Abstract
Objectives. We compared prevalence, severity, and specific symptom profiles for nicotine withdrawal across categories of mental illness. We also examined the influence of nicotine withdrawal on efforts to quit smoking among those with mental illness.
Methods. We analyzed data from 2 sources: wave 1 of the National Epidemiologic Survey on Alcohol and Related Conditions, limiting the sample to current smokers (2001–2002; n = 9913); and a 2-wave cohort telephone survey of a national sample of adult smokers (2004–2006; n = 751).
Results. Mental illness was associated with a substantially greater likelihood of nicotine withdrawal syndrome; approximately 44% of nicotine withdrawal syndrome diagnoses were attributable to mental illness. Symptom profiles were highly comparable between mental illness categories, although anxiety-related symptoms were better markers of withdrawal for those with an internalizing disorder. Smokers with mental illness were motivated to quit but were less likely to be successful in their quit attempts, and both dependence and withdrawal independently accounted for this lower likelihood of success.
Conclusions. Nicotine withdrawal may be a particularly important target for intervention among those with mental illness who smoke cigarettes.
Individuals with mental illness are more likely to smoke cigarettes, are more dependent on nicotine, and have greater difficulty quitting smoking1,2 than are those without mental illness. The prevalence of mental illness in the United States is approximately 28%; yet, smokers with mental illness consume 40%–50% of cigarettes.1,2 A self-medication hypothesis has largely driven the conceptualization of this issue3–8: smoking is initiated and maintained to reduce psychiatric symptoms, and these symptoms are exacerbated during abstinence. This notion, that smoking can be important for symptom self-management, has likely contributed to smoking disparities between those with and those without mental illness.3 There are effective means of treating smoking for those with mental illness9; however, nontreatment remains the norm.10 A growing body of researchers, clinicians, and policymakers has called for a paradigm shift in how we approach this issue.3,11–13 Smoking is becoming increasingly viewed as a preventable and treatable cause of diminished life quality among those with mental illness,3,12 rather than a necessary form of self-medication.
A 2008 National Institute of Mental Health report noted that the focus on a self-medication hypothesis has come at the expense of research on other important facets of smoking, particularly nicotine withdrawal.3 Studies have found that cigarette smokers with mental illness may experience more severe nicotine withdrawal symptoms14,15; however, these studies were conducted among small samples with a limited range of diagnoses. Weinberger et al. conducted an investigation using data from a US nationally representative sample of cigarette smokers and found that those with mental illness were more likely to report nicotine withdrawal symptoms and life problems associated with their withdrawal.16 Weinberger et al. focused on a few particular diagnoses; thus, they did not investigate the overall extent to which nicotine withdrawal is an issue among those with mental illness or comparisons of nicotine withdrawal between mental illness diagnoses. Previous research on this topic has also been limited in that specific nicotine withdrawal symptom profiles have not been compared across mental illness diagnoses. This type of analysis will potentially highlight specific nicotine withdrawal symptom targets for intervention. Finally, it remains unclear whether nicotine withdrawal in itself is associated with lower likelihood of quit success among those with mental illness or whether nicotine withdrawal is simply an extension of greater nicotine dependence among those with mental illness.
We conducted 2 studies of nicotine withdrawal, mental illness, and tobacco cessation. In the first, we compared the likelihood of being diagnosed with a nicotine withdrawal syndrome and the severity of nicotine withdrawal symptoms between smokers with and those without mental illness and across mental illness diagnoses. We then estimated the proportions of nicotine withdrawal syndrome in the population of smokers attributable to each mental illness category. We compared nicotine withdrawal symptom profiles between mental illness categories to better understand consistencies and differences in specific nicotine withdrawal symptoms.
In the second study, we examined whether smokers with mental illness were more or less motivated to quit smoking and more or less likely to make quit attempts. Among smokers who made a quit attempt, we examined whether those with mental illness were more or less likely to successfully stop using tobacco and how nicotine withdrawal and dependence influenced cessation efforts.
METHODS
We analyzed data from wave 1 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). A detailed description of this study can be found elsewhere.17 Briefly, the first wave of NESARC data was collected during 2001 and 2002. The response rate was 81%, and the sample of 43 093 represented the civilian, noninstitutionalized adult population in the United States. Surveys were administered face-to-face, using computer-assisted personal interviews. African Americans, Hispanics, and young adults were oversampled, and the data were weighted to adjust for nonresponse at the household and personal levels. We used subpopulation frequency estimates from the 2000 Decennial Census to adjust the data on sociodemographic variables to ensure an accurate representation of the US population. We limited the sample to those who smoked 100 cigarettes during their lifetime and smoked during the past year (n = 9913). Mean age for the sample was 40.7 years (SE = 0.11), 53.7% were male, and 75.0% were non-Hispanic White.
Study 1 Measures
Mental illness.
We assessed mental illness diagnoses with the Alcohol Use Disorder and Associated Disabilities Interview Schedule, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV).18,19 One of our primary objectives was to create mutually exclusive diagnostic categories of mental illness to accurately and parsimoniously compare those with mental illness with those without mental illness. To create theoretically sound diagnostic groupings while limiting our groups to a statistically manageable number, we categorized diagnoses into those manifesting from internalizing and externalizing latent processes and those with a psychotic component. We derived the internalizing and externalizing spectrum classifications from a large body of research demonstrating the theoretical validity of these constructs.20–25
Internalizing disorders included past year mood and anxiety disorders, whereas externalizing disorders included past year alcohol use disorders and drug use disorders and lifetime antisocial personality disorder. Because of the relatively low prevalence of psychotic disorders in the general population, individual disorders were not assessed with the Alcohol Use Disorder and Associated Disabilities Interview Schedule, DSM-IV measure. Instead, respondents were asked, “Did a doctor or other health professional ever tell you that you had schizophrenia or a psychotic illness or episode” and then, “Did this happen in the past 12 months?” We used affirmative responses to the latter question as a marker for a 12-month psychotic disorder or episode diagnosis. On the basis of these classifications, we created a categorical variable with 5 groups: (1) no disorder, (2) internalizing disorder only, (3) externalizing disorder only, (4) both internalizing disorder and externalizing disorder, and (5) psychotic episodes or disorders. Figure 1 displays the prevalence of these 4 mental illness groups in the NESARC sample. Of those in the psychotic episodes or disorders group, 23% did not have any comorbid internalizing or externalizing disorders; 34% had an externalizing disorder only; 6% had an internalizing disorder only; and 37% had both internalizing and externalizing disorders.
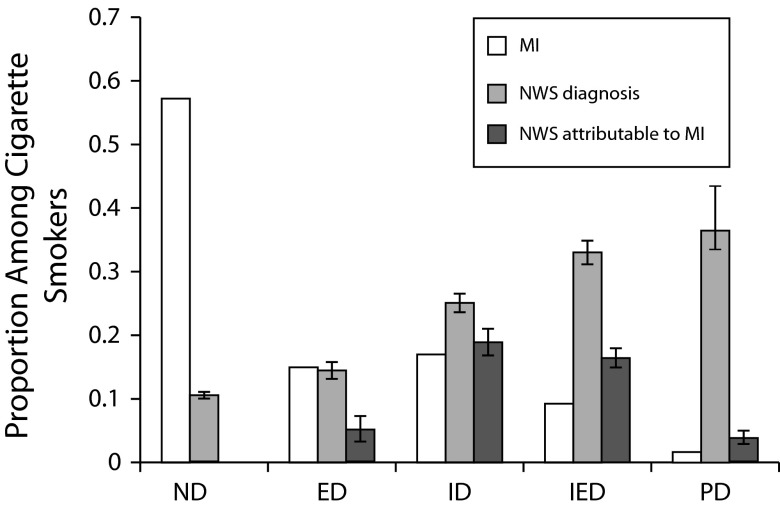
FIGURE 1—
Nicotine withdrawal syndrome (NWS) and mental illness (MI) among cigarette smokers (n = 9913 current smokers): the National Epidemiologic Survey on Alcohol and Related Conditions, 2001–2002.
Note. ED = externalizing disorder only; ID = internalizing disorder only; IED = internalizing and externalizing disorders; ND = no disorder; PD = psychotic episode or disorder. Error bars represent 95% confidence intervals. Nicotine withdrawal syndrome estimates are adjusted for gender, income, education, and age. Analyses accounted for the survey design, and we applied survey weights to generate nationally representative estimates.
Nicotine withdrawal.
Nicotine withdrawal symptoms were assessed with the following prompt: “Many people experience problems on occasions when they stop or cut down on their tobacco use. After stopping or cutting down on your tobacco use [during the past year], did you… .” The following 8 nicotine withdrawal symptoms were included in this measure: depression; difficulty falling or staying asleep; difficulty concentrating; increased appetite or weight gain; irritation, anger, or frustration; anxiety or nervousness; slowed heart rate; and restlessness. We created 2 summary variables: the first was a sum of the individual withdrawal items endorsed by respondents, ranging from 0 to 8, which we then recoded to a binary variable derived from a cutoff of 4 or more symptoms, consistent with the DSM-IV diagnosis of nicotine withdrawal syndrome.
Withdrawal-related distress.
For smokers who reported at least 2 of the aforementioned withdrawal symptoms, the NESARC interviewers assessed withdrawal-related distress with the following question: “You just mentioned that you had some experiences after stopping or cutting down on your tobacco use in the last 12 months. Were any of these experiences very uncomfortable or upsetting to you or did they cause problems in your life—like at work or school or with family or friends?” We utilized a binary variable representing whether respondents answered yes or no to this prompt.
Study 1 Analyses
We conducted all analyses using Stata, version 12.0.26 We first examined whether those with mental illness were more likely to be diagnosed with a nicotine withdrawal syndrome derived from the DSM-IV cutoff of 4 or more symptoms. We calculated risk ratios (RRs) using generalized linear models, specifying a binomial family and log-link function and accounting for the survey design. This included the application of sampling weights to generate nationally representative estimates. We adjusted the estimates for education, past year household income, gender, and age. We entered education into the model as a continuous variable, with values of 1–14 representing categories of no formal schooling to completed master’s degree or higher graduate degree. We used the same procedure for the income variable, with values of 1–21 representing from less than $5000 to $200 000. On the basis of these RR estimates, we calculated marginal probabilities of nicotine withdrawal syndrome for each diagnosis category.
We then used the RR estimates to calculate population-attributable fractions for each mental illness category, representing the fraction of nicotine withdrawal syndrome diagnoses in the population of smokers attributable to each mental illness category. In other words, the population-attributable fraction represents the proportion of nicotine withdrawal syndrome diagnoses attributable to each mental illness category after taking into account the base rate among those without mental illness.
Next, we examined whether those with mental illness were more likely to report nicotine withdrawal–related distress using generalized linear modeling and specifying a binomial family and log-link function. We adjusted estimates for the survey sampling design, income, education, gender, and age, and we applied sampling weights to generate nationally representative estimates.
We used item response theory analyses to examine differences in specific nicotine withdrawal symptoms that these mental illness categories reported.27 The following nicotine withdrawal symptoms were reported at wave 1: depression; difficulty falling or staying asleep; difficulty concentrating; increased appetite or weight gain; irritation, anger, or frustration; anxiety or nervousness; slowed heart rate; and restlessness. Item response theory analyses perform best if there is a single latent construct underlying the items in the analyses. To test this assumption, we first conducted factor analyses on the 8 withdrawal symptoms. The symptom slowed heart rate did not load well with the other symptoms (factor loading = 0.29), and we eliminated it from the item response theory analyses.
We conducted statistical comparisons between mental illness groups using differential item function analyses, testing the following null hypothesis: H0: agroup1 = agroup2 AND bgroup1 = bgroup2.28 For each item by group comparison, we calculated 2 logit models:
(1) f(Y) = b0 + b1θ + b2Group
(2) f(Y) = b0 + b1θ + b2Group + b3θXGroup
where Y represents whether the respondent endorsed a specific nicotine withdrawal symptom, θ is the ability parameter from the item response theory analyses, and Group is a dummy variable for the mental illness diagnoses being compared in the model. We then tested the significance of differences between these 2 models using a log-likelihood ratio test. We made 10 comparisons using this procedure for each item; thus, we used a Sidak correction for our α level to account for multiple comparisons. This resulted in a corrected α of 0.005.
Study 2 Procedures
We analyzed data from a 2-wave cohort, national telephone survey of US smokers aged 25 years or older who were sampled using equal probability random-digit dialing (Assessing Hardcore Smoking Survey, n = 751). In households with multiple eligible members, an individual was randomly selected for survey administration. A sample of n = 1000 current smokers and n = 256 former smokers (abstinent for ≤ 5 years) completed the computer-assisted telephone survey between May 2004 and March 2005 (46.0% response rate). Current smokers were then contacted for a follow-up interview 12–14 months after baseline. We included the n = 751 cigarette smokers who completed both waves of data collection (75.1% follow-up rate).
The baseline sample of current smokers had a mean age of 44.7 (SD = 12.9; range = 25–105) and a mean education level of 13–15 years. The sample consisted of 43.8% males, and 74.5% were White, non-Hispanic. Those lost to attrition were younger, were more likely to be of minority race/ethnicity, and had lower education levels than did those who completed the follow-up survey.
Study 2 Measures
Nonspecific psychological distress.
We measured mental illness using Kessler’s K6 screening tool, which has been well validated using the DSM-IV as a method of identifying individuals with nonspecific psychological distress in survey samples.29 Respondents answered 6 questions pertaining to the past year. For example, “During the one month when you were at your worst emotionally, how often did you feel hopeless?” Answers ranged from 1 to 5 (none of the time to all of the time). We summed the scores to the items and classified those who scored 13 or greater as having mental illness.
Nicotine dependence.
We measured nicotine dependence using the Heaviness of Smoking Index.30 We summed cigarettes per day and time to first cigarette, each grouped into 4 categories to generate a variable ranging from 0 to 6.
Nicotine withdrawal.
Only those who made a quit attempt (n = 368) completed the withdrawal measure (Minnesota Withdrawal Scale).31 The scale measured the severity of 8 withdrawal symptoms (ranked from 0 to 3: not at all to severely). Preliminary analyses showed that all items loaded well onto a single factor (factor loading ≥ 0.58) with the exception of the symptom feeling hungry (factor loading = 0.24), which we did not include in the analyses. We averaged the remaining items.
Quitting motives, quit attempts, and quit success.
We created a quitting motives scale using 7 items from the wave 1 survey derived from Curry et al.32; for example, “How concerned are you that your smoking is affecting your breathing and energy level?” Responses ranged from 0 to 2 (not at all concerned to very concerned). Cronbach α for these items was 0.81. Respondents self-reported quit attempts between wave 1 and wave 2 at wave 2. We created a binary variable derived from whether each respondent made at least 1 quit attempt between the 2 waves of data collection. We defined successful quitting as 30-day point abstinence from all forms of tobacco.33
Study 2 Analyses
To examine the relationship between nonspecific psychological distress and quitting motives, we calculated an ordinary least squares regression model, adjusting for gender, education, and age as covariates. We calculated the association of nonspecific psychological distress with quit attempts using probit regression, adjusting for the same covariates. We also used probit regression to examine the association of nonspecific psychological distress with quit success among those who made a quit attempt.
To examine the influence of withdrawal and dependence on quit success, we conducted mediation analyses derived from MacKinnon et al.34,35 We tested the relationship between nonspecific psychological distress and both withdrawal and dependence using ordinary least squares regression. We then used probit regression to examine the relationship between nonspecific psychological distress and quit success, adjusting for withdrawal, dependence, and sociodemographic covariates. Our calculation of the mediation effect (nonspecific psychological distress on quit success through withdrawal or dependence) accounted for the binary coding of the quit success variable.34 We calculated the significance of this effect using bootstrap methodology.35 We considered mediation to be evident if the predictor variable was associated with the mediator variable and the mediator variable was associated with the outcome.34
RESULTS
All mental illness categories were more likely to be diagnosed with nicotine withdrawal syndrome than were those in the no disorder category. For externalizing disorder, RR = 1.37 (95% confidence interval [CI] = 1.23, 1.53); for internalizing disorder, RR = 2.37 (95% CI = 2.19, 2.57); for internalizing and externalizing disorders, RR = 3.12 (95% CI = 2.90, 3.37); and for psychotic episode or disorder, RR = 3.45 (95% CI = 2.83, 4.20). Probabilities of nicotine withdrawal syndrome diagnosis, derived from these RR estimates, are displayed in Figure 1.
On the basis of these RR estimates, we calculated a population-attributable fraction for each mental illness category that represents the proportion of nicotine withdrawal syndrome diagnoses in the population of smokers that were attributable to mental illness. The population-attributable fraction for externalizing disorder was 3.2%, for internalizing disorder 16.8%, for internalizing and externalizing disorders 14.9%, and for psychotic episode or disorder 2.9% (Figure 1). If there was no mental illness in the population of smokers, one would expect nicotine withdrawal syndrome diagnoses to be reduced by about half (44.4%).
We examined whether smokers with mental illness reported more severe nicotine withdrawal symptoms. After adjusting estimates for sociodemographic covariates, the externalizing disorder group was only marginally more likely to report nicotine withdrawal–related distress than no disorder (RR = 1.26; 95% CI = 1.10, 1.44). The other groups were clearly more likely to report more severe distress than no disorder: for internalizing disorder, RR = 1.65 (95% CI = 1.53, 1.78); for internalizing and externalizing disorders, RR = 1.97 (95% CI = 1.79, 2.17); and for psychotic episode or disorder, RR = 2.47 (95% CI = 2.06, 2.95).
We then used item response theory and differential item function analyses to examine whether specific nicotine withdrawal symptoms differed between mental illness categories (Table 1). Overall, symptoms were largely consistent between those with and those without mental illness and across mental illness diagnoses. However, a few differences emerged. Anxiety or nervousness was a better marker of withdrawal for those in the internalizing disorder group than for those in all other groups. Restlessness was a better marker of withdrawal for internalizing and externalizing disorders than for the externalizing disorder, internalizing disorder, and psychotic episode or disorder groups.
TABLE 1—
Results From Item Response Theory Analyses Comparing the Symptom Profiles of Nicotine Withdrawal Between Mental Illness Diagnostic Categories: 2001–2002
| aia |
bib |
|||||||||
| Symptoms | ND | ED | ID | IED | PD | ND | ED | ID | IED | PD |
| Depression | 1.43 | 1.39 | 1.42 | 1.33 | 1.14 | 1.81 | 1.78 | 1.12 | 1.05 | 0.80 |
| Difficulty falling or staying asleepe | 1.53 | 1.38 | 1.49 | 1.70 | 1.47 | 1.90 | 1.76 | 1.25 | 0.95 | 0.93 |
| Difficulty concentratingd | 1.69 | 1.85 | 1.96 | 1.69 | 1.37 | 1.79 | 1.42 | 1.09 | 0.74 | 0.84 |
| Increased appetitece | 1.16 | 0.84 | 1.06 | 0.92 | 0.89 | 1.29 | 1.42 | 0.83 | 0.70 | 0.80 |
| Irritation, anger, or frustration | 2.61 | 2.64 | 2.90 | 2.32 | 1.77 | 0.97 | 0.66 | 0.43 | 0.07 | 0.20 |
| Anxiety or nervousnessdefhi | 2.82 | 2.42 | 3.68 | 2.38 | 1.76 | 1.04 | 0.82 | 0.47 | 0.15 | 0.04 |
| Restlessnesscfghj | 2.48 | 1.79 | 2.18 | 2.77 | 1.61 | 1.26 | 1.06 | 0.65 | 0.36 | 0.37 |
Note. ED = externalizing disorder only; DIF = differential item function; ID = internalizing disorder only; IED = internalizing and externalizing disorders; ND = no disorder; PD = psychotic disorder or episode.
ai = item discrimination, i.e., the item’s ability to distinguish between those scoring lower and higher on nicotine withdrawal symptom severity. Higher numbers represent better discrimination, with values > 1.70 considered very high discrimination; i.e., the item strongly differentiates between more severe and less severe withdrawal.
bi = item location, i.e., the relative level of severity indicated by an item within each mental illness group. Higher numbers represent a greater severity represented by the item, with values > 0.5 typically severe for a group; e.g., reporting the symptoms irritation, anger, or frustration would be considered relatively severe (atypical) for those with ND, whereas reporting the symptom would not be considered severe for those with PD relative to others with PD (i.e., the symptom is typical for those with PD).
DIF detected a significant difference between ND and ED for the symptoms increased appetite and restlessness (P < .005; Sidak corrected P value for multiple comparisons).
DIF detected significant differences between ND and ID for the symptoms difficulty concentrating and anxiety or nervousness.
DIF detected significant differences between ND and IED for the symptoms anxiety or nervousness, difficulty falling or staying asleep, and increased appetite.
DIF detected a significant difference between ED and ID for the symptom anxiety or nervousness.
DIF detected a significant difference between ED and IED for the symptom restlessness.
DIF detected significant differences between ID and IED for the symptoms anxiety or nervousness and restlessness.
DIF detected significant differences between ID and PD for the symptom anxiety or nervousness.
DIF detected a significant difference between IED and PD for the symptom restlessness.
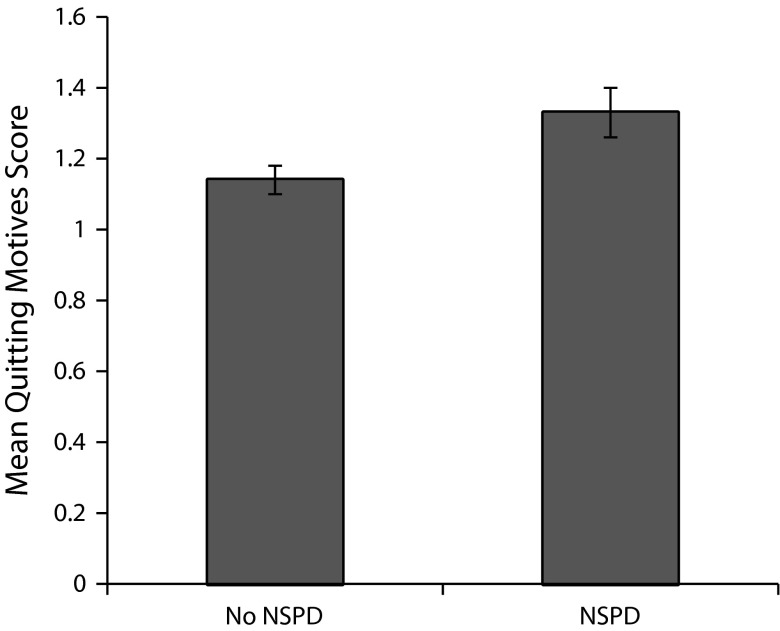
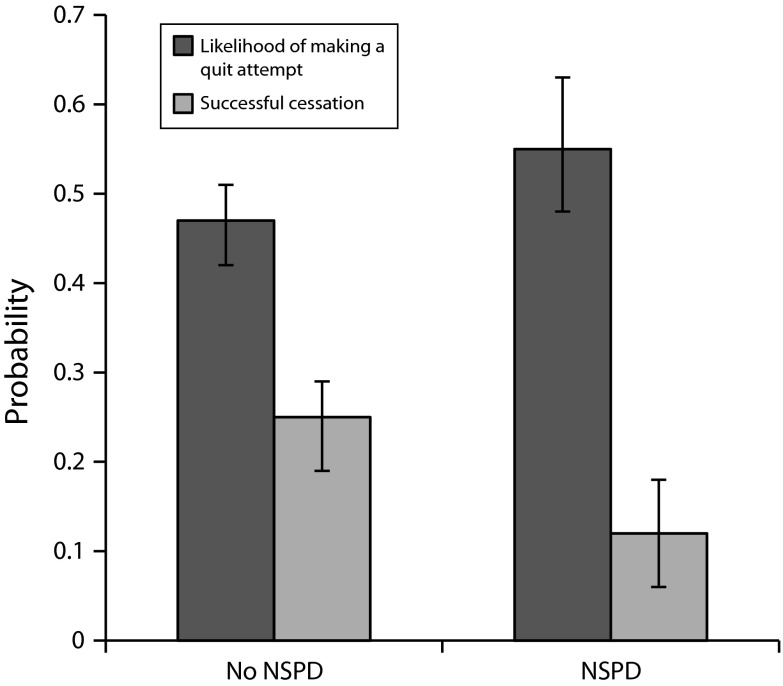
From study 2, after adjustment for sociodemographic covariates (gender, age, and education), smokers with nonspecific psychological distress were significantly more motivated to quit than were smokers without nonspecific psychological distress (b = 0.19; 95% CI = 0.110, 0.280; Figure 2). Smokers with nonspecific psychological distress were also more likely to make a quit attempt between waves 1 and 2 (b = 0.21; 95% CI = 0.001, 0.420; Figure 3).
FIGURE 2—
Quitting motives and nonspecific psychological distress: Assessing Hardcore Smoking Survey, Wave 1; 2004–2005.
Note. Those with nonspecific psychological distress (NSPD) reported stronger quitting motives than did those without NSPD. The figure is derived from ordinary least squares regression, using data from a national sample of smokers (n = 751). We adjusted estimates for age, education, and gender. The quitting motives scale ranged from 0 to 2. Error bars represent 95% confidence intervals.
FIGURE 3—
Quit attempts, successful quitting, and nonspecific psychological distress: Assessing Hardcore Smoking Survey, Waves 1 and 2; 2004–2006.
Note. Those with nonspecific psychological distress (NSPD) were more likely to make a quit attempt than were those without NSPD but less likely to be successful. The figure is derived from probit regression, using data from a national sample of smokers (n = 751 for quit attempt analyses; n = 368 made a quit attempt and were included in the quit success analyses). We adjusted estimates for age, education, and gender. Error bars represent 95% confidence interval.
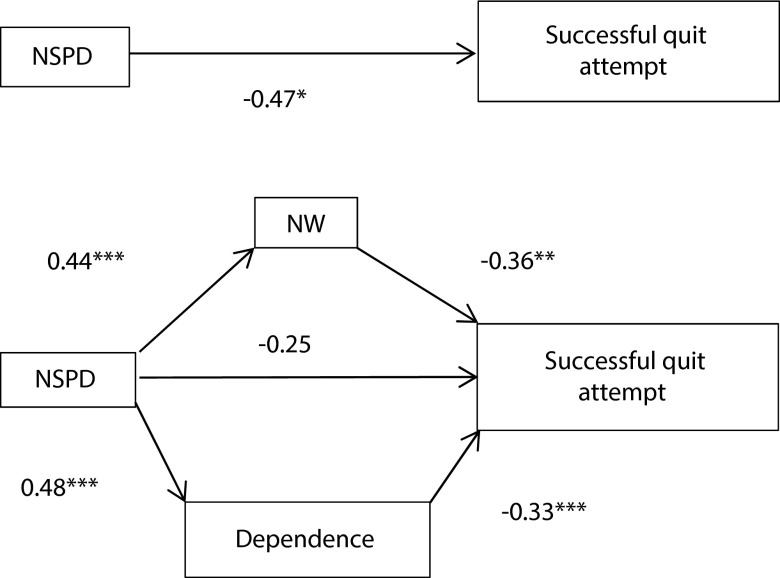
When examining the influence of nicotine withdrawal and dependence on quit success, we limited the sample to those who reported making a quit attempt between waves 1 and 2 (n = 368). Smokers with nonspecific psychological distress reported significantly more severe nicotine withdrawal (b = 0.44; 95% CI = 0.27, 0.60) and greater levels of nicotine dependence (b = 0.48; 95% CI = 0.10, 0.86) than did those without nonspecific psychological distress. Smokers with nonspecific psychological distress were less likely to successfully quit smoking than were smokers without nonspecific psychological distress (b = −0.47; 95% CI = −0.83, −0.11; Figure 3). Nicotine withdrawal and dependence fully mediated the relationship between nonspecific psychological distress and quit success (Figure 4). Both mediation pathways were statistically significant (P < .05).
FIGURE 4—
Successful quitting and nonspecific psychological distress, mediated by withdrawal symptoms and nicotine dependence: Assessing Hardcore Smoking Survey, Waves 1 and 2; 2004–2006.
Note. Nicotine withdrawal (NW) symptom severity and dependence fully mediated the negative relationship between nonspecific psychological distress (NSPD) and quit success among smokers with NSPD. Values are parameter estimates from regression modeling. The figure is derived from a national sample of cigarette smokers who made a quit attempt between 2 waves of data collection (n = 368). Both the mediation pathways were statistically significant (P < .05). We adjusted estimates for age, gender, and education.
*P < .05; **P < .01; ***P < .001.
DISCUSSION
Our results support the importance of addressing nicotine withdrawal among those with mental illness. Smokers with mental illness were substantially more likely to be diagnosed with nicotine withdrawal syndrome; approximately 44% of nicotine withdrawal syndrome diagnoses may be attributable to mental illness. This nicotine withdrawal was more likely to be distressful for those with mental illness. Of particular interest were differences between mental illness categories in nicotine withdrawal syndrome prevalence and nicotine withdrawal severity. The burden of nicotine withdrawal may be greatest for those with a psychotic disorder and those with comorbid internalizing and externalizing disorders. There were only marginal differences between those with an externalizing disorder only and smokers with no mental illness. Externalizing disorders primarily share a latent process of disinhibition, whereas negative affect is the common process underlying internalizing disorders.36 The majority of nicotine withdrawal symptoms involves negative affect, which may explain why internalizing disorder, internalizing and externalizing disorders, and psychotic episode or disorder were more strongly linked to nicotine withdrawal than was externalizing disorder only.
There was a high level of consistency in specific nicotine withdrawal symptoms between those with and those without mental illness and across mental illness diagnoses. This further supported the notion that nicotine withdrawal is, in itself, an important target for intervention among smokers with mental illness. For example, the symptom profiles of those with a psychotic episode or disorder did not differ from those with no mental illness, despite the greater level of withdrawal severity and higher prevalence of nicotine withdrawal syndrome in the psychotic episode or disorder group. If cigarettes were used simply as a means of self-medication for psychotic symptoms, one might have expected to find differing withdrawal profiles. Thus, these results lend support to the notion that nicotine dependence and withdrawal are important targets for intervention among those with psychotic symptomatology.3
We did find evidence of differential withdrawal symptom profiles for those in the internalizing disorder and internalizing and externalizing disorders groups. Cigarette smokers in these groups had withdrawal that was better differentiated by anxiety-related symptoms than were other categories. These findings are relevant in the context of evidence that anxiety sensitivity is related to negative reinforcement smoking motives and lower rates of cessation success.37,38 In a review of research on the use of anxiolytics as smoking cessation aids, Hughes et al.39 concluded that current evidence was insufficient to determine the efficacy of this approach. More recent reviews have reported the same conclusion,3,40 highlighting a need for further research in this area.
In our second study, we found that smokers with nonspecific psychological distress (as defined by Kessler et al.29) were motivated to stop using tobacco, which extends previous work on the topic.41 Despite this motivation, we found that these smokers were less likely to be successful in their quit attempts, which was likely because of nicotine withdrawal and dependence. Importantly, both dependence and withdrawal were uniquely associated with lower likelihood of quit success, after mutually adjusting for both constructs. Again, this speaks to the importance of addressing nicotine withdrawal in cessation efforts, particularly for those with mental illness.
Limitations
Limitations of this study were noted. The NESARC study of nicotine withdrawal syndrome prevalence and nicotine withdrawal severity was cross-sectional. Thus, the time course of nicotine withdrawal symptoms and whether the symptoms occurred during quit attempts was impossible to determine. However, the large NESARC sample size provided the opportunity to conduct highly powered comparative analyses between mental illness diagnoses.
Measures of smoking cessation were self-report. For study 2, only landlines were contacted, and those without landlines may have lower income and be younger.42 Furthermore, given the relatively small baseline sample size and loss of one fourth of the sample to follow-up, we do not consider these cohort data generalizable to the US population of smokers. However, because of the national scope of the surveys, participants were not limited to 1 geographic region of the United States.
Although the response rate was comparable to other national random-digit-dial surveys, such as the Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System,43 it may be that those with mental illness were more likely to not participate in the survey. However, it is likely that underrepresentation of those with more severe mental illness would have conservatively biased differences between those with and those without serious psychological distress.
We measured antisocial personality disorder as lifetime occurrence; thus, we may have misclassified some of those identified as having a past year externalizing disorder (the externalizing disorder and internalizing and externalizing disorders groups). However, antisocial personality disorder has been shown to be relatively stable among adults.44 Furthermore, inclusion of those with lifetime but not past year antisocial personality in the externalizing disorder or internalizing and externalizing disorders groups would most likely have conservatively biased the estimates.
Conclusions
Given evidence that smokers with mental illness are motivated to quit and, with adequate assistance, are able to do so,9 intervention efforts should be informed by a comprehensive view of tobacco use. This view should acknowledge self-medication, vulnerability to nicotine dependence, and more severe nicotine withdrawal as mechanisms that contribute to the heightened rates of smoking among individuals with mental illness.
Acknowledgments
The Robert Wood Johnson Foundation Innovators Combatting Substance Abuse Program and the American Legacy Foundation supported a portion of this research (awarded to G. A. G.).
Human Participant Protection
Study 2 was approved by the University at Buffalo, the State University of New York institutional review board, and the Roswell Park Cancer Institute institutional review board. Study 1, which involved secondary data analysis of de-identified data, was exempt from institutional review board review.
References
- 1.Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness. JAMA. 2000;284(20):2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- 2.Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(11):1107–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 3.Ziedonis D, Hitsman B, Beckham JC et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine & Tobacco Research. 2008;10(12):1691–1715. doi: 10.1080/14622200802443569. [DOI] [PubMed] [Google Scholar]
- 4.Harris JG, Kongs S, Allensworth D et al. Effects of nicotine on cognitive deficits in schizophrenia. Neuropsychopharmacology. 2004;29(7):1378–1385. doi: 10.1038/sj.npp.1300450. [DOI] [PubMed] [Google Scholar]
- 5.Picciotto MR, Brunzell DH, Caldarone BJ. Effect of nicotine and nicotinic receptors on anxiety and depression. Neuroreport. 2002;13(9):1097–1106. doi: 10.1097/00001756-200207020-00006. [DOI] [PubMed] [Google Scholar]
- 6.Glassman AH, Covey LS, Stetner F, Rivelli S. Smoking cessation and the course of major depression: a follow-up study. Lancet. 2001;357(9272):1929–1932. doi: 10.1016/S0140-6736(00)05064-9. [DOI] [PubMed] [Google Scholar]
- 7.Dalack GW, Becks L, Hill E, Pomerleau F, Meador-Woodruff JH. Nicotine withdrawal and psychiatric symptoms in cigarette smokers with schizophrenia. Neuropsychopharmacology. 1999;21(2):195–202. doi: 10.1016/S0893-133X(98)00121-3. [DOI] [PubMed] [Google Scholar]
- 8.Yang YK, Nelson L, Kamaraju L, Wilson W, McEvoy JP. Nicotine decreases bradykinesia-rigidity in haloperidol-treated patients with schizophrenia. Neuropsychopharmacology. 2002;27(4):684–686. doi: 10.1016/S0893-133X(02)00325-1. [DOI] [PubMed] [Google Scholar]
- 9.El-Guebaly N, Cathcart J, Currie S, Brown D, Gloster S. Smoking cessation approaches for persons with mental illness or addictive disorders. Psychiatr Serv. 2002;53(9):1166–1170. doi: 10.1176/appi.ps.53.9.1166. [DOI] [PubMed] [Google Scholar]
- 10.Prochaska JJ. Failure to treat tobacco use in mental health and addiction treatment settings: a form of harm reduction? Drug Alcohol Depend. 2010;110(3):177–182. doi: 10.1016/j.drugalcdep.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lawn S, Pols R. Smoking bans in psychiatric inpatient settings? A review of the research. Aust N Z J Psychiatry. 2005;39(10):866–885. doi: 10.1080/j.1440-1614.2005.01697.x. [DOI] [PubMed] [Google Scholar]
- 12.Prochaska JJ. Smoking and mental illness—breaking the link. N Engl J Med. 2011;365(3):196–198. doi: 10.1056/NEJMp1105248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joint Commission on Accreditation of Healthcare Organizations. Keeping your hospital property smoke-free: successful strategies for effective policy enforcement and maintenance. 2011. Available at: http://www.jointcommission.org/assets/1/18/Smoke_Free_Brochure2.pdf. Accessed March 26, 2012.
- 14.Covey LS, Glassman AH, Stetner F. Depression and depressive symptoms in smoking cessation. Compr Psychiatry. 1990;31(4):350–354. doi: 10.1016/0010-440x(90)90042-q. [DOI] [PubMed] [Google Scholar]
- 15.Piasecki TM, Jorenby DE, Smith SS, Fiore MC, Baker TB. Smoking withdrawal dynamics: II. Improved tests of withdrawal-relapse relations. J Abnorm Psychol. 2003;112(1):14–27. [PubMed] [Google Scholar]
- 16.Weinberger AH, Desai RA, McKee SA. Nicotine withdrawal in U.S. smokers with current mood, anxiety, alcohol use, and substance use disorders. Drug Alcohol Depend. 2010;108(1–2):7–12. doi: 10.1016/j.drugalcdep.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grant BF, Kaplan K, Shepard J, Moore T. Source and Accuracy Statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute of Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 18.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 19.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 20.Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56(10):921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 21.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 22.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. J Abnorm Psychol. 1998;107(2):216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 23.Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Arch Gen Psychiatry. 2001;58(6):597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stata Statistical Software, Version 12.0. [computer program]. College Station, TX: StataCorp LP; 2011.
- 27.Lord FM. Applications of Item Response Theory to Practical Testing Problems. Hillsdale, NJ: Erlbaum; 1980. [Google Scholar]
- 28.Crane PK, Gibbons LE, Jolley L, van Belle G. Differential item functioning analysis with ordinal logistic regression techniques: DIFdetect and difwithpar. Med Care. 2006;44(11) suppl 3:S115–S123. doi: 10.1097/01.mlr.0000245183.28384.ed. [DOI] [PubMed] [Google Scholar]
- 29.Kessler RC, Barker PR, Colpe LJ et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 30.Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84(7):791–799. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 31.Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43(3):289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- 32.Curry S, Wagner EH, Grothaus LC. Intrinsic and extrinsic motivation for smoking cessation. J Consult Clin Psychol. 1990;58(3):310–316. doi: 10.1037//0022-006x.58.3.310. [DOI] [PubMed] [Google Scholar]
- 33. North American Quitline Consortium. Measuring Quit Rates. Quality Improvement Initiative. Phoenix, AZ; 2009.
- 34.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mackinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behav Res. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior and personality: modeling the externalizing spectrum. J Abnorm Psychol. 2002;111(3):411–424. [PubMed] [Google Scholar]
- 37.Brown RA, Kahler CW, Zvolensky MJ, Lejuez CW, Ramsey SE. Anxiety sensitivity: relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addict Behav. 2001;26(6):887–899. doi: 10.1016/s0306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- 38.Zvolensky MJ, Stewart SH, Vujanovic AA, Gavric D, Steeves D. Anxiety sensitivity and anxiety and depressive symptoms in the prediction of early smoking lapse and relapse during smoking cessation treatment. Nicotine & Tobacco Research. 2009;11(3):323–331. doi: 10.1093/ntr/ntn037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hughes JR, Stead LF, Lancaster T. Anxiolytics for smoking cessation. Cochrane Database Syst Rev. 2000;(4) doi: 10.1002/14651858.CD002849. CD002849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bała MM, Leśniak W, Strzeszyński Ł. Efficacy of pharmacological methods used for treating tobacco dependence: meta-analysis. Pol Arch Med Wewn. 2008;118(1–2):20–28. [PubMed] [Google Scholar]
- 41.Siru R, Hulse GK, Tait RJ. Assessing motivation to quit smoking in people with mental illness: a review. Addiction. 2009;104(5):719–733. doi: 10.1111/j.1360-0443.2009.02545.x. [DOI] [PubMed] [Google Scholar]
- 42.Blumberg SJ, Luke JV. Coverage bias in traditional telephone surveys of low-income and young adults. Public Opin Q. 2007;71(5):734–749. [Google Scholar]
- 43. Centers for Disease Control and Prevention. 2005 Behavioral Risk Factor Surveillance System: Summary Data Quality Report. Atlanta, GA; 2006.
- 44.Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychol Rev. 1993;100(4):674–701. [PubMed] [Google Scholar]