Abstract
Purpose
The purpose of this study was to prove the hypothesis that soft tissues are well balanced using the gap technique with a navigation system in cruciate-retaining (CR) and posterior-stabilised (PS) total knee arthroplasty (TKA), leading to better clinical outcomes compared with the measured-resection technique.
Methods
One hundred and thirty-five TKAs (90 CR and 45 PS) were performed in patients with varus-type osteoarthritis using the gap technique guided by the offset-type tensor and a navigation system. Soft-tissue balance (joint-component gap and ligament balance) were intraoperatively assessed with the tensor under 40 lb of joint-distraction force. The achievement in the equalised rectangular gap at extension and flexion was assessed and retrospectively compared with the previous series in which the measured-resection technique was used (20 CR and 100 PS TKAs). In addition, clinical outcomes, including range of motion and Knee Society Score were assessed at a minimum two year follow-up.
Results
In achieving equalised rectangular gaps at extension and flexion, CR TKAs met criteria in more cases [66.7 % (64/90) vs. 44.4 % (20/45) of PS TKA] with the gap technique, which was superior to that with the measured-resection technique [50.0 % (10/20) of CR TKA and 28.0 % (28/100) of PS TKA]. However, clinical outcomes showed no significant differences among groups at minimum two year follow-up.
Conclusions
The superiority of CR TKA with the gap technique in achieving equalised rectangular gaps at extension and flexion does not directly reflect two year postoperative clinical outcomes.
Keywords: Total knee arthroplasty, Soft-tissue balance, Gap technique, Patellofemoral joint, Cruciate-retaining, Posterior-stabilised, Navigation system
Introduction
Appropriate soft-tissue balancing and accurate bony alignment are essential in total knee arthroplasty (TKA). Despite advanced accuracy in bony alignment achieved with the development of surgical instruments, such as the computer-assisted navigation system and various surgical jigs, obtaining an accurate intra-operative soft-tissue balance remains difficult, especially for young surgeons, as experienced surgeons traditionally address soft-tissue balance through “subjective feel”. Therefore, an offset-type tensor has been developed for use during TKA, which enables soft-tissue balance assessment throughout range of motion (ROM) in the physiological knee after TKA, with a reduced patellofemoral (PF) joint and femoral component in place [1]. This tensor permits intra-operative reproduction and postoperative alignment of the PF and tibiofemoral joints. This tensor design, initial intraoperative soft-tissue-balance measurement and its clinical relevance in TKA have been described previously [2–7]. In those studies, soft-tissue-balance measurements were performed using only the measured-resection technique. However, the best method for obtaining appropriate soft-tissue balance and rotational alignment of the femur remains controversial, with dispute focusing on the measured-resection and gap techniques [8–11]. Some investigators favour a measured-resection technique, in which bony landmarks (femoral epicondyles, posterior femoral condyles, anteroposterior axis) are the primary determinants of femoral-component rotation [8, 11–15]. However, others recommend a gap-balancing methodology, in which the femoral component is positioned parallel to the resected proximal tibia, with each collateral ligament equally tensioned [9, 10, 16]. In previous studies using the measured-resection technique, the pattern of soft-tissue balance differed between cruciate-retaining (CR) and posterior-stabilised (PS) TKA [3, 4]. Therefore, in our study, we applied the tensor using the gap technique, with a navigation system for soft-tissue balancing in 135 knees receiving CR or PS TKA based on the status of the posterior cruciate ligament (PCL). The hypothesis of the study was that soft-tissue balancing using the gap technique is superior to that using measured resection in terms of acquiring an equalised rectangular gap at extension and flexion. The first purpose of the study was to verify that hypothesis, and the second purpose was to investigate whether superiority in soft-tissue balancing is reflected in clinical outcome at a minimum 2-year follow-up.
Materials and methods
Inclusion criteria were substantial pain and loss of function due to osteoarthritis of the knee. In addition to the knee condition, patients who agreed to participate in the study also agreed to be followed up for greater than two years postoperatively. The exclusion criteria included knees with valgus deformity, severe bony defect requiring bone graft or augmentation, revision TKA and active knee-joint infection. Between 2008 and 2010, according to PCL condition, 90 knees (80 patients; 70 women, ten men) from a group of 135 knees met the above criteria for CR (e-motion; B. Braun Aesculap, Germany); the other 45 knees (40 patients; 36 women, four men) were assigned to PS (e-motion; B. Braun Aesculap). In all patients, a computed tomography (CT)–free navigation system (Orthopilot 4.2; B. Braun Aesculap) and offset-type tensor were used to assist in the gap technique [17]. Each surgery was performed by the two senior authors, who each have greater than ten years of experience performing TKA. The patients who underwent CR had a mean age of 74.5 (range, 58–86) years, and those who underwent PS had a mean age of 74.9 (range, 59–88) years; mean ages of the two groups were not significantly different. Preoperative coronal alignment was 10.9° ± 0.5° varus in the CR group and 9.5° ± 1.1° varus in the PS group, indicating no significant differences. Pre-operative ROM was −5.4°(range, 0°– 20°) in extension and 120.1°(range, 95°–135°) in flexion in the CR group and −9.8°(range, 0°–25°) in extension and 115.4°(range, 95°–130°) in flexion in the PS group, indicating no significant difference in pre-operative ROM in flexion and extension between groups.
Controls comprised 120 patients who underwent TKA between 2005 and 2007 with the measured-resection technique. Twenty knees (16 patients; 14 women, two men) received CR (NexGen CR Flex; Zimmer, Inc., Warsaw, IN, USA) and the other 100 knees (88 patients; 81 women, seven men) received PS (NexGen LPS Flex; Zimmer, Inc.). Patients who underwent CR had a mean age of 73.4 (range, 57–87) years, and those who underwent PS had a mean age of 74.1 (range, 60–86) years. Thus no significant difference with regard to age was observed between groups. Pre-operative coronal alignment was 9.6° ± 1.2° varus in the CR group and 11° ± 0.8° varus in the PS group, with no significant difference. Preoperative ROM was −7.9°(range, 0°–20°) in extension and 122.3°(range, 100°–135°) in flexion in the CR group, and −10.1°(range, 0°–25°) in extension and 116.2°(range, 95°–130°) in flexion in the PS group, with no significant difference.
Offset-type TKA tensor
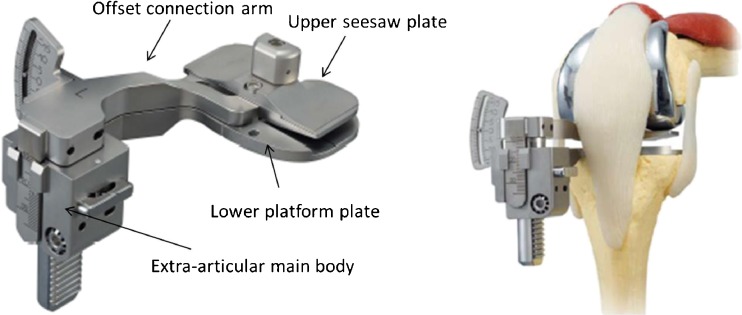
As previously described [2–4, 7], the tensor consists of three parts: an upper seesaw plate, a lower platform plate with a spike, and an extra-articular main body (Fig. 1). Following bony resection and soft-tissue release, we place the tensor, with the lower platform fixed to the proximal tibia. Even if the femoral condyle is not resected, the upper seesaw plate can be fitted to the femoral condyle or femoral prosthesis. After the PF joint is reduced, the medial parapatellar arthrotomy is repaired temporarily by applying stitches both proximally and distally to the connection arm of the tensor (Fig. 1). These mechanisms permit us to reproduce joint constraint. This device is ultimately designed to allow surgeons to measure the joint-centre gap (joint-component gap) and ligament balance (varus angle) while applying a constant joint-distraction force. Joint-distraction forces ranging from 20 lb (4.5 kg) to 80 lb (36.3 kg) can be exerted between the seesaw and platform plates through a specially made torque driver, which can change the applied torque value. After sterilisation, this torque driver is placed on a rack containing a pinion mechanism along the extra-articular main body, and the appropriate torque is applied to generate the designated distraction force; in preliminary in vitro experiments, we obtained an error for joint distraction within ± 3 %. Once appropriately distracted, attention is focused on a scale that corresponds to the tensor: the angle [degree, positive value in varus ligament balance (varus angle)] between the seesaw and platform plates, as well as the distance (mm) (joint centre/component gap) between the centre midpoints of the upper surface of the seesaw plate and the proximal tibial cut. By measuring these angular deviations and distances under a constant joint-distraction force, we are able to measure ligament balance and joint-centre gaps.
Fig. 1.
Offset-type tensor. The tensor consists of three parts: upper seesaw plate, to which a shaped insert can be attached; a lower platform plate; an extra-articular main body. Two plates are connected to the extra-articular main body by the offset connection arm through a medial parapatellar arthrotomy, which permits reduction of the patellofemoral (PF) joint while performing measurements
Operative procedure and intra-operative measurement
Preoperative coronal and sagittal long-leg radiographs were taken and used to select the appropriately sized femoral and tibial prostheses and determine the appropriate level and angle of osteotomies in relation to mechanical axes. An epicondylar radiograph and CT scan were taken to reference the original transepicondylar and posterior condylar axes and preoperatively identify osteophytes in the intercondylar notch for selecting the appropriate implant type (CR or PS).
First, we performed a stable bicortical fixation using self-cutting screws through femoral and tibial stab incisions. After inflating the air tourniquet to 280 mmHg, a medial parapatellar arthrotomy was performed. For kinematic referencing, detecting the kinematic centre of the hip, knee and ankle joints was performed with controlled movement. To register anatomical landmarks, the medial plateau, lateral plateau, eminence of the tibia, medial posterior condyle, lateral posterior condyle and anterior cortex of the femur were recorded. Surgery was performed with the tibia-first gap technique using the navigation system [17, 18], which leads to accurate bone cut and ROM measurement. Following the procedure, a tibial osteotomy was performed perpendicular to the tibial axis in the coronal and sagittal planes, according to the planned resection height and angle on the navigation system. For knees with a functional PCL, assessed by intraoperative findings, preoperative epicondylar radiograph and CT scan of intercondylar osteophytes, PCL insertion was preserved by a bony island. When it appeared that the PCL was not functional, the PCL was resected. After the tibial osteotomy, necessary removal of osteophytes and release of medial ligaments were performed in extension. At this point, appropriate step-by-step release of medial soft-tissue (posteromedial capsule, medial collateral ligament, semimembranosus muscle, pes anserine tendons) was performed in which residual lateral laxity was allowed. Following these procedures, the offset-type tensor was placed with the lower platform fixed to the proximal tibia and the upper seesaw plate fitted to the femoral condyle. Using the tensor with a distraction force of 40 lb, the joint-centre gap and varus ligament balance at extension and flexion with the PF joint reduced were recorded on the navigation system software. During each recording, the thigh and knee were aligned in the sagittal plane to eliminate the external load on the knee at each flexion angle. A distraction force of 40 lb was selected because it recreated the joint gap in full extension in the femoral trial, which corresponds to the insert thickness in preliminary clinical studies. This joint-distraction force was loaded several times until the joint-centre gap remained constant; this was done to reduce the error that can result from creep elongation of the surrounding soft tissue. The height and angle of the distal femoral osteotomy was planned perpendicular to the femoral mechanical axis on the navigation system. On the same navigation screen, based on soft-tissue balance with the tensor and the anatomical landmarks (including anterior cortex and posterior condylar axis), the size of the femoral component, amount of posterior femoral osteotomy, medial/lateral gap and varus/valgus balance were planned to create an acceptable, equalised rectangular extension and flexion gap. Femoral rotation was determined by adjusting the posterior condylar axis, transepicondylar axis, Whiteside line and soft-tissue balance at flexion. In this step, especially in PS, a flexion gap < 5 mm greater than the extension gap was permitted by allowing <3° of varus ligament balance. Following virtual planning on the screen, bony resections were performed. If osteophytes were present on the posterior aspect of the femur, they were removed. Following each bony resection, the tensor was fixed, and the femoral trial prosthesis and PF joint were reduced by temporarily suturing the medial parapatellar arthrotomy. Then, the final soft-tissue balance, including the joint-component gap and varus ligament balance, with the knee at 0° (full extension), 10° (extension), 30°, 60°, 90° (flexion), and 120° (deep flexion), was measured, guided by the navigation system.
Postoperative clinical outcome
At a minimum two year follow-up, a clinical evaluation was performed for each patient with regard to ROM and Knee Society Clinical Rating System [19], which includes a Knee Society Score (KSS), rating the knee itself for pain, stability and ROM, and a functional score [Knee Society Functional Score (KSFS)] assessing activities such as walking and stair climbing. In addition, any knee crepitus or other complications in PF articulation, such as subluxation or dislocation of the extensor mechanism or patellar fracture, were recorded carefully.
Statistical analysis
All values were expressed as the mean ± SE or mean (range). Results were analysed using a statistical software package (Statview 5.0; Abacus Concepts Inc., Berkeley, CA, USA). Nonpaired Student’s t test was utilised to compare parameters in averaged values and clinical scores between the CR and PS groups and between measured-resection and gap techniques. The paired Student’s t test was used to compare values at extension and flexion. The difference between the number of cases in CR and PS groups that achieved an equalised rectangular gap and between the measured-resection and gap techniques was analysed using Pearson’s chi-square test. P < 0.05 was considered statistically significant.
Results
Soft-tissue balance using the gap technique
Mean joint-component gap with the knee at extension and flexion was 14.7 ± 0.3 and 14.7 ± 0.4 mm in CR, and 14.6 ± 0.3 and 17.5 ± 0.5 mm in PS, respectively (Table 1). Whereas the extension value showed no significant differences between CR and PS (p = 0.8186), the flexion value in PS was significantly larger than that in CR (p = 0.0006).
Table 1.
Mean soft-tissue balance in gap technique and measured resection (mean ± standard error)
| Techniques | Component gap (mm) | Varus angle (°) | ||
|---|---|---|---|---|
| CR | PS | CR | PS | |
| Gap | ||||
| Extension | 14.7 ± 0.3 | 14.6 ± 0.3 | 3.0 ± 0.4 | 2.8 ± 0.5 |
| Flexion | 14.7 ± 0.4 | 17.5 ± 0.5* | 1.8 ± 0.4 | 3.0 ± 0.6 |
| Measured resection | ||||
| Extension | 15.4 ± 0.3 | 15.2 ± 0.3 | 3.8 ± 0.7 | 2.6 ± 0.3 |
| Flexion | 13.9 ± 0.5 | 18.2 ± 0.4* | 1.7 ± 0.9 | 4.7 ± 0.4* |
CR cruciate retaining, PS posterior stabiliased
*: P < 0.05 vs. CR
Mean varus ligament balance with the knee at extension and flexion was 3.0 ± 0.4° and 1.8 ± 0.4° in CR, and 2.8 ± 0.5° and 3.0 ± 0.6° in PS, respectively (Table 1). Extension and flexion values showed no significant differences between CR and PS (p = 0.8212, p = 0.0918).
Soft-tissue balance using the measured-resection technique
Mean joint-component gap with the knee at extension and flexion was 15.4 ± 0.3 and 13.9 ± 0.5 mm in CR, and 15.2 ± 0.3 and 18.2 ± 0.4 mm in PS, respectively (Table 1). Whereas the extension value showed no significant differences between CR and PS (p = 0.6428), the flexion value in PS was significantly larger than the value in CR (p < 0.0001). The mean varus ligament balance with the knee at extension and flexion was 3.8 ± 0.7° and 1.7 ± 0.9° in CR and 2.6 ± 0.3° and 4.7 ± 0.4° in PS, respectively (Table 1). Whereas the extension value showed no significant differences between CR and PS (p = 0.1378), the flexion value in PS was significantly larger than the value in CR (p = 0.0053).
Achieving equalised rectangular gap at extension and flexion
When both differences within ± 3-mm joint-component gap between extension and flexion and ± 3° ligament balance at extension and flexion were defined as equalised rectangular gaps, 66. 7 % of CR (64/90) and 44.4 % of PS (20/45) met criteria in the gap technique. In the measured-resection technique, 50 % (10/20) of patients in the CR group and 28 % (28/100) in the PS group met criteria (Table 2). The value in CR was superior to that in PS using both the gap and measured-resection techniques (p = 0.0047, p = 0.0364), and the value using the gap technique showed superior tendency but no significant difference to that using the measured-resection technique in both CR and PS (p = 0.2568, p = 0.0789).
Table 2.
Acquisition of equalised rectangular gap at extension and flexion
| Technique | Total knee arthroscopy type | |
|---|---|---|
| Gap | CR | PS |
| 64/90 (66.7 %) * | 20/45 (44.4 %) | |
| Measured resection | CR | PS |
| 11/20 (55.0 %) * | 28/100 (28.0 %) | |
CR cruciate retaining, PS posterior stabilised
*: P < 0.05 vs. PS
Minimum two year postoperative clinical outcome
Postoperative ROM using the gap technique was −1.2° (range, 0°–10°) in extension and 118.1° (range, 90°–135°) in flexion in the CR group, and −1.5° (range, 0°–15°) in extension and 121.3° (range, 90°–140°) in flexion in the PS group. There were no significant differences between groups (p = 0.5702) and flexion (p = 0.1834) (Table 3). Postoperative ROM using measured resection was −0.9° (range, 0°–10°) in extension and 125.9° (range, 100°–140°) in flexion in the CR group, and −2.2° (range, 0°–15°) in extension and 123.9° (range, 100°–135°) in flexion in the PS group. There were no significant differences between CR and PS in extension (p = 0.3351) and flexion (p = 0.5297) (Table 3).
Table 3.
Minumum 2-year clinical follow-up
| Measured resection | Gap technique | |||
|---|---|---|---|---|
| CR | PS | CR | PS | |
| Extension | −0.9 (0–10) | −2.2 (0–15) | −1.2 (0–10) | −1.5 (0–15) |
| Flexion | 125.9 (100–140) | 123.9 (100–135) | 118.1 (90–135) | 121.3 (90–140) |
| KSS | 96.5 (81–100) | 95.8 (82–100) | 95.4 (75–100) | 97.6 (82–100) |
| KSFS | 88.3 (72–100) | 83.4 (40–100) | 87.7 (40–100) | 86.5 (62–100) |
CR cruciate retaining, PS posterior stabiliazed, KSS Knee Society Knee Score, KSFS Knee Society Functional Score
Postoperative scores using the gap technique were 95.4 (range, 75–100) in KSS and 87.7 (range, 40–100) in KSFS in the CR group, and 97.6 (range, 82–100) in KSS and 86.5 (range, 62–100) in KSFS in the PS group. There were no significant differences between CR and PS in KSS (p = 0.0319) and KSFS (p = 0.5813) (Table 3). Postoperative scores using measured resection were 96.5 (range, 81–100) in KSS and 88.3 (range, 72–100) in KSFS in the CR group, and 95.8 (range, 82–100) in KSS and 83.4 (range, 40–100) in KSFS in the PS group. There were no significant differences between CR and PS in KSS (p = 0.6502) and KSFS (p = 0.3143) (Table 3).
Discussion
The most important finding in this study is that the superiority of CR using the gap technique in achieving an equalised rectangular gap is not directly reflected in the clinical outcome at a minimum two year follow-up. Achieving an equalised rectangular gap revealed that the gap technique showed superior trend in relation to the measured-resection technique, and that CR was superior to PS. However, there were no significant differences in postoperative ROM, KSS or KSFS at a minimum two year clinical follow-up. Recently, a close relationship was found between intra-operative and five year postoperative soft-tissue balance in CR and PS when preserving the physiologic condition of the knee [5]. Therefore, intra-operative soft-tissue balance is considered to remain postoperatively, to some extent. Because surgeons’ subjective clinical scores do not reflect patient-based objective outcomes, such as satisfaction, the KSS system was recently updated and validated to include objective and functional assessments to better reflect patient outcome following TKA [20]. As Matsuda et al. reported, this update in the scoring system may clarify the superiority of an operative procedure or prosthesis type in the future [21].
Traditionally, it is recognised that the PS prosthesis and procedure will result in a different knee condition, including postoperative kinematics and outcomes, compared with CR [22–25]. In our study, joint-component gap at flexion was significantly larger than at extension in PS using the measured-resection technique. This was caused primarily by resecting the PCL, as reported by Kadoya et al. [26]. However, the same pattern was found in the gap technique in our study. The advantage of the measured-resection technique involves preservation of the joint line by avoiding excessive release of medial structures [27, 28]. To this end, in procedures using measured resection, residual lateral ligament laxity tends to be allowed [29–31]. In contrast, focusing on the adjustment of varus/valgus ligament balance in the gap technique sometimes results in excessive release of medial structures to equalise lateral laxity and requires the use of a thicker polyethylene insert [27, 28]. Recognising this, in this study, even with the gap technique, a larger flexion gap of up to 5 mm and residual lateral laxity up to 3° were accepted in the soft-tissue-balancing procedure, especially in PS. This study, which had the same concept as the measured-resection technique with regard to avoiding joint-line elevation and allowing residual lateral ligamentous laxity, so called “medial gap technique”, demonstrated that soft-tissue balancing using the tibia-first gap technique had larger component gaps at flexion in PS. However, when using the gap technique, varus ligament balance showed no significant difference between extension and flexion. Adjustment using the gap technique and a navigation system may reduce the outliers of varus/valgus balance even at flexion.
As an essential concept in TKA, preparing an equalised rectangular gap in extension and flexion is desirable to ensure proper knee kinematics. Several investigators recently reported that navigation-assisted gap balancing achieved more rectangular extension and flexion gaps compared with the conventional measured-resection technique [32–34]. However, these investigators did not assess the difference between PS and CR. If this concept was applied to our study, in CR, the joint-component gap and ligament balance would show no significant differences between extension and flexion, suggesting that rectangular gaps were achieved. In fact, with our definition of equalised rectangular gap, 66.7 % (64/90) CR using the gap technique and 50 % (10/20) CR using the measured-resection technique met criteria. However, only 44.4 % (20/45) PS using the gap technique and 28 % (28/100) PS using the measured-resection technique met criteria. This difference between CR and PS may be explained as above. As for comparison between the measured-resection and gap techniques, the gap technique showed superiority in achieving an equalised rectangular gap. However, the superiority of the measured-resection or gap technique in bone cut during TKA remains controversial [8–11]. Recently, the “adopted” measured-resection technique, taking into account the native rotational geometry of the femur (as measured on preoperative CT), was reported to obtain appropriate femoral-component rotation, similar to the gap technique; and to reduce outliers, compared with the conventional measured-resection technique [35]. In the future, by incorporating the merit of each procedure, the combined procedure of the gap and measured-resection techniques, should be considered and assessed for the effectiveness on clinical outcome.
This study has several limitations. Comparisons between gap and measured-resection techniques were performed in a retrospective manner using different types of prosthesis. Future studies should be designed to compare the procedures in a prospective, randomised fashion using the same implant type. In addition, the populations assessed were limited to varus-type osteoarthritis and excluded severe osteoarthritic knees with large bony defects. In the future, valgus and severe osteoarthritic knees need to be assessed and compared with the populations in this series. Measurements of soft-tissue balance were performed only with 40 lb of distraction force throughout ROM. Asano et al. evaluated stiffness of the soft-tissue complex in osteoarthritic knees in PS and showed that stiffness in extension was significantly greater than that in flexion [36]. Different distraction forces may lead to different soft-tissue balance, which may result in different operative procedures and postoperative outcomes.
In conclusion, achieving an equalised rectangular gap at extension and flexion was compared between CR and PS and between the conventional measured-resection and tibia-first gap techniques. The superiority of CR using the gap technique was not directly reflected in the clinical outcome at a minimum two year follow-up. In the future, a procedure incorporating the merits of the measured-resection and gap techniques should be designed and assessed for itheir effect on clinical outcome.
Acknowledgments
Conflict of interest
None.
References
- 1.Muratsu H, Tsumura N, Yamaguchi M, Mizuno K, Kuroda R, Kurosaka M. Patellar eversion affects soft tissue balance in total knee arthroplasty. Trans Orthop Res. 2003;28:242. [Google Scholar]
- 2.Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M. Joint gap kinematics in posterior-stabilized total knee arthroplasty measured by a new tensor with the navigation system. J Biomech Eng. 2006;128(6):867–871. doi: 10.1115/1.2354201. [DOI] [PubMed] [Google Scholar]
- 3.Matsumoto T, Kuroda R, Kubo S, Muratsu H, Mizuno K, Kurosaka M. The intra-operative joint gap in cruciate-retaining compared with posterior-stabilised total knee replacement. J Bone Joint Surg Br. 2009;91(4):475–480. doi: 10.1302/0301-620X.91B4.21862. [DOI] [PubMed] [Google Scholar]
- 4.Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kurosaka M, Kuroda R. Soft tissue tension in cruciate-retaining and posterior-stabilized total knee arthroplasty. J Arthroplasty. 2011;26(5):788–795. doi: 10.1016/j.arth.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 5.Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kurosaka M, Kuroda R. Intraoperative soft tissue balance reflects minimum 5-year midterm outcomes in cruciate-retaining and posterior-stabilized total knee arthroplasty. J Arthroplasty. 2012;27(9):1723–1730. doi: 10.1016/j.arth.2012.02.020. [DOI] [PubMed] [Google Scholar]
- 6.Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kurosaka M, Kuroda R. Soft tissue balance measurement in posterior-stabilized total knee arthroplasty with a navigation system. J Arthroplasty. 2009;24(3):358–364. doi: 10.1016/j.arth.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Muratsu H, Matsumoto T, Kubo S, Maruo A, Miya H, Kurosaka M, Kuroda R. Femoral component placement changes soft tissue balance in posterior-stabilized total knee arthroplasty. Clin Biomech (Bristol, Avon) 2010;25(9):926–930. doi: 10.1016/j.clinbiomech.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 8.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res (286):40–47 [PubMed]
- 9.Dennis DA. Measured resection: an outdated technique in total knee arthroplasty. Orthopedics. 2008;31(9):940. doi: 10.3928/01477447-20080901-08. [DOI] [PubMed] [Google Scholar]
- 10.Fehring TK (2000) Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res (380):72–79 [DOI] [PubMed]
- 11.Griffin FM, Math K, Scuderi GR, Insall JN, Poilvache PL. Anatomy of the epicondyles of the distal femur: MRI analysis of normal knees. J Arthroplasty. 2000;15(3):354–359. doi: 10.1016/S0883-5403(00)90739-3. [DOI] [PubMed] [Google Scholar]
- 12.Whiteside LA, Arima J (1995) The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res (321):168–172 [PubMed]
- 13.Mantas JP, Bloebaum RD, Skedros JG, Hofmann AA. Implications of reference axes used for rotational alignment of the femoral component in primary and revision knee arthroplasty. J Arthroplasty. 1992;7(4):531–535. doi: 10.1016/S0883-5403(06)80075-6. [DOI] [PubMed] [Google Scholar]
- 14.Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE (1996) Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res (331):35–46 [DOI] [PubMed]
- 15.Schnurr C, Nessler J, Konig DP. Is referencing the posterior condyles sufficient to achieve a rectangular flexion gap in total knee arthroplasty? Int Orthop. 2009;33(6):1561–1565. doi: 10.1007/s00264-008-0656-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katz MA, Beck TD, Silber JS, Seldes RM, Lotke PA. Determining femoral rotational alignment in total knee arthroplasty: reliability of techniques. J Arthroplasty. 2001;16(3):301–305. doi: 10.1054/arth.2001.21456. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto T, Muratsu H, Kubo S, Matsushita T, Ishida K, Sasaki H, Oka S, Kurosaka M, Kuroda R. Soft tissue balance using the tibia first gap technique with navigation system in cruciate-retaining total knee arthroplasty. Int Orthop. 2012;36(5):975–980. doi: 10.1007/s00264-011-1377-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matsuzaki T, Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kawakami Y, Ishida K, Oka S, Kuroda R, Kurosaka M. Kinematic factors affecting postoperative knee flexion after cruciate-retaining total knee arthroplasty. Int Orthop. 2013;37(5):803–808. doi: 10.1007/s00264-013-1803-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res (248):13–14 [PubMed]
- 20.The Knee Society (2007) http://www.kneesociety.org/web/outcom
- 21.Matsuda S, Kawahara S, Okazaki K, Tashiro Y, Iwamoto Y. Postoperative alignment and ROM affect patient satisfaction after TKA. Clin Orthop Relat Res. 2013;471(1):127–133. doi: 10.1007/s11999-012-2533-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maruyama S, Yoshiya S, Matsui N, Kuroda R, Kurosaka M. Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19(3):349–353. doi: 10.1016/j.arth.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 23.Wunschel M, Leasure JM, Dalheimer P, Kraft N, Wulker N, Muller O. Differences in knee joint kinematics and forces after posterior cruciate retaining and stabilized total knee arthroplasty. Knee. 2013 doi: 10.1016/j.knee.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Seon JK, Park JK, Shin YJ, Seo HY, Lee KB, Song EK. Comparisons of kinematics and range of motion in high-flexion total knee arthroplasty: cruciate retaining vs. substituting designs. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2016–2022. doi: 10.1007/s00167-011-1434-z. [DOI] [PubMed] [Google Scholar]
- 25.McCalden RW, MacDonald SJ, Charron KD, Bourne RB, Naudie DD. The role of polyethylene design on postoperative TKA flexion: an analysis of 1534 cases. Clin Orthop Relat Res. 2010;468(1):108–114. doi: 10.1007/s11999-009-1127-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kadoya Y, Kobayashi A, Komatsu T, Nakagawa S, Yamano Y (2001) Effects of posterior cruciate ligament resection on the tibiofemoral joint gap. Clin Orthop Relat Res (391):210–217 [DOI] [PubMed]
- 27.Lee HJ, Lee JS, Jung HJ, Song KS, Yang JJ, Park CW. Comparison of joint line position changes after primary bilateral total knee arthroplasty performed using the navigation-assisted measured gap resection or gap balancing techniques. Knee Surg Sports Traumatol Arthrosc. 2011 doi: 10.1007/s00167-011-1468-2. [DOI] [PubMed] [Google Scholar]
- 28.Tigani D, Sabbioni G, Ben Ayad R, Filanti M, Rani N, Del Piccolo N. Comparison between two computer-assisted total knee arthroplasty: gap-balancing versus measured resection technique. Knee Surg Sports Traumatol Arthrosc. 2010;18(10):1304–1310. doi: 10.1007/s00167-010-1124-2. [DOI] [PubMed] [Google Scholar]
- 29.Lotke PA. Primary total knees: standard principles and technique. Knee Arthroplasty. Philadelphia: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- 30.Sculco TP. Soft tisseu balancing in total knee arthroplasty. Controversies of Total Knee Replacement. New York: Ranven Press; 1991. [Google Scholar]
- 31.Sekiya H, Takatoku K, Takada H, Sasanuma H, Sugimoto N. Postoperative lateral ligamentous laxity diminishes with time after TKA in the varus knee. Clin Orthop Relat Res. 2009;467(6):1582–1586. doi: 10.1007/s11999-008-0588-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee DH, Padhy D, Park JH, Jeong WK, Park JH, Han SB. The impact of a rectangular or trapezoidal flexion gap on the femoral component rotation in TKA. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1141–1147. doi: 10.1007/s00167-011-1422-3. [DOI] [PubMed] [Google Scholar]
- 33.Lee DH, Park JH, Song DI, Padhy D, Jeong WK, Han SB. Accuracy of soft tissue balancing in TKA: comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):381–387. doi: 10.1007/s00167-009-0983-x. [DOI] [PubMed] [Google Scholar]
- 34.Seon JK, Song EK, Park SJ, Lee DS. The use of navigation to obtain rectangular flexion and extension gaps during primary total knee arthroplasty and midterm clinical results. J Arthroplasty. 2011;26(4):582–590. doi: 10.1016/j.arth.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 35.Luyckx T, Peeters T, Vandenneucker H, Victor J, Bellemans J. Is adapted measured resection superior to gap-balancing in determining femoral component rotation in total knee replacement? J Bone Joint Surg Br. 2012;94(9):1271–1276. doi: 10.1302/0301-620X.94B9.28670. [DOI] [PubMed] [Google Scholar]
- 36.Fujimoto E, Sasashige Y, Masuda Y, Hisatome T, Eguchi A, Masuda T, Sawa M, Nagata Y. Significant effect of the posterior tibial slope and medial/lateral ligament balance on knee flexion in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012 doi: 10.1007/s00167-012-2059-6. [DOI] [PubMed] [Google Scholar]