Abstract
Purpose
ADVANCE® Medial Pivot (MP) (Wright Medical) total knee arthroplasty (TKA) was established to replicate normal tibio-femoral knee joint kinematics, however, its influence on the patello-femoral (PF) joint is unclear. The purpose in this study was to assess the PF joint conditions in Advance MP TKA, via radiography and three-dimensional image-matching software.
Methods
Ten subjects with osteoarthritis were treated with the ADVANCE MP TKA. Pre-operatively and one month after surgery, skyline views at 30, 60, and 90° of flexion were taken, and patella shift and tilt were measured. With 2D–3D registration techniques using software, implant orientations were matched with the pre-operative CT and changes in the anterior part of the femoral prosthesis, condylar twist angle (CTA) for femoral rotation, and tibial rotation were evaluated. The relationships between morphological and rotational changes were evaluated.
Results
There were significant differences in patella tilt at 60° and patella shift at all angles between pre- and post-operation (p < 0.05). No correlation was found between morphological changes in the anterior femur with patella tilt and shift. A positive correlation between postoperative CTA and patella shift at 90° was found (p < 0.05); however, no correlation was found between rotational alignment of the tibial component and patella tilt and shift.
Conclusions
ADVANCE MP TKA changed patello-femoral joint kinematics, compared to that found before surgery. The kinematic features were mainly due to the design concepts for tibio-femoral joint motion, indicating the difficulty to reproduce normal patello-femoral joint kinematics after TKA.
Keywords: Patello-femoral joint kinematics following TKR, ADVANCE MP® prosthesis, Patella tilt
Introduction
Nowadays, total knee arthroplasty (TKA) is a commonly performed operation for severe osteoarthritis and other conditions of cartilage degeneration. Total knee arthroplasty is a well-established procedure, however, as the number of TKAs performed has increased, the number of complications has also increased. Above all, complications related to the patellofemoral (PF) joint such as pain, maltracking, subluxation and patella fractures have been reported [1–3]. These complications can necessitate revision TKA [4, 5] and therefore, many researchers have conducted investigations of radiographic and clinical results in the PF joint [6–8]. Despite this interest, patello-femoral joint conditions and kinematics remain less well understood than the tibio-femoral joint. In addition, conditions and kinematics can vary depending on prosthesis design [9, 10]. Among several types of prosthesis, ADVANCE Medial-pivot (MP) TKA (Wright Medical Technology, Arlington, TN) has a unique design concept compared to cruciate retaining (CR), and posterior stabilised (PS) prostheses in that it aims to replicate the medial pivoting behaviour observed in normal knees and has been found to exhibit excellent anterior-posterior (AP) stability. Several studies have revealed in vitro and in vivo tibio-femoral kinematics of this prosthesis and reported its favourable performance for patients; however, details about the performance of the PF joint remain unknown at present [11–13].
Meanwhile, surgeons have tried to audit and improve their own surgery to improve patients’ subjective feeling and objective function. However, there are few available tools for assessing surgery in TKA. Usually, surgeons evaluate their TKA by using several methods including measurement of the amount of osteotomised bone, using X-ray and CT. However, it is generally difficult to compare the postoperative prosthesis orientation directly with conditions before operation. Some X-ray modifications have been made which reveal more detailed results [6, 14]; however the problem of assessing the postoperative knee three-dimensionally and comparing the postoperative conditions remains, especially in the PF joint. One innovative new tool is an automated image-matching technique using a computer-aided design (CAD) program which aims to assess alignment of the entire lower extremity for normal and implanted knees and the positioning of implants with respect to bone [15]. Three-dimensional digital templating software, “ATHENA KNEE” (SoftCube Co., Ltd., Osaka, Japan) was advanced as pre-operative template software for pre-operative surgical preparation. By using the software, the amount of osteotomised bone can be estimated and imaged and the appropriate size of prosthesis selected. Recently, application of this pre-operative template software has been tried as a postoperative surgery assessment tool in TKA patients. By matching the pre-operative 3D-reconstructed patient’s knee model with postoperative X-ray and CAD data of the prosthesis, we can easily visualise the current status of the implanted knee, the size of the osteotomised bone, and the rotational profile of the prosthesis. A recent paper has found that the evaluated osteotomised bone values are within 1.0 mm difference compared to the actual intra-operative measured bone value [16]. This suggests the potential of this software for orthopaedic surgeons as an easy and useful tool for TKA assessment.
In this study, the aim was to evaluate and compare the radiographic PF joint of ADVANCE TKA with the pre-operative condition. Furthermore, we used the software “ATHENA KNEE” for postoperative assessment to investigate the rotational profile and the morphological change of the PF joint, which helps interpret the correlation with the prosthesis orientation.
Materials and methods
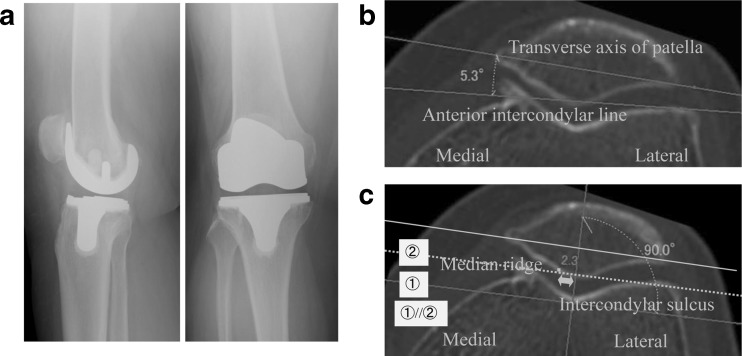
The study was approved by the institutional review board, and informed consent was obtained from all patients. From May to November 2010, ten ADVANCE MP TKA were performed in varus deformity patients diagnosed with osteoarthritis (Fig. 1a). Patients with valgus deformity, severe bony defects which required bone graft or augmentation instruments, and rheumatoid arthritis were excluded from this study. Patients included one man and nine women, with an average of 74.2 ± 5.2 years (range 66–80). There were five right and five left knees. The TKA was implanted by the same experienced surgeon (K.I.) using the conventional manual technique outlined below. Briefly, under tourniquet control, knees were exposed through a medial parapatellar arthrotomy and bony resection was performed using the measured resection technique. The posterior cruciate ligament (PCL) was sacrificed at the beginning of the procedure. An extramedullary guiding rod was used for the tibia, and an intramedullary guiding rod was used for femoral bone resection. The femoral component size was determined from posterior referencing and the rotational alignment of the femoral prosthesis was determined using an axial radiograph of the femur as reported by Kanekasu et al. [14]. The objectives whose femoral component was aligned at 3° of external rotation in relation to the posterior condylar axis were included. The femoral distal resection was performed at 5–7° of valgus alignment, according to each coronal femoral mechanical axis. When mediolateral overhang existed, we opted to use one smaller size of femoral prosthesis to adjust for the patient’s mediolateral diameter, then sometimes moved the cutting guide two millimetres anteriorly so as to avoid the anterior notch. Therefore, we allowed 2two millimetres over osteotomy of the femoral posterior condyle. The rotational alignment of the tibial component was referenced by the medial one-third of the tibial tubercle. The proximal tibial osteotomy was performed perpendicular to the long axis in the coronal plane with a 3° posterior slope in the sagittal plane. The tibial bony cut was made ten millimetres below the highest point of the articular cartilage on the lateral tibial plateau. No lateral retinacular release was performed and all patellae were unresurfaced and the surrounding osteophyte removed. All TKA were deemed clinically successful without any ligamentous laxity, postoperative surgical stiffness, or pain at one-year post-operation.
Fig. 1.
ADVANCE® Medial-pivot total knee arthroplasty, definition of patella tilt, and patella shift. (a) Post-operative radiographs after ADVANCE® Medial-pivot total knee arthroplasty. (b) The patella tilt is the angle between the anterior intercondylar line and the transverse axis of the patella. (c) Patella shift is the lateral displacement of the median ridge of the patella from the intercondylar sulcus of the femur
Radiological measurements
Before and one month after the operation, axial radiographs of the knee (a 320 mA, 0.03 s exposure at 80–100 kV, depending on soft-tissue thickness) were taken at 30, 60, and 90° knee flexion in each patient. Radiographic evaluations were performed according to previously reported methods [17]. Briefly, patella tilt was determined by the angles between the anterior intercondylar line and the transverse axis of the patella [17, 18] (Fig. 1b). The transverse axis of the patella is the line connecting the medial and lateral corners, a method which is independent of patella morphology, and probably corresponds more closely to clinical evaluation of tilt [17]. The medial and lateral corners of the patella were determined by referencing the radiographic articular surface, which represents the subchondral bone of each facet of the patella. Patella tilt was defined as positive when the transverse axis of the patella was tilted laterally with reference to the anterior intercondylar line.
Meanwhile, patella shift was determined by the distances between the intercondylar sulcus and the median ridge of the patella [17] (Fig. 1c). The intercondylar sulcus was defined as the deepest point of the femoral trochlea, which was determined on the radiograph as the lowest point of the trochlea in relation to the anterior intercondylar line. The intercondylar sulcus was determined by moving the digitally drawn anterior intercondylar line posteriorly until it touched the lowest point of the intercondylar area to reduce inter-observer variability [17]. The median ridge of the patella was also defined as the deepest point of the patella in relation to the transverse axis of the patella. The transverse axis of the patella was moved inferiorly by touching the most inferior part of the patella, at the point defined as the median ridge of the patella. When the median ridge of the patella was located lateral to the intercondylar sulcus, we defined patella shift as positive, and if the point was located medial to the sulcus, we defined it as negative [17]. In the postoperative evaluation, patella tilt and shift were measured the same way as the pre-operative radiographs, except that the prosthetic anterior intercondylar line and intercondylar sulcus were used.
The measurements were performed at least three times in each patient by two independent authors blinded to clinical information using commercially available imaging software systems (SYNAPSE; FUJIFILM, Tokyo, Japan) and the averages were used in this study.
Postoperative evaluations using three-dimensional digital template software
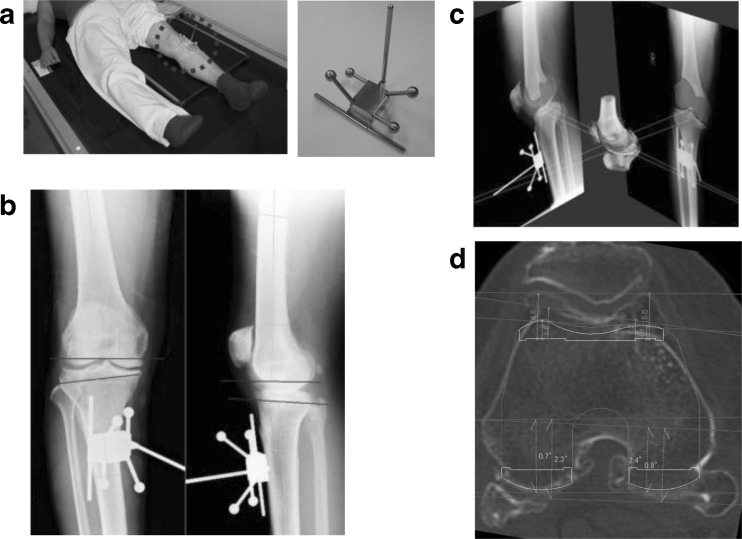
First, two X-ray images (antero-posterior and lateral views) of the knee joint were undertaken with a 3D marker attached to the surface of the patient’s lower leg (Fig. 2a) at one-month postoperatively. The silhouette of the 3D marker in the images was used to couple the two X-ray images three dimensionally using software “ATHENA KNEE” (Fig. 2b, c). Next, implanted components were matched to the images using a CAD program. In addition, images of computed tomography (CT; SOMATOM Emotion 6; Siemens thickness; 2.5 mm, energy; 10 kV, intensity; 20 mA) undertaken pre-operatively were matched to the coupled radiographic images. This matching with pre-operative CT data makes the determination of the rotation and position in the axial plane more precise, resolves the problem of artifacts made by the prosthesis in post-implanted CT, and enables accurate measurement of the thicknesses of the cut bone (Fig. 2d). Thereafter, we measured the angle between the clinical epicondylar axis (a line that connects the medial and lateral epicondylar prominences) and the posterior condylar axis (a line that connects the posterior margins of the medial and lateral femoral condyles, or components) and defined the angle as the condylar twist angle (CTA) in ATHENA. In addition, we measured the angle between the anteroposterior axis of the tibia and the tibial component; the anteroposterior axis of the tibia was determined according to Akagi et al. [19] as the line connecting the middle of PCL attachment to the medial border of the patellar tendon attachment. Furthermore, we evaluated the morphological changes of the anterior femur by selecting the most anterior-prominent part of the femur, and then measuring the thickness of the cut bone and thickness of the implant at this portion in each condyle.
Fig. 2.
Three-dimensional digital template software “ATHENA”. Two X-ray images of the knee joint undertaken with a 3D marker attached to the surface of the patient’s lower leg (a, b). The silhouette made by the marker on the images is used to couple the two X-ray images three dimensionally (c). Pre-operative CT was further matched, thus making it possible to assess postoperative conditions in pre-operative three-dimensional digital template software “ATHENA” (d). The changes in the anterior part of the femoral prosthesis and CTA were evaluated
Statistical analysis
Results were analysed statistically using a statistical software package (Stat Mate III; ATMS Co.,Ltd., Tokyo, Japan). Comparison between pre- and postoperative measurements was analysed using the paired Student t test. Correlations between the postoperative parameters (CTA, tibial rotation, and anterior femoral bony cut) and patella tilt and shift were analysed using linear regression. Differences of P < .0.05 were considered statistically significant.
Results
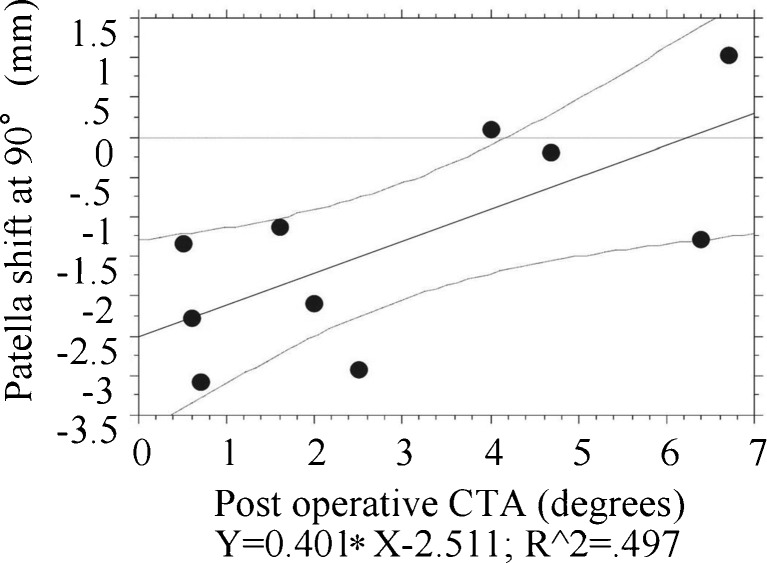
Pre- and postoperative patellar tilt at 30, 60, and 90° of flexion are shown in Table 1. Pre- and postoperative patellar shift are shown in Table 2. Patella tilt at 60° post-operation was significantly larger than pre-operation (p < 0.05). Meanwhile, patella shift was improved significantly at each angle after operation (p < 0.05). Pre- and postoperative CTA, and postoperative rotational profiles of tibial components measured using ATHENA are shown in Table 3. When the correlation between the patellar tilt and CTA was examined, a positive correlation was found between postoperative CTA and patella shift at 90° (Fig. 3; p < 0.05). Meanwhile, there was no significant correlation between patella tilt and CTA. In addition, the rotational profiles of the tibial component were not related to either patella shift or tilt. The anteromedial, and anterolateral differences measured by ATHENA KNEE between pre- and post-operation in the distal femur were 0.5 mm ± 3.5 and −2.1 ± 2.1, respectively (plus means prominence compared to pre operative condition). The anterior part of the femur changed to external rotation after operation. There was no significant correlation between the differences in distal femur and patella tilt and shift.
Table 1.
Comparison of patella tilt between pre- and post-operation (degrees)
| Measurement timing | Flexion (degrees) | ||
|---|---|---|---|
| 30 | 60 | 90 | |
| Pre-operation | 8.5 ± 4.6 | 6.1 ± 3.7* | 5.2 ± 3.0 |
| Post-operation | 10.6 ± 2.5 | 9.1 ± 2.8* | 6.2 ± 2.9 |
Values are expressed as mean ± SD
*P < 0.05
Table 2.
Comparison of patella shift between pre- and post-operation (degrees)
| Measurement timing | Flexion (degrees) | ||
|---|---|---|---|
| 30 | 60 | 90 | |
| Pre-operation | 1.9 ± 2.6* | 0.4 ± 1.9* | −0.4.5 ± 1.3* |
| Post-operation | −0.02 ± 3.7* | −1.1 ± 1.7* | −1.2 ± 1.5* |
Values are expressed as mean ± SD
*P < 0.05
Table 3.
Rotational profiles of components after operation (degrees)
| Measurement timing | Value |
|---|---|
| Pre-operative CTA | 6.0 ± 2.2 |
| Femoral component CTA | 3.0 ± 2.8 |
| Tibial component | −0.3 ± 3.5 |
Values are expressed as mean ± SD. Positive values mean internal rotation, and negative values mean external rotation
CTA condylar twist angle
Fig. 3.
Examination of the correlation between patellar tilt and condylar twist angle (CTA). Positive correlation between postoperative CTA and patella shift at 90°
Discussion
This study is important for revealing the features of the patellofemoral joint in ADVANCE MP TKA. Additionally, we applied new three-dimensional digital template software to assess the orientation of the femoral prosthesis postoperatively, which is a relatively new method.
There are some limitations in this study. First, evaluations were performed in the early postoperative period. The timing of the evaluation may change with those of surrounding tissues. As far as we know, there have been no reports investigating the influence of time after operation to kinematics, so the true influence is unknown. However, the importance of medial ligamentous structures, especially the medial patellofemoral ligament, for patella tracking is well known [20, 21]. Although postoperative muscle weakness is a well aired topic, the influence of muscle strength on PF joint kinematics is controversial [21–24]. We considered that the influence of vastus medialis weakness on PF kinematics in TKA patients is relatively low, compared to a normal knee, because the kinematics were strongly influenced by the design of the prosthesis or its tibio-femoral motion kinematics [25, 26]. Nevertheless, an understanding of the influence of the healing tissues on the kinematics is important when comparing it to the pre-operative condition. Second, several important factors affecting the patello-femoral joint have been reported [27, 28], and the influences of such factors could not be identified by this study. Our study did not find any effect of the rotational profiles of tibial component on patella tilt and shift. Because there was one surgeon and consistent surgical methods, the influence of varying such factors should be negligible in this study.
Generally, direct comparison of the postoperative prosthesis orientation with the conditions before operation is difficult. Although X-ray, CT and MRI as methods of evaluation have been assessed in many reports [29–31], there are some weaknesses in these methods. Although a 2D–3D registration technique, combined with fluoroscopic analysis, has been used to assess postoperative tibio-femoral joint kinematics with high accuracy [32], limitations remain for assessing the PF joint [33]. In addition, the huge device required for these methods is hard to use in daily clinical practice. Therefore, compared to other evaluation tools, there could be many advantages in using pre-operative templating software. First, the software can visualise 3D postoperative conditions and it is possible to measure the differences between pre-operative and postoperative conditions. By combining results with various X-rays, we can estimate both dynamic conditions and the PF joint, which is usually difficult to assess. Second, there is no need for postoperative CT, thus avoiding artifacts, and excessive radiation exposure to patients. Finally, this program system does not require special devices, apart from a 3D marker, which can reduce the medical cost and be widely spread for clinical use. Thus the pre-operative templating software used in this study could be convenient, persuasive, and useful for most orthopaedic surgeons to evaluate their own surgery in daily use. Hence, it is suggested that the three-dimensional digital template software is a useful tool for postoperative evaluation.
The results found that patella shift was improved after surgery, however, patella tilt at 60° postoperatively was significantly larger than pre-operatively. Generally, TKA causes the patella to tilt laterally between 20 and 30° of flexion [34]. In addition, isolated changes in trochlear groove alignment produced patellar shear forces [9], and Barink et al. reported that even asymmetrical patella groove TKA could not improve patella tracking [34]. In this study, the anterior part of the femur component including the sulcus, measured by the software, changed to external rotation after operation. The result was probably a consequence of the TKA thus supporting the hypothesis of Barink et al.
Another important reason could be considered from the viewpoint of femoro-tibial kinematics and joint gap theory [30, 35, 36]. Komistek et al. pointed out that femoro-tibial kinematics can play a major role in patellofemoral kinematics [37]. Theoretically, ADVANCE MP TKA induces a medial pivot motion and does not allow posterior rollback as in the post and cam mechanism. However, Miyazaki et al. reported that the lateral condyle showed anterior movement in the early stage, changing thereafter to posterior movement, in contrast to the fixed medial condyle in ADVANCE TKA [12]. The report suggested that this prosthesis had a relatively low medial pivot motion at lower flexion angle. It is supposed that this motion pattern could possibly act to increase the patellofemoral contact pressure in the early stage. Moreover, the design concept of ADVANCE MP TKA might be disadvantageous for posterior roll-back, which reduces patellofemoral pressure and has superior patellofemoral kinematics for prosthetic knees [38]. Meanwhile, the joint gap with reduced PF joint increased with knee flexion and reached its peak at 60° of flexion in PS TKA [39]. Their report implies that the most relaxed joint condition was at 60° of flexion and the lever arm of the patella that forced the femur posteriorly was relatively difficult to transmit to the joint in the PCL sacrificed position.
In this study, patella shift at 90° was positively correlated with postoperative CTA. Merican et al. have suggested that with external rotation of the femoral component, the tibia rotated into adduction in flexion leading to a decrease of the Q-angle and external rotation leading to an increase of the Q-angle is unfavourable for patella tracking in extension [40]. Their paper concluded that femoral rotation alone might not restore all aspects of patellar kinematics both at extension and flexion [40]. The results of our study supported their suggestion. This may be also because, as Kainz [41] suggested, the patella sits deeply in the trochlear groove, and its kinematics are predominantly controlled by the geometry of the groove in deep flexion.
It is considered that our results showing the increment of patella tilt after ADVANCE MP prosthesis is not so unfavorable for patients. Many previous reports have already stated that symptomatic PF joint is independent of lateral patellar tilt [42, 43]. Indeed, the patients followed up in this study are clinically asymptomatic, and doing well. It could not be concluded whether the features of the PF joint hold clinically important implications in this study.
Conclusion
In summary, this study showed for the first time radiographic patellofemoral joint kinematics in ADVANCE MP TKA. The results in this study indicated that ADVANCE MP TKA changed patellofemoral joint kinematics, compared to that of before surgery. The kinematic features were mainly due to the design concepts for tibiofemoral joint motion, rather than on rotation of the femoral prosthesis, or design of the femoral trochlea, suggesting the difficulty to improve patellofemoral joint congruity after TKA. The results also found that pre-operative templating software was an easy and useful tool for assessing the postoperative prosthesis condition.
Acknowledgement
We thank Ms. Janina Tubby for English rewriting.
Conflict of interest statement
We, all authors, did not receive any financial and personal relationships with other people or organisations that could inappropriately influence (bias) our work.
Footnotes
The first two authors, Nobuaki Chinzei and Kazunari Ishida, contributed equally to this manuscript.
References
- 1.Kelly MA. Extensor mechanism complications in total knee arthroplasty. Instr Course Lect. 2004;53:193–199. [PubMed] [Google Scholar]
- 2.Mochizuki RM, Schurman DJ. Patellar complications following total knee arthroplasty. J Bone Joint Surg [Am] 1979;61A:879–883. [PubMed] [Google Scholar]
- 3.Ortiguera CJ, Berry DJ. Patellar fracture after total knee arthroplasty. J Bone Joint Surg [Am] 2002;84A:532–540. doi: 10.2106/00004623-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Chew JT, Stewart NJ, Hanssen AD, Luo ZP, Rand JA, An KN. Differences in patellar tracking and knee kinematics among three different total knee designs. Clin Orthop Relat Res. 1997;345:87–98. doi: 10.1097/00003086-199712000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Dalury DF, Dennis DA. Extensor mechanism problems following total knee replacement. J Knee Surg. 2003;16:118–122. [PubMed] [Google Scholar]
- 6.Baldini A, Anderson JA, Cerulli-Mariani P, Kalyvas J, Pavlov H, Sculco TP. Patellofemoral evaluation after total knee arthroplasty. Validation of a new weight-bearing axial radiographic view. J Bone Joint Surg [Am] 2007;89A:1810–1817. doi: 10.2106/JBJS.E.00432. [DOI] [PubMed] [Google Scholar]
- 7.Berger RA, Rosenberg AG, Barden RM, Sheinkop MB, Jacobs JJ, Galante JO. Long-term followup of the Miller-Galante total knee replacement. Clin Orthop Relat Res. 2001;388:58–67. doi: 10.1097/00003086-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Kraay MJ, Darr OJ, Salata MJ, Goldberg VM. Outcome of metal-backed cementless patellar components: the effect of implant design. Clin Orthop Relat Res. 2001;392:239–244. doi: 10.1097/00003086-200111000-00030. [DOI] [PubMed] [Google Scholar]
- 9.D'Lima DD, Chen PC, Kester MA, Colwell CW., Jr Impact of patellofemoral design on patellofemoral forces and polyethylene stresses. J Bone Joint Surg [Am] 2003;4(85A Suppl):85–93. doi: 10.2106/00004623-200300004-00010. [DOI] [PubMed] [Google Scholar]
- 10.Ma HM, Lu YC, Kwok TG, Ho FY, Huang CY, Huang CH. The effect of the design of the femoral component on the conformity of the patellofemoral joint in total knee replacement. J Bone Joint Surg [Br] 2007;89B:408–412. doi: 10.1302/0301-620X.89B3.18276. [DOI] [PubMed] [Google Scholar]
- 11.Barnes CL, Sharma A, Blaha JD, Nambu SN, Carroll ME. Kneeling is safe for patients implanted with medial-pivot total knee arthroplasty designs. J Arthroplasty. 2011;26:549–554. doi: 10.1016/j.arth.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 12.Miyazaki Y, Nakamura T, Kogame K, Saito M, Yamamoto K, Suguro T. Analysis of the kinematics of total knee prostheses with a medial pivot design. J Arthroplasty. 2011;26:1038–1044. doi: 10.1016/j.arth.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 13.Omori G, Onda N, Shimura M, Hayashi T, Sato T, Koga Y. The effect of geometry of the tibial polyethylene insert on the tibiofemoral contact kinematics in advance medial pivot total knee arthroplasty. J Orthop Sci. 2009;14:754–760. doi: 10.1007/s00776-009-1402-3. [DOI] [PubMed] [Google Scholar]
- 14.Kanekasu K, Kondo M, Kadoya Y. Axial radiography of the distal femur to assess rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2005;434:193–197. doi: 10.1097/01.blo.0000156819.24866.8b. [DOI] [PubMed] [Google Scholar]
- 15.Martelli S, Ellis RE, Marcacci M, Zaffagnini S. Total knee arthroplasty kinematics. Computer simulation and intraoperative evaluation. J Arthroplasty. 1998;13:145–155. doi: 10.1016/S0883-5403(98)90092-4. [DOI] [PubMed] [Google Scholar]
- 16.Tei K, Ishida K, Matsumoto T, Kubo S, Sasaki H, Shibanuma N, et al. Novel image-matching software for postoperative evaluation after TKA. Orthopedics. 2012;35:e1711–5. doi: 10.3928/01477447-20121120-14. [DOI] [PubMed] [Google Scholar]
- 17.Chia SL, Merican AM, Devadasan B, Strachan RK, Amis AA. Radiographic features predictive of patellar maltracking during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2009;17:1217–1224. doi: 10.1007/s00167-009-0832-y. [DOI] [PubMed] [Google Scholar]
- 18.Grelsamer RP, Bazos AN, Proctor CS. Radiographic analysis of patellar tilt. J Bone Joint Surg [Br] 1993;75B:822–824. doi: 10.1302/0301-620X.75B5.8376449. [DOI] [PubMed] [Google Scholar]
- 19.Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C. An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res. 2004;420:213–219. doi: 10.1097/00003086-200403000-00030. [DOI] [PubMed] [Google Scholar]
- 20.Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215–220. doi: 10.1016/S0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 21.Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20:331–336. doi: 10.1007/s00167-011-1598-6. [DOI] [PubMed] [Google Scholar]
- 22.Goh JC, Lee PY, Bose K. A cadaver study of the function of the oblique part of vastus medialis. J Bone Joint Surg [Br] 1995;77B:225–231. [PubMed] [Google Scholar]
- 23.Nagamine R, Otani T, White SE, McCarthy DS, Whiteside LA. Patellar tracking measurement in the normal knee. J Orthop Res. 1995;13:115–122. doi: 10.1002/jor.1100130117. [DOI] [PubMed] [Google Scholar]
- 24.Sawatsky A, Bourne D, Horisberger M, Jinha A, Herzog W (2012) Changes in patellofemoral joint contact pressures caused by vastus medialis muscle weakness. Clin Biomech (Bristol, Avon) 27(6):595–601 [DOI] [PubMed]
- 25.Heegaard J, Leyvraz PF, Van Kampen A, Rakotomanana L, Rubin PJ, Blankevoort L. Influence of soft structures on patellar three-dimensional tracking. Clin Orthop Relat Res. 1994;299:235–243. [PubMed] [Google Scholar]
- 26.Kessler O, Patil S, Colwell CW, Jr, D’Lima DD. The effect of femoral component malrotation on patellar biomechanics. J Biomech. 2008;41:3332–3339. doi: 10.1016/j.jbiomech.2008.09.032. [DOI] [PubMed] [Google Scholar]
- 27.Konig C, Sharenkov A, Matziolis G, Taylor WR, Perka C, Duda GN, et al. Joint line elevation in revision TKA leads to increased patellofemoral contact forces. J Orthop Res. 2010;28:1–5. doi: 10.1002/jor.20952. [DOI] [PubMed] [Google Scholar]
- 28.Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE. Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:38–45. doi: 10.1097/00003086-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Carpenter RD, Brilhault J, Majumdar S, Ries MD. Magnetic resonance imaging of in vivo patellofemoral kinematics after total knee arthroplasty. Knee. 2009;16:332–336. doi: 10.1016/j.knee.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 30.Leszko F, Sharma A, Komistek RD, Mahfouz MR, Cates HE, Scuderi GR. Comparison of in vivo patellofemoral kinematics for subjects having high-flexion total knee arthroplasty implant with patients having normal knees. J Arthroplasty. 2010;25:398–404. doi: 10.1016/j.arth.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 31.Luring C, Perlick L, Bathis H, Tingart M, Grifka J. The effect of femoral component rotation on patellar tracking in total knee arthroplasty. Orthopedics. 2007;30:965–967. doi: 10.3928/01477447-20071101-15. [DOI] [PubMed] [Google Scholar]
- 32.Shimizu N, Tomita T, Yamazaki T, Yoshikawa H, Sugamoto K. The effect of weight-bearing condition on kinematics of a high-flexion, posterior-stabilized knee prosthesis. J Arthroplasty. 2011;26:1031–1037. doi: 10.1016/j.arth.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 33.Amiri S, Wilson DR, Masri BA, Sharma G, Anglin C. A novel multi-planar radiography method for three dimensional pose reconstruction of the patellofemoral and tibiofemoral joints after arthroplasty. J Biomech. 2011;44:1757–1764. doi: 10.1016/j.jbiomech.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 34.Barink M, Meijerink H, Verdonschot N, van Kampen A, de Waal MM. Asymmetrical total knee arthroplasty does not improve patella tracking: a study without patella resurfacing. Knee Surg Sports Traumatol Arthrosc. 2007;15:184–191. doi: 10.1007/s00167-006-0158-y. [DOI] [PubMed] [Google Scholar]
- 35.Matsumoto T, Kuroda R, Kubo S, Muratsu H, Mizuno K, Kurosaka M. The intra-operative joint gap in cruciate-retaining compared with posterior-stabilised total knee replacement. J Bone Joint Surg [Br] 2009;91B:475–480. doi: 10.1302/0301-620X.91B4.21862. [DOI] [PubMed] [Google Scholar]
- 36.Stiehl JB. A clinical overview patellofemoral joint and application to total knee arthroplasty. J Biomech. 2005;38:209–214. doi: 10.1016/j.jbiomech.2004.02.026. [DOI] [PubMed] [Google Scholar]
- 37.Komistek RD, Dennis DA, Mabe JA, Walker SA. An in vivo determination of patellofemoral contact positions. Clin Biomech (Bristol, Avon) 2000;15:29–36. doi: 10.1016/S0268-0033(98)00061-8. [DOI] [PubMed] [Google Scholar]
- 38.Becher C, Heyse TJ, Kron N, Ostermeier S, Hurschler C, Schofer MD, et al. Posterior stabilized TKA reduce patellofemoral contact pressure compared with cruciate retaining TKA in vitro. Knee Surg Sports Traumatol Arthrosc. 2009;17:1159–1165. doi: 10.1007/s00167-009-0768-2. [DOI] [PubMed] [Google Scholar]
- 39.Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kuroda R, Yoshiya S, et al. Joint gap kinematics in posterior-stabilized total knee arthroplasty measured by a new tensor with the navigation system. J Biomech Eng. 2006;128:867–871. doi: 10.1115/1.2354201. [DOI] [PubMed] [Google Scholar]
- 40.Merican AM, Ghosh KM, Iranpour F, Deehan DJ, Amis AA. The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:1479–1487. doi: 10.1007/s00167-011-1499-8. [DOI] [PubMed] [Google Scholar]
- 41.Kainz H, Reng W, Augat P, Wurm S. Influence of total knee arthroplasty on patellar kinematics and contact characteristics. Int Orthop. 2012;36:73–78. doi: 10.1007/s00264-011-1270-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heesterbeek PJ, Keijsers NL, Wymenga AB. Femoral component rotation after balanced gap total knee replacement is not a predictor for postoperative patella position. Knee Surg Sports Traumatol Arthrosc. 2011;19:1131–1136. doi: 10.1007/s00167-011-1409-0. [DOI] [PubMed] [Google Scholar]
- 43.Song CY, Lin JJ, Jan MH, Lin YF. The role of patellar alignment and tracking in vivo: the potential mechanism of patellofemoral pain syndrome. Phys Ther Sport. 2011;12:140–147. doi: 10.1016/j.ptsp.2011.02.008. [DOI] [PubMed] [Google Scholar]