Abstract
Nonmedical prescription opioid misuse remains a growing public problem in need of action and is concentrated in areas of US states with large rural populations such as Kentucky, West Virginia, Alaska, and Oklahoma. We developed hypotheses regarding the influence of 4 factors: (1) greater opioid prescription in rural areas, creating availability from which illegal markets can arise; (2) an out-migration of young adults; (3) greater rural social and kinship network connections, which may facilitate drug diversion and distribution; and (4) economic stressors that may create vulnerability to drug use more generally. A systematic consideration of the contexts that create differences in availability, access, and preferences is critical to understanding how drug use context varies across geography.
Nonmedical prescription opioid use is a rapidly escalating public health problem. Unintentional overdose deaths from opioid pain relievers has quadrupled since 1999 and by 2007 outnumbered those involving heroin and cocaine combined.1 Much of this growth has been because of an increased misuse of opioid analgesics, which contributed to 21% of all poisoning deaths in 1999 and 37% in 2006.2 By 2010, 2.4 million Americans initiated nonmedical prescription opioid use; this equals 6600 daily initiates.3 Other evidence demonstrates a sharp increase in rates of use of prescription opioids4,5 abuse or dependence,4 emergency department visits,6,7 and overdose injury among all age groups in the United States.8–10
Although all states have demonstrated an increase in nonmedical prescription opioid morbidity and mortality during the past decade, death and injury from nonmedical prescription opioid misuse are concentrated in states with large rural populations, such as Kentucky, West Virginia, Alaska, and Oklahoma.11–13 Distinctions between urban and rural areas are not binary but reflect a continuum of population density and proximity to the 1098 defined metropolitan areas of the United States.14 We conceptualized rural areas as nonmetropolitan counties, acknowledging that this is a heterogeneous category for geographical areas.
Individuals in counties outside metropolitan areas have higher rates of drug poisoning deaths, including deaths from opioids, and opioid poisonings in nonmetropolitan counties have increased at a rate greater than threefold the increase in metropolitan counties.11 Drug-related deaths involving opioid analgesics are higher in these rural areas even after adjusting for population density,15 and the ratio of nonmedical users to medical users is higher in rural areas as well.16 Nationally representative surveys have indicated that, in rural areas, not only are there higher mortality and injury rates but also adolescents are more likely to use prescription opioids nonmedically than are their urban counterparts.17–20 These surveys also report that factors such as polydrug use and depression are associated with nonmedical opioid use in rural areas.20
Why is nonmedical prescription opioid misuse more prevalent in rural areas than in urban areas? There is, surprisingly, little empirical data that help us address this question. Risk factors that explain rural–urban differences in nonmedical prescription opioid use must vary across rural versus urban geographical contexts and be either associated with drug use generally or use of nonmedical prescription opioids specifically. Although contextual determinants of drug use are important in explaining why individuals use drugs and become dependent,21,22 our understanding of the mechanisms through which broadly defined geographical settings influence drug use remains limited.
We approached this issue in 3 steps. First, we explicated an array of known risk factors associated with illicit drug use generally. Second, we considered whether any of these factors are associated specifically with nonmedical prescription opioid use. Third, we linked the factors to the rural context, providing hypotheses that may explain the excess burden of prescription opioid misuse in rural compared with urban areas.
RISK FACTORS THAT DRIVE ILLICIT DRUG USE
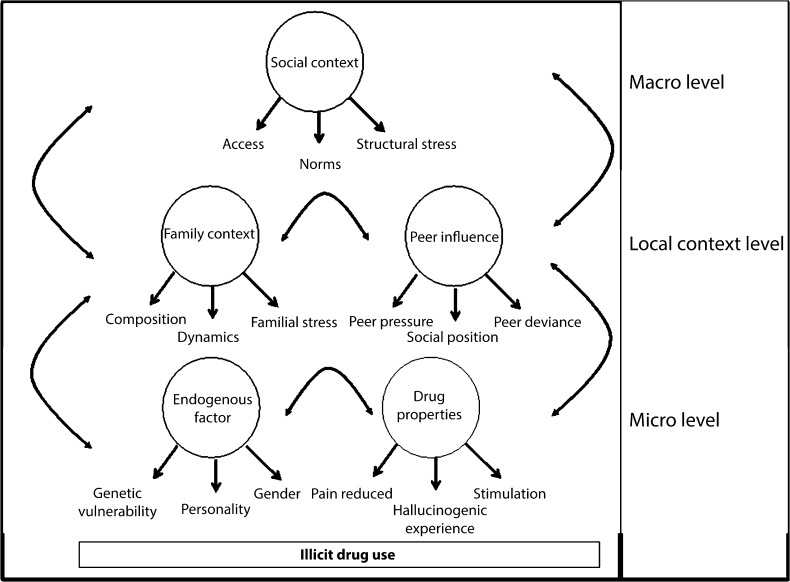
Our model of drug use risk factors is grounded in ecosocial theory and ecological systems theory21,23,24 and is organized by 3 levels of influence that dynamically interact (Figure 1).
FIGURE 1—
A conceptual framework for the etiology of illicit drug use.
The first is the macro level, where the social context structures the availability of drugs and the norms around use.25,26 Furthermore, stressors at a macro level such as economic deprivation,27 inequality,28 structural discrimination,29 and other pervasive stressors in the environment may serve as risk factors for drug use.30,31
The second is the local context, which includes family dynamics (e.g., supervision, conflict),32–35 family composition (e.g., older siblings),36 and family stress (e.g., unemployment). Furthermore, peer influence is a strong correlate of drug use.37,38
The third is the micro level. Endogenous factors such as genetic vulnerability,39 neurobiological factors,40–42 pharmacological reactivity,43 personality traits such as sensation seeking and impulsivity,44,45 psychiatric morbidity,46–48 and gender and age49,50 have strong and substantial influences on the propensity to misuse drugs and develop chronic drug dependencies. The pharmacological properties of a drug are important in determining who uses them and how they use them.22
These 3 levels of influence interact in dynamic ways; for example, social norms regarding substance use, a contextual influence, may affect how peers interact and form relationships around substance use.51
NONMEDICAL PRESCRIPTION DRUGS VS OTHER ILLICIT DRUGS
Many of the well-documented risk factors for illicit drug use predict both nonmedical prescription opioid use and other illicit drug use. Therefore, these cannot readily explain why nonmedical prescription opioid use is increasing, especially in rural areas. For example, nonmedical prescription drug users are more likely to be male,52,53 be young,54 be polydrug users,55 have comorbid psychopathology,54,56–59 and have positive expectations about the effects of use.60–62 These are all risk factors for illicit drug use more generally. We identified 3 factors for which empirical evidence indicates specificity in association with nonmedical prescription opioid use versus other illicit drugs.
Increased Availability and Access
Prescription opioids became widely available in the mid-1990s. Between 1997 and 2007, per capita retail purchases of methadone, hydrocodone, and oxycodone increased 13-fold, 4-fold, and 9-fold, respectively.63 By 2010, enough prescription opioids were sold to medicate every adult in the United States with a dose of 5 milligrams of hydrocodone every 4 hours for 1 month.64
A study of national trends found that during 1999 through 2008, overdose death rates, sales, and substance abuse treatment admissions related to prescription opioids increased in parallel.64 This coincided with a larger movement in the medical community in the late 1990s to identify and treat pain as a fifth vital sign; bodies such as the American Pain Society established guidelines that included aggressive treatment of reported pain, and a campaign initiated by the Department of Veterans Affairs in part fueled the movement with the intention of improving pain management and treating chronic pain.65–67
Increased medical use of prescription opioids has resulted in increased access to opioids for nonmedical use, either through the nonmedical use of legitimately acquired prescriptions or through formal or informal distribution networks.68–73 Studies indicate that the large majority of adults who use opioids nonmedically obtain them from friends and relatives or from street-level dealers.68–73 A substantial proportion of overdose deaths and emergency department visits occurs among individuals who have never received a prescription.10,74–76 The proliferation of illicit high-volume prescribers and clinics (so-called pill mills) has also contributed to increases in overdoses in states such as Florida and Texas.18,77
Although availability of and access to prescription opioids have clearly increased across all areas of the United States, evidence regarding changes in the availability and access of illicit drugs, such as heroin and cocaine, is more mixed. Data on emergency department visits suggest that emergency department visits for prescription opioids more than doubled from 2004 to 2010, whereas cocaine-related visits increased 10% and heroin-related visits decreased.78 National survey research indicates no evidence of an increase in the proportion of adolescents and adults who report that drugs such as marijuana are fairly easy or very easy to obtain over the past 10 years79 (we did not assess comparable data on opioids), suggesting that the availability of nonopioid illicit drugs may not be keeping pace with the availability of prescription opioids, at least among adolescents.
However, data from the National Drug Threat Assessment indicates that heroin and cocaine availability is increasing nationally,80 although information on comparisons with availability of prescription opioids is not available. Although the available evidence thus suggests that increases in prescription opioid availability have outpaced that of illicit drugs, the nonmedical prescription opioid use epidemic may portend future increases in illicit drug use as well, considering that nonmedical prescription opioid users are more likely than are nonusers to transition to heroin and other illicit drugs.81
Lower Perceptions of Harm
Adolescents perceive prescription opioids such as OxyContin and Vicodin as more harmful than other prescription drugs such as Adderall and amphetamines, but they perceive prescription opioid use as less harmful than the use of almost all other drugs except experimental alcohol and occasional marijuana use.82 Lower perceptions of harm for prescription opioids compared with other illicit drugs could be owing to 2 factors.
First, opioid use for pain management is increasingly common; thus, nonmedical users observe and are acquainted with the effective pharmacological action of the drugs among individuals in social and kin networks. Second, prescription opioid use does not necessarily involve routes of transmission with higher social stigma and greater adverse health consequences such as smoking, snorting, and injecting,83,84 although some evidence indicates that rural nonmedical prescription opioid users are more likely to use nonoral modes of administration than are urban users.85,86
Self-Medicating for Pain
When used as prescribed under medical supervision, opioid analgesics are effective and used as standard practice in managing acute and chronic pain.87,88
Because of the fast action in reducing pain and anxiety symptoms, many individuals who overuse legitimate prescriptions or obtain prescription opioids illegally do so to manage existing chronic or acute pain or emotional problems.89
RURAL AREA USE VS URBAN AREA USE
We next considered specific factors that might explain the urban versus rural differences in nonmedical prescription opioid use. We hypothesized that 4 factors might be particularly relevant in explaining these patterns. These hypotheses have an empirical basis but require testing.
More Increased Availability in Rural Than Urban Areas
Although availability of prescription opioids has increased in all areas, there is evidence that it has increased more in rural areas. Specifically, per capita sales data indicate that states with large rural populations such as West Virginia are among the highest prescribers of opioid analgesics. The data are not entirely consistent with increased availability in rural areas, however, with Florida being a central outlier.
Several nonrural counties in Florida have the highest mean milligrams of opioids dispensed as of 2008,90 and many of the top-prescribing doctors and clinics are in the state of Florida, although recent data indicate that control measures are reducing diversion of and doctor shopping for opioids in Florida.91 Considering the evidence in total, however, a general picture emerges whereby high prescription rates in many rural counties indicate increased availability in these areas. The marketing of prescription opioids such as OxyContin has been more aggressive in rural communities such as those surrounding Appalachia.92
Rural populations are on average older than are urban populations93,94; thus, there may be more chronic pain for which management with opioid analgesics is indicated. Furthermore, evidence indicates that chronic pain and injury are more common in rural than in urban areas.95–97 Finally, qualitative research indicates that prescription drug use in rural areas such as Appalachian Kentucky is an embedded part of the culture of the area, with prescription narcotics often prescribed to maintain a steady workflow in mines and other heavy labor occupations.98 A higher density of available opioids may create opportunities for illegal markets in rural areas because family and friends are a primary distribution source of nonmedical prescription opioids.68–73,99
Out-Migration of Young People
In the past 2 decades, rural areas have evidenced an out-migration of many young adults during peak producing ages. For example, data from the 2010 census indicated that the percentage of individuals older than 65 years in West Virginia (which has a high proportion of rural counties) is twice the percentage of those aged 18 to 24 years (in 1970 the percentages of these 2 age groups were approximately equal).100
There are 2 consequences of this out-migration that may be related to increases in nonmedical prescription opioid use in rural areas. First is the effect on the economic conditions of the area. Areas with an aging workforce have less new economic infrastructure.93,101,102 Adverse economic conditions and high rates of unemployment may create greater vulnerability to drug use in these populations. Second is a selection effect. Young adults who stay in economically deprived areas may have a greater accumulation of risk factors for problematic drug use and may be more likely to have established drug dependencies at a young age that cause downward social drift.
Although data on young adult migration patterns in the United States are scant, substantial research has documented that adolescents in rural areas overall have lower academic aspirations and academic achievement103,104 as well as fewer returns on academic investment.103–105 Individuals who have the material resources and aspirations to migrate to urban areas are likely different from individuals who stay on an array of risk factors for drug use, including educational attainment. Data on differences in young adult migration as it relates to risk factors for prescription opioid use are critical for testing and advancing these hypotheses.
Social and Kinship Networks
The influence of family structures and family life is a central cultural difference between rural life and urban life. Although rural areas are increasingly connected to urban spaces as urbanization continues in the United States, there are substantial differences in social norms, expectations, and cultural values between families of rural versus urban areas.106–108 For example, in many rural areas a higher value is placed on work and on investment in the community than on education.109 Individuals in rural areas report knowing the members of their social network longer and being more closely related to members of their social network than are individuals in urban areas.106 Furthermore, substantial sociological research has documented that individuals in rural areas trust their neighbors more and are more likely to engage socially with neighbors and others who are geographically close.108,110 Ties to the community are often stronger in rural areas, and greater value is placed on maintaining strong social capital.107
In the context of such strong social and kinship networks, economic hardship associated with industrial restructuring and rural to urban migration of youths may generate strain not only in affected individuals but also in the broader social network, increasing the risk for illicit drug use across the social structure.107 However, strong social ties with family and community may serve as a buffer against the stress of economic hardship,111 in which case strong social ties would be associated with reduced drug use in rural areas. Testing and differentiating these pathways are critical for advancing our understanding of rural communities and drug use.
Family structures in rural areas are also larger and fertility rates are higher,112 suggesting that rural kinship networks are often wider than are urban kinship networks. Substantial empirical evidence indicates that, in contrast to the sources of other illicit drugs, one of the main sources of illicit prescription opioids is the diversion of prescriptions legitimately filled by parents, relatives, friends, or acquaintances.68–72,99 Thus, family networks matter more for prescription drugs than for other drugs because they are more often obtained from family members, whereas other drugs are more often obtained through friends or the drug trade.
Interestingly, OxyContin use has been significantly associated with increased social capital in rural areas,113 suggesting that nonmedical prescription opioid distribution networks integrate into social networks in important ways in isolated rural communities. The breadth and proximity of the social network in rural areas may allow faster diffusion of prescription drugs to potential nonmedical users, and sources of prescription opioids through families may be more accessible in rural areas. These wide social networks with close ties across individuals may facilitate the distribution of prescription opioid medication. Little research has mapped social networks of prescription opioid diversion in rural areas; the hypotheses we have outlined provide a road map for addressing the potential differences in diversion and dissemination of prescription opioids in rural versus urban settings.
Structural Stressors of Modern Rural Living
Although there are stressors associated with living in both urban and rural areas, economic downturns have more adversely affected rural areas in the United States114; thus, stress owing to unemployment and lack of available industry may be more strongly felt in rural areas. It has been well documented that geographical context shapes risk of drug use,21,22,25,115–117 including poverty and unemployment.27,28,118–124 Rural counties in particular have faced job sector and industry shifts as populations shift to meet the labor demands of changing markets,125,126 resulting in long-term economic deprivation, high rates of unemployment, and fewer opportunities for establishing a long-term career with potential for upward mobility.125
Numerous economic analyses have revealed mismatches between the skills of residents and the jobs available to them, and industrial restructuring predicts a shift into poverty of many in the United States.24,80 Furthermore, in the United States, there have been decreases in the wage rate for low-skilled jobs126 and the demand for manufacturing jobs127 coupled with an increase in the demand for high-skilled workers.80,86 These factors affect rural more than urban counties,127 which generally have a greater diversity of labor markets and workers.
SUMMARY AND FUTURE DIRECTIONS
In the box on this page we have summarized our hypotheses regarding the responsible drivers of the increased prescription opioid misuse in rural areas. We posited that increases could, in part, be attributed to (1) increased sales of opioid analgesics in rural areas that lead to greater availability for nonmedical use through drug diversion networks, (2) out-migration of upwardly mobile young adults from rural areas that increases economic deprivation and creates an aggregation of young adults at high risk for drug use, (3) tight kinship and social networks that allow faster diffusion of nonmedical prescription opioids among those at risk, and (4) increasing economic deprivation and unemployment that create a stressful environment that places individuals at risk for drug use. These factors interact in dynamic ways with identified risk factors that are not unique to nonmedical prescription opioid use to lead to epidemics of prescription opioid use and associated injury in rural areas.
Four Factors That Explain Increases in Nonmedical Prescription Opioid Misuse in Rural More Than Urban Areas
| 1. Increased sales of opioid analgesics in rural areas lead to greater availability for nonmedical use through diversion. |
| 2. Out-migration of upwardly mobile young adults from rural areas increases economic deprivation and creates an aggregation of young adults at high risk for drug use. |
| 3. Tight kinship and social networks allow faster diffusion of nonmedical prescription opioids among those at risk. |
| 4. Increasing economic deprivation and unemployment create a stressful environment that places individuals at risk. |
The hypotheses we have proposed do not explain all the observed patterns of nonmedical prescription opioid use and overdose. For example, states such as Florida and Washington have relatively high rates of nonmedical prescription opioid overdose but are largely urban, whereas Iowa and North Dakota have relatively low rates despite substantial rural areas11,18,128; thus, the mapping of rural geographical area to increases in nonmedical prescription opioid overdose is not linear.
Furthermore, demographic factors in both urban and rural areas likely interact with the factors we have mentioned in ways that remain to be elaborated. For example, Black and Hispanic individuals face the same if not greater stress because of economic hardship than do Whites and yet have lower overall rates of nonmedical prescription opioid use.52,53 The intersection of demographic factors such as race and ethnicity with drug and alcohol use remains among the unexplained anomalies in the epidemiological literature on substance use.129
Finally, although we focused on prescription opioids, there is growing evidence that the abuse of other prescription drugs such as stimulants and benzodiazepines is also increasing,57,125 especially among adolescents and young adults.82 Understanding the distinctions among underlying risk factors for misuse of distinct types of prescription drugs is an important public health priority, as prevention and intervention strategies may differ depending on the type of drug.
The differences in drug use between urban and rural areas are just 1 example of how macrolevel forces shape population-level patterns of drug use. A comprehensive understanding of why, for example, rates of alcohol and drug use differ across time, across countries, in countries across states, and across certain population subgroups is critical and understudied. Social norms, cultural traditions, attitudes, availability, and policies are all likely critical to understanding broad differences in prevalence of substance use across areas,21,36,51,130 yet few efforts have been made to comprehensively collect this information across time and across geographical spaces to examine the influence and the interaction of these factors with more microlevel determinants such as families, peers, and genetics.
We suggest that a strategic comparison between groups with different outcomes is an important way forward for the study of macrolevel influences on substance use. We have demonstrated that comparing urban and rural drug use is one way to find variation in structural factors that affect individual-level risk, yet empirical data to test our model remain critical.
National studies with sufficient sample sizes of urban and rural adolescents, young adults, and older adults with information on the economic and social characteristics of geographical spaces such as counties and neighborhoods are needed to advance this literature. Furthermore, the incorporation of novel methods such as agent-based or other generative modeling12,124 would be useful to correctly develop empirical tests in the context of a dynamic social and political space where individuals interact in networks and with their surroundings.
The crisis of nonmedical use of prescription opioids is an important public health priority, and the greatest public health threat remains concentrated in rural, low-income areas of the United States. Responding to this threat requires new theories from which new hypotheses can be developed and new data and methods that can be used to test novel hypotheses. Increased understanding of spatial factors is critical for developing a better model for the etiology of substance use considering the importance of physical setting, as well as for identifying points of intervention and prevention at a population level.
Acknowledgments
This research was funded by the National Institute of Alcohol Abuse and Alcoholism (grant K01AA021511 to K. M. K.), the National Institute on Drug Abuse (grants K01DA030449-01 to M. C.; R21DA029670 to J. E. B.; R01DA033862, R01DA024598 to J. R. H.), and the Centers for Disease Control and Prevention (grant 1R49CE002096-01 to J. E. B).
Human Participant Protection
No protocol approval was necessary because no human participants were involved in this study.
References
- 1.National Institute on Drug Abuse. Prescription Drugs: Abuse and Addiction. Washington, DC: US Department of Health and Human Services; 2011. [Google Scholar]
- 2.Warner M, Chen LH, Makuc DM. Increase in Fatal Poisonings Involving Opioid Analgesics in the United States, 1999–2006. Hyattsville, MD: National Center for Health Statistics; 2009. [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration. Results From the 2010 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: 2011. [Google Scholar]
- 4.Blanco C, Alderson D, Ogburn E et al. Changes in the prevalence of non-medical prescription drug use and drug use disorders in the United States: 1991–1992 and 2001–2002. Drug Alcohol Depend. 2007;90(2–3):252–260. doi: 10.1016/j.drugalcdep.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. College on Problems of Drug Dependence taskforce on prescription opioid non-medical use and abuse: position statement. Drug Alcohol Depend. 2003;69(3):215–232. doi: 10.1016/s0376-8716(03)00003-6. [DOI] [PubMed] [Google Scholar]
- 6.Gilson AM, Ryan KM, Joranson DE, Dahl JL. A reassessment of trends in the medical use and abuse of opioid analgesics and implications for diversion control: 1997–2002. J Pain Symptom Manage. 2004;28(2):176–188. doi: 10.1016/j.jpainsymman.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Joranson DE, Ryan KM, Gilson AM, Dahl JL. Trends in medical use and abuse of opioid analgesics. JAMA. 2000;283(13):1710–1714. doi: 10.1001/jama.283.13.1710. [DOI] [PubMed] [Google Scholar]
- 8.Paulozzi LJ. Opioid analgesic involvement in drug abuse deaths in American metropolitan areas. Am J Public Health. 2006;96(10):1755–1757. doi: 10.2105/AJPH.2005.071647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15(9):618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- 10.Paulozzi LJ, Ryan GW. Opioid analgesics and rates of fatal drug poisoning in the United States. Am J Prev Med. 2006;31(6):506–511. doi: 10.1016/j.amepre.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 11.Paulozzi LJ, Xi Y. Recent changes in drug poisoning mortality in the United States by urban–rural status and by drug type. Pharmacoepidemiol Drug Saf. 2008;17(10):997–1005. doi: 10.1002/pds.1626. [DOI] [PubMed] [Google Scholar]
- 12.Diez Roux AV. Complex systems thinking and current impasses in health disparities research. Am J Public Health. 2011;101(9):1627–1634. doi: 10.2105/AJPH.2011.300149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Havens JR, Oser CB, Leukefeld CG et al. Differences in prevalence of prescription opiate misuse among rural and urban probationers. Am J Drug Alcohol Abuse. 2007;33(2):309–317. doi: 10.1080/00952990601175078. [DOI] [PubMed] [Google Scholar]
- 14.US Census Bureau. Metropolitan and micropolitan statistical areas main. 2013. Available at: http://www.census.gov/population/metro. Accessed November 7, 2013.
- 15.Wunsch MJ, Nakamoto K, Behonick G, Massello W. Opioid deaths in rural Virginia: a description of the high prevalence of accidental fatalities involving prescribed medications. Am J Addict. 2009;18(1):5–14. doi: 10.1080/10550490802544938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cicero TJ, Surratt H, Inciardi JA, Munoz A. Relationship between therapeutic use and abuse of opioid analgesics in rural, suburban, and urban locations in the United States. Pharmacoepidemiol Drug Saf. 2007;16(8):827–840. doi: 10.1002/pds.1452. [DOI] [PubMed] [Google Scholar]
- 17.McCauley JL, Danielson CK, Amstadter AB et al. The role of traumatic event history in non-medical use of prescription drugs among a nationally representative sample of US adolescents. J Child Psychol Psychiatry. 2010;51(1):84–93. doi: 10.1111/j.1469-7610.2009.02134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Drug overdose deaths—Florida, 2003–2009. MMWR Morb Mortal Wkly Rep. 2011;60(26):659–672. [PubMed] [Google Scholar]
- 19.Dew B, Elifson K, Dozier M. Social and environmental factors and their influence on drug use vulnerability and resiliency in rural populations. J Rural Health. 2007;23(suppl):16–21. doi: 10.1111/j.1748-0361.2007.00119.x. [DOI] [PubMed] [Google Scholar]
- 20.Havens JR, Young AM, Havens CE. Nonmedical prescription drug use in a nationally representative sample of adolescents: evidence of greater use among rural adolescents. Arch Pediatr Adolesc Med. 2011;165(3):250–255. doi: 10.1001/archpediatrics.2010.217. [DOI] [PubMed] [Google Scholar]
- 21.Galea S, Ahern J, Vlahov D. Contextual determinants of drug use risk behavior: a theoretic framework. J Urban Health. 2003;80(4, suppl 3):iii50–iii58. doi: 10.1093/jurban/jtg082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zinberg NE. Drug, Set, and Setting. New Haven, CT: Yale University Press; 1984. [Google Scholar]
- 23.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol. 2001;30(4):668–677. doi: 10.1093/ije/30.4.668. [DOI] [PubMed] [Google Scholar]
- 24.Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 25.Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol Rev. 2004;26:36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- 26.Cerdá M, Tracy M, Messner SF, Vlahov D, Tardiff K, Galea S. Misdemeanor policing, physical disorder, and gun-related homicide: a spatial analytic test of “broken-windows” theory. Epidemiology. 2009;20(4):533–541. doi: 10.1097/EDE.0b013e3181a48a99. [DOI] [PubMed] [Google Scholar]
- 27.Nandi A, Glass TA, Cole SR et al. Neighborhood poverty and injection cessation in a sample of injection drug users. Am J Epidemiol. 2010;171(4):391–398. doi: 10.1093/aje/kwp416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nandi A, Galea S, Ahern J, Bucciarelli A, Vlahov D, Tardiff K. What explains the association between neighborhood-level income inequality and the risk of fatal overdose in New York City? Soc Sci Med. 2006;63(3):662–674. doi: 10.1016/j.socscimed.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Crawford ND, Ford C, Galea S, Latkin C, Jones KC, Fuller CM. The relationship between perceived discrimination and high-risk social ties among illicit drug users in New York City, 2006–2009. AIDS Behav. 2012;17(1):419–426. doi: 10.1007/s10461-012-0201-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Furr-Holden CD, Milam AJ, Reynolds EK, Macpherson L, Lejuez CW. Disordered neighborhood environments and risk-taking propensity in late childhood through adolescence. J Adolesc Health. 2012;50(1):100–102. doi: 10.1016/j.jadohealth.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Suglia SF, Staudenmayer J, Cohen S, Enlow MB, Rich-Edwards JW, Wright RJ. Cumulative stress and cortisol disruption among Black and Hispanic pregnant women in an urban cohort. Psychol Trauma. 2010;2(4):326–334. doi: 10.1037/a0018953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sheridan MJ. A proposed intergenerational model of substance abuse, family functioning, and abuse/neglect. Child Abuse Negl. 1995;19(5):519–530. doi: 10.1016/0145-2134(95)00012-w. [DOI] [PubMed] [Google Scholar]
- 33.Anderson AR, Henry CS. Family system characteristics and parental behaviors as predictors of adolescent substance use. Adolescence. 1994;29(114):405–420. [PubMed] [Google Scholar]
- 34.Klagsbrun M, Davis DI. Substance abuse and family interaction. Fam Process. 1977;16(2):149–173. doi: 10.1111/j.1545-5300.1977.00149.x. [DOI] [PubMed] [Google Scholar]
- 35.Ledoux S, Miller P, Choquet M, Plant M. Family structure, parent–child relationships, and alcohol and other drug use among teenagers in France and the United Kingdom. Alcohol Alcohol. 2002;37(1):52–60. doi: 10.1093/alcalc/37.1.52. [DOI] [PubMed] [Google Scholar]
- 36.Brown SA, McGue M, Maggs J et al. A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics. 2008;121(suppl 4):S290–S310. doi: 10.1542/peds.2007-2243D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kandel D. Adolescent marihuana use: role of parents and peers. Science. 1973;181(4104):1067–1070. doi: 10.1126/science.181.4104.1067. [DOI] [PubMed] [Google Scholar]
- 38.Smith KP, Christakis NA. Social networks and health. Annu Rev Sociol. 2008;34:405–429. [Google Scholar]
- 39.Dick DM, Agrawal A. The genetics of alcohol and other drug dependence. Alcohol Res Health. 2008;31(3):111–118. [PMC free article] [PubMed] [Google Scholar]
- 40.Urban NB, Martinez D. Neurobiology of addiction: insight from neurochemical imaging. Psychiatr Clin North Am. 2012;35(2):521–541. doi: 10.1016/j.psc.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 41.Hillemacher T. Biological mechanisms in alcohol dependence—new perspectives. Alcohol Alcohol. 2011;46(3):224–230. doi: 10.1093/alcalc/agr026. [DOI] [PubMed] [Google Scholar]
- 42.Rahman S. Brain nicotinic receptors as emerging targets for drug addiction: neurobiology to translational research. Prog Mol Biol Transl Sci. 2011;98:349–365. doi: 10.1016/B978-0-12-385506-0.00008-9. [DOI] [PubMed] [Google Scholar]
- 43.Volkow ND, Wang GJ, Fowler JS, Tomasi D, Telang F, Baler R. Addiction: decreased reward sensitivity and increased expectation sensitivity conspire to overwhelm the brain’s control circuit. Bioessays. 2010;32(9):748–755. doi: 10.1002/bies.201000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dayan J, Bernard A, Olliac B, Mailhes AS, Kermarrec S. Adolescent brain development, risk-taking and vulnerability to addiction. J Physiol Paris. 2010;104(5):279–286. doi: 10.1016/j.jphysparis.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 45.Keyes KM, Keyes MA, March D, Susser E. Levels of risk: maternal-, middle childhood-, and neighborhood-level predictors of adolescent disinhibitory behaviors from a longitudinal birth cohort in the United States. Ment Health Subst Use. 2011;4(1):22–37. doi: 10.1080/17523281.2011.533445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fenton MC, Keyes K, Geier T et al. Psychiatric comorbidity and the persistence of drug use disorders in the United States. Addiction. 2011;107(3):599–609. doi: 10.1111/j.1360-0443.2011.03638.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 48.Keyes KM, Martins SS, Hasin DS. Past 12-month and lifetime comorbidity and poly-drug use of ecstasy users among young adults in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2008;97(1–2):139–149. doi: 10.1016/j.drugalcdep.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 50.Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005;66(6):677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- 51.Keyes KM, Schulenberg JE, O’Malley PM et al. The social norms of birth cohorts and adolescent marijuana use in the United States, 1976–2007. Addiction. 2011;106(10):1790–1800. doi: 10.1111/j.1360-0443.2011.03485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ghandour LA, Martins SS, Chilcoat HD. Understanding the patterns and distribution of opioid analgesic dependence symptoms using a latent empirical approach. Int J Methods Psychiatr Res. 2008;17(2):89–103. doi: 10.1002/mpr.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Martins SS, Storr CL, Zhu H, Chilcoat HD. Correlates of extramedical use of OxyContin versus other analgesic opioids among the US general population. Drug Alcohol Depend. 2009;99(1–3):58–67. doi: 10.1016/j.drugalcdep.2008.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Edlund MJ, Martin BC, Fan MY, Devries A, Braden JB, Sullivan MD. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP study. Drug Alcohol Depend. 2010;112(1–2):90–98. doi: 10.1016/j.drugalcdep.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sung HE, Richter L, Vaughan R, Johnson PB, Thom B. Nonmedical use of prescription opioids among teenagers in the United States: trends and correlates. J Adolesc Health. 2005;37(1):44–51. doi: 10.1016/j.jadohealth.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 56.Hall MT, Howard MO, McCabe SE. Prescription drug misuse among antisocial youths. J Stud Alcohol Drugs. 2010;71(6):917–924. doi: 10.15288/jsad.2010.71.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McCabe SE, Cranford JA, West BT. Trends in prescription drug abuse and dependence, co-occurrence with other substance use disorders, and treatment utilization: results from two national surveys. Addict Behav. 2008;33(10):1297–1305. doi: 10.1016/j.addbeh.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Martins SS, Fenton MC, Keyes KM, Blanco C, Zhu H, Storr CL. Mood/anxiety disorders and their association with non-medical prescription opioid use and prescription opioid use disorder: longitudinal evidence from the National Epidemiologic Study on Alcohol and Related Conditions. Psychol Med. 2012;42(6):1261–1272. doi: 10.1017/S0033291711002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Martins SS, Keyes KM, Storr CL, Zhu H, Chilcoat HD. Pathways between nonmedical opioid use/dependence and psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2009;103(1–2):16–24. doi: 10.1016/j.drugalcdep.2009.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boyd CJ, Teter CJ, West BT, Morales M, McCabe SE. Non-medical use of prescription analgesics: a three-year national longitudinal study. J Addict Dis. 2009;28(3):232–242. doi: 10.1080/10550880903028452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McCabe SE, Boyd CJ, Young A. Medical and nonmedical use of prescription drugs among secondary school students. J Adolesc Health. 2007;40(1):76–83. doi: 10.1016/j.jadohealth.2006.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McCabe SE, Teter CJ, Boyd CJ, Knight JR, Wechsler H. Nonmedical use of prescription opioids among U.S. college students: prevalence and correlates from a national survey. Addict Behav. 2005;30(4):789–805. doi: 10.1016/j.addbeh.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 63.Department of Justice Drug Enforcement Administration. Automation of reports and consolidated orders system. Available at: http://www.deadiversion.usdoj.gov/arcos. Accessed November 7, 2013.
- 64.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 65.Mularski RA, White-Chu F, Overbay D, Miller L, Asch SM, Ganzini L. Measuring pain as the 5th vital sign does not improve quality of pain management. J Gen Intern Med. 2006;21(6):607–612. doi: 10.1111/j.1525-1497.2006.00415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lorenz KA, Sherbourne CD, Shugarman LR et al. How reliable is pain as the fifth vital sign? J Am Board Fam Med. 2009;22(3):291–298. doi: 10.3122/jabfm.2009.03.080162. [DOI] [PubMed] [Google Scholar]
- 67.Rosenblum A, Marsch LA, Joseph H, Portenoy RK. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol. 2008;16(5):405–416. doi: 10.1037/a0013628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Inciardi JA, Surratt HL, Cicero TJ, Beard RA. Prescription opioid abuse and diversion in an urban community: the results of an ultrarapid assessment. Pain Med. 2009;10(3):537–548. doi: 10.1111/j.1526-4637.2009.00603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Inciardi JA, Surratt HL, Cicero TJ, Kurtz SP, Martin SS, Parrino MW. The “black box” of prescription drug diversion. J Addict Dis. 2009;28(4):332–347. doi: 10.1080/10550880903182986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ward L, Patel NM, Hanlon A, Eldakar-Hein S, Sherlinski K, Ward SH. Prescription medication borrowing among adult patients at an urban medical center. J Urban Health. 2011;88(6):997–1014. doi: 10.1007/s11524-011-9589-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Carise D, Dugosh KL, McLellan AT, Camilleri A, Woody GE, Lynch KG. Prescription OxyContin abuse among patients entering addiction treatment. Am J Psychiatry. 2007;164(11):1750–1756. doi: 10.1176/appi.ajp.07050252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Green TC, Grimes Serrano JM, Licari A, Budman SH, Butler SF. Women who abuse prescription opioids: findings from the Addiction Severity Index-Multimedia Version Connect prescription opioid database. Drug Alcohol Depend. 2009;103(1–2):65–73. doi: 10.1016/j.drugalcdep.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Inciardi JA, Surratt HL, Cicero TJ et al. Prescription drugs purchased through the Internet: who are the end users? Drug Alcohol Depend. 2010;110(1–2):21–29. doi: 10.1016/j.drugalcdep.2010.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hempstead K. Manner of death and circumstances in fatal poisonings: evidence from New Jersey. Inj Prev. 2006;12(suppl 2):ii44–ii48. doi: 10.1136/ip.2006.012583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hall AJ, Logan JE, Toblin RL et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300(22):2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- 76.Toblin RL, Paulozzi LJ, Logan JE, Hall AJ, Kaplan JA. Mental illness and psychotropic drug use among prescription drug overdose deaths: a medical examiner chart review. J Clin Psychiatry. 2010;71(4):491–496. doi: 10.4088/JCP.09m05567blu. [DOI] [PubMed] [Google Scholar]
- 77.Forrester MB. Ingestions of hydrocodone, carisoprodol, and alprazolam in combination reported to Texas poison centers. J Addict Dis. 2011;30(2):110–115. doi: 10.1080/10550887.2011.554778. [DOI] [PubMed] [Google Scholar]
- 78.Substance Abuse and Mental Health Services Administration. Drug abuse warning network. 2012. Available at: http://www.samhsa.gov/data/DAWN.aspx. Accessed November 7, 2013. [PubMed]
- 79.Substance Abuse and Mental Health Services Administration. National Household Survey on Drug Abuse. 2011. Available at: http://oas.samhsa.gov/nsduh.htm. Accessed November 7, 2013.
- 80.National Drug Intelligence Center. National drug threat assessment. 2011. Available at: http://www.justice.gov/archive/ndic/pubs44/44849/44849p.pdf. Accessed November 7, 2013.
- 81.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers—United States, 2002–2004 and 2008–2010. Drug Alcohol Depend. 2013;132(1–2):95–100. doi: 10.1016/j.drugalcdep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 82. Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future. National Survey Results on Drug Use, 1975–2009. Vol. 2: College Students and Adults Ages 19–50. Bethesda, MD: National Institute on Drug Abuse; 2010. NIH Publication 10–7585.
- 83.Foltin RW, Fischman MW. Self-administration of cocaine by humans: choice between smoked and intravenous cocaine. J Pharmacol Exp Ther. 1992;261(3):841–849. [PubMed] [Google Scholar]
- 84.Des Jarlais DC, Arasteh K, Perlis T et al. The transition from injection to non-injection drug use: long-term outcomes among heroin and cocaine users in New York City. Addiction. 2007;102(5):778–785. doi: 10.1111/j.1360-0443.2007.01764.x. [DOI] [PubMed] [Google Scholar]
- 85.Young AM, Havens JR, Leukefeld CG. Route of administration for illicit prescription opioids: a comparison of rural and urban drug users. Harm Reduct J. 2010;7:24. doi: 10.1186/1477-7517-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Young AM, Havens JR. Transition from first illicit drug use to first injection drug use among rural Appalachian drug users: a cross-sectional comparison and retrospective survival analysis. Addiction. 2012;107(3):587–596. doi: 10.1111/j.1360-0443.2011.03635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 vs. 2000. Pain. 2004;109(3):514–519. doi: 10.1016/j.pain.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 88.Boudreau D, Von Korff M, Rutter CM et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf. 2009;18(12):1166–1175. doi: 10.1002/pds.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Havens JR, Walker R, Leukefeld CG. Prescription opioid use in the rural Appalachia: a community-based study. J Opioid Manag. 2008;4(2):63–71. doi: 10.5055/jom.2008.0010. [DOI] [PubMed] [Google Scholar]
- 90.McDonald DC, Carlson K, Izrael D. Geographic variation in opioid prescribing in the US. J Pain. 2012;13(10):988–996. doi: 10.1016/j.jpain.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Barnard A. Prescription drug abuse: Florida’s health crisis. Presented at the American Medical Association State Legislative Strategy Conference; January 3–5, 2013; Aventura, Florida. Available at: http://www.ama-assn.org/resources/doc/arc/no-index/2013-01-04-drug-diversion-abuse-benard.pdf. Accessed November 7, 2013.
- 92.Wininger PJ. Pharmaceutical overpromotion liability: the legal battle over rural prescription drug abuse. KY Law J. 2005;93(1):269. [Google Scholar]
- 93.Glasgow N. Rural/urban patterns of aging and caregiving in the United States. J Fam Issues. 2000;21(5):611–631. [Google Scholar]
- 94.Hunsucker SC, Frank DI, Flannery J. Meeting the needs of rural families during critical illness: the APN’s role. Dimens Crit Care Nurs. 1999;18(3):24–32. doi: 10.1097/00003465-199905000-00004. [DOI] [PubMed] [Google Scholar]
- 95.Hoffman PK, Meier BP, Council JR. A comparison of chronic pain between an urban and rural population. J Community Health Nurs. 2002;19(4):213–224. doi: 10.1207/S15327655JCHN1904_02. [DOI] [PubMed] [Google Scholar]
- 96.Leff M, Stallones L, Keefe TJ, Rosenblatt R, Reeds M. Comparison of urban and rural non-fatal injury: the results of a statewide survey. Inj Prev. 2003;9(4):332–337. doi: 10.1136/ip.9.4.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Coben JH, Tiesman HM, Bossarte RM, Furbee PM. Rural–urban differences in injury hospitalizations in the US, 2004. Am J Prev Med. 2009;36(1):49–55. doi: 10.1016/j.amepre.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 98.Leukefeld CG, Walker R, Havens JR, Leedham VT. What does the community say: key informant perceptions of rural prescription drug use. J Drug Issues. 2007;37(3):503–524. [Google Scholar]
- 99.Inciardi JA, Surratt HL, Kurtz SP, Cicero TJ. Mechanisms of prescription drug diversion among drug-involved club- and street-based populations. Pain Med. 2007;8(2):171–183. doi: 10.1111/j.1526-4637.2006.00255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.US Census Bureau. 2010 census data. Available at: http://www.census.gov/2010census/data. Accessed November 7, 2013.
- 101.Rupasingha A, Goetz SJ, Freshwater D. Social and institutional factors as determinants of economic growth: evidence from the United States counties. Pap Reg Sci. 2002;81(2):139–155. [Google Scholar]
- 102.McGranahan DA. How people make a living in rural America. In: Brown DL, Swanson LE, Barton AW, editors. Challenges for Rural America in the Twenty-First Century. University Park, PA; Pennsylvania State University Press: 2004. pp. 135–151. [Google Scholar]
- 103.Blackwell DL, McLaughlin DK. Do rural youth attain their educational goals? Rural Development Perspectives. 1999;12(2):37–44. [Google Scholar]
- 104.Roscigno VJ, Crowley ML. Rurality, institutional disadvantage, and achievement/attainment. Rural Sociol. 2001;66(2):268–292. [Google Scholar]
- 105.DeYoung AJ. Rural Education: Issues and Practice. New York, NY: Garland Publishing; 1991. [Google Scholar]
- 106.Beggs J, Haines V, Hurlbert J. Revisiting the rural–urban contrast: personal networks in nonmetropolitan and metropolitan settings. Rural Sociol. 1996;61(2):306–325. [Google Scholar]
- 107.Conger RD, Elder GH. Families in Troubled Times: Adapting to Change in Rural America. Hawthorne, NY: Aldine Transaction; 1994. [Google Scholar]
- 108.Turcotte M. Social engagement and civic participation: are rural and small town populations really at an advantage? Rural Small Town Can Anal Bull. 2005;6(4):1–24. [Google Scholar]
- 109.Singh K, Dika S. The educational effects of rural adolescents’ social networks. J Res Rural Educ. 2003;18(2):114–128. [Google Scholar]
- 110.Costa DL, Kahn ME. Civic engagement and community heterogeneity: an economist’s perspective. Perspect Polit. 2003;1:103–111. [Google Scholar]
- 111.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Glasgow N. The Nonmetro Elderly: Economic and Demographic Status. Washington, DC: US Department of Agriculture, Economic Research Service; 1988. Rural Development Research Report 70. [Google Scholar]
- 113.Jonas AB, Young AM, Oser CB, Leukefeld CG, Havens JR. OxyContin(R) as currency: OxyContin(R) use and increased social capital among rural Appalachian drug users. Soc Sci Med. 2012;74(10):1602–1609. doi: 10.1016/j.socscimed.2011.12.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Partidge MD, Rickman DS. High-poverty nonmetropolitan counties in America: can economic development help? Int Reg Sci Rev. 2005;28:415–440. [Google Scholar]
- 115.Fuller CM, Borrell LN, Latkin CA et al. Effects of race, neighborhood, and social network on age at initiation of injection drug use. Am J Public Health. 2005;95(4):689–695. doi: 10.2105/AJPH.2003.02178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Galea S, Ahern J, Tracy M, Vlahov D. Neighborhood income and income distribution and the use of cigarettes, alcohol, and marijuana. Am J Prev Med. 2007;32(6, suppl):S195–S202. doi: 10.1016/j.amepre.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hembree C, Galea S, Ahern J et al. The urban built environment and overdose mortality in New York City neighborhoods. Health Place. 2005;11(2):147–156. doi: 10.1016/j.healthplace.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 118.Messner SF. Economic inequality and levels of homicide: an analysis of urban neighborhoods. Criminology. 1985;24(2):297–317. [Google Scholar]
- 119.Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. J Health Soc Behav. 2001;42(2):151–165. [PubMed] [Google Scholar]
- 120.Cerdá M, Buka SL, Rich-Edwards JW. Neighborhood influences on the association between maternal age and birthweight: a multilevel investigation of age-related disparities in health. Soc Sci Med. 2008;66(9):2048–2060. doi: 10.1016/j.socscimed.2008.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Duncan SC, Duncan TE, Strycker LA. A multilevel analysis of neighborhood context and youth alcohol and drug problems. Prev Sci. 2002;3(2):125–133. doi: 10.1023/a:1015483317310. [DOI] [PubMed] [Google Scholar]
- 122.Hannon L, Cuddy MM. Neighborhood ecology and drug dependence mortality: an analysis of New York City census tracts. Am J Drug Alcohol Abuse. 2006;32(3):453–463. doi: 10.1080/00952990600753966. [DOI] [PubMed] [Google Scholar]
- 123.Cerdá M, Diez-Roux AV, Tchetgen ET, Gordon-Larsen P, Kiefe C. The relationship between neighborhood poverty and alcohol use: estimation by marginal structural models. Epidemiology. 2010;21(4):482–489. doi: 10.1097/EDE.0b013e3181e13539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Galea S, Riddle M, Kaplan GA. Causal thinking and complex system approaches in epidemiology. Int J Epidemiol. 2010;39(1):97–106. doi: 10.1093/ije/dyp296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gorevski E, Bian B, Kelton CM, Martin Boone JE, Guo JJ. Utilization, spending, and price trends for benzodiazepines in the US Medicaid program: 1991–2009. Ann Pharmacother. 2012;46(4):503–512. doi: 10.1345/aph.1Q618. [DOI] [PubMed] [Google Scholar]
- 126.Topel R. What have we learned from empirical studies of unemployment and turnover? Am Econ Rev. 1993;83(2):110–115. [Google Scholar]
- 127.Bluestone B. The great U-turn revisited: economic restructuring, jobs, and the redistribution of earnings. In: Kasarda JD, editor. Jobs, Earnings, and Employment Growth Policies in the United States. Boston, MA: Kluwer Academic Publishers; 1990. pp. 7–43. [Google Scholar]
- 128.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 129.Keyes KM, Liu XC, Cerda M. The role of race/ethnicity in alcohol-attributable injury in the United States. Epidemiol Rev. 2012;34(1):89–102. doi: 10.1093/epirev/mxr018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ahern J, Galea S, Hubbard A, Midanik L, Syme SL. “Culture of drinking” and individual problems with alcohol use. Am J Epidemiol. 2008;167(9):1041–1049. doi: 10.1093/aje/kwn022. [DOI] [PMC free article] [PubMed] [Google Scholar]