prevention messaging, including safer sex messaging, may extend the reach of these individuals to House and Ball community members who are not already their sexual partners. Useful strategies for HIV prevention interventions may include targeting the unique relationships among House members for HIV prevention message dissemination, integrating group cohesion into HIV prevention activities, and enhancing HIV prevention communication skills. The personal endorsement of risk reduction by influential House members may promote social norms of HIV risk reduction among their own network members as well as other peers in the community.
Limitations
This study is subject to the limitations of the sampling method, use of self-report data, study design, and measurement. We recruited participants from a range of venues, including Balls, House meetings, and community events, with the intention of capturing the broadest possible sample of participants in these communities, but some Houses may be underrepresented. The risk behavior data were all self-reported, although we collected all measures via audio, computer-assisted self-interview methods intended to reduce social desirability bias in responding.
The cross-sectional study design limits the assignment of causality; we cannot determine whether the confluence of sexual partners, House members in the network, and influence lead to varying levels of risk behaviors or whether those who have these constellations of network members and relationships tend to engage in different levels of risk behaviors owing to other, unmeasured variables. Future longitudinal research will be needed to disentangle these effects.
Finally, it was not possible to measure all possible risk or protective factors in a single survey, particularly of network members’ attitudes and behavior, and thus there may be confounding variables or alternate explanations we could not assess and test directly.
Conclusions
This study is an important contribution to the literature on HIV risk and prevention in a difficult-to-reach population, and these findings suggest that the constellation of sexual network members and the levels of influence among these members are important variables to assess. Future research should assess network members’ attitudes and behavior in detail to provide a greater understanding of the dynamics of social influence and identify additional avenues for intervention.
Acknowledgments
This study was funded by the National Institute on Drug Abuse, National Institutes of Health (grant R01 DA22968).
The authors would like to acknowledge the contributions of the staff members who contributed to collection, management, analysis, and review of these data: Veronica Abernathy, Teela Davis, Deandre Ellison, Judith Grout, Cody Haight, Nefe Iredia, Tattiya Kliengklom, Sylvia Lambrechts, Donna Luebbe, Griselda Monroy, Heather Reyes, Marcia Higareda, Luis Salazar, Milton Smith, Flor Vindel, and Carolyn Wong. The authors would also like to acknowledge the insightful and practical commentary of the members of the P3 Advisory Board, the mothers and fathers from the House of Allure, House of Chanel, House of Ebony, House of Escada, House of Etro Galliano, House of Herrera, House of Garcon, House of Gotti, House of Lauren van Cartier, House of Mizarahi, House of Miyake Mugler, House of Revlon, House of Rodeo, and House of Ultra Omni. We are especially grateful to all of the parents, leaders, and members of the Los Angeles House and Ball communities for their commitment and willingness to share their diverse and often profound personal experiences as well as welcoming us into a part of their lives.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
Human Participant Protection
All participants provided written informed consent to participate in the study. This study was approved by the Committee on Clinical Investigations at Children’s Hospital Los Angeles.
References
- 1.Centers for Disease Control and Prevention. HIV surveillance in men who have sex with men. Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/slides/msm. Accessed May 31, 2012.
- 2.Hall HI, Song R, Rhodes P et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Phillips G, Wohl A, Xavier J, Jones K, Hidalgo J. Epidemiologic data on young men of color who have sex with men. AIDS Patient Care STDS. 2011;25(suppl 1):S3–S8. doi: 10.1089/apc.2011.9882. [DOI] [PubMed] [Google Scholar]
- 4.Tieu HV, Murrill CS, Xu G, Koblin BA. Sexual partnering and HIV risk among Black men who have sex with men: New York City. J Urban Health. 2010;87(1):113–121. doi: 10.1007/s11524-009-9416-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chauncey G. Gay New York. New York, NY: Basic Books; 1994. [Google Scholar]
- 6.Murrill CS, Liu K, Guilin V et al. HIV prevalence and associated risk behaviors in New York City’s House Ball community. Am J Public Health. 2008;98(6):1074–1080. doi: 10.2105/AJPH.2006.108936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arnold EA, Bailey MM. Constructing home and family: how the ballroom community supports African American GLBTQ youth in the face of HIV/AIDS. J Gay Lesbian Soc Serv. 2009;21(2–3):171–188. doi: 10.1080/10538720902772006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. HIV-related tuberculosis in a transgender network—Baltimore, Maryland, and New York City area, 1998–2000. MMWR Morb Mortal Wkly Rep. 2000;49(15):317–320. [PubMed] [Google Scholar]
- 9.Sanchez T, Finlayson T, Murrill CS, Guilin V, Dean L. Risk behaviors and psychosocial stressors in the New York City House Ball community: a comparison of men and transgender women who have sex with men. AIDS Behav. 2010;14(2):351–358. doi: 10.1007/s10461-009-9610-6. [DOI] [PubMed] [Google Scholar]
- 10.Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48(2–3):218–253. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kubicek K, McNeeley M, Holloway IH, Weiss G, Kipke MD. “It’s like our own little world”: resilience as a factor in participating in the ballroom community subculture. AIDS Behav. 2013;17(4):1524–1539. doi: 10.1007/s10461-012-0205-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mutchler MG, McKay T, Candelario N, Liu H, Stackhouse B, Ayala G. Sex, drugs, peer connections, and HIV: use and risk among African-American, Latino, and multiracial young men who have sex with men (YMSM) in Los Angeles and New York. J Gay Lesbian Soc Serv. 2011;23(2):271–295. doi: 10.1080/10538720.2011.560100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong CF, Schrager SM, Holloway IW, Meyer IH, Kipke MD. Minority stress experiences and psychological well-being: the impact of support from and connection to social networks within the Los Angeles House and Ball communities. Prev Sci. 2013 doi: 10.1007/s11121-012-0348-4. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peterson JL, Rothenberg R, Kraft JM, Beeker C, Trotter R. Perceived condom norms and HIV risks among social and sexual networks of young African American men who have sex with men. Health Educ Res. 2009;24(1):119–127. doi: 10.1093/her/cyn003. [DOI] [PubMed] [Google Scholar]
- 15.Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Soc Sci Med. 2003;56(3):465–476. doi: 10.1016/s0277-9536(02)00047-3. [DOI] [PubMed] [Google Scholar]
- 16.Dawber TR, Meadors GF, Moore FE., Jr Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health. 1951;41(3):279–281. doi: 10.2105/ajph.41.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fisher JD. Possible effects of reference group-based social influence on AIDS-risk behavior and AIDS prevention. Am Psychol. 1988;43(11):914–920. doi: 10.1037//0003-066x.43.11.914. [DOI] [PubMed] [Google Scholar]
- 18.Tucker JS, Hu J, Golinelli D, Kennedy DP, Green HD, Wenzel S. Social network and individual correlates of sexual risk behavior among homeless young men who have sex with men. J Adolesc Health. 2012;51(4):386–392. doi: 10.1016/j.jadohealth.2012.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97(7):891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- 20.Kipke MD, Kubicek K, Supan J, Weiss G, Schrager SM. Laying the groundwork for an HIV prevention intervention: a descriptive profile of the Los Angeles House and Ball communities. AIDS Behav. 2013;17(3):1068–1081. doi: 10.1007/s10461-012-0227-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.MacKellar DA, Valleroy LA, Karon JM, Lemp GF, Janssen RS. The Young Men’s Survey: methods for estimating HIV seroprevalence and risk factors among young men who have sex with men. Public Health Rep. 1996;111(suppl 1):138–144. [PMC free article] [PubMed] [Google Scholar]
- 22.Shneyderman Y, Schwartz SJ. Contextual and intrapersonal predictors of adolescent risky sexual behavior and outcomes. Health Educ Behav. 2013;40(4):400–414. doi: 10.1177/1090198112447800. [DOI] [PubMed] [Google Scholar]
- 23.Holloway IW, Traube DE, Kubicek K, Supan J, Weiss G, Kipke MD. HIV prevention service utilization in the Los Angeles House and Ball communities: past experiences and recommendations for the future. AIDS Educ Prev. 2012;24(5):431–444. doi: 10.1521/aeap.2012.24.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burke SM, Carron AV, Patterson MM et al. Cohesion as shared beliefs in exercise classes. Small Group Res. 2005;36(3):267–288. [Google Scholar]
- 25.Christensen U, Schmidt L, Budtz-Jørgensen E, Avlund K. Group cohesion and social support in exercise classes: results from a Danish intervention study. Health Educ Behav. 2006;33(5):677–689. doi: 10.1177/1090198105277397. [DOI] [PubMed] [Google Scholar]
- 26.Lee RE, O’Connor DP, Smith-Ray R et al. Mediating effects of group cohesion on physical activity and diet in women of color: health is power. Am J Health Promot. 2012;26(4):e116–e125. doi: 10.4278/ajhp.101215-QUAN-400. [DOI] [PMC free article] [PubMed] [Google Scholar]