Abstract
Objectives. We compared seasonal influenza hospital use among older adults in long-term care (LTC) and community settings.
Methods. We used provincial administrative data from Ontario to identify all emergency department (ED) visits and hospital admissions for pneumonia and influenza among adults older than 65 years between 2002 and 2008. We used sentinel laboratory reports to define influenza and summer seasons and estimated mean annual event rates and influenza-associated rates.
Results. Mean annual pneumonia and influenza ED visit rates were higher in LTC than the community (rate ratio [RR] for influenza season = 3.9; 95% confidence interval [CI] = 3.8, 4.0; for summer = 4.9; 95% CI = 4.8, 5.1) but this was attenuated in influenza-associated rates (RR = 2.4; 95% CI = 2.1, 2.8). The proportion of pneumonia and influenza ED visits attributable to seasonal influenza was 17% (15%–20%) in LTC and 28% (27%–29%) in the community. Results for hospital admissions were comparable.
Conclusions. We found high rates of hospital use from LTC but evidence of lower impact of circulating influenza in the community. This differential impact of circulating influenza between the 2 environments may result from different influenza control policies.
Influenza has been identified as among the top 10 infectious agents that are causes of health burden,1 and it continues to create significant morbidity and mortality among older adults. Individuals older than 65 years, in particular those with preexisting chronic conditions, are at increased risk for hospitalization2,3 and death4,5 associated with influenza. The Canadian province of Ontario first introduced universal influenza immunization in 2000, granting all provincial residents aged 6 months or older the option for annual immunization without out-of-pocket cost. Although immunization coverage in the general population remains relatively low, levels are highest among community-dwelling adults older than 65 years, with coverage exceeding 70%.6
For residents of long-term care (LTC) facilities, also known as nursing homes, immunization coverage generally exceeds 90% in Ontario7 and 80% in other jurisdictions, mainly because of concerted efforts to reach this group.8,9 LTC residents are a particularly vulnerable segment of the older population, with an average age of 80 years, significant cognitive and physical impairments, and a high burden of complex chronic conditions, including cardiovascular and respiratory illnesses. Despite high immunization coverage in residents, influenza continues to cause significant burden. Influenza has been associated with increased rates of functional decline and pressure ulcers in this group.10 It is also among the most common reasons for transfer to the hospital and accounts for a significant proportion of mortality in this population.11–13
A single study reported that rates of hospitalization for influenza were 3 times as high among LTC as among community residents, both during and before the identified influenza season.14 In addition to their heightened vulnerability, LTC residents face other risk factors for infection, including congregate living and shared bedrooms, that community residents do not experience. Because of this, LTC is targeted for strong infection prevention and control (IPC) measures, including staff immunization. Although evidence from Ontario suggests that LTC staff immunization rates are generally higher than 70%,7 well above that reported in hospitals, other evidence points to generally poor compliance with other IPC practices.15
To date, little is known about the burden of influenza in LTC and how it compares to that in the community. Our objectives were to compare the burden of influenza, as measured by hospital use, both emergency department (ED) visits and inpatient admissions, among older adults in LTC and community settings.
METHODS
We conducted a retrospective longitudinal study on weekly counts of hospital admissions and ED visits among older adults (aged 66–105 years) from both LTC and community settings in Ontario over 6 influenza seasons (2002–2003 to 2007–2008). The study period extended from September 2002 to August 2008, comprising 313 study weeks. We truncated the data in 2008 to avoid the 2009 influenza A (H1N1) pandemic, which had a different epidemiology.16 All Ontario residents with a valid health care number were eligible for inclusion, but we restricted our analysis to persons aged 66 years and older.
Ontario is Canada’s most populous province (∼12.2 million people as of 2006), and all residents have access to hospital and physician services and influenza vaccines. In Ontario, LTC specifically refers to care in a residential setting for individuals aged 18 years or older who require 24-hour access to nursing care or supervision (comparable to long-stay nursing home services in the United States). LTC services are covered under the province’s universal health insurance system, and access is centrally managed through regional care coordination centers.
Data Sources
We used linked population-based administrative health care data from Ontario, housed at the Institute for Clinical Evaluative Sciences in Toronto. We linked the databases through encrypted health card numbers that served as unique identifiers. The Registered Persons Database contains basic vital statistics for all Ontario residents eligible for health services; we used it to create weekly counts of all older adults in Ontario during the study years. We obtained information on ED visits from the National Ambulatory Care Reporting System and information on hospital admissions from the Discharge Abstract Database. The Ontario Health Insurance Plan database contains billing claims from Ontario physicians.17 The Ontario Drug Benefits database contains outpatient prescription drug claims covered by the provincial drug benefits program for all adults aged 65 years and older.18 Both health insurance and drug benefits claims include special markers for services provided to LTC residents.
Viral surveillance data and influenza season identification.
We obtained influenza viral surveillance data comprising weekly reports of the number of respiratory virus tests performed and the number of those tests that were positive for influenza and respiratory syncytial virus submitted by a provincial network of sentinel laboratories to the Public Health Agency of Canada. These laboratories used mainly viral culture and direct antigen detection techniques to test samples for influenza. We used the weekly percentage of tests positive for influenza as our measure of viral circulation.
We defined the start and end dates for influenza seasons as, respectively, the first and last occurrences of 2 consecutive weeks with 10% or more influenza isolates testing positive. For each influenza season, we defined a summer season (control period where little to no influenza would be circulating in the community) that started in the first week of June following the influenza season and was of equivalent weekly duration. This resulted in a total of 65 weeks designated as influenza season, with increased activity, and a total of 65 weeks designated as summer season, with limited activity.
Hospital use.
We used 2 measures of hospital use, hospital admissions and ED visits, which were identified in the Discharge Abstract Database and National Ambulatory Care Reporting System, respectively. We used International Classification of Disease 10th Revision19 codes J10 to J18 to identify all hospital use for pneumonia and influenza, which was consistent with literature on influenza-related hospital use that found that influenza codes alone underestimate the true burden.2,20 We excluded transfers between acute care and ambulatory care centers. For our primary analysis, we included events with pneumonia and influenza coded in any diagnostic field. As a sensitivity analysis, we restricted cases to pneumonia and influenza coded in the primary diagnostic field (the diagnosis most responsible for length of stay in the hospital records and first diagnostic field for ED records). We aggregated all pneumonia and influenza outcomes into weekly counts and stratified them by age at hospital admission or ED presentation (66–85 years or 86–105 years) and residence (LTC or community).
Long-term care resident identification.
Ontario had approximately 70 000 LTC beds during the study period. To identify outcomes among LTC residents, we looked for any health insurance billing or drug benefits claim with a LTC marker in the 45 days prior to either hospital admission or ED visit. We selected a 45-day window because our previous work showed that nearly all residents receive prescription drugs and that these claims are processed on a minimum 7-day to 30-day schedule21; we used the health insurance claims for the minority of LTC residents who did not receive prescription drugs. We assumed that any older adult who was not identified as a LTC resident was living in the community (private homes and assisted or supportive living environments).
Analyses
For each age–residence group, we calculated the mean annual observed rates of pneumonia and influenza hospitalizations and pneumonia and influenza ED visits per 100 000 individuals during both influenza and summer seasons. We used the Registered Persons Database to estimate the total number of individuals aged 66 years or older as of October for each study year. We then searched health insurance and drug benefits claims for a LTC flag, with a 45-day look-back period to determine the count of individuals in LTC at the start of each study year. We estimated the annual denominators for the LTC and community groups from the Registered Persons Database as the number with and without a concurrent LTC flag, respectively.
We used previously developed methods to calculate influenza-associated (also known as excess influenza) outcome rates during influenza seasons.2,20,22 Briefly, for each pneumonia and influenza outcome, we developed separate Poisson regression models for each age–residence group (totaling 8 models). The dependent variable was the weekly outcome counts for the age–residence group. The main predictors in the model were the weekly percentage of tests positive for influenza A, influenza B, and respiratory syncytial virus, as well as linear and quadratic terms to model time trends, sine and cosine functions with periods of 1 year to model seasonal fluctuations, and categorical terms to adjust for changes in health care service volumes during the Christmas and post–Christmas holiday periods. Once we estimated the initial parameters for each predictor in the model, we reran the models after setting the terms for influenza A and B circulation to zero, thus generating a weekly expected baseline of outcomes in the hypothetical absence of influenza activity.2,22 We computed influenza-associated outcomes as the difference between the observed and expected baseline outcomes for each week during influenza season, and we aggregated these to produce mean annual influenza-associated rates for each outcome and every age–residence group. All models accounted for variance overdispersion in the estimates of all standard errors to account for potential clustering of outcomes within the weekly strata.
We produced rate ratios (RRs) for 3 different comparisons to meet our objectives. First, we compared outcome rates of LTC residents to those of community residents during each of the influenza and summer seasons. By directly comparing LTC to community rates during each type of season, we were able to determine whether a relatively greater increase in hospital use for pneumonia and influenza occurred among LTC residents during influenza season. Second, we estimated the proportion of observed pneumonia and influenza hospital use rates that were attributable to influenza (during influenza season only). We accomplished this by taking the ratio of the influenza-associated outcome rate to the observed rate during influenza season for each residence group. Third, we compared the observed outcome rates during the influenza season to the observed outcome rates during the summer season within each residence group. This provided an estimate of increased hospital use for pneumonia and influenza when circulating influenza was at its highest relative to hospital use when it was at its lowest; we then compared the RRs for the LTC and community groups. We calculated each of these RRs for the full cohort and for each age stratum. We computed standard errors for each RR, used to calculate 95% confidence intervals (CIs), assuming a Poisson distribution for the overall counts; we incorporated the variance of the predicted baseline whenever we compared excess influenza rates.23 We performed all analyses with SAS version 9.2.24
RESULTS
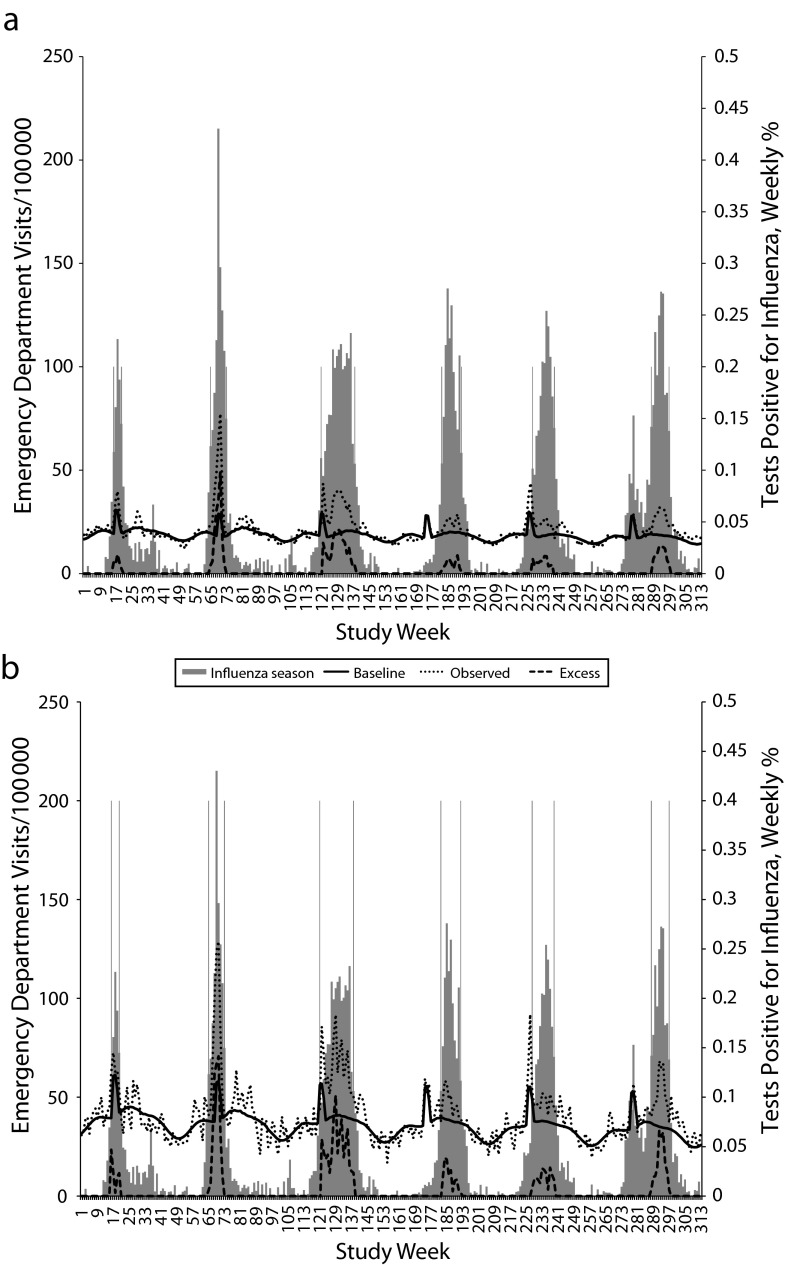
Figure 1 displays the observed (dots) and influenza-associated (dashes) ED visit rates for each age and residence group for each week between week 1 (ending September 7, 2002) and week 313 (ending August 30, 2008). Regardless of age or residence, visit rates peaked over the winter months, and influenza season duration varied each year. The relatively large peak around week 69 represented the severe 2003–2004 influenza season. Both observed and influenza-associated ED visit rates were consistently higher among the LTC than the community groups. In the community setting, the older age group (86–105 years) had higher visit rates than the younger age group (66–85 years), with the reverse among LTC residents. We observed similar patterns for hospital admissions (data not shown).
FIGURE 1—
Observed and influenza-associated emergency department visits for pneumonia and influenza among older adults (a) aged 66–85 years living in the community, (b) aged 86–105 years in living the community, (c) aged 66–85 years in long-term care, and (d) aged 86–105 years in long-term care: Ontario, 2002–2008.
Note. Gray-shaded areas represent weekly influenza viral surveillance data expressed as the percentage of tests positive for influenza.
Table 1 displays the influenza-associated and observed pneumonia and influenza ED visit and hospital admission rates for all age and residence groups. Observed pneumonia and influenza hospital use rates were consistently higher among the LTC than the community group during each summer and influenza period. During both seasonal periods, pneumonia and influenza rates decreased with age for the LTC group but increased with age for the community group. Influenza-associated pneumonia and influenza hospital use rates were also higher for the LTC than the community group but increased with age for both.
TABLE 1—
Influenza-Associated and Observed Pneumonia and Influenza Hospital Use Rates by Residence Type, Season, and Age Group: Ontario, 2002–2008
| Observed |
||||
| Age Group | Influenza-Associated,a No. | Influenza Season, No. | Summer Season, No. | Attributable to Influenza,b % (95% CI) |
| Long-term care | ||||
| Emergency department visits | ||||
| All | 300.5 | 1756.9 | 1277.0 | 17 (15, 20) |
| 66–85 y | 290.6 | 1976.6 | 1458.6 | 15 (12, 18) |
| 86–105 y | 310.0 | 1543.0 | 1100.0 | 20 (17, 24) |
| Hospital admissions | ||||
| All | 322.5 | 1945.6 | 1400.0 | 17 (15, 19) |
| 66–85 y | 319.5 | 2193.5 | 1603.6 | 15 (12, 18) |
| 86–105 y | 325.4 | 1704.0 | 1201.6 | 19 (16, 23) |
| Community residence | ||||
| Emergency department visits | ||||
| All | 124.7 | 445.3 | 258.8 | 28 (27, 29) |
| 66–85 y | 113.5 | 403.1 | 237.5 | 28 (27, 29) |
| 86–105 y | 210.9 | 770.5 | 423.4 | 27 (25, 30) |
| Hospital admissions | ||||
| All | 86.0 | 445.6 | 284.7 | 19 (18, 20) |
| 66–85 y | 69.1 | 385.2 | 253.7 | 18 (17, 19) |
| 86–105 y | 215.65 | 910.9 | 523.5 | 24 (22, 26) |
Note. CI = confidence interval.
Per 100 000 persons.
Estimated as the proportion of the observed influenza hospital use rate during influenza season that was influenza associated.
Table 2 displays the RRs and 95% CIs comparing the influenza-associated and observed pneumonia and influenza hospital use rates among LTC and community residents. The overall observed pneumonia and influenza ED visit RR was 4.0 (95% CI = 3.8, 4.0) during influenza season and 4.9 (95% CI = 4.8, 5.1) during the summer months. During both seasonal periods, the RRs were substantially lower among the older than the younger groups. The RRs derived from observed rates were greater than the RRs derived from influenza-associated rates (full sample RR = 2.4; 95% CI = 2.1, 2.8). The difference between the RRs by age was also attenuated for the influenza-associated rates. The proportion of observed pneumonia and influenza ED visits for influenza was an estimated 17% (15%–20%) for the LTC group and 28% (27%–29%) for the community group (Table 1). The attributable proportion increased with age for the LTC group but not for the community group. We observed comparable patterns for the rates of pneumonia and influenza hospital admissions, except that the attributable proportion among the community group also showed an increase with age.
TABLE 2—
Relative Rates of Pneumonia and Influenza Hospital Use by Residence Type and Season: Ontario, 2002–2008
| Long-Term Care vs Community Residence |
Influenza Season vs Summer |
||||
| Age Group | Influenza-Associated, RR (95% CI) | Observed, Influenza Season, RR (95% CI) | Observed, Summer Season, RR (95% CI) | Long-Term Care, RR (95% CI) | Community, RR (95% CI) |
| Emergency department visits | |||||
| All | 2.4 (2.1, 2.8) | 4.0 (3.8, 4.0) | 4.9 (4.8, 5.1) | 1.4 (1.3, 1.4) | 1.7 (1.7, 1.8) |
| 66–85 y | 2.6 (2.1, 3.2) | 4.9 (4.7, 5.1) | 6.1 (5.9, 6.4) | 1.4 (1.3, 1.4) | 1.7 (1.7, 1.7) |
| 86–105 y | 1.5 (1.2, 1.8) | 2.0 (1.9, 2.1) | 2.6 (2.5, 2.7) | 1.4 (1.3, 1.5) | 1.8 (1.8, 1.9) |
| Hospital admissions | |||||
| All | 3.7 (3.2, 4.3) | 4.4 (4.3, 4.5) | 4.9 (4.8, 5.1) | 1.4 (1.3, 1.4) | 1.6 (1.5, 1.6) |
| 66–85 y | 4.6 (3.7, 5.7) | 5.7 (5.5, 5.9) | 6.3 (6.1, 6.5) | 1.4 (1.3, 1.4) | 1.5 (1.5, 1.5) |
| 86–105 y | 1.5 (1.3, 1.8) | 1.9 (1.8, 1.9) | 2.3 (2.2, 2.4) | 1.4 (1.3, 1.5) | 1.7 (1.7, 1.8) |
Note. CI = confidence interval; RR = rate ratio.
Table 2 also shows RRs comparing observed pneumonia and influenza hospital use rates during influenza seasons to observed rates during the summer seasons for the LTC and community groups. The RR for the LTC group was 1.4 (95% CI = 1.3, 1.4) and for the community group, 1.7 (95% CI = 1.7, 1.8). We found little difference by age group and similar patterns for rates of pneumonia and influenza hospital admission. Sensitivity analyses of only the main diagnostic field from ED and hospital records showed comparable results.
DISCUSSION
We observed clear seasonal trends among older adults in pneumonia and influenza hospital use, for both ED visits and hospital admissions. As expected, we found much higher rates of hospital use among older adults in LTC than in the community; however, we also found that the effect of influenza activity during peak periods was not greater among LTC than community residents. In fact, our results suggested that the impact of influenza, as measured by elevations in pneumonia and influenza ED visits and hospital admissions, was actually lower in the LTC setting than in the community setting.
The relative rate of hospital use comparing LTC to community residents was smaller during influenza seasons than during summer seasons, and the relative influenza-associated rates were even lower. Further, the proportion of pneumonia and influenza hospital use during influenza season that could be attributed to circulating influenza activity was consistently higher among the community group than the LTC group. These findings suggest that ongoing IPC activities in LTC have had a positive impact on residents, at least with respect to hospital transfers for pneumonia and influenza. IPC is listed as a key risk indicator by the Ontario Ministry of Health and Long-Term Care25 and is a systemwide standard for accreditation in both Canada and the United States.26,27 Immunization continues to be the most frequently reported IPC practice in LTC, with some estimates of resident immunization as high as 93%.15
Despite high rates of immunization among LTC residents, concerns have been raised about the effectiveness of immunization in this population; some evidence suggests that high rates of immunization are not associated with a reduction in outbreaks or related outcomes in LTC.8 High rates of staff immunization, however, have been shown to be associated with a decreased occurrence of outbreaks.28 Although other jurisdictions have reported significant barriers to staff immunization, including perceptions about safety and lack of understanding of the effects on resident health,27 the high staff immunization rates in Ontario LTC homes may at least partially explain the relatively lesser impact of influenza on LTC residents than on community-dwelling older adults. Beyond the effects of IPC activities, these results may also reflect differences in opportunities for exposure. For instance, older adults in the community may have more regular contact with young children, such as grandchildren, whereas LTC residents may have less contact during times when family members might be sick.
The relatively lower impact of increased influenza activity on pneumonia and influenza hospital use rates may also reflect different care processes in the 2 settings. In LTC, nurses and health care aides are on site 24 hours per day and may be able to implement care plans for ill residents that could not be provided for older adults in their own homes. For example, a clinical program designed to enable pneumonia care in LTC settings has been shown to be successful at reducing hospital transfers without higher mortality29; however, even with programs such as these, LTC treatment processes alone likely do not account for our findings. LTC residents have very high rates of ED use and hospitalization, and pneumonia and influenza rank among the most common reasons for transfer.11 We also also observed very high rates of ED visits and hospital admission for pneumonia and influenza, often more than double the rates in the community group. Sources report that some of the main drivers for such high rates of transfer from LTC are the difficulty in accessing physicians in a timely manner and limited ability to implement treatment programs in the LTC setting.30,31
We also found interesting age trends. Hospital use rates were often greater among younger (66–85 years) than older (86–105 years) LTC residents, but the reverse was true for community-dwelling older adults. This reflects some important underlying characteristics of both populations. For older adults in the community, older age is associated with greater vulnerability. For older adults in LTC, though, the converse is often true. Adults aged 65 to 75 years of age are a small proportion of the LTC population; they are frequently admitted because they have particularly high levels of need and frailty for their age, making them more vulnerable than their counterparts in the community.
Limitations
We did not include physician visits or other markers of less severe illness, primarily because we were interested in hospital use. Thus we focused on the more severe outcomes, and the differences in hospital use between the LTC and community populations may have overestimated the severity of illness in either group. We did not use data more recent than 2008. We decided to truncate the data before the 2009 influenza A (H1N1) pandemic, which had a different epidemiology than seasonal influenza.16
We estimated the influenza-associated rates with statistical models, and the accuracy of these models depended on the validity of our inputs and assumptions. Although other estimation methods have been proposed, they appear to produce largely similar results.32 Finally, we lacked data on immunization and could only infer higher rates of immunization in the LTC group from other reported evidence. Future research is required to address more intricate questions related to seasonality and other issues.
Conclusions
We found high rates of ED visits and hospital admission for pneumonia and influenza in the LTC population; however, relative to older adults in the community setting, we found no evidence that older adults in LTC were more strongly affected by increased circulating influenza activity. In fact, in some cases, it appeared that older adults in the community were more strongly affected. Whether this was attributable to high rates of immunization among LTC residents and staff, more limited contact with infectious individuals, or other factors is yet unknown.
Acknowledgments
This research was funded by an operating grant from the Canadian Institutes of Health Research (CIHR) Institute for Health Services and Policy Research (Emergency Department Visits by Nursing Home Residents in Ontario; MOP 89943) and by an Interdisciplinary Capacity Enhancement Grant from the CIHR Institute of Gender and Health (Reducing Health Disparities and Promoting Equity for Vulnerable Populations; HOA 80075). A. Gruneir was partially supported by a team grant from the CIHR Institute of Nutrition, Metabolism, and Diabetes (OTG 88591). V. Mor was supported by a grant from the US Agency for Healthcare Research and Quality (HS018462). This study was conducted at the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC).
The authors acknowledge the sentinel laboratories participating in the Respiratory Virus Detection Surveillance System and the FluWatch team at the Public Health Agency of Canada for providing the viral surveillance data used in this study and Grace Karam, Women’s College Research Institute, for her assistance in preparing the article.
Note. The opinions, results, and conclusions reported in this article are those of the authors and not of ICES or the Ontario MOHLTC.
Human Participant Protection
The research ethics board of Sunnybrook Health Sciences Centre, Toronto, approved the study protocol.
References
- 1.Kwong JC, Ratnasingham S, Campitelli MA et al. The impact of infection on population health: results of the Ontario burden of infectious diseases study. PLoS ONE. 2012;7(9):e44103. doi: 10.1371/journal.pone.0044103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson WW, Shay DK, Weintraub E et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292(11):1333–1340. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 3.Zhou H, Thompson WW, Viboud CG et al. Hospitalizations associated with influenza and respiratory syncytial virus in the United States, 1993–2008. Clin Infect Dis. 2012;54(10):1427–1436. doi: 10.1093/cid/cis211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tinetti ME, McAvay GJ, Murphy TE, Gross CP, Lin H, Allore HG. Contribution of individual diseases to death in older adults with multiple diseases. J Am Geriatr Soc. 2012;60(8):1448–1456. doi: 10.1111/j.1532-5415.2012.04077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schanzer DL, Langley JM, Tam TW. Co-morbidities associated with influenza-attributed mortality, 1994–2000, Canada. Vaccine. 2008;26(36):4697–4703. doi: 10.1016/j.vaccine.2008.06.087. [DOI] [PubMed] [Google Scholar]
- 6.Kwong JC, Rosella LC, Johansen H. Trends in influenza vaccination in Canada, 1996/1997 to 2005. Health Rep. 2007;18(4):9–19. [PubMed] [Google Scholar]
- 7. Surveillance Services Public Health Ontario. Ontario influenza bulletin, 2012–2013. 2012. Available at: http://www.oahpp.ca/resources/documents/flubulletin/Influenza%20Bulletin-Weeks%2036_37.pdf. Accessed February 21, 2013.
- 8.Shugarman LR, Hales C, Setodji CM, Bardenheier B, Lynn J. The influence of staff and resident immunization rates on influenza-like illness outbreaks in nursing homes. J Am Med Dir Assoc. 2006;7(9):562–567. doi: 10.1016/j.jamda.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 9.McArthur MA, Simor AE, Campbell B, McGeer A. Influenza vaccination in long-term-care facilities: structuring programs for success. Infect Control Hosp Epidemiol. 1999;20(7):499–503. doi: 10.1086/501659. [DOI] [PubMed] [Google Scholar]
- 10.Gozalo PL, Pop-Vicas A, Feng Z, Gravenstein S, Mor V. Effect of influenza on functional decline. J Am Geriatr Soc. 2012;60(7):1260–1267. doi: 10.1111/j.1532-5415.2012.04048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gruneir A, Bell CM, Bronskill SE, Schull M, Anderson GM, Rochon PA. Frequency and pattern of emergency department visits by long-term care residents—a population-based study. J Am Geriatr Soc. 2010;58(3):510–517. doi: 10.1111/j.1532-5415.2010.02736.x. [DOI] [PubMed] [Google Scholar]
- 12.Gaillat J, Chidiac C, Fagnani F et al. Morbidity and mortality associated with influenza exposure in long-term care facilities for dependent elderly people. Eur J Clin Microbiol Infect Dis. 2009;28(9):1077–1086. doi: 10.1007/s10096-009-0751-3. [DOI] [PubMed] [Google Scholar]
- 13.Ellis SE, Coffey CS, Mitchel EF, Jr, Dittus RS, Griffin MR. Influenza- and respiratory syncytial virus-associated morbidity and mortality in the nursing home population. J Am Geriatr Soc. 2003;51(6):761–767. doi: 10.1046/j.1365-2389.2003.51254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Menec VH, MacWilliam L, Aoki FY. Hospitalizations and deaths due to respiratory illnesses during influenza seasons: a comparison of community residents, senior housing residents, and nursing home residents. J Gerontol A Biol Sci Med Sci. 2002;57(10):M629–M635. doi: 10.1093/gerona/57.10.m629. [DOI] [PubMed] [Google Scholar]
- 15.Zoutman DE, Ford BD, Gauthier J. A cross-Canada survey of infection prevention and control in long-term care facilities. Am J Infect Control. 2009;37(5):358–363. doi: 10.1016/j.ajic.2008.10.029. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Update: influenza activity—United States, 2009–10 season. MMWR Morb Mortal Wkly Rep. 2010;59(29):901–908. [PubMed] [Google Scholar]
- 17.Chan B. Supply of physicians’ services in Ontario. Hosp Q. 1999–2000;3(2):17. doi: 10.12927/hcq..16734. [DOI] [PubMed] [Google Scholar]
- 18.Levy AR, O’Brien BJ, Sellors C, Grootendorst P, Willison D. Coding accuracy of administrative drug claims in the Ontario Drug Benefit database. Can J Clin Pharmacol. 2003;10(2):67–71. [PubMed] [Google Scholar]
- 19.International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 20.Kwong JC, Stukel TA, Lim J et al. The effect of universal influenza immunization on mortality and health care use. PLoS Med. 2008;5(10):e211. doi: 10.1371/journal.pmed.0050211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daneman N, Gruneir A, Newman A et al. Antibiotic use in long-term care facilities. J Antimicrob Chemother. 2011;66(12):2856–2863. doi: 10.1093/jac/dkr395. [DOI] [PubMed] [Google Scholar]
- 22.Thompson WW, Shay DK, Weintraub E et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289(2):179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 23.Rothman KJ, Greenland S, editors. Modern Epidemiology. 2nd ed. Philadelphia, PA: Lippencott-Raven; 1998. [Google Scholar]
- 24. SAS Institute Inc. SAS 9.2 product documentation. 2013. Available at: http://support.sas.com/documentation/92/index.html. Accessed February 21, 2013.
- 25. Ontario Ministry of Health and Long-Term Care. Patient safety. Available at: http://www.health.gov.on.ca/en/public/programs/patient_safety. Accessed February 21, 2013.
- 26. Accreditation Canada. Infection prevention and control. Available at: http://www.accreditation.ca/accreditation-programs/qmentum/standards/infection-prevention-and-control. Accessed February 21, 2013.
- 27.Sand KL, Lynn J, Bardenheier B, Seow H, Nace DA. Increasing influenza immunization for long-term care facility staff using quality improvement. J Am Geriatr Soc. 2007;55(11):1741–1747. doi: 10.1111/j.1532-5415.2007.01422.x. [DOI] [PubMed] [Google Scholar]
- 28.Lemaitre M, Meret T, Rothan-Tondeur M et al. Effect of influenza vaccination of nursing home staff on mortality of residents: a cluster-randomized trial. J Am Geriatr Soc. 2009;57(9):1580–1586. doi: 10.1111/j.1532-5415.2009.02402.x. [DOI] [PubMed] [Google Scholar]
- 29.Loeb M, Carusone SC, Goeree R et al. Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial. JAMA. 2006;295(21):2503–2510. doi: 10.1001/jama.295.21.2503. [DOI] [PubMed] [Google Scholar]
- 30.Brooks S, Warshaw G, Hasse L, Kues JR. The physician decision-making process in transferring nursing home patients to the hospital. Arch Intern Med. 1994;154(8):902–908. [PubMed] [Google Scholar]
- 31.Jones JS, Dwyer PR, White LJ, Firman R. Patient transfer from nursing home to emergency department: outcomes and policy implications. Acad Emerg Med. 1997;4(9):908–915. doi: 10.1111/j.1553-2712.1997.tb03818.x. [DOI] [PubMed] [Google Scholar]
- 32.Thompson WW, Weintraub E, Dhankhar P et al. Estimates of US influenza-associated deaths made using four different methods. Influenza Other Respi Viruses. 2009;3(1):37–49. doi: 10.1111/j.1750-2659.2009.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]