Abstract
Purpose
Internal fixation versus joint replacement for treating intracapsular hip fractures is still a major debate. The Targon® FN fixation concept is innovative; two small case series are promising. We present the first larger series.
Methods
We conducted prospective documentation of all Targon® FN cases since 2006. The implant was used for all undisplaced fractures, and for displaced fractures in patients of a biological age ≤60 years. Besides demographic data and fracture classification, we analysed infection, haematoma, implant perforation, nonunion and operative revision procedures.
Results
In 135 cases (mean age 71 years; average operation time 60 minutes; average hospital stay ten days), we found a surgical complication rate of 16.4 %. Conversion to joint replacement was necessary in 9.6 %. Complication rate was significantly higher in displaced fractures.
Conclusions
Our study confirms low general complication rates. However, implant perforation seems to be underestimated. Optimised reduction technique may help to reduce this complication.
Keywords: Femoral-neck fracture, Intracapsular fracture, Hip screw, Complication rate, Cutout
Introduction
Proximal femoral fractures are a common reason why elderly patients are admitted to an acute orthopaedic ward. About half of these fractures are intracapsular. From 1934 to now, this particular fracture has been termed the “unsolved fracture” because of the continuing controversy between preserving the femoral head using internal fixation or replacing it using hemi-arthroplasty or total hip arthroplasty (THA) [1–4]. Consistently, the acceptance of published treatment guidelines remains limited [5]. Although mortality after arthroplasty has decreased during recent years [6], internal fixation is still well accepted for undisplaced fractures, and for younger patients with displaced intracapsular fractures. However, the limits of biological age and fracture displacement are still under discussion [7–10].
Secondary displacement of the fracture is the main complication associated with fixation of an intracapsular fracture. This is reported in about 5 % of undisplaced fractures and up to 30 % of displaced fractures treated by reduction and fixation [11–13]. This complication is essentially mechanical, with the traditional screw fixation obviously failing to fix the fracture in a sufficiently stable configuration. The Targon® FN implant was designed to overcome these shortcomings by applying up to four so-called TeleScrews with 10- to 20-mm telescoping capacity, allowing for controlled fracture collapse. Angular stable attachment of the TeleScrews to a small contoured lateral locking plate was meant to reduce the risk of femoral-head rotation or tilting [14]. Some smaller case series have been published, reporting encouraging results [14, 15]. However, there is still insufficient data to determine whether this novel method is superior to conventional screw fixation. We present the first respectable series of >100 consecutive cases treated with the Targon® FN.
Patients and methods
Between August 2006 and June 2013, every femoral fracture fixation in our urban academic teaching hospital was performed using the Targon® FN implant. Indication for fracture fixation versus joint replacement was made as follows:
Patients ≤60 years were treated by osteosynthesis (Targon® FN) regardless of fracture classification.
Patients >60 years were treated by osteosynthesis (Targon® FN) for fractures Garden 1 and 2 or by arthroplasty for fractures Garden 3 and 4.
Patients with severe osteoarthritis or renal osteopathy were treated with arthroplasty.
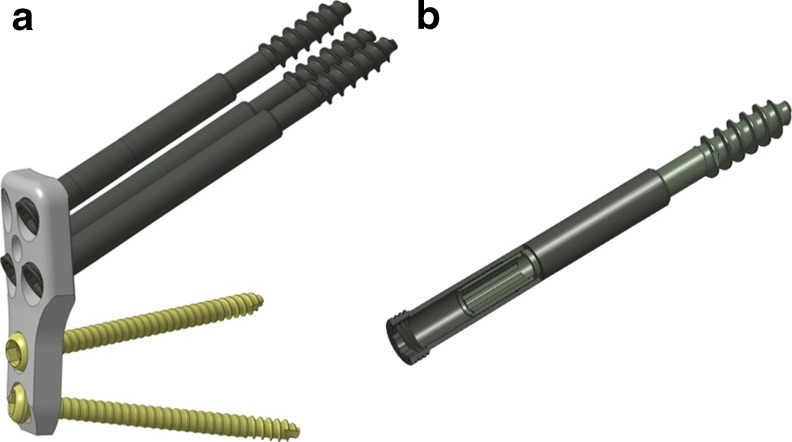
All cases were collected prospectively in a database that includes general information, i.e. age, gender, fracture type (classifications according to Pauwels and Garden), American Society of Anesthesiologists (ASA) score, preoperative haemoglobin level, time to surgery, operative time and number and length of TeleScrews used [16–18]. Furthermore, parameters included all surgical complications that either occurred during the initial hospital stay or caused readmission. Complications were assigned to wound infection, haematoma, cutout and nonunion. All reoperations were registered. In all patients, a Targon® FN nail was used (Aesculap AG, Tuttlingen, Germany). This novel implant provides dynamic fracture fixation with up to four so-called TeleScrews, which are 6.5 mm cancellous screws with an integrated telescoping capacity of 10–20 mm (Fig. 1). The TeleScrews are attached to an anatomically shaped locking side plate, which is attached to the femoral shaft by another two 4.5-mm bicortical screws.
Fig. 1.
The Targon® FN system consists of a contoured locking sideplate, with up to four 6.5-mm TeleScrews for fracture fixation and two 4.5-mm bicortical screws for the shaft (a). TeleScrews have an integrated gliding capacity of 10–20 mm without the risk of backing out (b)
Statistics were performed using IBM® SPSS® Version 19.0.0. All confidence intervals (CI) are 95 %. To detect significantly different complication frequencies, we used the χ2 test in cases with all expected values greater than five; otherwise, we used the two-sided Fisher’s exact test. Means were compared using the Wilcoxon two-sample signed-rank test (Mann–Whitney U test). Correlations were determined using Spearman’s rho [19].
Results
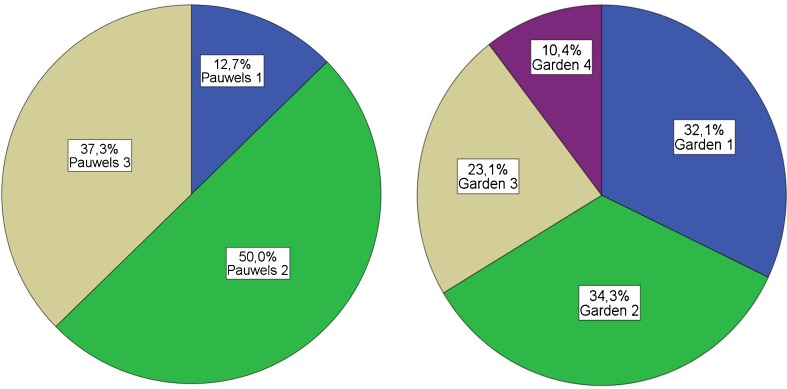
Our series consisted of 135 Targon® FN implantations (right, 66; left, 69) in 135 patients [76 women (56.3 %)]. Mean patient age was 71.1 [range 26–95; standard deviation (SD) 15.3] years. On average, men were significantly younger than women (65.8 vs. 75.2 years; p < 0.001). ASA score was one in 19 patients (14.1 %), two in 46 patients (34.1 %), three in 65 patients (48.1 %), and four in five patients (3.7 %). ASA score distribution did not significantly differ between men and women (p = 0.4 ; Mann–Whitney U test). All fractures except one were intracapsular. There was one case of converting failed femoral-neck screws into Targon® FN fixation; all other cases were primary implantations. Fracture classification according to Pauwels and Garden is shown in Fig. 2. Mean time between injury and operation was two (range: zero–21; SD 3.0) days. Higher ASA scores were correlated with longer time to surgery (Spearman’s ρ = 0.38, p < 0.00001).
Fig. 2.
Proportion of fracture types according to Pauwels and Garden
Mean operative time was 60.4 (range 33–151; 95 % CI, 57.0–63.9) minutes. In 111 cases, three TeleScrews were used (82.2 %), 23 implantations made use of four TeleScrews (17.0 %) and in one case (0.7 %), only two such screws were used. Operative time was somewhat longer if four TeleScrews were used (64.9 vs. 59.5 min); however, this difference was not significant (p = 0.24). Neither TeleScrew number nor length was associated with cutout. Median hospital stay was 10.0 [interquartile range (IQR) seven) days; 55.2 % of patients were discharged to their home, 32.8 % to a rehabilitation facility (8.2 % geriatric rehabilitation), 4.5 % to personal care home and 5.2 % to another medical ward for reasons unrelated to the fracture. Overall surgical complication rate was 16.4 % (95 % CI, 10.1–22.8), and 30-day mortality rate was 2.2 % (95 % CI, 0–4.7 %). There were no infections; haematoma rate was 4.4 % (95 % CI, 0.9–8.0); nonunion rate was 2.2 % (95 % CI, 0–4.7); cutout rate was 9.6 % (95 % CI, 4.6–14.7). Operative revision rates are shown in Table 1.
Table 1.
Surgical revision rates with 95 % confidence interval (CI). The main reason for revision surgery was conversion to arthroplasty because of implant perforation
| Percentage | 95 % CI | |
|---|---|---|
| Wound revision (hematoma) | 4.4 | 0.9–8.0 |
| Correction of TeleScrew | 3.7 | 0.5–6.9 |
| Conversion to hemiarthroplasty | 5.2 | 1.4–9.0 |
| Conversion to total hip arthroplasty | 4.4 | 0.9–8.0 |
Fracture angle according to Pauwels classification influenced surgical complication rate: complication rates differed following Pauwels fracture grade 1 (5.9 %; 95 % CI, 0–18.4), grade 2 (9.0 %; 95 % CI, 1.9–16.0 %]) and grade 3 (28.0 %; 95 % CI, 15.1–40.9 %]). These differences were significant on Mann Whitney U test (p = 0.004). Complication rate was also associated with Garden classification: differences between Garden 1 (11.6 %; 95 % CI, 1.6–21.6), 2 (10.9 %; 95 % CI, 1.5–20.2), 3 (22.6 %; 95 % CI, 7.0–38.2) and 4 (42.9 %; 95 % CI, 13.2–72.5) were significant (p = 0.007). Complication rate of displaced fractures (Garden 3/4) was 28.9 % (95 % CI, 15.1–42.7) and in undisplaced fractures (Garden 1/2) 11.2 % (95 % CI, 4.5–17.9); this difference was significant (p = 0.01). No associations were found between surgical complication rate and age, gender, ASA score, preoperative haemoglobin level and number or length of TeleScrews used. Average operation time in complication cases was longer (63.5 vs. 59.9 min; p = 0.4), whereas mean time to surgery by tendency was shorter (1.2 vs. 2.1 days; p = 0.2).
Discussion
Multiple parallel screws are reported to have limited purchase on the lateral femoral cortex, provoking fixation failure by fracture tilt into the varus position. The sliding hip screw, which may be regarded as an alternative, provides a reliable lateral fixation and allows the fracture to collapse along the femoral-neck axis. However, medial purchase is limited, causing a lack of rotational stability, which facilitates implant perforation by cutting out [14]. The Targon® FN was designed with these specific shortcomings in mind. Linking proximal sliding screws (TeleScrews) and distal bicortical screws with a locking plate is intended to provide a stable construction with superior rotational stability than would be found with either method of fixation. The theoretical concept of combining the advantages of parallel screws (good medial hold) and sliding screw (good lateral hold) is convincing; however, publications on clinical experiences are rare [14, 15]. This is the first report on a consecutive series of >100 Targon® FN implantations (n = 135). In 2010, Parker and Stedtfeld published a series of 83 patients [14]; the Dutch publication of Körver et al. reports a smaller series of 16 patients [15].
Whereas patient demographics and total surgical complication rate are similar, the kind of complications reported differ remarkably (Table 2). Reports of haematomas and infection were rare in all published series; we found implant perforation (cutout) to be the main complication. This contrasts with findings of Parker and Stedtfeld, who reported only one such case and emphasised nonunion as the predominant problem [14]. This might be explained by the lower rate of displaced fractures in our series, reflecting our reservation against the Targon® FN for fracture fixation in orthogeriatrics. Conn and Parker [11] reported a nonunion rate of 6 % even for undisplaced fractures fixed by parallel cancellous screws, which seems to be reduced to 2.2 % in our Targon® FN cases. For displaced fractures, nonunion rates up to 33 % are reported [12].
Table 2.
Overview of patient demographics, operation time, fracture displacement and complication rates in the literature and in our series
| Parker and Stedtfeld [14] | Körver et al. [15] | Our series | |
|---|---|---|---|
| No. patients | 83 | 16 | 135 |
| Mean patient age | 75 years | 79 years | 71 years |
| M/F ratio | 30/53 | 4/12 | 59/76 |
| Mean operation time (min) | 45 (20–110) | 53 (39–73) | 60 (33–151) |
| Mean hospital stay (days) | 11.4 | – | 12.0 |
| Displaced fractures (Garden 3 + 4) | 55 % | 42 % | 34 % |
| Total surgical complication rate | – | 12.5 % | 16.4 % |
| Haematoma | 0 % | 0 % | 4.4 % |
| Infection | 2.4 % | 0 % | 0 % |
| Hip perforation (cutout, cut through) | 1.2 % | 12.5 % | 9.6 % |
| Nonunion | 9.6 % | 0 % | 2.2 % |
Indications for the Targon® FN
Consistent with other reports, we found a significantly higher complication rate in displaced fractures (28.9 % vs. 11.2 %; p = 0.01) [11–14]. This is also consistent with reports on equal total socio-economic costs comparing fracture fixation and joint replacement for displaced intracapsular fractures [20]. Although we found no association between patient age and complication rate, we preferred primary hip replacement (hemiarthroplasty) in elderly patients with displaced fractures. Some authors favour internal fracture fixation in these patients, emphasising the advantage of a less-invasive operation but accepting the risk for reoperation. For orthogeriatric patients, however, we follow a philosophy of “one shot for each fracture”, thus being restrictive in fixation of displaced fractures.
Fracture reduction
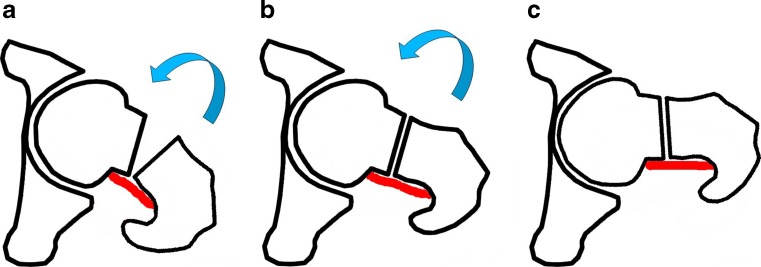
Hip perforation was the predominant mechanism of failure in our series (9.6 %; 95 % CI, 4.6–14.7), causing conversion to hemiarthroplasty or THA. In all these cases, fracture reduction was incomplete to some degree. Fracture reduction is achieved in a two-step procedure: First, reduction in the anteroposterior view is achieved by traction. Then, reduction is completed in the axial view by internal rotation. The necessary internal rotation, however, may be immense in some cases. In fear of internal rotation displacement, surgeons often tend to completely refrain from performing this manoeuvre. It is a matter of training to understand that in intracapsular hip fractures (not in trochanteric fractures), internal rotation is very rarely exaggerated due to the effect of the tight Weitbrecht ligament, which remains intact in most cases (Fig. 3).
Fig. 3.
The ligament of Weitbrecht remains intact in most cases, and internal rotation of the leg is needed for reduction (a). With full reduction the posterior joint capsule is tight (b). In intracapsular fractures, further internal rotation will not result in displacement, as reduction will be maintained by the tension of Weitbrecht’s ligament (c)
Length and number of TeleScrews
There is neither literature nor manufacturer advice on how many screws to use. We used three TeleScrews in the majority of cases (82 %) and four in cases of severe dislocation (Garden 4) or poor bone stock, determined by individual surgeon decision. We placed the TeleScrews as centrally as possible. A significant difference in complication rate according to the number or length of TeleScrews was not seen.
Limitations of this study are that it is from a single centre without a control group or randomisation to a group treated with a conventional fixation method, such as the sliding hip screw or multiple screws. Surgical delay between time of injury and operation may also contribute to complication rates [21]; however, this factor was not analysed in our study. Comparison to the limited number of other case series is complicated by different indication philosophies, especially in the orthogeriatric field. As reported by other publications, the elderly population studied is associated with a considerable mortality rate, making it impossible to follow all patients with a complete radiographic series.
In summary, our study confirms the encouragingly low complication rates of the Targon® FN system. However, we found that the impact of fixation failure leading to hip perforation by cutout may have been thus far underestimated. Further biomechanical and clinical studies are needed to determine whether cutout rate can be influenced by improved fracture reduction techniques.
Conclusions
Our experience with the Targon® FN supports preliminary reports suggesting that this implant may be a major advancement in managing the intracapsular fracture and a possible solution to the dilemma of the “unsolved fracture”. However, we found evidence that cutout may be a relevant problem with this method. Detailed studies examining the influence of factors such as fracture reduction and TeleScrew positioning should be undertaken in order to better evaluate the Targon® FN system.
References
- 1.Dickson JA. The “unsolved” fracture. J Bone Joint Surg Am. 1953;35:805. [PubMed] [Google Scholar]
- 2.McCarroll HR. Has a solution for the “unsolved fracture” been found? Problems and complications of fractures of femoral neck. JAMA. 1953;153:536–540. doi: 10.1001/jama.1953.02940230008004. [DOI] [PubMed] [Google Scholar]
- 3.Kannan A, Kancherla R, McMahon S, Hawdon G, Soral A, Malhotra R. Arthroplasty options in femoral-neck fracture: answers from the national registries. Int Orthop. 2012;36:1–8. doi: 10.1007/s00264-011-1354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim JW, Nam KW, Yoo JJ, Kim HJ. The role of preoperative bone scan for determining the treatment method for femoral neck fracture. Int Orthop. 2007;31:61–64. doi: 10.1007/s00264-006-0138-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zielinski SM, Meeuwis MA, Heetveld MJ, Verhofstad MH, Roukema GR, Patka P, Van Lieshout EM. Dutch femoral neck fracture investigator group. Adherence to a femoral neck fracture treatment guideline. Int Orthop. 2013;37:1327–1334. doi: 10.1007/s00264-013-1888-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schneppendahl J, Grassmann JP, Petrov V, Böttner F, Körbl B, Hakimi M, Betsch M, Windolf J, Wild M. Decreasing mortality after femoral neck fracture treated with bipolar hemiarthroplasty during the last twenty years. Int Orthop. 2012;36:2021–2026. doi: 10.1007/s00264-012-1600-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Health Technol Assess. 2005;9:iii–iv. doi: 10.3310/hta9410. [DOI] [PubMed] [Google Scholar]
- 8.Parker MJ, Pryor G, Gurusamy K. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures: a long-term follow-up of a randomized trial. Injury. 2010;41:370–373. doi: 10.1016/j.injury.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Parker MJ, Pryor GA. Internal fixation or arthroplasty for displaced cervical hip fractures in the elderly: a randomized controlled trial of 208 patients. Acta Orthop Scand. 2000;71:440–446. doi: 10.1080/000164700317381090. [DOI] [PubMed] [Google Scholar]
- 10.Heetveld MJ, Rogmark C, Frihagen F, Keating J. Internal fixation versus arthroplasty for displaced femoral neck fractures: what ist he evidence? J Orthop Trauma. 2009;23:395–402. doi: 10.1097/BOT.0b013e318176147d. [DOI] [PubMed] [Google Scholar]
- 11.Conn KS, Parker MJ. Undisplaced intracapsular hip fracture: results of internal fixation in 375 patients. Clin Orthop Relat Res. 2004;421:249–254. doi: 10.1097/01.blo.0000119459.00792.c1. [DOI] [PubMed] [Google Scholar]
- 12.Lu-yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck: a meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76:15–25. doi: 10.2106/00004623-199401000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Parker MJ, Raghavan R, Gurusamy K. Incidence of fracture-healing complications after femoral neck fractures. Clin Orthop Relat Res. 2007;458:175–179. doi: 10.1097/BLO.0b013e3180325a42. [DOI] [PubMed] [Google Scholar]
- 14.Parker MJ, Stedtfeld H. Internal fixation of intracapsular hip fractures with a dynamic locking plate; initial experience and results for 83 patients treated with a new implant. Injury. 2010;41:348–351. doi: 10.1016/j.injury.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Körver RJ, Wieland AW, Kaarsemaker S, Nieuwenhuis JJ, Janzing HM. Clinical experience, primary results and pitfalls in the treatment of intracapsular hip fractures with the Targon® FN locking plate. Injury. 2013 doi: 10.1016/j.injury.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 16.Pauwels F. Biomechanics of the normal and diseased hip. New York: Springer; 1976. [Google Scholar]
- 17.Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961;43:647–663. [Google Scholar]
- 18.American Society of Anesthesiologists (ASA) New classification of physical status. Anesthesiology. 1963;24:111. [Google Scholar]
- 19.Peacock JL, Peacock PJ. Oxford Handbook of Medical Statistics. Oxford: Oxford University Press; 2011. [Google Scholar]
- 20.Johansson T, Bachrach-Lindström M, Aspenberg P, Jonsson D, Wahlström O. The total costs of a displaced femoral neck fracture: comparison of internal fixation and total hip replacement. A andomized study of 146 hips. Int Orthop. 2006;30:1–6. doi: 10.1007/s00264-005-0037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sebestyén A, Boncz I, Sándor J, Nyárády J. Effect of surgical delay on early mortality in patients with femoral neck fracture. Int Orthop. 2008;32:375–379. doi: 10.1007/s00264-007-0331-z. [DOI] [PMC free article] [PubMed] [Google Scholar]