Abstract
Purpose
Osteosarcoma (OS) is a serious disease affecting mainly children and young adults. In a resource poor setting the treatment options are limited and further obstacles can be found with respect to late presenting pathology, access to modern treatment modalities such as effective chemotherapy, and cultural reluctance to undergo certain treatments. Clinical outcome studies and epidemiology for this disease in developing countries are scarce.
Methods
We report on the outcomes of 30 patients treated by the CSC, a rehabilitative surgery centre in Cambodia, from 2002 to present. Enneking staging, location, and treatment protocols were evaluated. Outcome measures were months of survival, EDQ5S life quality scores and clinically relevant inquiries. Kaplan-Meier analysis estimates and the Wilcoxon chi-square test were used for statistical inferences.
Results
We find a grim prognosis for patients diagnosed with OS in Cambodia, 53 % survive the first year after presentation and the five-year survival stands at 8 %. There is a higher mean age for presentation of OS compared to Western norms, namely, 18.8 years and 21.7 years for females and males, respectively.
Conclusions
Most patients opted for surgical treatment without adjuvant chemotherapy, which is not within the means of many Cambodian patients. Acceptance of amputation, earlier diagnosis, patient education, and access to standardized chemotherapy needs to be enhanced if Cambodian patients are to have a fighting chance.
Keywords: Osteosarcoma, Sarcoma, Cancer, Orthopaedics, Amputation, Limb salvage, Resource poor setting, Oncology, Epidemiology
Introduction
Osteosarcoma (OS), alternatively known as osteogenic sarcoma, is a diagnosis resulting in a battle of life and limb for any patient, regardless of the health care setting they are in. Unfortunately, since the advent of multi-agent chemotherapy in the 1970s, little further improvement in this battle has been made in improving overall prognosis of OS. Studies on prognosis of OS are rare in developing countries. Treatment options are very limited in resource poor settings and there is far less access to the more advanced treatment pathways available in a developed healthcare system [1–4].
Cambodia is one of the poorer and more underdeveloped countries in South-Eastern Asia, according to standardized developmental indices [5]. The Children’s Surgical Centre (CSC; www.csc.org), situated in the Kien Khleang Rehabilitative Centre in the capital city, Phnom Penh, is an NGO offering free rehabilitative surgery to those in need. Over the last 12 years, the CSC has had an increasing number of patients presenting with osteosarcoma. Patients will often present with neglected and advanced pathology, causing treatment for such conditions to be even more challenging. Traditional medicine still has a strong role in the rural areas of Cambodia and there is a cultural resistance to the idea of amputation. Furthermore, access to chemotherapy is both limited and expensive with currently only one centre in Phnom Penh, the Khmer Russian Friendship Hospital, offering treatment at a cost. This study aims to highlight the outcomes of those patients treated at the CSC with osteosarcoma and the challenges faced in such a setting.
The most common malignancy of primary bone tissue is OS [2, 6]. It is a relatively rare disease with estimated incidence of four million cases a year worldwide, but it is the eighth most common malignancy of childhood, and accounts for 20 % of mortality in children due to malignancy in the developed world [6]. The peak incidence of OS is in children and adolescents in the second decade of life with a second smaller peak in incidence in the seventh or eighth decade of life [7, 8].
Historically, OS prognosis has indeed been grim, with only 5 % survival in the older studies. With the ascent of multi-agent chemotherapy in the 1980s, the survival increased dramatically; unfortunately the survival has not improved much in the decades since [1]. The current standard for OS chemotherapy includes a combination of doxyrubicin, cisplatin, methotrexate with leukovorin-rescue factor, and ifosfamide [9, 10]. The use of neoadjuvant chemotherapy has been shown to induce tumour necrosis of OS, thus improving survival [11]. Furthermore, neoadjuvant chemotherapy has been shown to reduce the margin of surgical excision required, perhaps making surgery less difficult and preserving healthy tissue [12].
Data on OS-treatment in developing resource-poor countries is scarce [3]. A nine-year review of the survival rates of OS in a tertiary hospital in neighbouring Thailand showed somewhat lower survival than what was to be expected from comparable treatment in Europe [13]. Another study measured five-year survival rates to be about half of what US studies have found [4, 7]. We believe this is the first outcome-based study of its kind in Cambodia.
Materials and methods
Patients
The electronic database of the CSC was retrospectively searched for multiple keywords, including osteosarcoma, osteogenic sarcoma, bone cancer, bone malignancy, bone sarcoma, sarcoma and cancer, until a definitive list of all bone cancers in the system treated since 2002 was collected. Paper records with the same criteria were then searched. After analysing each case, including available patient histories, radiographs and pathology reports, only patients with a confirmed histopathology report of osteosarcoma and/or a convincing radiograph of the disease, were included in the study. Those patients whose records were missing or incomplete were omitted from the study.
Contacting patients
Some patients were followed up by regular consultation in the clinic. However, for those patients lost to follow up, or in whom the outcomes were not known, telephonic contact was tried, and when possible, the patient was requested to re-visit the CSC. For those patients whose correct contact details were unavailable, attempts were made to visit the often remote village of the patient in order to successfully ascertain the outcome.
Measurements
Enneking stage
The Enneking staging at admission was used to evaluate prognosis where possible. It is a well recognized staging system for OS and other musculoskeletal tumours [14–16]. The CSC does not routinely have access to CT imaging and thus distant metastases were based on clinical examination, ultrasound exam of the abdomen, and plain radiographs of the chest.
Quality of life
The EQ5D is a European standardized quality of life (QoL) measurement tool, often used to assess QoL in surgical patients [17, 18]. The EQ5D was chosen because of its standardized content, peer reviewed publication frequency and simplistic questions that readily translate from English to Cambodian without apparent need for standardization. The questionnaire was submitted to all surviving and contacted patients. Written permission was obtained from EuroQol to use the score in this study (permission received 11.2.2013, second author).
Treatment
Treatment was defined simply as surgery, in the form of amputation or limb salvage, as well chemotherapy, radiotherapy or patient’s refusal of treatment.
Survival
Survival rates were calculated in months from the date of presentation to CSC, to the date of death or the date of last follow up. Survival rates as ratios were calculated from censored data. Kaplan-Maier survival analysis was implemented for all patients and for patients sorted by three treatment paradigms: no treatment, surgical resection only and chemotherapy with or without surgical resection. The chi-square test was used in survival analysis. Statistics were calculated using R.
Other inquiries
Patients and families were asked about a number of clinically relevant factors regarding treatment at the CSC. These included where the patient died, the time the patient was in significant pain, whether health care professionals at CSC had explained the condition and prognosis adequately, and what their feelings were towards the treatment offered by the CSC.
Results
Forty-four patients were initially identified via the computer database search. On further review, seven patients had insufficient information documented to ascertain the correct diagnosis either radiologically or histologically whilst another seven patients had a confirmed histological diagnosis other than osteosarcoma.
Demographics
Thirty patients met the inclusion criteria, eight of whom were female (27 %) and 22 (73 %) were male. The mean age at presentation was 20.9 years, ranging from five to 47 years old at presentation. The mean age for females was 18.8 years and 21.7 years for males.
Table 1 highlights the sites of tumour origin with the distal femur being the most common site (47 %) followed by proximal tibia (37 %).
Table 1.
Sites and frequency of tumors in this dataset
| Site of tumour origin | Number of patients |
|---|---|
| Distal femur | 14 |
| Proximal tibia | 11 |
| Proximal humerus | 2 |
| Midshaft humerus | 1 |
| Distal radius | 1 |
| Ethmoid | 1 |
All tumours were extra compartmental on presentation, with examples displayed in Fig. 1. Twelve patients had confirmed histological reports of high grade tumours, two had reports of low grade osteosarcomas. The remaining pathology reports did not specify the grade of the tumour. Only three patients had clear signs of lung metastases on a plain chest radiograph. No patient had any further investigations for metastases once one was recognised on a chest X-ray.
Fig. 1.
Three examples of late presenting osteosarcoma tumours to the centre
Treatments
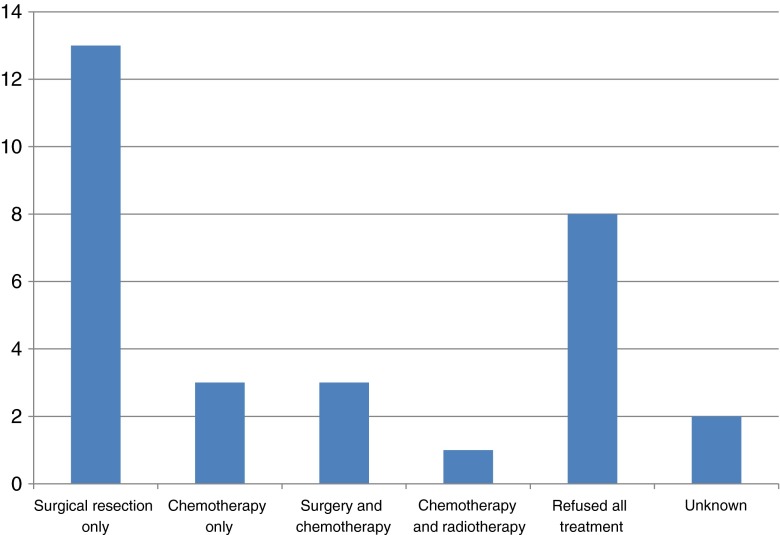
Figure 2 highlights the treatments undergone by the patients. Sixteen patients had surgical resection of the tumour with no adjuvant treatment, either because it was not available, not affordable, or not acceptable. Fifteen of these were in the form of amputations (sometimes for pathological fractures through the tumour), whilst one was a surgical resection with a limb salvage procedure. Eight patients refused treatment altogether, three patients had surgery along with chemotherapy whilst three patients had chemotherapy alone. One patient had chemotherapy and radiotherapy but no surgery. Two patients had biopsies confirming osteosarcoma but all treatment records were lost and the patients were uncontactable thereafter.
Fig. 2.
Treatments received by the patients
Outcomes
At the time of the study, seven patients treated remained alive, 20 were deceased and three were not contactable and their survival was unknown. Of the seven current survivors, only two patients have progressed beyond one year of treatment, surviving 28 months and 88 months respectively. Mean survival was 14.1 months for all patients.
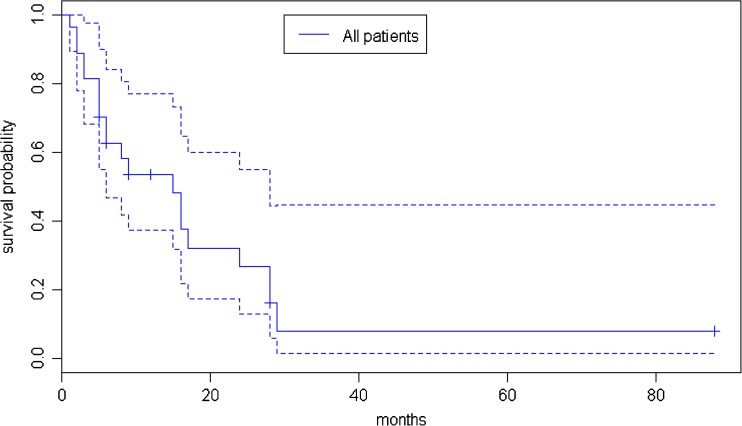
Table 2 and Fig. 3 display the survival rates from six months to three years. The current survivors who had not yet reached the follow-up milestones in the table were omitted from further mortality rate calculations. The overall mortality rate at one year was 52 %. Two of the three patients who had clear chest metastases died at one month and three months post diagnosis (both of whom had amputations of the limb). The third patient refused surgery but completed a course of chemotherapy and is now nine months post diagnosis. From follow up, we understand the patient is now becoming unwell at home.
Table 2.
Overall survival rates of all patients with osteosarcoma
| Timeframe | Number of patients | Mortality rate as percentage |
|---|---|---|
| Mortality within six months | 10 out of 27 | 37 % |
| Mortality within 12 months | 12 out of 23 | 52 % |
| Mortality within 18 months | 16 out of 22 | 73 % |
| Mortality within 24 months | 17 out of 22 | 77 % |
| Mortality within 36 months | 20 out of 21 | 95 % |
Fig. 3.
Kaplan-Maier survival curve of all patients presented with 95 % confidence interval. Dotted lines indicate the 95 % confidence interval. Right-truncated censorship of survival are marked with a cross-mark on the curve
All patients who received only surgery, except one, died within three years, with the only survivor in this only surgery group being a 25-year-old male with a low grade osteosarcoma of his distal femur who underwent a limb salvage procedure. He is now 28 months post operation. Table 3 highlights the outcomes of those patients undergoing surgical resection only.
Table 3.
Overall survival rates of all patients who received a surgical resection only
| Timeframe | Number of patients | Mortality rate as percentage |
|---|---|---|
| Mortality within six months | 5 out of 12 | 42 % |
| Mortality within 12 months | 6 out of 12 | 50 % |
| Mortality within 18 months | 8 out of 12 | 67 % |
| Mortality within 24 months | 9 out of 12 | 75 % |
| Mortality within 36 months | 11 out of 11 | 100 % |
One patient who had an amputation has an unknown outcome. The only survivor is 28 months post surgery
Only seven patients in total received chemotherapy treatment, either as the sole means of treatment, or in conjunction with surgery, or in one case, radiotherapy. Table 4 shows an overall trend of much higher survival rates.
Table 4.
Overall survival rates of all patients who received chemotherapy within their overall treatment
| Timeframe | Number of patients | Mortality rate as percentage |
|---|---|---|
| Mortality within six months | 0 out of 7 | 0 % |
| Mortality within 12 months | 1 out of 5 | 20 % |
| Mortality within 18 months | 3 out of 4 | 75 % |
| Mortality within 24 months | 3 out of 4 | 75 % |
| Mortality within 36 months | 3 out of 4 | 75 % |
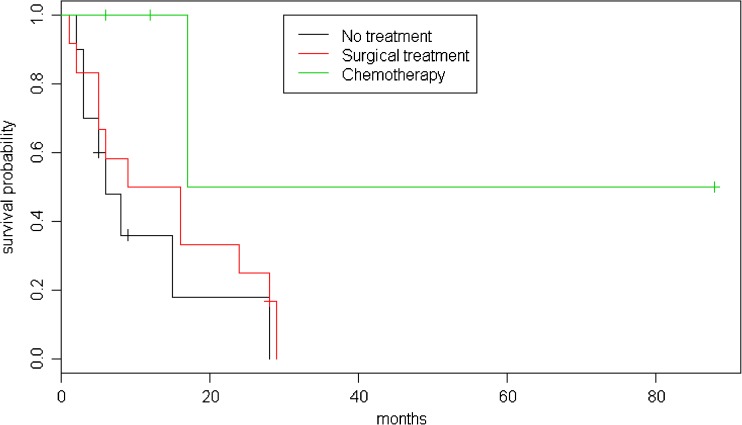
Comparison of the surgical group and the overall group revealed no statistically significant difference between the groups (Fig. 4). The only patient to survive more than three years in this dataset had no surgery but radiotherapy and chemotherapy, and when his data was omitted the surgery group seemed to fare slightly better than others, whereby the chi-square statistic was 1.5 and p-value was 0.225.
Fig. 4.
Kaplan-Maier survival curve factoring treatment options
Social outcomes
Of the seven patients currently still alive, from the EQ5D questionnaire four reported on-going problems with their mobility. Two reported difficulties in self care and two reported on-going problems with pain. Five patients reported elements of anxiety and depression associated with their disease. From the visual analogue score of “overall perceived health” (100 representing “feel completely healthy”, 0 representing a “worst imaginable health state”), the overall score from the current survivors was 57.
Of the 20 deceased patients, all died at home. Upon questioning the families, the patients were in a significant amount of pain for an average of two weeks prior to death. Relatives of two patients felt they had not been fully informed about the diagnosis or the prognosis of the patient, whilst the remainder felt they were told and understood the patient died of cancer. Most families expressed gratitude and acceptance of the treatment offered by the CSC and were grateful for the service. A full qualitative analysis for the rationale of the families’ treatment decisions was not explored due to the difficult nature of the interviews.
Discussion
Our results highlight the extreme difficulties in treating osteosarcoma with a combination of advanced pathology, poor access to investigative modalities, cultural reluctance to comply with Western treatment, limited access to adjuvant therapy, and lack of modern surgical limb salvage techniques.
Prior to chemotherapy, an analysis of 430 patients in 1957 [19] suggested an overall 19.3 % five-year survival rate and prior to that, at the turn of the 20th century, a 5 % survival rate [1]. Of all the 27 patients currently followed up in this study, only one patient has lived beyond five years. Survival estimates in Cambodia are thus 53.6 % at 12 months from presentation, 16.1 % at three years and 8 % at five years. Those patients receiving just an amputation fared only slightly better than the overall group. Thus the current figures are more comparable to outcomes in the early 20th century than the early 21st century.
Chemotherapy has only recently become more readily available in Cambodia with only seven of the patients thus far having this mode of treatment. Although difficult to compare with such a small sample (and many of the patients only having had chemotherapy within the last year), it appears that chemotherapy may have some life prolonging results in this subgroup. Funding for chemotherapy is economically challenging for many patients, thus making it a difficult treatment option regardless of the perceived clinical benefit and risks.
Eight patients refused treatment altogether, highlighting another difficulty in treating patients within Cambodia, as both the cultural and social stigma of an amputation often result in patients preferring the poor prognosis of their tumour, or putting their faith once more into traditional medicine.
Although this study attempted to find the current outcomes of patients with osteosarcoma in Cambodia, following up patients for a prolonged period of time proved to be difficult. Patients are often from remote villages and even up-to-date phone contact details can become obsolete within a matter of months, as mobile phones are often abandoned or changed. A considerable and concerted effort was made to identify these patients many years after treatment, often resulting in long journeys in person to find the outcome of the patient.
Further difficulties in the study include confirming accurate diagnosis, with pathological services in Cambodia being inaccurate and limited until more recent times; previously, biopsy samples were transported abroad to obtain a diagnosis. Incomplete records preventing clear confirmation of a diagnosis of osteosarcoma meant a further seven patients were omitted from the study as previous X-rays and histology reports had become lost.
Conclusion
This study highlights the urgent need to update the approach to osteosarcoma within Cambodia, with a more streamlined approach to patient education, diagnosis, treatment pathways, standardized effective chemotherapy regimens and follow-up care, in order that Cambodia can move this battle with osteosarcoma into the 21st century, and life can be saved, even at the cost of a limb.
Acknowledgments
Competing interests
Authors state no apparent competing interests. CSC is an NGO and funded by charity.
Abbreviations
- OS
Osteosarcoma
- CSC
Children's Surgical Centre
- SD
Standard deviation
- NGO
Non-governmental organization
Contributor Information
Saqib Noor, Email: saqqqqq@gmail.com.
Hjörleifur Skorri Þormóðsson, Email: hjolliskorri@gmail.com.
Colin Thomas Zervas, Email: czervas@gmail.com.
Tho Ly, Email: ly@csc.org.
James Gollogly, Email: jim@csc.org.
References
- 1.Allison DC, Carney SC, Ahlmann ER, Hendifar A, Chawla S, Fedenko A, Angeles C, et al. A meta-analysis of osteosarcoma outcomes in the modern medical era. Sarcoma. 2012;2012:704872. doi: 10.1155/2012/704872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Broadhead ML, Clark JCM, Myers DE, Dass CR, Choong PFM. The molecular pathogenesis of osteosarcoma: a review. Sarcoma. 2011;2011:959248. doi: 10.1155/2011/959248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jain K, Sunila, Ravishankar R, Mruthyunjaya, Rupakumar CS, Gadiyar HB, Manjunath GV. Bone tumors in a tertiary care hospital of south India: a review 117 cases. Indian J Med Paediatr Oncol Off J Indian Soc Med Paediatr Oncol. 2011;32(2):82–85. doi: 10.4103/0971-5851.89778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiromrat P, Jetsrisuparb A, Komvilaisak P, Sirichativapee W, Kamsa-Ard S, Wiangnon S. Incidence and survival rates among pediatric osteogenic sarcoma cases in Khon Kaen, Thailand, 1985–2010. Asian Pac J Cancer Prev APJCP. 2012;13(9):4281–4284. doi: 10.7314/APJCP.2012.13.9.4281. [DOI] [PubMed] [Google Scholar]
- 5.Malik K, Kugler M, Kovacevic M, Bhattacharjee, Subhra Bonin A, Calderón C, Fuchs A, Gaye A et al. (2013) The rise of the south: human progress in a diverse world. Human Developmental Report 2013. United Nations Developmental Programme, New York
- 6.PosthumaDeBoer J, Witlox MA, Kaspers GJL, Van Royen BJ. Molecular alterations as target for therapy in metastatic osteosarcoma: a review of literature. Clin Exp Metastasis. 2011;28(5):493–503. doi: 10.1007/s10585-011-9384-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mirabello L, Troisi RJ, Savage SA. Osteosarcoma incidence and survival rates from 1973 to 2004: data from surveillance, epidemiology, and end results program. Cancer. 2009;115(7):1531–1543. doi: 10.1002/cncr.24121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Savage SA, Mirabello L. Using epidemiology and genomics to understand osteosarcoma etiology. Sarcoma. 2011;2011:548151. doi: 10.1155/2011/548151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ritter J, Bielack SS. Osteosarcoma. Ann Oncol Off J Eur Soc Med Oncol ESMO. 2010;21(Suppl 7):vii320–vii325. doi: 10.1093/annonc/mdq276. [DOI] [PubMed] [Google Scholar]
- 10.Windsor RE, Strauss SJ, Kallis C, Wood NE, Whelan JS. Germline genetic polymorphisms may influence chemotherapy response and disease outcome in osteosarcoma: a pilot study. Cancer. 2012;118(7):1856–1867. doi: 10.1002/cncr.26472. [DOI] [PubMed] [Google Scholar]
- 11.Li X, Ashana AO, Moretti VM, Lackman RDX. The relationship of tumour necrosis and survival in patients with osteosarcoma. Int Orthop. 2011;35(12):1847–1853. doi: 10.1007/s00264-011-1209-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li X, Moretti VM, Ashana AO, Lackman RD. Impact of close surgical margin on local recurrence and survival in ostesarcoma. Int Orthop. 2012;36(1):131–137. doi: 10.1007/s00264-011-1230-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choeyprasert W, Natesirinilkul R, Charoenkwan P, Sittipreechacharn S. Carboplatin and doxorubicin in treatment of pediatric osteosarcoma: a 9-year single institute experience in the Northern Region of Thailand. Asian Pac J Cancer Prev APJCP. 2013;14(2):1101–1106. doi: 10.7314/APJCP.2013.14.2.1101. [DOI] [PubMed] [Google Scholar]
- 14.Jawad MU, Scully SP. In brief: classifications in brief: enneking classification: benign and malignant tumors of the musculoskeletal system. Clin Orthop Relat Res. 2010;468(7):2000–2002. doi: 10.1007/s11999-010-1315-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lu B-J, Wang Y-Q, Wei X-J, Rong L-Q, Wei D, Yan C-M, Wang D-J, et al. Expression of WNT-5a and ROR2 correlates with disease severity in osteosarcoma. Mol Med Rep. 2012;5(4):1033–1036. doi: 10.3892/mmr.2012.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yuan J, Chen L, Chen X, Sun W, Zhou X. Identification of serum microRNA-21 as a biomarker for chemosensitivity and prognosis in human osteosarcoma. J Int Med Res. 2012;40(6):2090–2097. doi: 10.1177/030006051204000606. [DOI] [PubMed] [Google Scholar]
- 17.Andersson J, Angenete E, Gellerstedt M, Angerås U, Jess P, Rosenberg J, Fürst A, et al. Health-related quality of life after laparoscopic and open surgery for rectal cancer in a randomized trial. Br J Surg. 2013;100(7):941–949. doi: 10.1002/bjs.9144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee BH, Park J-O, Suk K-S, Kim T-H, Lee H-M, Park M-S, Lee S-H, et al. Pre-emptive and multi-modal perioperative pain management may improve quality of life in patients undergoing spinal surgery. Pain Physician. 2013;16(3):E217–E226. [PubMed] [Google Scholar]
- 19.Coventry M, Dahlin D. Osteogenic sarcoma: a critical analysis of 430 cases. J Bone Joint Surg. 1957;39(4):741–758. [PubMed] [Google Scholar]