Abstract
There is a strong body of literature that lends support to the health-promoting effects of an optimistic personality disposition, observed across various physical and psychological dimensions. In accordance with this evidence base, it has been suggested that optimism may positively influence the course and experience of pain. Although the associations among optimism and pain outcomes have only recently begun to be adequately studied, emerging experimental and clinical research links optimism to lower pain sensitivity and better adjustment to chronic pain. This review highlights recent studies that have examined the effects of optimism on the pain experience using samples of individuals with clinically painful conditions as well as healthy samples in laboratory settings. Furthermore, factors such as catastrophizing, hope, acceptance and coping strategies, which are thought to play a role in how optimism exerts its beneficial effects on pain, are also addressed.
Introduction
Optimism is a dimension of personality that received substantially increased research attention throughout the 1980’s and 90’s given its presumed ability to positively impact individuals’ health and subjective well-being during times of adversity. Scientific interest in optimism continues, and indeed, the vast majority of empirical evidence thus far has shown that optimism reliably exerts widespread mental and physical health promoting effects [1–4]. Optimism is an individual difference factor that relates to generalized outcome expectancies and was defined by Scheier and Carver [5] on the basis of their broader theory of self-regulation [6]. Individuals high in optimism are people who expect positive outcomes to occur in their future. As a consequence, they expect to cope effectively with everyday stress and challenge. Conversely, individuals who are low in optimism expect negative outcomes in their future and do not expect to cope successfully [reviewed in 5, 7, 8]. Individuals high in optimism are likely to persist in their goal-directed efforts, whereas those with low optimism are more likely to withdraw effort, become passive, and potentially give up on achieving their goals. As such, individuals with greater levels of optimism are hypothesized to demonstrate enhanced resilience to stressful situations and to experience greater physical and psychological well-being than their counterparts with low optimism. Support for this hypothesis has come from previous research which has shown that a high level of optimism is linked to both enhanced physiological recovery and psychosocial adjustment to coronary artery bypass surgery, bone marrow transplant, postpartum depression, traumatic brain injury, Alzheimer’s disease, lung cancer, breast cancer, and failed in vitro fertilization [9*]. Whether or not optimism might similarly exert beneficial effects on the experience of pain is a topic that would benefit from greater clarification.
Other positive psychological constructs related to optimism have been shown to be important factors in biopsychosocial models predicting how individuals adjust to acute and chronic pain experiences [10], particularly hopefulness and acceptance. Hopefulness has been conceptualized as a cognitive set involving both agency (i.e., the belief in one’s ability to initiate and sustain actions) and pathways (i.e., the belief in ones’ ability to generate routes to achieve desired goals) [11]. In line with this conceptualization, high levels of hope have been found to be related to lower levels of pain, psychological distress, and functional disability in patients with chronic illnesses such as traumatic brain injury [12], HIV [13], and cancer [14]. Acceptance of pain involves accepting what cannot be changed, reducing unsuccessful attempts at eliminating pain and engaging in valued activities despite pain [15]. Pain acceptance is not giving up and succumbing to the pain, but rather accepting pain as a part of life and learning how to live more effectively in spite of it. Studies have shown that, over time, individuals with higher levels of pain acceptance actually tend to report significantly lower levels of pain and pain-related disability [16, 17]. Given that optimism is related to positive expectancies for the future and the ability to adapt, one might expect that persons with a high level of optimism are more likely to report greater hopefulness and pain acceptance. Along this vein, it is conceivable that optimism could indirectly influence the experience of pain through hopefulness and pain acceptance. At this time it seems that the field of pain medicine and research could benefit from a thorough review of the literature addressing positive psychological variables, particularly optimism, in relation to the pain experience.
In 2000, Garofalo conducted a review of the then scant body of literature specifically addressing whether optimism confers any benefit for the experience and management of chronic pain [18]. At the time, the influence of optimism on individuals’ experiences of chronic pain, or any type of pain for that matter, had never been systematically examined. Garofalo reasoned that one likely explanation for the sparse attention given to the relationship between optimism and chronic pain was that the overwhelming majority of relevant studies (at the time of his review) had predominantly focused on negative personality and psychological constructs that increase the risk for poor pain outcomes. For instance, pain catastrophizing, depressed mood, and neuroticism all exert deleterious effects on the experience of pain [19–21], and a common pain psychology treatment goal involves reducing the negative impact of these factors. Despite the limited number of studies from which to draw conclusions [22, 23], Garofalo’s review led him to tentatively assert that preliminary evidence supports the positive effects of optimism on the experience of pain and its course of treatment. Over the past decade, the consensus that optimism positively influences the course and experience of acute and chronic pain as well as individuals’ responses to pain treatments has continued to grow. This has resulted in increased efforts to examine the influence of optimism on pain outcomes in clinical settings, as well as experimental pain sensitivity, placebo analgesia, and endogenous pain processing. This article summarizes the literature since Garofalo’s review that is derived from clinical and experimental research examining the associations between optimism and the experience of pain.
Optimism and clinically painful conditions
Chronic pain
The preponderance of recent research relating optimism to the experience of persistent pain indicates that optimists typically report experiencing less intense pain than pessimists and may also respond better to treatment. For example, in a heterogeneous sample of patients with different types of cancer (all solid tumor cancers or non-Hodgkins lymphoma), greater optimism predicted less severe pain intensity reports following a 10 week pain and fatigue symptom control intervention [24]. The positive association between greater optimism and less severe cancer-related pain was further corroborated in a Chinese sample of patients with lung cancer [25], as well as a French sample of patients with head and neck cancer [26]. It appears that the positive influence of optimism is not just limited to cancer pain, but also extends to pain of musculoskeletal origins. A study of patients with osteoarthritis revealed that greater optimism was significantly correlated with reports of less severe pain as well as greater life satisfaction [27]. Likewise, greater optimism was related to less pain in separate samples of patients with rheumatoid arthritis [28] and temporomandibular joint disorder [29]. Not every study has revealed a significant relationship between optimism and pain. For instance, optimism did not significantly correlate with pain ratings in a sample of adolescents with sickle cell disease [30]; however, optimism was shown to be a significant moderator of the relationship between pain intensity and daily opioid medication use. This finding suggests that the more optimistic adolescents with sickle cell were better able to match their opioid use to their pain severity relative to pessimistic adolescents.
Adjustment to chronic pain
It is possible that individuals with greater optimism have better chronic pain outcomes because they are less attentive to pain and better able to adjust to life with a pain condition. Support for this notion comes from research described by Affleck, Tennen, and Apter [31], whereby it was revealed that optimistic asthma patients were less attentive to increases in pain than pessimistic asthma patients. Similarly, optimists reported attending less to painful sensations than pessimists in a sample of elderly osteoarthritis patients [32]. In addition to its associations with less attention to pain, optimism has also been reported to promote better pain-related functioning, less psychological distress, and less engagement in maladaptive cognitive processes such as pain catastrophizing [33, 34]. Along this vein, greater optimism was associated with higher levels of positive daily mood, more life satisfaction, and fewer pain-related activity limitations in patients with rheumatoid arthritis [28, 35]. In a separate study of women with rheumatoid arthritis, it was reported that greater optimism was associated with less catastrophizing about reoccurring pain [36].
Post-operative pain
In addition to its beneficial influence on persistent pain and treatment responses, empirical evidence has also shown that greater optimism measured pre-operatively is related with improved outcomes following major invasive and minor elective surgeries. In a sample of patients recovering from coronary artery bypass graft (CABG) surgery, those with greater optimism reported experiencing less severe pain at two weeks, one month, and three months following surgery compared to patients with low optimism [37]. Optimism was also related with a more favorable recovery and greater health-related quality of life at six month follow-up in a study of Dutch patients who underwent surgeries classified as minor, intermediate, or major according to anticipated level of post-operative pain [38]. However, it should be noted that optimism was not directly related with post-operative pain intensity ratings in this Dutch study. The positive impact of being optimistic has also been found in individuals receiving minimally-invasive corrective surgery. There is evidence that in a sample of adults undergoing arthroscopic knee surgery, greater optimism prospectively predicted lower ratings of pain severity one year post-operatively [39].
Optimism and induced pain in the laboratory setting
Until recently, most research on optimism and pain had been conducted outside of a laboratory setting with patient samples experiencing chronic pain or enduring painful procedures as described above. Examining optimism and pain in a laboratory setting with healthy adult samples is advantageous for two key reasons: 1) it provides a context free of numerous factors (e.g., differential pain severity, disability, medication use) that may unduly alter the relationship in patient samples, and 2) it allows for the use of sophisticated quantitative sensory testing protocols to determine whether optimism is related to the nociceptive processing of painful stimuli (i.e., pain sensitivity), or just to patients’ verbal pain reports. From the limited research described below that has examined optimism and pain in the laboratory setting, it appears that optimism is indeed related to pain sensitivity.
Pain sensitivity
Quantitative sensory testing (QST) is an approach to pain sensitivity assessment that is derived from experimental psychophysics and consists of measuring the responses evoked by various standardized modalities of noxious stimulation (e.g., heat, cold, mechanical, ischemic) [40]. Optimism has recently been shown to be associated with the percept of pain produced by QST across several different stimulation modalities. For example, in a study of healthy adults, participants were subjected to a cold pressor task (CPT) and had their blood pressure monitored in order to examine responses to cold pain [41]. Results showed that participants with the highest levels of optimism not only provided the least intense ratings of pain (i.e., less pain sensitivity), but also demonstrated lower cardiovascular reactivity and reported less distress due to the CPT. A follow-up study conducted by Hood and colleagues [42*] corroborated these findings in a separate sample of healthy adults by also reporting that greater optimism was associated with less severe ratings of pain intensity in response to the CPT.
The effects of optimism on pain sensitivity appear to extend to other QST modalities as well. Costello and colleagues induced ischemic pain using a submaximal effort tourniquet procedure, which was done to examine interleukin-6 (a pro-inflammatory cytokine) levels during stress in relation to optimism and pain sensitivity in a sample of patients with temporomandibular joint disorder (TMJD) [43]. In this study it was revealed that TMJD patients with low optimism had greater interleukin-6 levels during stress, were less able to tolerate the ischemic pain task, and subsequently rated their experience of ischemic pain as more unpleasant when compared to TMJD patients with high optimism. This study and others [41, 42*] highlight the association of optimism with a single instance of evoked pain; however, whether optimism promotes the ability to adapt to repeated painful stimuli, a process commonly referred to as habituation, has received only limited attention. In a study of healthy women, participants were repeatedly exposed to heat and cold pain using a contact Peltier thermode [44]. Results showed that optimism was significantly associated with participants’ ability to habituate to repeated cold pain contacts; however, this effect was less pronounced for repeated heat pain contacts. Although it remains to be empirically tested, enhanced ability to adapt/habituate to repeat occurrences of pain could be one possible explanation for why optimism has been shown to be related with better adjustment in clinical studies [28, 33, 34, 36].
One overarching limitation of the laboratory-based research that thus far has examined the effects of optimism on pain sensitivity is the correlational nature of the data. This is because the construct of optimism has historically been measured as a disposition using self-report questionnaires like the Life Orientation Test-Revised (LOT-R) [8]. The LOT-R consists of a set of statements (e.g., I’m always optimistic about my future, I rarely count of good things happening to me) to which people indicate their agreement or disagreement on a multi-point scale. This is not to say that use of the LOT-R is without merit, because the LOT-R has been instrumental in helping researchers to better understand the role of optimism in relation to pain and, more broadly, health. However, without some direct experimental manipulation of optimism, it is difficult to make causal inferences about the effects of optimism on pain sensitivity. An optimism manipulation called the “best possible self” (BPS), a positive future thinking and imagery technique, has been developed and shown to be an effective means of inducing optimism by increasing expectancies of positive future events [45*]. For greater detail regarding the BPS manipulation, readers are directed to the work of Peters and colleagues [46]. A recent Dutch study took healthy volunteers and randomized them to either the BPS manipulation or a control condition and subsequently subjected them all to the cold pressor task [47**]. The results of this study found that, relative to the control condition, the BPS manipulation was significantly associated with increased levels of optimism and in turn, this induced optimism was related to lower pain intensity ratings during the CPT. These data are some of the first to support a causal effect of optimism towards pain sensitivity.
Placebo analgesia
Several laboratory-based studies have examined the relationship of optimism with pain-related phenomena other than pain sensitivity, such as placebo analgesia. The placebo effect is a psychophysiological reaction to an inactive substance or procedure [48]. Increased attention has been devoted to the placebo effect as an outcome of interest, particularly as it relates to the experience of analgesia (i.e., decreased pain perception) [49]. Currently, there is great need to better understand predictors of placebo analgesia, as treatments for both acute and chronic pain could benefit from clinically meaningful placebo effects [50]. It has been suggested that optimism may be one such predictor, given that optimism is generally defined as the expectation for positive future outcomes and placebo effects seem to be driven by expectations [51]. To explore this possibility, a recent study by Geers and colleagues randomly assigned healthy participants to either receive a placebo expectation or no expectation prior to completing a cold pressor task [52**]. All study participants were administered the LOT-R optimism measure and had a medicinal-smelling, yet inert, cream applied to the hand that was to be submerged in the cold water. The difference in conditions involved informing the placebo expectation condition that the cream was a new topical anesthetic that possessed powerful pain-reducing effects, whereas the no expectation condition was told the cream was simply a hand-cleaning product. Results showed that greater optimism was significantly associated with lower ratings of pain intensity in the placebo expectation condition but not in the condition that received no expectation. Based upon these results, the authors concluded that optimism can be an important predictor of placebo analgesia. Further evidence supporting the ability of optimism to predict placebo analgesia comes from a separate project that incorporated research methods very similar to those described in the study by Geers and colleagues. In this separate project, it was shown that greater dispositional optimism was associated with the reproducibility of placebo analgesia, such that repeated placebo responders were individuals with the highest levels of optimism [53].
Endogenous pain processing
Recent developments in the field include classification of chronic pain as a disease of the central nervous system (CNS) associated with aberrations in the endogenous processing of painful stimuli [54]. Accordingly, it has been hypothesized that these aberrations in the CNS processing of pain signals may put individuals at risk for the development or perpetuation of chronic pain [55]. Endogenous pain processing broadly refers to the phenomenon whereby the CNS modulates pain signals by either facilitating or inhibiting them [56]. In a laboratory setting, dysfunction of endogenous inhibition of pain is often assessed in humans using a “pain-inhibition-by-pain” model where pain in a local area (test stimulus) is inhibited by a second pain applied distally to the test stimulus (conditioning stimulus) [57]. The term “conditioned pain modulation” (CPM) has recently been used to refer to this inhibitory phenomenon [57]. Temporal summation (TS) refers to a form of pain facilitation characterized by the perception of increased pain despite constant or even reduced peripheral afferent input, and TS is considered a perceptual manifestation of enhanced central excitability [58]. Dysfunction of pain facilitation can be assessed with TS by administering short-duration repeated painful stimuli of a constant intensity and measuring the consequent increase in pain as an indirect method of evaluating sensitization of the CNS [59].
Although new research has helped to clarify that optimism influences experimental pain sensitivity and reports of chronic pain severity, until recently it was unclear whether optimism might also be related to the endogenous pain processes thought to subserve pain sensitivity and the overall experience of pain. Recent evidence suggests there may be a neuroanatomical basis for a relationship between optimism and endogenous pain processing. For instance, studies examining how pain is processed in the human brain have suggested that a network of subcortical (e.g., amygdala, periaqueductal gray) and cortical structures (e.g., prefrontal cortex, anterior cingulate cortex, insula, somatosensory cortices) appear to be involved [60, 61]. Moreover, additional developments in functional neuroimaging studies have shown that many of the cortical regions thought to be relevant to endogenous pain processing are also implicated in the generation of optimistic expectations [62]. For instance, the experimental induction of an optimism bias has been found to be associated with greater activation of regions in the prefrontal cortex and anterior cingulate, as well as corresponding attenuations in activation of key pain-processing areas such as the insula and secondary somatosensory cortex [63, 64]. Thus, optimism appears to be associated with the engagement of many of the cortical regions involved in the endogenous processing of pain.
A series of studies by Goodin and colleagues set out to examine the relationships between optimism and endogenous pain processing using CPM and TS methodology. In their first study of healthy adults, it was revealed that higher levels of optimism were significantly associated with greater CPM, or an enhanced ability for central pain inhibition [65*]. In a subsequent study of older adults with symptomatic knee osteoarthritis, higher levels of optimism were also found to be significantly related with less TS of heat pain, suggesting attenuated central pain facilitation [66*]. Taken together, these results provide preliminary support for a link between optimism and endogenous pain processing. Furthermore, these findings indirectly support the possibility that the diminished pain sensitivity reported by individuals with greater optimism [41–43] may be related to enhancements in the endogenous inhibition of pain as well as diminished pain facilitation. Whether the relationships among optimism and endogenous pain processes directly translate into less pain sensitivity and less severe reports of chronic pain is a topic in need of further investigation.
Cognitive and behavioral mediators of optimism’s effects on the pain experience
How optimism comes to exert its influence on the experience of pain has received increased empirical attention. Although it could be argued that other factors such as endogenous pain processing mechanisms (e.g., CPM and TS) might mediate the effects of optimism on the experience of pain, this section is limited to discussing cognitive and behavioral mediators because they have thus far received the most direct attention. One important mediator of the optimism and pain relationship that has emerged is pain catastrophizing, which is an exaggerated negative response to actual or anticipated pain [19]. The association between greater optimism and less pain catastrophizing was initially reported in clinical studies as proof that optimism predicts better adjustment to chronic pain [33, 34, 36]. However, the recent laboratory-based study of healthy individuals conducted by Hood and colleagues [42*] expanded upon the current knowledge base by demonstrating that the association between optimism and pain intensity ratings was mediated by pain catastrophizing. More specifically, individuals who demonstrated the greatest levels of optimism tended to engage in less pain catastrophizing in anticipation of a painful stimulus. In turn, less pain catastrophizing predicted less severe pain intensity rating in response to a cold pressor task. The ability of diminished pain catastrophizing to mediate optimism’s beneficial effect on the pain experience has been further confirmed by two subsequent studies involving healthy, young adults [47**] and older adults with chronic knee pain [66*].
In the introduction to this review, it was suggested that persons with a high level of optimism may be more likely to report greater hopefulness and pain acceptance, which is important because both have been shown to be predictive of better chronic pain outcomes [12–17]. In studies that have sought to determine the extent to which optimism and hopefulness represent overlapping constructs, it has been consistently reported that optimism is related to how hopeful individuals are about their future well-being [67, 68]. Hopefulness and optimism appear to be related but not identical constructs, because hopefulness seems more directly related to the personal attainment of specific goals, whereas optimism focuses more broadly on the expected quality of future outcomes in general [68]. Not only does hopefulness relate to less severe pain intensity among persons with chronic health conditions, it also appears to predict less pain sensitivity in laboratory studies of healthy adults [69]. Support for the association between optimism and pain acceptance comes from a study involving patients with rheumatoid arthritis and multiple sclerosis [70]. In this study, optimism was positively related with greater patient acceptance of their respective diseases, and, in turn, greater acceptance was related with less reported pain for the rheumatoid arthritis patients as well as less fatigue for the multiple sclerosis patients. Several additional studies have found that the mechanisms for dealing with stressful events preferred by persons with high levels of optimism are more often acceptance and approach-oriented coping and less often avoidance or denial, when compared to persons with less optimistic outlooks [71–73].
Coping strategies also appear to be related to the influence of optimism on pain experiences. Compared to those with low optimism, individuals with high levels of optimism have been found more likely to engage in approach coping strategies (i.e., planning, seeking support) and less likely to engage in avoidance coping strategies (i.e., denial, isolating oneself) when confronted with threats or challenges [74]. Approach- and avoidance-based coping strategies have been examined in relation to the pain experience, and while not formally demonstrated as a mediator, approach coping strategies have been shown to not only be related to greater optimism but also to less severe reports of pain severity among chronic pain patients [34]. These findings provide indirect support for the hypothesis that the beneficial effects of optimism on pain are due, at least in part, to the use of more approach-based pain coping strategies by those individuals with greater optimism.
Conclusions
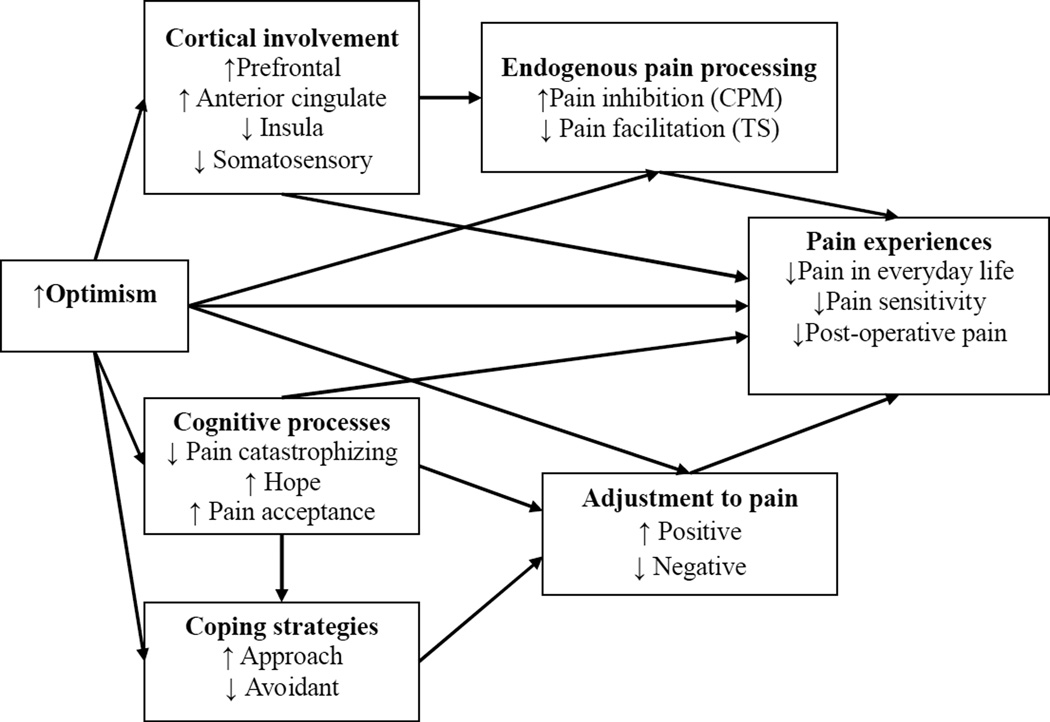
In his review of the optimism and pain literature published in 2000 [18], Garafalo suggested that the scant amount of completed research addressing the beneficial effects of optimism on pain were compelling but too preliminary to make any meaningful generalizations. He concluded by stating that further exploration of optimism’s role as a protective factor in the experience of pain was needed. As can be gleaned from this review of the literature, multiple studies have since examined the relationship between optimism and pain in clinical and laboratory settings, with the predominant finding being that optimism seems to benefit the pain experience and its course of treatment. Figure 1 provides a simplified, working conceptual model describing both direct and indirect pathways by which optimism is likely to contribute to the experience of pain. In the future, individuals who treat and research pain need to pay more attention to the role that positive psychological factors such as optimism play in the pain experience. Determining how the current empirical findings relating optimism to the pain experience can best be translated into improved clinical practice represents an important effort moving forward.
Figure 1.
Conceptual path analytic model of optimism effects on pain experiences and other important pain-related factors. CPM = conditioned pain modulation; TS = temporal summation.
One area for further investigation would be to address whether cognitive-behavioral therapy (CBT) for the psychological treatment of chronic pain could benefit from focusing on optimism. In the past, chronic pain patients provided with a trial of CBT for pain management have shown mixed responses to treatment, with some patients benefiting [75] and others not [76]. Whether differences in patients’ responses to CBT may be accounted for, at least in part, by optimism is unknown. For instance, it might be that patients’ baseline levels of optimism interact with CBT treatments that target their pain, such that patients with high optimism derive more benefit from CBT than patients with low optimism. Such a hypothesis is currently speculative and additional research is needed to address this possibility. Furthermore, it has been suggested that the development and refinement of new clinical interventions that can directly cultivate optimism and other positive resources for coping with pain is a worthy pursuit [77]. Standard CBT for the management of chronic pain often lends most of its emphasis to the targeting of negative cognitions (i.e., catastrophizing) for reduction. Yet there may be instances when simply reducing negative cognitions may not be sufficient. The addition of "optimism training" techniques as a component of CBT may be particularly useful for helping patients by increasing the frequency of positive cognitions and self-statements that foster optimism and motivate adaptive behavior.
It appears that individuals can learn to be more optimistic and clinical researchers have begun to develop optimism training interventions that increase optimism by shifting expectancies for the future from negative to positive [78]. These interventions often include positive future thinking techniques that require envisioning an imaginary future in which everything has turned out in the most optimal way. Writing about and imagining a future where everything has turned out optimally has been shown to increase optimism in terms of expecting favorable outcomes, and this increase in optimism has been found to be independent of changes in positive mood [46]. A common limitation of the previous research evaluating optimism training is that most often only the immediate post-intervention effects of a single session have been studied. Perhaps more encouraging was that optimism has been shown to increase and remained significantly elevated, relative to baseline, in response to a two-week optimism training intervention [45*]. The clinical relevance of optimism training as a component of CBT for the psychological treatment of chronic pain remains unclear and future research is warranted. However, CBT techniques such as guided imagery are regularly used by pain clinicians to help chronic pain patients better manage their stress levels [79, 80]. Thus, it is not unfathomable to consider that pain clinicians might be able to further assist chronic pain patients with their pain experiences by facilitating future thinking techniques that incorporate positive images of an optimal life as a means of increasing optimism.
Acknowledgements
This work was supported by funds provided to Dr. Burel R. Goodin from the University of Alabama at Birmingham, Department of Psychology.
Footnotes
Disclosure
Dr. Burel R. Goodin and Mrs. Hailey W. Bulls report no potential conflicts of interest relevant to this article.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as:
* Of importance
** Of major importance
- 1.Achat H, Kawachi I, Spiro A, et al. Optimism and depression as predictors of physical and mental health functioning: the Normative Aging Study. Ann Behav Med. 2000;22:127–130. doi: 10.1007/BF02895776. [DOI] [PubMed] [Google Scholar]
- 2.de Moor JS, de Moor CA, Basen-Engquist K, et al. Optimism, distress, health-related quality of life, and change in cancer antigen 125 among patients with ovarian cancer undergoing chemotherapy. Psychosom Med. 2006;68:555–562. doi: 10.1097/01.psy.0000222379.71389.91. [DOI] [PubMed] [Google Scholar]
- 3.Steptoe A, Wright C, Kunz-Ebrecht SR, et al. Dispositional optimism and health behaviour in community-dwelling older people: associations with healthy ageing. Br J Health Psychol. 2006;11:71–84. doi: 10.1348/135910705X42850. [DOI] [PubMed] [Google Scholar]
- 4.Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: a meta-analytic review. Ann Behav Med. 2009;37:239–256. doi: 10.1007/s12160-009-9111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4:219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 6.Carver CS, Scheier MF. Attention and self-regulation: a control theory approach to human behavior. New York, NY: Springer; 1981. [Google Scholar]
- 7.Scheier MF, Carver CS. Dispositional optimism and physical well-being: the influence of generalized outcome expectancies on health. J Pers. 1987;55:169–210. doi: 10.1111/j.1467-6494.1987.tb00434.x. [DOI] [PubMed] [Google Scholar]
- 8.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 9. Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev. 2010;30:879–889. doi: 10.1016/j.cpr.2010.01.006. This article is a good, comprehensive review of the beneficial effects of optimism on well-being and health.
- 10.Gatchel RJ, Peng YB, Peters ML, et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psych Bull. 2007;133:581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- 11.Snyder CR, Harris C, Anderson JR, et al. The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol. 1991;60:570–585. doi: 10.1037//0022-3514.60.4.570. [DOI] [PubMed] [Google Scholar]
- 12.Peleg G, Barak O, Harel Y, et al. Hope, dispositional optimism and severity of depression following traumatic brain injury. Brain Inj. 2009;23:800–808. doi: 10.1080/02699050903196696. [DOI] [PubMed] [Google Scholar]
- 13.Scioli A, MacNeil S, Partridge V, et al. Hope, HIV and health: a prospective study. AIDS Care. 2012;24:149–156. doi: 10.1080/09540121.2011.597943. [DOI] [PubMed] [Google Scholar]
- 14.Berendes D, Keefe FJ, Somers TJ et al. Hope in the context of lung cancer: relationships of hope to symptoms, psychological distress, and relationship quality. J Pain Symptom Manage. 2010;40:174–182. doi: 10.1016/j.jpainsymman.2010.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCracken LM. Learning to live with the pain: acceptance of pain predicts adjustment in persons with chronic pain. Pain. 1998;74:21–27. doi: 10.1016/S0304-3959(97)00146-2. [DOI] [PubMed] [Google Scholar]
- 16.McCracken LM, Eccleston C. A prospective study of acceptance of pain and patient functioning with chronic pain. Pain. 2005;118:164–169. doi: 10.1016/j.pain.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 17.McCracken LM, Vowles KE. A prospective analysis of acceptance of pain and values-based action in patients with chronic pain. Health Psychol. 2008;27:215–220. doi: 10.1037/0278-6133.27.2.215. [DOI] [PubMed] [Google Scholar]
- 18.Garofalo JP. Perceived optimism and chronic pain. In: Gatchel RJ, Weisberg JN, editors. Personality characteristics of patients with pain. Washington, DC: American Psychological Association; 2000. pp. 203–217. [Google Scholar]
- 19.Sullivan MJL, Thorn B, Haythornthwaite JA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Bair MJ, Robinson RL, Katon W, et al. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 21.Goubert L, Crombez G, Van Damme S. The role of neuroticism, pain catastrophizing, and pain-related fear in vigilance to pain: a structural equations approach. Pain. 2004;107:234–241. doi: 10.1016/j.pain.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 22.Haerkaepaeae K, Jarvikoski A, Estlander A-M. Health optimism and controls beliefs as predictors for treatment outcome of a multimodal back treatment program. Psychol Health. 1996;12:123–134. [Google Scholar]
- 23.Novy DM, Nelson DV, Hetzel RD, et al. Coping with chronic pain: sources of intrinsic and contextual variability. J Behav Med. 1998;21:19–34. doi: 10.1023/a:1018711420797. [DOI] [PubMed] [Google Scholar]
- 24.Kurtz ME, Kurtz JC, Given CW, et al. Patient optimism and mastery – do they play a role in cancer patients’ management of pain and fatigue? J Pain Symptom Manage. 2008;36:1–10. doi: 10.1016/j.jpainsymman.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 25.Wong WS, Fielding R. Quality of life and pain in Chinese lung cancer patients: is optimism a moderator or mediator? Qual Life Res. 2007;16:53–63. doi: 10.1007/s11136-006-9106-z. [DOI] [PubMed] [Google Scholar]
- 26.Allison PJ, Guichard C, Gilain L. A prospective investigation of dispositional optimism as a predictor of health-related quality of life in head and neck cancer patients. Qual Life Res. 2000;9:951–960. doi: 10.1023/a:1008931906253. [DOI] [PubMed] [Google Scholar]
- 27.Ferreira VM, Sherman AM. The relationship of optimism, pain and social support to well-being in older adults with osteoarthritis. Aging Ment Health. 2007;11:89–98. doi: 10.1080/13607860600736166. [DOI] [PubMed] [Google Scholar]
- 28.Treharne GJ, Kitas GD, Lyons AC, et al. Well-being in rheumatoid arthritis: the effects of disease duration and psychosocial factors. J Health Psychol. 2005;10:457–474. doi: 10.1177/1359105305051416. [DOI] [PubMed] [Google Scholar]
- 29.Sipila K, Ylostalo PV, Ek E, et al. Association between optimism and self-reported facial pain. Acta Odontol Scand. 2006;64:177–182. doi: 10.1080/00016350500514816. [DOI] [PubMed] [Google Scholar]
- 30.Pence L, Valrie CR, Gil KM, et al. Optimism predicting daily pain medication use in adolescents with sickle cell disease. J Pain Symptom Manage. 2007;33:302–309. doi: 10.1016/j.jpainsymman.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 31.Affleck G, Tennen H, Apter A. Optimism, pessimism, and daily life with chronic illness. In: Chang EC, editor. Optimism & pessimism: implications for theory, research, and practice. Washington DC: American Psychological Association; 2001. pp. 147–168. [Google Scholar]
- 32.Benyamini Y. Can high optimism and high pessimism co-exist? Findings from arthritis patients coping with pain. Pers Individ Diff. 2005;38:1463–1473. [Google Scholar]
- 33.Wright MA, Wren AA, Somers TJ, et al. Pain acceptance, hope, and optimism: relationships to pain adjustment in patients with chronic musculoskeletal pain. J Pain. 2011;12:1155–1162. doi: 10.1016/j.jpain.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 34.Ramirez-Maestre C, Esteve R, Lopez AE. The role of optimism and pessimism in chronic pain patients’ adjustment. Span J Psychol. 2012;15:286–294. doi: 10.5209/rev_sjop.2012.v15.n1.37335. [DOI] [PubMed] [Google Scholar]
- 35.Tennen H, Affleck G, Urrows S, et al. Perceiving control, construing benefits, and daily processes in rheumatoid arthritis. Can J Behav Sci. 1992;24:186–203. [Google Scholar]
- 36.Sinclair VG. Predictors of pain catastrophizing in women with rheumatoid arthritis. Arch Psychiatr Nurs. 2001;15:279–288. doi: 10.1053/apnu.2001.28686. [DOI] [PubMed] [Google Scholar]
- 37.Mahler HIM, Kulik JA. Optimism, pessimism and recovery from coronary bypass surgery: prediction of affect, pain and functional status. Psychol Health Med. 2000;5:347–358. [Google Scholar]
- 38.Peters ML, Sommer M, de Rijke JM, et al. Somatic and psychological predictors of long-term unfavorable outcome after surgical intervention. Ann Surg. 2007;245:487–494. doi: 10.1097/01.sla.0000245495.79781.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenberger PH, Kerns R, Jokl P, et al. Mood and attitude predict pain outcomes following arthroscopic knee surgery. Ann Behav Med. 2009;37:70–76. doi: 10.1007/s12160-008-9078-z. [DOI] [PubMed] [Google Scholar]
- 40.Hansson P, Backonja M, Bouhassira D. Usefulness and limitations of quantitative sensory testing: clinical and research applications in neuropathic pain states. Pain. 2007;129:256–259. doi: 10.1016/j.pain.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 41.Geers AL, Wellman JA, Helfer SG, et al. Dispositional optimism and thoughts of well-being determine sensitivity to an experimental pain task. Ann Behav Med. 2008;36:304–313. doi: 10.1007/s12160-008-9073-4. [DOI] [PubMed] [Google Scholar]
- 42. Hood A, Pulvers K, Carillo J, et al. Positive traits linked to less pain through lower pain catastrophizing. Pers Individ Dif. 2012;52:401–405. doi: 10.1016/j.paid.2011.10.040. This study is one of the first to experimentally demonstrate that the association of greater optimism with less severe ratings of pain intensity is mediated by lower pain catastrophizing.
- 43.Costello NL, Bragdon EE, Light KC, et al. Temporomandibular disorder and optimism: relationships to ischemic pain sensitivity and interleukin-6. Pain. 2002;100:99–110. doi: 10.1016/s0304-3959(02)00263-4. [DOI] [PubMed] [Google Scholar]
- 44.Smith BW, Tooley EM, Montague EQ, et al. The role of resilience and purpose in life in habituation to heat and cold pain. J Pain. 2009;10:493–500. doi: 10.1016/j.jpain.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 45. Meevissen YMC, Peters ML, Alberts HJEM. Become more optimistic by imagining a best possible self: effects of atwo week intervention. J Behav Ther Exp Psychiatry. 2011;42:371–378. doi: 10.1016/j.jbtep.2011.02.012. This study is important because it demonstrated that a two-week intervention designed to enhance optimism was effective for sustaining a significant increase in optimism from baseline independent of the mood effect.
- 46.Peters ML, Flink IK, Boersma K, et al. Manipulating optimism: can imagining a best possible self to be used to increase positive future expectancies? J Posit Psychol. 2010;5:204–211. [Google Scholar]
- 47. Hanssen MM, Peters ML, Vlaeyen JWS, et al. Optimism lowers pain: evidence of the causal status and underlying mechanisms. Pain. 2012 doi: 10.1016/j.pain.2012.08.006. In press. The study is important because it is the first to experimentally manipulate optimism and provide causal evidence of the ability for optimism to diminish the experience of pain.
- 48.Oken BS. Placebo effects: clinical aspects and neurobiology. Brain. 2008;131:2812–2823. doi: 10.1093/brain/awn116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Price DD, Fillingim RB, Robinson ME. Placebo analgesia: friend or foe? Curr Rheumatol Rep. 2006;8:418–424. doi: 10.1007/s11926-006-0035-1. [DOI] [PubMed] [Google Scholar]
- 50.Puhl AA, Reinhart CJ, Rok ER, et al. An examination of the observed placebo effect associated with the treatment of low back pain – a systematic review. Pain Res Manag. 2011;16:45–52. doi: 10.1155/2011/625315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Scott DJ, Stohler CS, Egnatuk CM, et al. Individual differences in reward responding explain placebo-induced expectations and effects. Neuron. 2007;19:325–336. doi: 10.1016/j.neuron.2007.06.028. [DOI] [PubMed] [Google Scholar]
- 52. Geers AL, Wellman JA, Fowler SL, et al. Dispositional optimism predicts placebo analgesia. J Pain. 2010;11:1165–1171. doi: 10.1016/j.jpain.2010.02.014. This laboratory-based study revealed that optimism significantly predicted placebo analgesia, such that optimism was related to less cold pressor pain in a placebo condition as compared to a control condition.
- 53.Morton DL, Watson A, El-Deredy W, et al. Reproducibility of placebo analgesia: effect of dispositional optimism. Pain. 2009;146:194–198. doi: 10.1016/j.pain.2009.07.026. [DOI] [PubMed] [Google Scholar]
- 54.Siddall PJ, Cousins MJ. Persistent pain as a disease entity: implications for clinical management. Anesth Analg. 2004;99:510–520. doi: 10.1213/01.ANE.0000133383.17666.3A. [DOI] [PubMed] [Google Scholar]
- 55.Edwards RR. Individual differences in endogenous pain modulation as a risk factor for chronic pain. Neurology. 2005;65:437–443. doi: 10.1212/01.wnl.0000171862.17301.84. [DOI] [PubMed] [Google Scholar]
- 56.Ossipov MH, Dussor GO, Porreca F. Central pain modulation. J Clin Invest. 2010;120:3779–3787. doi: 10.1172/JCI43766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yarnitsky D. Conditioned pain modulation (the diffuse noxious inhibitory control-like effect): its relevance for acute and chronic pain states. Curr Opin Anaesthesiol. 2010;23:611–615. doi: 10.1097/ACO.0b013e32833c348b. [DOI] [PubMed] [Google Scholar]
- 58.Eide PK. Wind-up and the NMDA receptor complex from a clinical perspective. Eur J Pain. 2000;4:5–17. doi: 10.1053/eujp.1999.0154. [DOI] [PubMed] [Google Scholar]
- 59.Staud R, Vierck CJ, Cannon RL, Mauderli AP, Price DD. Abnormal sensitization and temporal summation of second pain (wind-up) in patients with fibromyalgia syndrome. Pain. 2001;91:165–175. doi: 10.1016/s0304-3959(00)00432-2. [DOI] [PubMed] [Google Scholar]
- 60.Piche M, Arsenault M, Rainville P. Cerebral and cerebrospinal processes underlying counterirritation analgesia. J Neurosci. 2009;29:14236–14246. doi: 10.1523/JNEUROSCI.2341-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wilder-Smith CH, Schindler D, Lovblad K, Redmond SM, Nirkko A. Brain functional magnetic resonance imaging of rectal pain and activation of endogenous inhibitory mechanisms in irritable bowel syndrome patient subgroups and healthy controls. Gut. 2004;53:1595–1601. doi: 10.1136/gut.2003.028514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sharot T, Riccardi AM, Raio CM, et al. Neural mechanisms mediating optimism bias. Nature. 2007;450:102–105. doi: 10.1038/nature06280. [DOI] [PubMed] [Google Scholar]
- 63.Wiech K, Kalisch R, Weiskopf N, et al. Anterolateral prefrontal cortex mediates the analgesic effect of expected and perceived control over pain. J Neurosci. 2006;26:11501–11509. doi: 10.1523/JNEUROSCI.2568-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wiech K, Ploner M, Tracey I. Neurocognitive aspects of pain perception. Trends Cogn Neurosci. 2008;12:306–313. doi: 10.1016/j.tics.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 65. Goodin BR, Kronfli T, King CD, et al. Testing the relation between dispositional optimism and conditioned pain modulation: does ethnicity matter? J Behav Med. 2012 doi: 10.1007/s10865-012-9411-7. In press. This study of healthy volunteers demonstrated that optimism was significantly related to enhanced endogenous pain-inhibitory processes, and that the strength of this relationship was consistent across different ethnic/racial backgrounds.
- 66. Goodin BR, Glover TL, Sotolongo A, et al. The association of greater dispositional optimism with less endogenous pain facilitation is indirectly transmitted through lower levels of pain catastrophizing. J Pain. 2012 doi: 10.1016/j.jpain.2012.10.007. In press. In a clinical sample of older adults with knee osteoarthritis, results of this study showed that optimism predicted diminished temporal summation of heat pain, a purported proxy of central sensitization.
- 67.Magletta PR, Oliver JR. The hope construct, will, and ways: their relations with self-efficacy, optimism, and general well-being. J Clin Psychol. 1999;55:539–551. doi: 10.1002/(sici)1097-4679(199905)55:5<539::aid-jclp2>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 68.Bryant FB, Cvengros JA. Distinguishing hope and optimism: two sides of a coin, or two separate coins? J Soc Clin Psychol. 2004;23:273–302. [Google Scholar]
- 69.Snyder CR, Berg C, Woodward JT, et al. Hope against the cold: individual differences in trait hope and acute pain tolerance on the cold pressor task. J Pers. 2005;73:287–312. doi: 10.1111/j.1467-6494.2005.00318.x. [DOI] [PubMed] [Google Scholar]
- 70.Evers AWM, Kraaimaat FW, van Lankveld W, et al. Beyond unfavorable thinking: the illness cognition questionnaire for chronic diseases. J Consult Clin Psychol. 2001;69:1026–1036. [PubMed] [Google Scholar]
- 71.Edgar L, Remmer J, Rosberger Z, et al. Resource use in women completing treatment for breast cancer. Psychooncology. 2000;9(5):428–438. doi: 10.1002/1099-1611(200009/10)9:5<428::aid-pon481>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 72.King KB, Kimble MA, Zerwic JJ. Coping and long-term recovery from coronary bypass in women. Res Nurs Health. 1998;21:15–26. doi: 10.1002/(sici)1098-240x(199802)21:1<15::aid-nur3>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 73.Epping-Jordan JE, Compas BE, Osowiecki DM, et al. Psychological adjustment in breast cancer: processes of emotional distress. Health Psychol. 1999;18:315–326. doi: 10.1037//0278-6133.18.4.315. [DOI] [PubMed] [Google Scholar]
- 74.Solberg Nes L, Segerstrom SC. Dispositional optimism and coping: a meta-analytical review. Pers Soc Psychol Rev. 2006;10:235–251. doi: 10.1207/s15327957pspr1003_3. [DOI] [PubMed] [Google Scholar]
- 75.Litt MD, Shafer DM, Ibanez CR, et al. Momentary pain and coping in temporomandibular disorder pain: exploring mechanisms of cognitive behavioral treatment for chronic pain. Pain. 2009;145:160–168. doi: 10.1016/j.pain.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Turner JA, Clancy S. Comparison of operant behavioral and cognitive-behavioral group treatment for chronic low back pain. J Consult Clin Psychol. 1988;56:262–266. doi: 10.1037//0022-006x.56.2.261. [DOI] [PubMed] [Google Scholar]
- 77.Keefe FJ, Wren AA. Optimism and pain: a positive move forward. Pain. 2013;154:7–8. doi: 10.1016/j.pain.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fosnaugh J, Geers AL, Wellman JA. Giving off a rosy glow: the manipulation of an optimistic orientation. J Soc Psychol. 2009;149:249–263. doi: 10.3200/SOCP.149.3.349-364. [DOI] [PubMed] [Google Scholar]
- 79.Lewandowski W, Good M, Draucker CB. Changes in the meaning of pain with the use of guided imagery. Pain Manage Nurs. 2005;6:58–67. doi: 10.1016/j.pmn.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 80.Baird CL, Sands LP. Effect of guided imagery with relaxation on health-related quality of life in older women with osteoarthritis. Research in Nursing and Health. 2006;29:442–451. doi: 10.1002/nur.20159. [DOI] [PubMed] [Google Scholar]