Abstract
Objectives. Guided by the life-course perspective, we examined whether there were subgroups with different likelihood curves of smoking onset associated with specific developmental periods.
Methods. Using 12 waves of panel data from 4088 participants in the National Longitudinal Survey of Youth 1997, we detected subgroups with distinctive risk patterns by employing developmental trajectory modeling analysis.
Results. From birth to age 29 years, 72% of female and 74% of US males initiated smoking. We detected 4 exclusive groups with distinctive risk patterns for both genders: the Pre-Teen Risk Group initiated smoking by age 12 years, the Teenage Risk Group initiated smoking by age 18 years, the Young Adult Risk Group initiated smoking by age 25 years, and the Low Risk Group experienced little or no risk over time. Groups differed on several etiological and outcome variables.
Conclusions. The process of smoking initiation from birth to young adulthood is nonhomogeneous, with distinct subgroups whose risk of smoking onset is linked to specific stages in the life course.
Studies suggest that there have been recent increases in adolescent smoking in the United States.1,2 More effective prevention requires further understanding of tobacco use etiology. Numerous researchers have documented the timing and risk of early onset of tobacco use.3–8 Although children as young as 4 to 5 years have reported smoking,3,4 the hazard of smoking onset (defined as the probability for a never-smoker to initiate smoking during a 1-year period) is relatively low (0%–3%) before age 10 years.3–6 The risk then increases rapidly to peak at around age 14 to 16 years, with initiation rates ranging from 5% to 15%, depending on study population and time of measurement, before it declines.3–6 The risk of smoking initiation in later adolescence and early adulthood remains at less than 10%.9–13
Despite this general age pattern of the risk of smoking onset, it remains unclear whether there are actual subgroups with unique risk curves associated with different developmental periods. Most studies of smoking risk trajectories are based, either implicitly or explicitly, on the assumption that 1 probability curve quantifies the risk of smoking onset for all individuals across ages and developmental periods, which may not be the case. An additional limitation of the current literature is that much of the previous research has relied on cross-sectional or brief longitudinal samples of adolescents rather following adolescents through young adulthood.
According to the life-course perspective,14–16 the interplay of intrapersonal factors and environmental factors determines who is at risk for smoking initiation at what time periods (i.e., ages). Such influential factors may include age- and development-related differences in individual vulnerability to tobacco use17 and external influences such as peer pressure, parental monitoring, and social support.11,18–20 Therefore, the process of smoking onset may not be homogeneous but diverse, involving subgroups of individuals with unique time patterns corresponding to different developmental periods in the life span.
In general, very young children and adolescents are less likely than older adolescents to be self-motivated to smoke.21 Rather, children are likely to be influenced by external factors, such as parents and peers.22–24 For example, some young adolescents may be left home alone around friends who smoke; they may mimic others and simply pick up a cigarette. Those who pass through preadolescence without smoking may face new risks in high school. Most youths have more freedom from their parents in high school than they did previously. The increased unsupervised time allows adolescents more opportunities to start smoking when they feel the need, such as being with other smokers or feeling stressed or depressed.25,26 Research among young adults (primarily college students) indicates that lack of self-efficacy, being more rebellious, and previous use of other substances are among the most influential factors for smoking onset in this period.10,11,18
Further support for the existence of subgroups for smoking initiation is the research finding of subgroups with different trajectories in frequency and amount of tobacco use.27–38 Labels vary, but typical subgroups reported by these studies include nonsmokers, occasional smokers, early and late stable smokers, escalators, and quitters. Although not linked to specific developmental periods, each subgroup has its own risk curve across the age span from adolescence to young adulthood. Additionally, researchers have found significant differences in a variety of factors among trajectory subgroups, including gender, race/ethnicity, mental health, and parental monitoring.27–38 A landmark longitudinal study found that early stable smokers had more smoking friends than experimenters, abstainers, late stable smokers, and quitters; abstainers were more likely than early and late stable smokers to have enrolled in college; and late stable smokers were least likely to be married.31
We are not aware of other research examining subgroups with time patterns of smoking onset risk that are directly linked to specific periods in the life span, which has direct implications for smoking prevention. Guided by the life-course perspective, we used 12 rounds of panel data from a nationally representative sample. Our goals were to detect subgroups with distinctive time patterns regarding likelihood of smoking initiation and then to determine whether the detected subgroups varied systematically by established risk factors in adolescence and outcome measures in young adulthood.
METHODS
Data were from the National Longitudinal Survey of Youth 1997 (NLSY97), an ongoing project sponsored by the US Department of Labor. NLSY97 participants were randomly selected to represent all US adolescents aged 12 to 16 years by the end of 1996. Participants completed follow-up surveys annually after the baseline survey in 1997. Trained staff collected data at participants’ homes. The data for sensitive questions, including those for cigarette smoking, were collected by audio computer-assisted self-interviewing, whereas other data were collected by computer-assisted personal interviewing.
We analyzed data from baseline to the 2008 survey (12 rounds). At baseline, 6748 adolescents completed the survey. Of these participants, we included 4088 (60.58%) who provided data on age and smoking initiation. There were no significant differences between the included participants and those excluded regarding key variables at baseline, which included race/ethnicity (66.1% of included participants and 64.2% of those excluded were non-Hispanic White) and mean age of smoking onset (12.1 years for included vs 12.2 years for excluded); however, significantly more females than males were included (2095 vs 1993; P < .01). To minimize potential selection bias attributable to this gender difference, we analyzed the data by gender.
Smoking Initiation
Cigarette smoking initiation was self-reported. At baseline, participants who responded positively to the question “Have you ever smoked cigarettes in your life?” were further asked, “How old were you when you smoked an entire cigarette the first time?” We used the reported age of smoking the first whole cigarette to model the time trajectory of smoking initiation. Those who responded negatively to the first question at baseline were asked at subsequent follow-up surveys, “Have you ever smoked an entire cigarette since the last survey on [date of the last survey]?” We thus used respondent’s age at the time of the follow-up survey in our modeling analysis for those who responded positively in a follow-up.
Additional Variables
Baseline.
We assessed race/ethnicity as White and others (Black; American Indian, Eskimo, or Aleut; Asian or Pacific Islander; and something else). We assessed peer smoking as the perceived proportion of children in the same grade who smoked or had smoked cigarettes (1 = almost none, 2 = about 25%, 3 = about half, 4 = 75%, and 5 = all). Because of a highly skewed distribution, for analysis, we recoded this variable as 0 (almost none) and 1 (some). We assessed parental monitoring on the basis of youths’ report at age 12 to 14 years using an established instrument.39,40 Four items asked about the extent to which the youth’s parents knew (1) the youth’s close friends, (2) the friends’ parents, (3) whom the youth was with when not at home, and (4) the youth’s teachers and what the youth was doing in school (0 = knows nothing; 4 = knows everything). We assessed monitoring for mothers and fathers separately; we summed scale scores (αfather = 0.81; αmother = 0.71), with higher scores reflecting closer monitoring. We assessed depressed affect at age 12 to 14 years with 1 item from the Child Behavior Checklist scale.41 Participants indicated how often they felt unhappy, sad, or depressed (0 = not true; 1 = sometimes true; 2 = often true). We used these variables as predictors of subgroups with distinctive smoking onset risk patterns at the baseline assessment.
Age 24 years.
We assessed the following variables (scored yes or no): education (ever enrolled in a 4-year college), employment (ever employed), current smoking (smoked in the past 30 days), and marital status (currently married). These variables were used as outcome variables. We selected age 24 years because it was the last age for which we had data for all participants in the sample and because of the low likelihood of smoking initiation after this age.
Accelerated Longitudinal Design
The 12 rounds of the NLSY97 survey data from 1997 to 2008 made it possible to directly assess the risk of smoking initiation from ages 12 to 29 years using an accelerated longitudinal design (Table 1).42 To assess smoking initiation before age 12 years, we used the reported age of first smoking at baseline to reconstruct the birth cohort following the method widely used in tobacco research.3,5,9 For example, if an adolescent who was aged 14 years at baseline in 1997 reported smoking initiation at age 7 years, we used age 7 years in modeling analysis. Table 1 shows the number of participants by age and survey waves, as well as the number and percentage of participants who initiated smoking.
TABLE 1—
Accelerated Longitudinal Design, Sample Size, and Number of Persons Who Initiated Cigarette Smoking in the United States: National Longitudinal Survey of Youth 1997
| Survey Wave (Year), No. |
||||||||||||||
| Age, Years | 1 (1997) | 2 (1998) | 3 (1999) | 4 (2000) | 5 (2001) | 6 (2002) | 7 (2003) | 8 (2004) | 9 (2005) | 10 (2006) | 11 (2007) | 12 (2008) | Total, No. | Initiators, No. (%) |
| 4 | 4088 | 4088 | 28 (0.7) | |||||||||||
| 5 | 4088 | 4088 | 10 (0.2) | |||||||||||
| 6 | 4088 | 4088 | 16 (0.4) | |||||||||||
| 7 | 4088 | 4088 | 28 (0.7) | |||||||||||
| 8 | 4088 | 4088 | 47 (1.1) | |||||||||||
| 9 | 4088 | 4088 | 48 (1.2) | |||||||||||
| 10 | 4088 | 4088 | 124 (3.0) | |||||||||||
| 11 | 4088 | 4088 | 170 (4.2) | |||||||||||
| 12 | 561 | 561 | 342 (8.4) | |||||||||||
| 13 | 865 | 41 | 906 | 427 (10.4) | ||||||||||
| 14 | 884 | 821 | 47 | 1752 | 415 (10.2) | |||||||||
| 15 | 827 | 894 | 857 | 19 | 2597 | 325 (8.0) | ||||||||
| 16 | 680 | 845 | 879 | 820 | 21 | 3245 | 257 (6.3) | |||||||
| 17 | 265 | 795 | 873 | 898 | 833 | 3664 | 219 (5.4) | |||||||
| 18 | 6 | 638 | 750 | 838 | 885 | 859 | 43 | 4019 | 173 (4.2) | |||||
| 19 | 54 | 646 | 778 | 830 | 879 | 835 | 22 | 4044 | 120 (2.9) | |||||
| 20 | 36 | 669 | 802 | 854 | 901 | 843 | 35 | 4140 | 83 (2.0) | |||||
| 21 | 66 | 655 | 786 | 843 | 884 | 848 | 62 | 4144 | 61 (1.5) | |||||
| 22 | 62 | 668 | 781 | 845 | 892 | 849 | 99 | 4196 | 49 (1.2) | |||||
| 23 | 42 | 662 | 788 | 841 | 885 | 853 | 85 | 4156 | 33 (0.8) | |||||
| 24 | 23 | 673 | 799 | 854 | 891 | 848 | 4088 | 22 (0.5) | ||||||
| 25 | 33 | 642 | 798 | 850 | 887 | 3210 | 14 (0.3) | |||||||
| 26 | 31 | 624 | 777 | 849 | 2281 | 11 (0.3) | ||||||||
| 27 | 16 | 608 | 791 | 1415 | 2 (0.0) | |||||||||
| 28 | 10 | 616 | 626 | 0 | ||||||||||
| 29 | 12 | 12 | 0 | |||||||||||
Source. National Longitudinal Survey of Youth 1997 (12 rounds from 1997 to 2008). Data of year 1997 for participants aged birth to 11 years were from reconstructed cohort; data for birth to 3 years (no initiators) are not shown.
Trajectory Modeling Analysis
Developmental trajectory analysis, also known as growth mixture modeling, is a methodology devised to detect and quantify unique subgroups of a study population on the basis of a heterogeneous population assumption.43 We challenged the traditional one-age-pattern-for-all hypothesis by assuming the existence of multiple subgroups with unique age patterns for smoking initiation. We used growth mixture modeling43 (implemented with SAS PROC TRAJ procedure44 [SAS Institute, Cary, NC]) to detect these subgroups and to quantify the trajectory pattern of smoking initiation across ages and developmental periods. We used the Bayesian Information Criterion (BIC) to determine the optimal number of subgroups by evaluating whether adding 1 more group was associated with reductions in BIC of at least 5 units.
We used a 2-step procedure established from our previous experience with this method45,46 to conduct the modeling analysis. In step 1, we started with a model with a larger number of subgroups (5–7), all being set as cubic polynomial. In step 2, we revised the model by reducing the number of groups or altering the degree of the polynomial (zero to cubic) for individual subgroups, using the BIC criterion and significance tests of the estimated model coefficients.
Comparing Influential Variables by Risk Group
After establishing the subgroups with different developmental trajectories, we classified participants in the total sample into specific groups on the basis of the posterior probability. We then compared factors among the 4 smoking initiation risk subgroups using the χ2 test or analysis of variance. We completed group comparisons using the relative risk statistic with 95% confidence interval (following a significant χ2) or Dunnett’s t post hoc test (following a significant F). Because of the age restriction (12–14 years) for assessing parental monitoring and depressed affect in the NLSY97, only participants in this age range at baseline were included when these variables were used in an analysis.
RESULTS
Among the 4088 participants, 2095 (51.25%) were female and 1993 (48.75%) were male; 72% of the total sample was White. Table 1 shows that, overall, the sample included youths aged 12 through 29 years. Average age was 14.72 years (SD = 1.44) at baseline in 1997 and 26.27 (SD = 1.42) at the last wave in 2008. Overall, smoking onset was most likely at ages 13 (10.4%) and 14 (10.2%) years.
Developmental Trajectories of Smoking Initiation
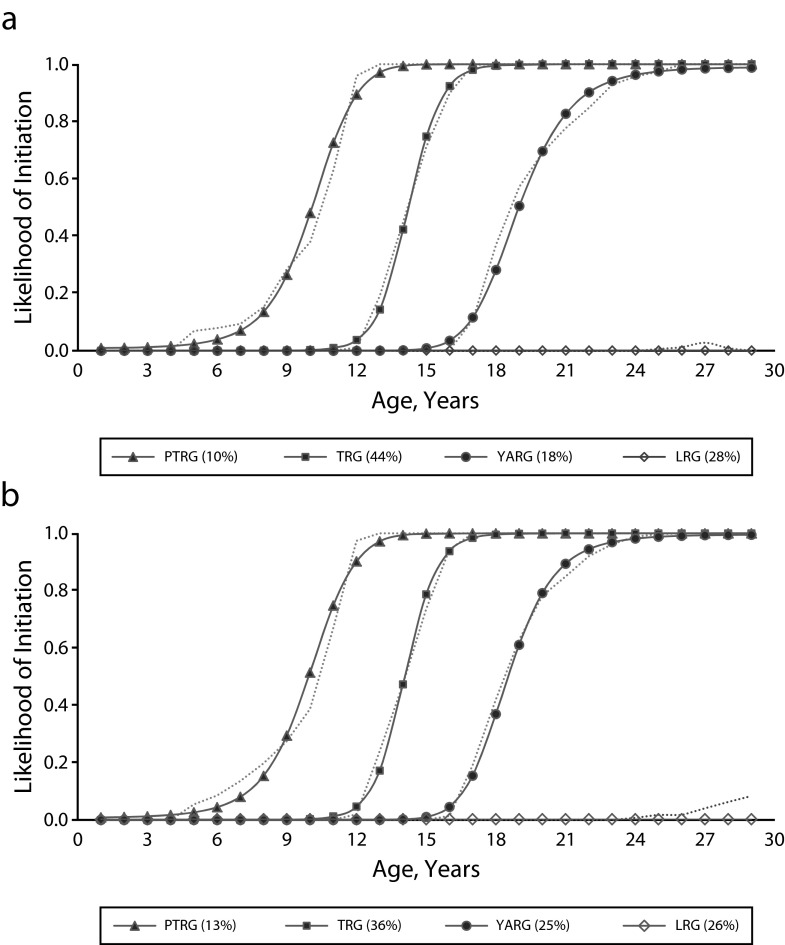
A 4-group trajectory model fit the data well for both genders (BIC = −6927.75 for females and BIC = −7027.94 for males). Figure 1 depicts the trajectories of smoking initiation by gender, and Table 2 includes the final model parameters.
FIGURE 1—
Trajectories of the likelihood of smoking initiation from birth through young adulthood among (a) US females and (b) US males: National Longitudinal Survey of Youth 1997.
Note. LRG = Low Risk Group; PTRG = Preteen Risk Group; TRG = Teenage Risk Group; YARG = Young Adult Risk Group.
TABLE 2—
Parameter Estimates of Developmental Trajectories Models of the Likelihood of Smoking Initiation Among US Young Persons: National Longitudinal Survey of Youth 1997
| Group | %a (95% CI) | Intercept (β0) | Linear (β1) | Quadratic (β3) |
| Females (n = 2095) | ||||
| PTRG | 9.69 (8.27, 11.12) | 4.98*** | 11.72*** | 3.57*** |
| TRG | 44.18 (41.83, 46.52) | −0.44*** | 10.20*** | −1.43* |
| YARG | 18.32 (16.45, 20.20) | −6.71*** | 11.27*** | −2.85*** |
| LRG | 27.81 (25.88, 29.73) | −6.91*** | ||
| Males (n = 1993) | ||||
| PTRG | 12.96 (11.32, 14.61) | 4.97*** | 11.30*** | 3.28*** |
| TRG | 36.39 (34.03, 38.74) | −0.24** | 10.20*** | −1.31 |
| YARG | 24.95 (22.82, 27.08) | −6.86*** | 12.13*** | −3.03*** |
| LRG | 25.70 (23.77, 27.63) | −5.92*** |
Note. LRG = Low Risk Group; PTRG = Preteen Risk Group; TRG = Teenage Risk Group; YARG = Young Adult Risk Group. Model fit: Bayesian Information Criterion (BIC) = −6927.75 for females and BIC = −7027.94 for males. Trajectory modeling test indicated significantly more males than females in the PTRG (t = 3.01; P < .01) and YARG (t = 4.34; P < .001).
The percentage of each gender represented in each risk group.
*P < .05; **P < .01; ***P < .001.
Data in Figure 1a illustrate 4 subgroups of females with distinctive developmental trajectories of smoking onset likelihood. We labeled the first one the Pre-Teenage Risk Group (PTRG; 9.69% of the sample). This group was characterized by a low risk (< 5.0%) of smoking onset before age 6 years. The risk increased rapidly thereafter, approaching 100% at age 12 years. A similar but slightly steeper risk curve characterized the second group, the Teenage Risk Group (TRG; 44.18%), with the smoking onset age curve delayed 5 to 6 years. The risk was rather low before age 12 years and increased rapidly thereafter, approaching 100% at age 18 years. The risk curve for the third group, the Young Adult Risk Group (YARG; 18.32%), started to grow after age 17 years, rapidly increased thereafter, and started approaching 100% at age 24 years. Finally, the risk curve for the last group, the Low Risk Group (LRG; 27.81%), was basically flat throughout the study age range of birth to 29 years. Ten women (1.7%) in the LRG began smoking between ages 23 and 26 years.
Data in Figure 1b demonstrate a 4-group developmental trajectory pattern for males. The pattern was similar to that for females, except for a few differences. The risk curves for the TRG (t = 2.67; P < .01), YARG (t = 4.59; P < .001), and LRG (t = 2.47, P < .05) of males increased slightly quicker along the horizontal age line than those of females. Of the males, 12.96% were in the PTRG, 36.39% in the TRG, 24.95% in the YARG, and 25.70% in the LRG. Twenty men (3.9%) included in the LRG began smoking after age 23 years. Trajectory analysis indicated that significantly more males than females were included in the PTRG (t = 3.01; P < .01) and YARG (t = 4.34; P < .01).
As shown in Table 2, for both genders, the PTRG, TRG, and YARG were adequately described by a binomial model, whereas the LRG was adequately described with an intercept-only model. With the exception of the quadratic term for males in the TRG, all model coefficients were statistically significant. The PTRG, TRG, and YARG all contained a positive linear growth component (β1); the quadratic component β2 was positive and greatest for the PTRG but declined in the TRG and YARG.
Factors Associated With Individual Risk Groups
Table 3 summarizes the results from the analyses comparing the 4 risk groups. Overall, differences tended to be strongest between the PTRG with LRG and weaker between the YARG with LRG. Among females, all 9 variables showed significant differences between the PTRG and LRG. Females in the PTRG were significantly more likely than LRG females to be White, to have peers who smoked, to be married, and to currently smoke, and less likely to have attended a 4-year college and to be employed. PTRG females also reported significantly lower paternal and maternal monitoring and higher depressed affect than LRG females. The same pattern was found between TRG and LRG females, except that marital status was no longer significantly different. There were fewer differences between YARG females and LRG females. YARG females were significantly more likely than LRG females to be White, less likely to have attended college, and more likely to currently smoke.
TABLE 3—
Factors Associated With Detected Risk Groups of Smoking Initiation Among Young US Females and Males: National Longitudinal Survey of Youth 1997
| Smoking Initiation Risk Group |
||||||
| Variable | PTRG | TRG | YARG | LRG | No. | Omnibus Statistic |
| Females, baseline variables | ||||||
| Race/ethnicity | ||||||
| White, % | 74.51 | 77.41 | 67.02 | 59.31 | 2088 | χ2 = 58.31*** |
| RR (95% CI) | 2.01 (1.41, 2.86) | 2.35 (1.87, 2.95) | 1.39 (1.06, 1.83) | 1.00 (Ref) | ||
| Peer smoking | ||||||
| Some, % | 88.18 | 83.03 | 69.97 | 66.02 | 2066 | χ2 = 77.51*** |
| RR (95% CI) | 3.84 (2.42, 6.08) | 2.52 (1.97, 3.21) | 1.20 (0.91, 1.59) | 1.00 (Ref) | ||
| Parental monitoring | ||||||
| Father, mean (SD) | 6.09 (4.20)a | 7.56 (3.77)a | 9.28 (3.69) | 9.35 (3.73) | 1012 | F = 28.38*** |
| Mother, mean (SD) | 9.35 (3.23)a | 10.18 (3.16)a | 11.33 (2.88) | 11.43 (3.01) | 1290 | F = 24.57*** |
| Depressed affect, mean (SD) | 0.90 (0.70)a | 0.69 (0.67)a | 0.47 (0.60) | 0.46 (0.59) | 1328 | F = 24.04*** |
| Females, variables at age 24 y | ||||||
| Education | ||||||
| No college, % | 73.66 | 55.50 | 43.27 | 35.16 | 2095 | χ2 = 109.36*** |
| RR (95% CI) | 5.16 (3.62, 7.35) | 2.30 (1.86, 2.85) | 1.41 (1.08, 1.83) | 1.00 (Ref) | ||
| Employment | ||||||
| Ever employed, % | 82.67 | 83.08 | 87.27 | 88.56 | 2078 | χ2 = 10.70* |
| RR (95% CI) | 0.62 (0.39, 0.96) | 0.63 (0.47, 0.86) | 0.89 (0.60, 1.32) | 1.00 (Ref) | ||
| Currently smoking | ||||||
| Yes, % | 67.58 | 54.87 | 38.59 | 0.36 | 1864 | χ2 = 106.37*** |
| RR (95% CI) | 570.15 (137.68, 2361.14) | 332.49 (82.54, 1339.38) | 171.83 (42.15, 700.52) | 1.00 (Ref) | ||
| Marital status | ||||||
| Currently married, % | 22.17 | 17.15 | 13.46 | 15.78 | 2092 | χ2 = 7.66* |
| RR (95% CI) | 1.52 (1.02, 2.27) | 1.10 (0.83, 1.46) | 0.83 (0.57, 1.20) | 1.00 (Ref) | ||
| Males, baseline variables | ||||||
| Race/ethnicity | ||||||
| White, % | 81.58 | 77.41 | 68.06 | 72.48 | 1976 | χ2 = 21.79*** |
| RR (95% CI) | 1.68 (1.17, 2.43) | 1.30 (1.00, 1.69) | 0.81 (0.62, 1.06) | 1.00 (Ref) | ||
| Peer smoking | ||||||
| Some, % | 80.75 | 75.18 | 61.65 | 55.58 | 1970 | χ2 = 78.16*** |
| RR (95% CI) | 3.35 (2.36, 4.77) | 2.42 (1.89, 3.09) | 1.28 (1.00, 1.65) | 1.00 (Ref) | ||
| Parental monitoring | ||||||
| Father, mean (SD) | 6.76 (3.97)a | 8.29 (3.70)a | 9.38 (3.50) | 9.17 (3.81) | 1022 | F = 17.98*** |
| Mother, mean (SD) | 8.71 (3.61)a | 9.80 (3.22)a | 10.87 (2.77) | 10.73 (3.16) | 1246 | F = 23.09*** |
| Depressed affect, mean (SD) | 0.55 (0.66) | 0.53 (0.60)a | 0.40 (0.56) | 0.42 (0.56) | 1292 | F = 4.98** |
| Males, variables at age 24 y | ||||||
| Education | ||||||
| No college, % | 77.82 | 63.38 | 50.20 | 39.14 | 1993 | χ2 = 125.87*** |
| RR (95% CI) | 5.46 (3.89, 7.66) | 2.69 (2.13, 3.40) | 1.57 (1.22, 2.01) | 1.00 (Ref) | ||
| Employment | ||||||
| Ever employed, % | 85.88 | 87.04 | 87.58 | 87.82 | 1972 | χ2 = 0.66 |
| RR (95% CI) | 0.84 (0.54, 1.31) | 0.93 (0.66, 1.31) | 0.98 (0.67, 1.42) | 1.00 (Ref) | ||
| Currently smoking | ||||||
| Yes, % | 68.51 | 62.58 | 52.34 | 0.61 | 1763 | χ2 = 108.49*** |
| RR (95% CI) | 351.74 (109.56, 1129.24) | 270.37 (86.02, 849.82) | 177.52 (56.26, 560.17) | 1.00 (Ref) | ||
| Marital status | ||||||
| Currently married, % | 9.40 | 9.89 | 5.53 | 9.39 | 1991 | χ2 = 7.97* |
| RR (95% CI) | 1.00 (0.60, 1.66) | 1.06 (0.72, 1.56) | 0.57 (0.35, 0.92) | 1.00 (Ref) | ||
Note. CI = confidence interval; LRG = Low Risk Group; PTRG = Preteen Risk Group; RR = risk ratio; TRG = Teenage Risk Group; YARG = Young Adult Risk Group. 95% CIs not containing 1.00 are significantly different from the LRG. Female sample was as follows: for PTRG, n = 205 (9.79%); for TRG, n = 928 (44.30%); for YARG, n = 379 (18.09%); for LRG, n = 583 (27.83%). Male sample was as follows: for PTRG, n = 266 (13.35%); for TRG, n = 710 (35.62%); for YARG, n = 506 (25.39%); for LRG, n = 511 (25.64%).
Significantly different from the LRG mean when Dunnett’s t test was used.
*P < .05; **P < .01; ***P < .001.
Generally, males exhibited group differences similar to those of females. However, there was no association between employment status and smoking initiation risk group for males. In addition, compared with LRG males, YARG males were significantly more likely to have had smoking peers in adolescence and significantly less likely to be currently married. There were no differences in racial makeup between YARG and LRG males, or in marital status between PTRG and LRG males.
DISCUSSION
Understanding smoking initiation is critical to strengthening current tobacco prevention efforts. Traditionally, the risk of smoking initiation is viewed as a homogeneous process, generally increasing over time as youths enter and pass through adolescence.10–13 In this study, we explored the process of smoking initiation through a new analytical strategy based on a heterogeneous hypothesis. We tested the hypothesis using the accelerated design and longitudinal data collected from a large, nationally representative sample. We first confirmed the existence of 4 distinct and mutually exclusive subgroups of US youths. Each risk subgroup had its own time curve for smoking initiation. Furthermore, these subgroups were clearly linked with different developmental periods, from preschool age to young adulthood. Finally, comparison analyses revealed potential impacts of risk factors in early adolescence that may have contributed to smoking onset for individual subgroups, and outcome measures that may have been affected by these risk subgroups.
Early initiation of tobacco use has been linked to an increased likelihood of long-duration smoking, higher risk of nicotine dependence, and a greater lifelong risk of developing smoking-related cancers.47,48 Great effort has therefore been devoted to understanding the timing of and risk factors associated with the early onset of tobacco use.3–9 We identified 4 subgroups with distinctive risk trajectories for smoking onset, supporting the heterogeneous hypothesis. The first 3 groups were characterized by initiating smoking before age 12 years (PTRG), between ages 13 and 18 years (TRG), and after age 17 years (YARG), and the LRG was characterized by a zero risk (before age 22 years) to low risk (3%, after age 22 years) to initiate smoking over a period of the first 29 years in life.
The homogeneous hypothesis suggests that adolescence is the risk zone for smoking initiation. However, the current study demonstrates that there are 3 periods with heightened risk of smoking onset, with each being unique to a specific subgroup. The 3 high-risk groups (i.e., PTRG, TRG, and YARG) can be considered as 3 “tests”: 1 for preadolescents, 1 for adolescents, and 1 for young adults. From preadolescence to young adulthood, a person will be less likely to initiate smoking only if he or she “passes” all the 3 tests. Our study findings indicate that approximately 11% of US youths failed the first test by starting smoking before age 12 years; approximately 40% (the TRG) failed the second test, even though they passed the first one by not starting smoking before 12 years; and approximately 22% failed the third test (YARG) and initiated smoking during young adulthood, although they passed the 2 previous tests. Overall, only about 27% US youths passed the 3 tests (LRG) by age 29 years.
There were marked differences across subgroups in variables associated with smoking initiation. Relative to girls, boys were more likely to be in the PTRG and YARG. There were larger proportions of White youths in both the PTRG and TRG, and in the female YARG, than in LRG groups. Consistent with previous research suggesting that earlier smoking initiation is associated more strongly with external factors,22–24 we found more peer smokers among those who started smoking earlier. Peer smoking was most common for PTRG youths, followed by TRG youths and then YARG youths. Parental monitoring was lower and depression was higher among PTRG and TRG youths than among YARG and LRG youths.
In addition, risk group membership significantly predicted a number of variables measured at age 24 years. Relative to individuals in the LRG, participants in other subgroups who had initiated smoking were less likely to have been admitted into a 4-year college and more likely to be currently smoking. The risk to smoke later in life was also substantially higher for youths in the 3 risk groups (PTRG, TRG, and YARG), both males and females, compared with the LRG youths. Interestingly, the relationships linking smoking initiation risk group with college acceptance and marital status were weaker for males than for females.
Identification of the distinctive subgroups with unique time patterns of risk trajectories for smoking onset has important implications for strengthening tobacco control. First, the risk subgroups are clearly associated with schooling (preadolescence associated with grade school level, adolescence with middle and high school level, and young adulthood starting after high school). This finding adds new evidence supporting the strategy of school-based smoking prevention programs.2 Furthermore, continued smoking prevention must be maintained across all school grades from primary school to college, with emphasis on the high school period, when approximately 40% of US youths smoked their first cigarette.
Our findings also provide evidence supporting appropriate selection of targeted risk factors for intervention at different periods. Early prevention programs should target emotional issues (e.g., depressed affect), peer influence, and parental monitoring to assist US adolescents with passing the first 2 tests by not initiating smoking. Lastly, tobacco use prevention during young adulthood may need to strengthen regulatory and policy measures related to education and employment places to assist US youths with passing the third test by not initiating smoking during this period.49
This study is among the first to systematically investigate the risk of smoking initiation with a life-course perspective, and the findings are unique and promising; however, there are several limitations. The study relied on self-reported age of smoking initiation; measurement error could not be assessed at the individual level. Furthermore, initiation of smoking before age 12 years was retrospectively reported within a much longer period (from birth to baseline assessment) compared with initiation of smoking at age 12 years or older (reported at follow-up, with duration varying from 6 months to 23 months). The differential recall periods may result in biased age data because of forward telescoping.50 Lastly, the analysis of factors associated with smoking onset risk subgroups was limited by the variables available from the NLSY97.
Despite these limitations, this study’s findings advance our understanding of the process of smoking initiation. The likelihood of smoking initiation is not homogeneous across the life span; rather, individuals in different risk groups face increased risks of smoking at different developmental periods, and such risks are associated with different influential factors. These findings provide new evidence supporting both etiological and prevention intervention studies targeting risk subgroups at different developmental periods. To win the war against tobacco, future research should adapt the heterogeneity strategy to continue exploring factors affecting the risk of smoking initiation by subgroups, to improve the existing tobacco prevention programs, and to devise new and more effective programs.
Acknowledgments
This study was supported in part by a research grant from the National Institutes of Health (award R01 DA022730; X. C., PI).
Yifan Jiang provided assistance in data processing and some preliminary analysis under the guidance of X. Chen.
Human Participant Protection
The study protocol was approved by the Human Investigation Committee at Wayne State University.
References
- 1.Dietz NA, Westphal L, Arheart KL et al. Changes in youth cigarette use following the dismantling of an antitobacco media campaign in Florida. Prev Chronic Dis. 2010;7(3):A65. [PMC free article] [PubMed] [Google Scholar]
- 2.Chen X, Ren Y, Lin F, MacDonell K, Jiang YF. Exposure to school and community based prevention programs and reductions in cigarette smoking among adolescents in the United States, 2000–08. Eval Program Plann. 2012;35(3):321–328. doi: 10.1016/j.evalprogplan.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen X, Li Y, Unger JB, Gong J, Johnson CA, Guo Q. Hazard of smoking initiation by age among adolescents in Wuhan, China. Prev Med. 2001;32(5):437–445. doi: 10.1006/pmed.2001.0826. [DOI] [PubMed] [Google Scholar]
- 4.Edelen MO, Tucker JS, Ellickson PL. A discrete time hazards model of smoking initiation among West Coast youth from age 5 to 23. Prev Med. 2007;44(1):52–54. doi: 10.1016/j.ypmed.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Chen X, Unger JB. Hazards of smoking initiation among Asian American and non-Asian adolescents in California: a survival model analysis. Prev Med. 1999;28(6):589–599. doi: 10.1006/pmed.1999.0487. [DOI] [PubMed] [Google Scholar]
- 6.Lau M, Chen X, Ren Y. Increased risk of cigarette smoking among immigrant children and girls in Hong Kong: an emerging public health issue. J Community Health. 2012;37(1):144–152. doi: 10.1007/s10900-011-9428-9. [DOI] [PubMed] [Google Scholar]
- 7.Bidstrup PE, Tjornhoj-Thomsen T, Mortensen EL, Vinther-Larsen M, Johansen C. Critical discussion of social-cognitive factors in smoking initiation among adolescents. Acta Oncol. 2011;50(1):88–98. doi: 10.3109/02841861003801155. [DOI] [PubMed] [Google Scholar]
- 8.Pederson LL, Lefcoe NM. Change in smoking status among a cohort of late adolescents: prediction and explanation of initiation, maintenance and cessation. Int J Epidemiol. 1986;15(4):519–526. doi: 10.1093/ije/15.4.519. [DOI] [PubMed] [Google Scholar]
- 9.Kandel DB, Kiros GE, Schaffran C, Hu MC. Racial/ethnic differences in cigarette smoking initiation and progression to daily smoking: a multilevel analysis. Am J Public Health. 2004;94(1):128–135. doi: 10.2105/ajph.94.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Myers MG, Doran NM, Trinidad DR, Wall TL, Klonoff EA. A prospective study of cigarette smoking initiation during college: Chinese and Korean American students. Health Psychol. 2009;28(4):448–456. doi: 10.1037/a0014466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Von Ah D, Ebert S, Ngamvitroj A, Park N, Kang DH. Factors related to cigarette smoking initiation and use among college students. Tob Induc Dis. 2005;3(1):27–40. doi: 10.1186/1617-9625-3-1-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Everett SA, Husten CG, Kann L, Warren CW, Sharp D, Crossett L. Smoking initiation and smoking patterns among US college students. J Am Coll Health. 1999;48(2):55–60. doi: 10.1080/07448489909595674. [DOI] [PubMed] [Google Scholar]
- 13.Baron-Epel O, Haviv-Messika A. Factors associated with age of smoking initiation in adult populations from different ethnic backgrounds. Eur J Public Health. 2004;14(3):301–305. doi: 10.1093/eurpub/14.3.301. [DOI] [PubMed] [Google Scholar]
- 14.Kuh D, Ben-Shlomo Y. A Life Course Approach to Chronic Disease Epidemiology. 2nd ed. New York, NY: Oxford University Press; 2004. [Google Scholar]
- 15.Johnson MK, Crosnoe R, Elder GH., Jr Insights on adolescence from a life course perspective. J Res Adolesc. 2011;21(1):273–280. doi: 10.1111/j.1532-7795.2010.00728.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hutchison ED. A life course perspective. In: Hutchison ED, editor. Dimensions of Human Behavior: The Changing Life Course. 3rd ed. Thousand Oaks, CA: Sage; 2008. pp. 1–38. [Google Scholar]
- 17.Chen X, Stacy A, Zheng H et al. Sensations from initial exposure to nicotine predicting adolescent smoking in China: a potential measure of vulnerability to nicotine. Nicotine Tob Res. 2003;5(4):455–463. doi: 10.1080/14622200307239. [DOI] [PubMed] [Google Scholar]
- 18.Choi WS, Harris KJ, Okuyemi K, Ahluwalia JS. Predictors of smoking initiation among college-bound high school students. Ann Behav Med. 2003;26(1):69–74. doi: 10.1207/S15324796ABM2601_09. [DOI] [PubMed] [Google Scholar]
- 19.Simons-Morton BG. Prospective analysis of peer and parent influences on smoking initiation among early adolescents. Prev Sci. 2002;3(4):275–283. doi: 10.1023/a:1020876625045. [DOI] [PubMed] [Google Scholar]
- 20.Hofstetter CR, Hovell MF, Jung KR, Raman R, Irvin V, Ni R. The first puff: forces in smoking initiation among Californians of Korean descent. Nicotine Tob Res. 2007;9(12):1277–1286. doi: 10.1080/14622200701704863. [DOI] [PubMed] [Google Scholar]
- 21.Kremers SP, Mudde AN, De Vries H. Model of unplanned smoking initiation of children and adolescents: an integrated stage model of smoking behavior. Prev Med. 2004;38(5):642–650. doi: 10.1016/j.ypmed.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Bidstrup PE, Frederiksen K, Siersma V et al. Social-cognitive and school factors in initiation of smoking among adolescents: a prospective cohort study. Cancer Epidemiol Biomarkers Prev. 2009;18(2):384–392. doi: 10.1158/1055-9965.EPI-08-0584. [DOI] [PubMed] [Google Scholar]
- 23.Unger JB, Yan L, Shakib S et al. Peer influences and access to cigarettes as correlates of adolescent smoking: a cross-cultural comparison of Wuhan, China, and California. Prev Med. 2002;34(4):476–484. doi: 10.1006/pmed.2001.0996. [DOI] [PubMed] [Google Scholar]
- 24.Voorhees CC, Ye C, Carter-Pokras O et al. Peers, tobacco advertising, and secondhand smoke exposure influences smoking initiation in diverse adolescents. Am J Health Promot. 2011;25(3):e1–e11. doi: 10.4278/ajhp.090604-QUAN-180. [DOI] [PubMed] [Google Scholar]
- 25.Audrain-McGovern J, Rodriguez D, Kassel JD. Adolescent smoking and depression: evidence for self-medication and peer smoking mediation. Addiction. 2009;104(10):1743–1756. doi: 10.1111/j.1360-0443.2009.02617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, Bowes G. Depression, anxiety, and smoking initiation: a prospective study over 3 years. Am J Public Health. 1998;88(10):1518–1522. doi: 10.2105/ajph.88.10.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brook DW, Brook JS, Zhang C, Whiteman M, Cohen P, Finch SJ. Developmental trajectories of cigarette smoking from adolescence to the early thirties: personality and behavioral risk factors. Nicotine Tob Res. 2008;10(8):1283–1291. doi: 10.1080/14622200802238993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Orlando M, Tucker JS, Ellickson PL, Klein DJ. Developmental trajectories of cigarette smoking and their correlates from early adolescence to young adulthood. J Consult Clin Psychol. 2004;72(3):400–410. doi: 10.1037/0022-006X.72.3.400. [DOI] [PubMed] [Google Scholar]
- 29.White HR, Pandina RJ, Chen PH. Developmental trajectories of cigarette use from early adolescence into young adulthood. Drug Alcohol Depend. 2002;65(2):167–178. doi: 10.1016/s0376-8716(01)00159-4. [DOI] [PubMed] [Google Scholar]
- 30.Bernat DH, Erickson DJ, Widome R, Perry CL, Forster JL. Adolescent smoking trajectories: results from a population cohort study. J Adolesc Health. 2008;43(4):334–340. doi: 10.1016/j.jadohealth.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chassin L, Presson C, Pitts SC, Sherman SJ. The natural history of cigarette smoking from adolescence to adulthood in a midwestern community sample: multiple trajectories and heir psychosocial correlates. Health Psychol. 2000;19(3):223–231. [PubMed] [Google Scholar]
- 32.Chen X, Unger JB, Palmer P et al. Prior cigarette smoking initiation predicting current alcohol use: evidence for a gateway drug effect among California adolescents from eleven ethnic groups. Addict Behav. 2002;27(5):799–817. doi: 10.1016/s0306-4603(01)00211-8. [DOI] [PubMed] [Google Scholar]
- 33.Costello DM, Dierker LC, Jones BL, Rose JS. Trajectories of smoking from adolescence to early adulthood and their psychosocial risk factors. Health Psychol. 2008;27(6):811–818. doi: 10.1037/0278-6133.27.6.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ennett ST, Faris R, Hipp J et al. Peer smoking, other peer attributes, and adolescent cigarette smoking: a social network analysis. Prev Sci. 2008;9(2):88–98. doi: 10.1007/s11121-008-0087-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Juon HS, Ensminger ME, Sydnor KD. A longitudinal study of developmental trajectories to young adult cigarette smoking. Drug Alcohol Depend. 2002;66(3):303–314. doi: 10.1016/s0376-8716(02)00008-x. [DOI] [PubMed] [Google Scholar]
- 36.Soldz S, Cui X. Pathways through adolescent smoking: a 7-year longitudinal grouping analysis. Health Psychol. 2002;21(5):495–504. [PubMed] [Google Scholar]
- 37.Tucker JS, Ellickson PL, Orlando M, Klein DJ. Cigarette smoking from adolescence to young adulthood: women’s developmental trajectories and associates outcomes. Womens Health Issues. 2006;16(1):30–37. doi: 10.1016/j.whi.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 38.White HR, Nagin D, Replogle E, Stouthamer-Loeber M. Racial differences in trajectories of cigarette use. Drug Alcohol Depend. 2004;76(3):219–227. doi: 10.1016/j.drugalcdep.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 39.Hetherington EM, Cox M, Cox R. Effects of divorce on parents and children. In: Lamb ME, editor. Nontraditional Families. Hillsdale, NJ: Erlbaum; 1982. pp. 233–288. [Google Scholar]
- 40.Maccoby EE, Mnookin RH. Dividing the Child: Social and Legal Dilemmas of Custody. Cambridge, MA: Harvard University Press; 1992. [Google Scholar]
- 41.Achenbach T, Edelbrock C. The Manual for the Youth Self-Report and Profile. Burlington, VT: University of Vermont; 1987. [Google Scholar]
- 42.Rothman KJ, Grenland S, Lash TL. Modern Epidemiology. 3rd ed. Philadelphia, PA: Lippincott, Williams, & Wilkins; 2008. [Google Scholar]
- 43.Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol Methods. 1999;4(2):139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 44.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29(3):374–393. [Google Scholar]
- 45.Li X, Fang X, Stanton B et al. Psychometric evaluation of the Trauma Symptoms Checklist for Children (TSCC) among children affected by HIV/AIDS in China. AIDS Care. 2009;21(3):261–270. doi: 10.1080/09540120802195119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen X, Naar-King S, Murphy D, Parson JT. A clinic-based motivational intervention improves condom use among subgroups of youth living with HIV-A multicenter randomized controlled trial. J Adolesc Health. 2011;49(2):193–198. doi: 10.1016/j.jadohealth.2010.11.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.National Cancer Institute. Cancer Trends Progress Report 2009/2010 Update. Bethesda, MD: National Cancer Institute, National Institutes of Health; 2010. [Google Scholar]
- 48.Riggs NR, Chou C-P, Li C, Pentz MA. Adolescent to emerging adulthood smoking trajectories: when do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine Tob Res. 2007;9(11):1147–1154. doi: 10.1080/14622200701648359. [DOI] [PubMed] [Google Scholar]
- 49.Pabayo R, O’Loughlin J, Barnett TA, Cohen JE, Gauvin L. Does intolerance of smoking at school or in restaurants or corner stores decrease cigarette use initiation in adolescents? Nicotine Tob Res. 2012;14(10):1154–1160. doi: 10.1093/ntr/ntr326. [DOI] [PubMed] [Google Scholar]
- 50.Johnson EO, Schultz L. Forward telescoping bias in reported age of onset: an example from cigarette smoking. Int J Methods Psychiatr Res. 2005;14(3):119–129. doi: 10.1002/mpr.2. [DOI] [PMC free article] [PubMed] [Google Scholar]