Abstract
Purpose
The optimal treatment of calcaneal fractures is controversial. A specific subgroup of healthy patients has good outcomes with open reduction and internal fixation using an extensile lateral approach. However, there are many patients who do not fit into this category. Consequently, they are either denied surgical intervention or put at significant risk of developing complications as a result of open surgical intervention. Minimally invasive reduction and fixation (MIRF) of calcaneal fractures can restore the height, width, length and shape of the hindfoot in addition to restoring the orientation of the posterior facet of the calcaneus (Böhler’s angle).
Methods
We present a series of 31 patients treated with minimally invasive reduction and fixation technique using threaded K wires and Steinmann pins as an alternative treatment method in patients who are not suitable for open reduction and internal fixation.
Results
The mean time to surgery from injury was six days (range one to ten days). The mean duration of surgery was 35 minutes (range 11–52 minutes). The mean followup was 14.9 months (range of seven to 30 months). The mean change in Böhler’s angle and length of the calcaneus from intra-operative fixation to final followup were 18.7° and 4.7 mm, respectively. The complication rate was low and there was one case of a superficial wound infection and no cases of deep infection or peroneal impingement in this series.
Conclusion
The MIRF technique with the use of threaded K wires has not been previously described in the literature. In our experience, the operative time is short and can be safely performed even in the presence of extensive soft tissue swelling in the immediate period following injury. The infection risk is low and calcaneal morphology was improved and maintained in terms of Böhler’s angle. This technique is suitable to be considered in patients who have significant medical co-morbidities (smokers, diabetics, peripheral vascular disease) and in those patients who are not suitable for an extensile lateral approach and internal fixation.
Keywords: Minimally invasive, Calcaneum, Fracture, Fixation
Introduction
Open reduction and internal fixation of displaced calcaneal fractures has been shown to be superior to nonoperative treatment in a select group of healthy patients [1].] However, many patients will not fit into this subgroup either due to medical co-morbidities, wound concerns or non-compliance. The complications of an extensile lateral approach with the calcaneus have been reported extensively in the literature with infection rates varying from 1.8 to 27 % [1, 2]. The incidence of osteomyelitis has been reported to be approximately 2.5 % [3]. The cost of infectious complications is significant [4].
The use of minimally invasive reduction and fixation of calcaneal fractures (MIRF) may have a role in this group of patients where there is a concern regarding wound healing and infection [5]. Numerous studies have reported satisfactory reductions of both intra and extra-articular fractures and reduced wound complications using MIRF [6–14]. In addition, it is advantageous to improve hindfoot morphology in an ‘at risk’ group of patients who otherwise would potentially be treated nonoperatively.
This paper reports the surgical technique of using MIRF in a group of patients that were deemed unsuitable for open reduction and internal fixation using an extensile lateral approach due to medical co-morbidity. The incidence of infection and radiographic results are also reported.
Materials and methods
Between January 2000 and December 2012, 31 patients with displaced intra-articular calcaneal fractures not deemed suitable for an extensile lateral approach and internal fixation were identified. They were treated with MIRF by a single surgeon (senior author) in a Level 1 trauma centre. Sanders type IV fractures were excluded. Approval was obtained from the Institutional Review Board and chart data was analysed for patient demographics, details of surgical treatment and incidence of complications from the time of injury to most recent followup. All fractures were classified using the Sanders, Essex-Lopresti and Orthopedic Trauma Association classifications based on pre-operative radiographs and computed tomography (CT) scans [15, 16]. Pre-operative, at time of intervention and final followup radiographs (lateral and Harris axial views) were reviewed and the Böhler’s angle and length were measured as described by Abdelgaid [8]. Following appropriate training on how to measure these radiographic parameters, two assessors not directly involved with patient care independently reviewed patients’ radiographs. There were no significant intra and interobserver differences in the parameters measured.
Surgical technique
‘Joint-depression’ fracture
The patient is positioned in the lateral decubitus position on a radiolucent table and a tourniquet applied. A small oblique 2-cm incision is made 2-cm distal to the tip of the fibula with the use of intra-operative fluoroscopy to ensure access to the posterior facet via the lateral wall fracture. The sural nerve is often visualised in the operative field and protected. Blunt dissection is performed inferior to the peroneal tendons and the lateral wall of the calcaneus identified. A large Steinmann pin positioned from lateral to medial in the inferior portion of the posterior calcaneum is utilised as a reduction tool in order to adjust calcaneal height and to some degree control varus-valgus alignment. Intra-operative fluoroscopy is then used to determine the entry point for a small periosteal elevator to create a tract across to the medial aspect of the posterior facet of the calcaneus (Fig. 1a,b). Elevation of the posterior facet is then achieved with the use of a laminar spreader that reduces the posterior facet by using the corresponding articular surface of the talus as a template (Fig. 2a–d). This initial manoeuvre restores the height of the calcaneus and partially restores the articular surface of the posterior facet of the calcaneus.
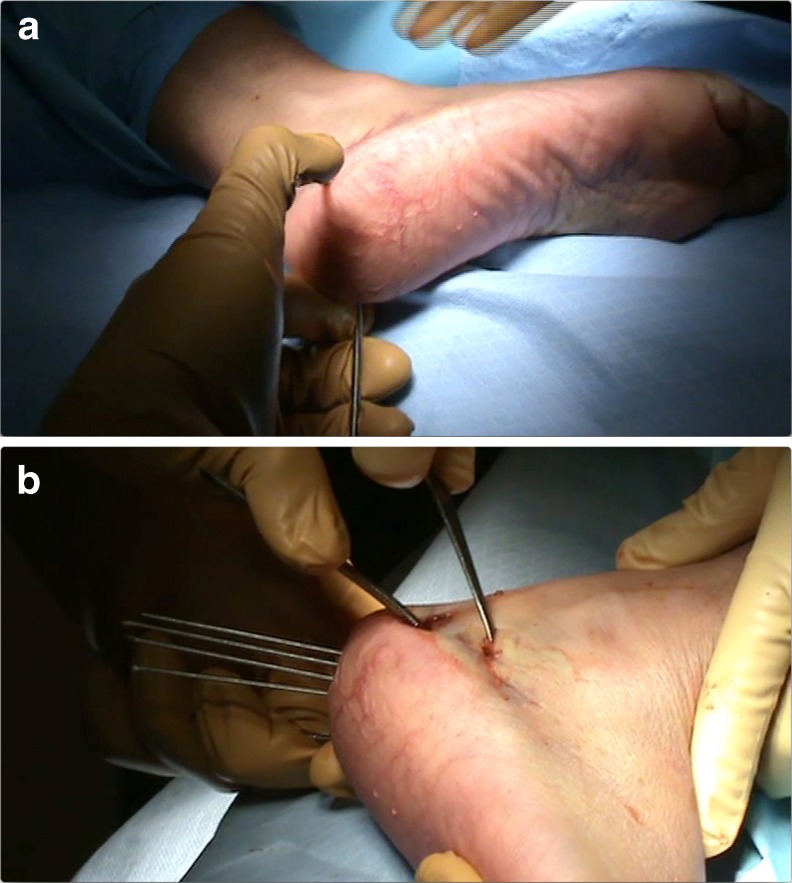
Fig. 1.
a A large Steinmann pin is used as a reduction tool to manipulate the posterior tuberosity fragment and retension of the Achilles tendon and restore some calcaneal height and control varus-valgus alignment. b Periosteal elevator inserted via lateral wall fracture and threaded K wires positioned initially in posterior tuberosity not crossing the fracture line are also used to facilitate fracture reduction
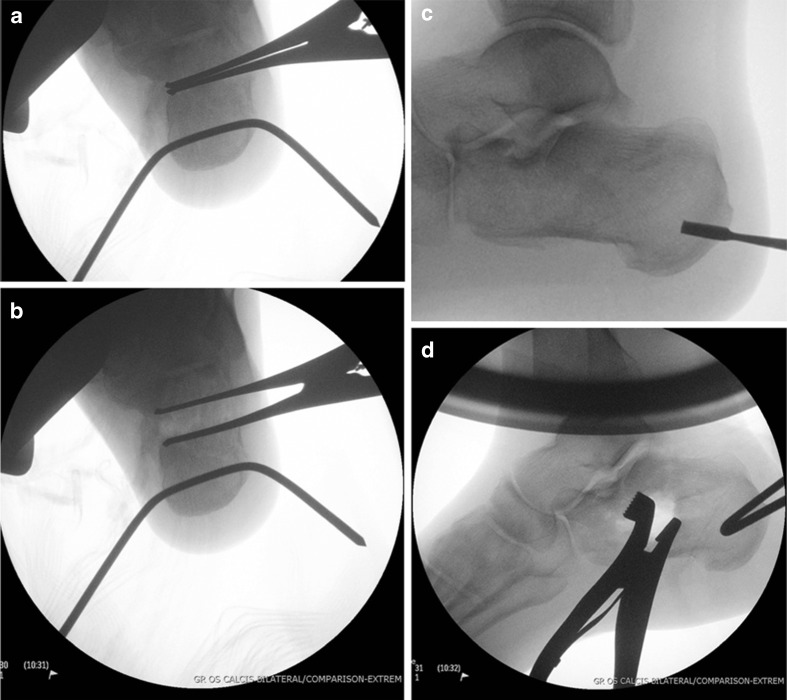
Fig. 2.
(a and b) Harris axial radiograph demonstrating the use of a laminar spreader inserted along width of posterior facet and used to elevate fragment using the talus as a template for reduction. (c and d) Pre and post reduction manoeuvre lateral radiograph illustrating resultant bone defect
Fully threaded 0.062-in K wires (usually 4 or 5) are positioned in the posterior aspect of the plantar surface of the heel into the posterior aspect of the calcaneal tuberosity (Fig. 1b). The K wires can then be used to control the varus-valgus alignment of the heel. Longitudinal traction (using the Steinmann pin) tensions the Achilles tendon distracting the calcaneal tuberosity fragment (Fig. 3). If a subchondral lag screw is to be placed, it is drilled and positioned in the posterior subtalar bone compressing any split in the facet. The K wires are then advanced into the subchondral bone of the posterior articular facet and maintain the reduction of height and valgus alignment of the heel. Following disimpaction of the posterior facet the bone defect is filled with calcium sulphate bone graft substitute (Osteoset, Wright Medical Technology Inc., Arlington, TN; Fig. 4a,b). Reduction of the fracture was assessed intra-operatively with fluoroscopy using a lateral, Harris axial and multiple Broden’s views of the posterior facet [17].
Fig. 3.

Calcaneal height has been increased following reduction and gaping of lateral incision is seen as a result
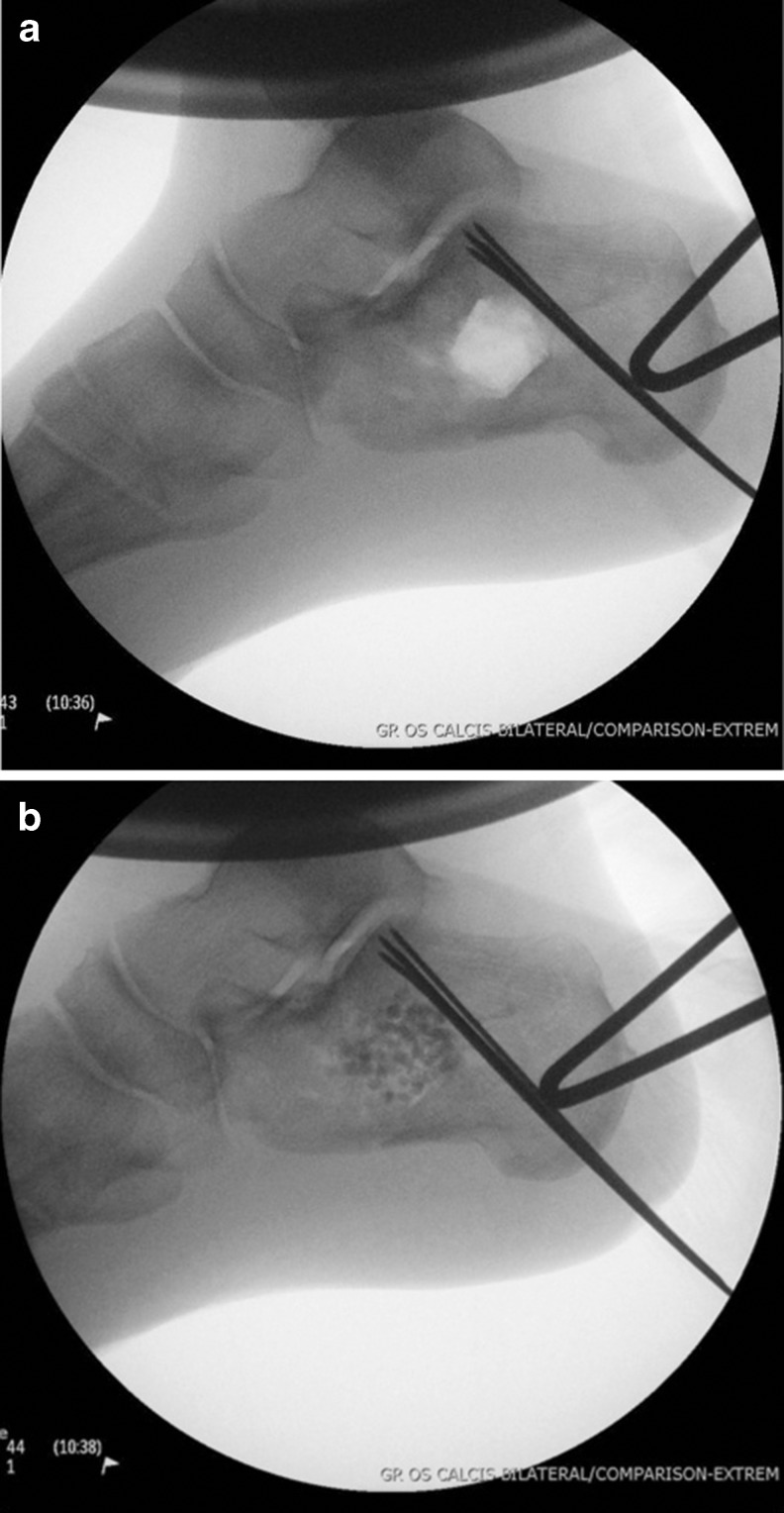
Fig. 4.
a Void following reduction of posterior facet with multiple threaded K wires positioned in subchondral bone along the width of the posterior facet from medial to lateral . b Void filled with calcium sulphate bone substitute
The K wires are cut approximately 1 cm from the skin (Fig. 5) and dressed with protective gauze dressings and a plaster slab applied. The plaster slab is removed two days postoperatively and the patient encouraged to mobilise the ankle and subtalar joints. They are not allowed to bear weight. No prefabricated boot is used for additional protection. Pin-site care involves daily washing with soap and water only. Patients are commonly discharged on the second postoperative day. The K wires are removed in the outpatient clinic ten to 12 weeks postoperatively using a power tool on reverse as the thread still provides good fixation with little evidence of loosening and full weightbearing is begun on the injured limb.
Fig. 5.

Intraoperative photograph showing restoration of hindfoot valgus and K wires cut 1-cm long
‘Tongue-type’ fracture
Tongue type fractures were treated by manipulating the large posterior facet fragment with either one or two large Steinmann pins positioned posteriorly along the length of the fracture fragment, as previously been described by Tornetta [18]. The fracture reduction was maintained using the Steinmann pins which were advanced into the anterior calcaneal tuberosity and if necessary in poor bone into the cuboid crossing the calcaneocuboid joint. Assessment of reduction was performed fluoroscopically as described for joint depression fractures. The postoperative regimen was the same as for joint-depression fractures and the Steinmann pin removed in the outpatient clinic ten to 12 weeks following surgery.
Results
Patient demographics are shown in Table 1. The mean time to surgery from injury was six days (range one to ten days). The mean duration of surgery was 35 minutes (range 11–52 minutes). There were no problems with wound healing or necrosis in the followup period except one case of a superficial wound infection. The mean followup was 14.9 months (range seven to 30 months). At final followup, all fractures were healed. The radiographic parameters recorded at time of injury, intra-operatively and at final followup are shown in Table 2. A Shapiro-Wilk W test was used to assess all radiographic variables for normal distribution. All normally distributed variables were statistically analysed using a paired t-test. The Böhler’s angle at the time of injury was the only variable that was not normally distributed, and this was assessed using a Wilcoxon signed-rank test. The mean change in Böhler’s angle and length of the calcaneus from intraoperative fixation to final followup were 18.7° and 4.7 mm, respectively. Calcium sulphate bone graft substitute was used in 23 (74 %) of cases and the complications of treatment are shown in Table 3.
Table 1.
Patient demographics from the Orthopedic Trauma Association (OTA)
| Characteristic | Value |
|---|---|
| Age (mean) | 45.6 years (range 24–64) |
| Gender | 9 female, 22 male |
| Smokers | 24 (77 %) |
| Patient co-morbidities | 3 Alcohol abuse |
| 2 Poorly controlled Type-2 diabetes | |
| 1 Congestive cardiac failure (severe peripheral oedema) | |
| 2 Peripheral vascular disease | |
| Open fractures | 2 |
| Sanders II/OTA 73-C1 | 12/31 |
| Sanders III/OTA 73-C2 | 9/31 |
| Tongue | 10/31 |
| Joint-depression | 21/31 |
Table 2.
Radiographic analysis of fractures
| Measure | Injury (SD) | Intra op (SD) | Healed (SD) | Δ Injury to intra op | Δ Intra OP to healed |
|---|---|---|---|---|---|
| Mean Böhler’s angle (degrees) | 6.1° (10.97) | 24.8° (7.0) | 22.1° (6.6) | 18.7 (p = 0.0000) | 2.87 (p > 0.05) |
| Mean length (mm) | 80.9 (10.28) | 85.6 (6.98) | 84.1 (8.36) | 4.7 (p = 0.0037) | 1.7 (p > 0.05) |
P < 0.05 was considered statistically significant
Table 3.
Complications of treatment
| Complication | N |
|---|---|
| Superficial wound infection | 1 |
| Deep infection | 0 |
| Subtalar fusion | 0 |
| Peroneal impingement | 0 |
Discussion
The treatment of calcaneal fractures still remains controversial [1, 14]. The extensile lateral approach traditionally has been used to treat displaced intra-articular calcaneal fractures in healthy patients who are deemed suitable for surgical intervention. Due to the complications of the extensile lateral approach minimally invasive techniques may be an alternative with fewer adverse outcomes in high risk unhealthy patients. One of the earliest descriptions of minimally invasive treatment of calcaneal fractures using ligamentotaxis was by Clark [19] in 1855. MIRF were also described by Westhues and subsequently modified by Essex-Lopresti for ‘tongue-type’ fractures [15]. Tornetta [18] reported using the Essex-Lopresti reduction technique for treating Sanders IIC fractures with screw fixation. There have been numerous reports of less invasive surgical techniques using screws [6, 8, 9], bioabsorbable screws [20], arthroscopically assisted with screws [10], K wires [7, 12], external fixation to aid reduction with percutaneous screws [11], and external fixation [21] alone to treat displaced intra and extraarticular fractures with satisfactory results described. Schildhauer and Sangeorzan [22] described the use of a push screw, which allows controlled and gradual reconstitution of the length and height (Böhler’s angle) of the hindfoot, though, it is only recommended as a temporary salvage procedure. The MIRF technique with threaded K wires used in this study has not been described in the literature. Patients were selected based upon having significant multiple medical co-morbidities and smoking status, which would exclude them from receiving internal fixation using an extensile lateral approach.
The goals of treating calcaneal fractures are to restore articular congruity and hindfoot morphology. Nonoperative treatment has been associated with poor results secondary to subtalar arthrosis and abnormal hindfoot morphology [1, 3]. Anatomical reduction of the posterior facet may not be essential for good clinical results, and restoration of hindfoot morphology may be a more important factor than previously thought [23]. Levine and Helfet [24] reported preservation of subtalar movement with ‘near anatomic’ percutaneous reduction and fixation. Their explanation was minimal dissection results in less postoperative swelling and periarticular scarring compared to an extensive open approach. Böhler’s angle has been correlated with outcomes in displaced intra-articular calcaneal fractures [25]. Our results have demonstrated that MIRF can achieve good restoration of hindfoot morphology with a mean increase in Böhler’s angle of 16° (mean pre-operative Böhler’s angle of 6.1° and final Böhler’s angle of 22.1°). A mean loss of 2.9° from initial reduction to final followup was observed which was not statistically significant. This correlates with data published on percutaneous reduction with screw fixation [9] and fractures treated with an extensile lateral approach and plate fixation [26]. Bakker et al. reported a significant secondary decrease of Böhler’s angle of 11° at one year following trauma in conservatively treated fractures [27]. There was only a small increase in the length of the calcaneum by 4.7 mm. The ability to control length of the calcaneum using K wires is difficult and a limitation of this technique.
The risk of deep infection and potential limb threatening complications following open reduction and internal fixation of calcaneal fractures is significant [1, 2, 4]. DeWall et al. [9] reported a deep infection rate of 14.3 % and minor wound complication rate of 21.4 % in patients treated with open reduction via an extensile lateral approach and no deep infections and 6 % minor wound complication rate with percutaneous treatment. Stulik et al. [7] report a superficial infection rate of 7 % and deep infection rate of 1.7 % using percutaneous K wire fixation. Abelgaid [8] and Rammelt et al. [10] reported no deep infections in their series of percutaneous screw fixation of 61 Sanders II fractures. The cohort of patients in this study was at greater risk of developing wound complications as a result of medical co-morbidity and smoking status. There was one case of a superficial wound infection and no deep wound infections in this series. This was despite using K wires which were not buried beneath the skin. This may be explained by a relatively short operative time (mean 35 minutes) and threaded K wires inhibiting micromotion, loosening and soft tissue irritation. The threaded K wires are not loose at 12 weeks postoperatively and need to be removed with a power tool to reverse them out. Demcoe et al. [28] showed an infection rate of 1.8 % using threaded K wire fixation using an extensile lateral approach.
The mean time from injury to surgery in our study was six days. However, the ease of fracture reduction correlated with early surgery in this study and operating as early as day one post injury had no adverse outcome. The risk of wound complications using MIRF does not necessitate soft tissue swelling to subside. Stulik et al. [7] performed surgery within 48 hours on 89 % of patients in their series and also stated earlier surgery facilitated reduction. Rammelt et al. [10] also found that after ten days percutaneous reduction of fractures was difficult. Tornetta [18] reported that in ideal situations surgery is performed within three to five days. Our recommendation is that if the patient is fit for surgery, the earlier it is performed the better.
There are concerns whether the use of bone substitutes increase the risk of infection. Calcium sulphate bone graft substitute (Osteoset, Wright Medical Technology Inc., Arlington, TN) was used for 23 patients (74 %) in this study with no increased risk of infection. Chen et al. [29] reported percutaneous fixation with the use of calcium sulphate bone cement. They allowed earlier weight bearing compared to open reduction and internal fixation of displaced intra-articular calcaneal fractures. The use of autologous bone graft has not been shown to have radiological or functional benefit [26]. Balloon reduction and cement fixation of fresh calcaneal fractures (“balloon calcaneoplasty”) has been reported as a safe and effective procedure in a variety of calcaneal fractures with lasting and excellent clinical results [13].
The limitations of this study are that it is a retrospective chart review with small numbers of patients and only radiographic assessment performed. Weight bearing radiographs and Broden views were not routinely performed at followup. Comparison radiographs of the contralateral calcaneum and postoperative CT scans were not performed on all patients and residual articular displacement is difficult to determine on plain radiographs.
The surgical technique of MIRF of calcaneal fractures is technically demanding and has an extensive learning curve for surgeons who have significant experience in treating calcaneal fractures with traditional extensile open surgery. The fracture subgroups that would benefit most from MIRF remains unknown and needs further robust research. Minimally invasive calcaneal fracture surgery has many benefits in those patients where hindfoot morphology should be improved. The subgroup of patients where traditional extensile open surgery poses significant risk can be helped by this less invasive technique.
To the best of our knowledge, a MIRF technique with the use of threaded K wires has not been previously described in the literature. In our experience, the operative time is short and can be safely performed even in the presence of extensive soft tissue swelling in the immediate period following injury. The infection risk is low and calcaneal morphology was improved and maintained in terms of Böhler’s angle. This technique is suitable to be considered in patients who have significant medical co-morbidities (smokers, diabetics, peripheral vascular disease) and in those patients who are not suitable for an extensile lateral approach and internal fixation. However, the long-term outcome of subtalar arthrosis using this technique remains unknown.
Acknowledgments
No funds were received in support of this work.
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Buckley R, Tough S, McCormack R, Pate G, Leighton R, Petrie D, Galpin R. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84-A(10):1733–1744. doi: 10.2106/00004623-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Benirschke SK, Kramer PA. Wound healing complications in closed and open calcaneal fractures. J Orthop Trauma. 2004;18(1):1–6. doi: 10.1097/00005131-200401000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 2000;82(2):225–250. doi: 10.2106/00004623-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Brauer CA, Manns BJ, Ko M, Donaldson C, Buckley R. An economic evaluation of operative compared with nonoperative management of displaced intra-articular calcaneal fractures. J Bone Joint Surg Am. 2005;87(12):2741–2749. doi: 10.2106/JBJS.E.00166. [DOI] [PubMed] [Google Scholar]
- 5.Stein H, Rosen N, Lerner A, Kaufman H. Minimally invasive surgical techniques for the reconstruction of calcaneal fractures. Orthopedics. 2003;26(10):1053–1056. doi: 10.3928/0147-7447-20031001-15. [DOI] [PubMed] [Google Scholar]
- 6.Hammond AW, Crist BD. Percutaneous treatment of high-risk patients with intra-articular calcaneus fractures: A case series. Injury. 2013 doi: 10.1016/j.injury.2013.01.033. [DOI] [PubMed] [Google Scholar]
- 7.Stulik J, Stehlik J, Rysavy M, Wozniak A. Minimally-invasive treatment of intra-articular fractures of the calcaneum. J Bone Joint Surg Br. 2006;88(12):1634–1641. doi: 10.1302/0301-620X.88B12.17379. [DOI] [PubMed] [Google Scholar]
- 8.Abdelgaid SM. Closed reduction and percutaneous cannulated screws fixation of displaced intra-articular calcaneus fractures. Foot Ankle Surg. 2012;18(3):164–179. doi: 10.1016/j.fas.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 9.DeWall M, Henderson CE, McKinley TO, Phelps T, Dolan L, Marsh JL. Percutaneous reduction and fixation of displaced intra-articular calcaneus fractures. J Orthop Trauma. 2010;24(8):466–472. doi: 10.1097/BOT.0b013e3181defd74. [DOI] [PubMed] [Google Scholar]
- 10.Rammelt S, Amlang M, Barthel S, Gavlik JM, Zwipp H. Percutaneous treatment of less severe intraarticular calcaneal fractures. Clin Orthop Relat Res. 2010;468(4):983–990. doi: 10.1007/s11999-009-0964-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schepers T, Schipper IB, Vogels LM, Ginai AZ, Mulder PG, Heetveld MJ, Patka P. Percutaneous treatment of displaced intra-articular calcaneal fractures. J Orthop Sci. 2007;12(1):22–27. doi: 10.1007/s00776-006-1076-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walde TA, Sauer B, Degreif J, Walde HJ. Closed reduction and percutaneous Kirschner wire fixation for the treatment of dislocated calcaneal fractures: surgical technique, complications, clinical and radiological results after 2-10 years. Arch Orthop Trauma Surg. 2008;128(6):585–591. doi: 10.1007/s00402-008-0590-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacquot F, Letellier T, Atchabahian A, Doursounian L, Feron JM. Balloon reduction and cement fixation in calcaneal articular fractures: a five-year experience. Int Orthop. 2013;37(5):905–910. doi: 10.1007/s00264-013-1865-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schepers T, van Lieshout EM, van Ginhoven TM, Heetveld MJ, Patka P. Current concepts in the treatment of intra-articular calcaneal fractures: results of a nationwide survey. Int Orthop. 2008;32(5):711–715. doi: 10.1007/s00264-007-0385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Essex-Lopresti P. The mechanism, reduction technique, and results in fractures of the os calcis. Br J Surg. 1952;39(157):395–419. doi: 10.1002/bjs.18003915704. [DOI] [PubMed] [Google Scholar]
- 16.Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;290:87–95. [PubMed] [Google Scholar]
- 17.Broden B. Roentgen examination of the subtaloid joint in fractures of the calcaneus. Acta Radiol. 1949;31(1):85–91. doi: 10.3109/00016924909136638. [DOI] [PubMed] [Google Scholar]
- 18.Tornetta P., 3rd Percutaneous treatment of calcaneal fractures. Clin Orthop Relat Res. 2000;375:91–96. doi: 10.1097/00003086-200006000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Clark LG. Fracture of the os calcis. Lancet. 1855;65:403–404. doi: 10.1016/S0140-6736(02)61561-2. [DOI] [Google Scholar]
- 20.Zhang J, Xiao B, Wu Z. Surgical treatment of calcaneal fractures with bioabsorbable screws. Int Orthop. 2011;35(4):529–533. doi: 10.1007/s00264-010-1183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Magnan B, Bortolazzi R, Marangon A, Marino M, Dall’Oca C, Bartolozzi P. External fixation for displaced intra-articular fractures of the calcaneum. J Bone Joint Surg Br. 2006;88(11):1474–1479. doi: 10.1302/0301-620X.88B11.17759. [DOI] [PubMed] [Google Scholar]
- 22.Schildhauer TA, Sangeorzan BJ. Push screw for indirect reduction of severe joint depression-type calcaneal fractures. J Orthop Trauma. 2002;16(6):422–424. doi: 10.1097/00005131-200207000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Burdeaux BD., Jr Historical and current treatment of calcaneal fractures. J Bone Joint Surg Am. 2001;83-A(9):1438–1440. doi: 10.2106/00004623-200109000-00041. [DOI] [PubMed] [Google Scholar]
- 24.Levine DS, Helfet DL. An introduction to the minimally invasive osteosynthesis of intra-articular calcaneal fractures. Injury. 2001;32(Suppl 1):SA51–SA54. doi: 10.1016/S0020-1383(01)00061-4. [DOI] [PubMed] [Google Scholar]
- 25.Loucks C, Buckley R. Bohler’s angle: correlation with outcome in displaced intra-articular calcaneal fractures. J Orthop Trauma. 1999;13(8):554–558. doi: 10.1097/00005131-199911000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Longino D, Buckley RE. Bone graft in the operative treatment of displaced intraarticular calcaneal fractures: is it helpful? J Orthop Trauma. 2001;15(4):280–286. doi: 10.1097/00005131-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Bakker B, Halm JA, Van Lieshout EM, Schepers T. The fate of Bohler’s angle in conservatively-treated displaced intra-articular calcaneal fractures. Int Orthop. 2012;36(12):2495–2499. doi: 10.1007/s00264-012-1706-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Demcoe AR, Verhulsdonk M, Buckley RE. Complications when using threaded K-wire fixation for displaced intra-articular calcaneal fractures. Injury. 2009;40(12):1297–1301. doi: 10.1016/j.injury.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 29.Chen L, Zhang G, Hong J, Lu X, Yuan W. Comparison of percutaneous screw fixation and calcium sulfate cement grafting versus open treatment of displaced intra-articular calcaneal fractures. Foot Ankle Int. 2011;32(10):979–985. doi: 10.3113/FAI.2011.0979. [DOI] [PubMed] [Google Scholar]