Abstract
Purpose
Several authors have observed that standard instrumentation (SI) may be insufficient for addressing component malalignment. Patient-matched cutting blocks (PMCB) technology was introduced to improve surgeons’ ability to achieve a neutral postoperative mechanical axis following total knee arthroplasty (TKA). The current retrospective study was designed to compare the ability of SI and PMCB to achieve a hip-knee-ankle angle (HKA) within ±3° of the ideal alignment of 180°.
Methods
Between October 2009 and December 2012, 170 TKAs in 166 patients (four bilateral) using VISIONAIRE (Smith & Nephew) PMCB technology were performed. Additionally, 160 TKAs in 160 consecutive patients that had received a total knee arthroplasty using SI during the same time period were used as a control group, All surgeries were performed by the same surgeon. Standardized pre- and postoperative long-leg standing x-rays were retrospectively evaluated to compare the two patient cohorts.
Results
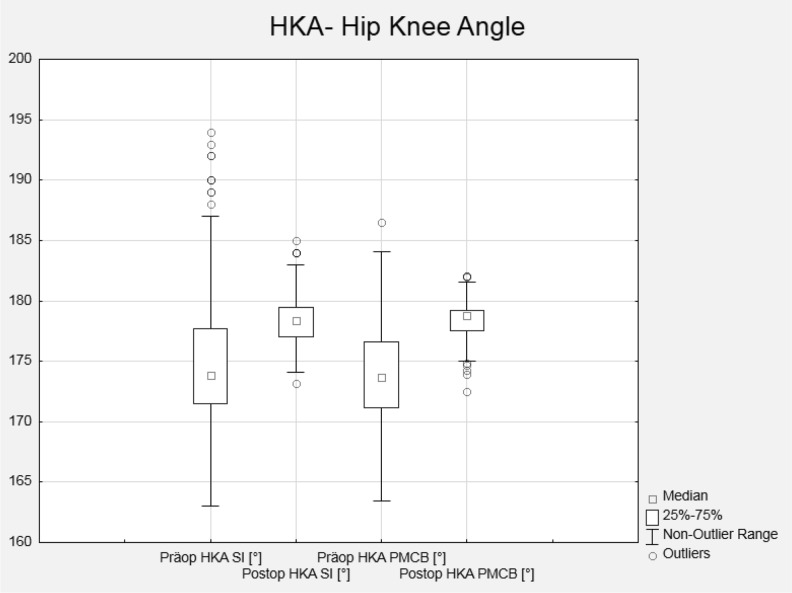
X-rays were available for analysis for 156 knees in the SI group and 150 in the PMCB group. The average post-surgical HKA was 178.7 ± 2.5 in the SI group and 178.4 ± 1.5 in the PMCB group. However, the rate of ± 3° outliers was 21.2 % in the SI group and 9.3 % in the PMCB group. There were no intraoperative complications with the use of PMCB technology or SI.
Conclusions
PMCB technology proved superior to conventional instrumentation in achieving a neutral mechanical axis following TKA. Further follow-up will be needed to ascertain the long-term impact of these findings.
Keywords: Total knee replacement, Total knee arthroplasty, Patient matched cutting blocks, Standard knee instrumentation, Component malalignment, Neutral mechanical axis, Hip-knee-ankle angle
Introduction
Total knee arthroplasty (TKA) has a high success rate for addressing pain and improving function [4]. However, in instances where incorrect positioning and malignment of the TKA components are observed, patients can experience a range of negative postoperative outcomes such as loss of thickness of polyethylene tibial bearings, eccentric loading, implant loosening, and eventual early revision [10, 35, 36, 39, 43]. To avoid these complications, achieving a postoperative alignment within the range of 0° ± 3° of the mechanical axis is recommended [20, 33]. Manual intramedullary/extramedullary guides are not thought to be capable of consistently achieving axes in this range [30, 41], and though computer-assisted navigation has shown superior results in comparison with conventional instrumentation [30], it is also limited by increased surgical times and no clear superiority in improving short-term clinical outcomes [8].
Thus, there has been in a push in the orthopaedic community to create more precise technologies to aid in the reconstruction of the knee’s mechanical axis. Patient-specific instrumentation (PSI), which uses anatomical data obtained primarily from pre-operative axial computed tomography (CT) or magnetic resonance imaging (MRI) to create disposable cutting jigs individualized to the patient’s unique anatomy, was created with this goal [16].
The aim of the current comparative analysis was to analyze post-surgical alignment in a cohort of patients undergoing TKA with a PSI system (VISIONAIRE; Smith & Nephew, Memphis, TN, USA) and a cohort undergoing TKA with conventional instrumentation. The study is based to our previous clinical results with a single analysis of the clinical outcome of PSI technology [12].
It was hypothesized PSI would lead to a neutral mechanical axis on average more frequently than conventional instrumentation.
Methods
This study was conducted between October 2009 and December 2012. During that period, the senior author (C.O.T.) performed 170 TKAs in 166 patients (four bilateral) using VISIONAIRE patient-matched cutting blocks technology (PMCB group). A group of 160 TKAs in 160 consecutive patients using standard instrumentation (SI group) from the same time period served as control group. These two groups were obtained from different hospitals. In the one hospital, the VISIONAIRE technology is used for all TKAs, whereas in the other hospital standard instrumentation is employed. This study follows the Declaration of Helsinki. In Germany, where this study was conducted, retrospective epidemiological studies without personally identifiable data do not need to be sent to the ethical committee for approval.
Patients had a diagnosis of either primary or posttraumatic osteoarthritis, no signs of a mediolateral instability or a varus/valgus deformity with a deviation of >15°, and to be able to undergo preoperative MRI, with no metallic hardware in close proximity to the operated knee. Additionally, those in the PMCB group needed to be willing to wait the four to six weeks typically required for this specialized instrumentation to be prepared.
In the SI group, there was no calculation of the rate of patients who were lost to follow-up, as they were chosen based on the availability of x-rays. However, in four cases (2.5 %) the x-rays could not be evaluated due to the following reasons: rotation on the whole leg x-ray was incorrect (three patients) and flexion contracture >10° (one patient). This left a cohort of 156 evaluable knees. In the PMCB group, there were 159 x-rays available. Eleven x-rays (6.4 %) were not available as they were either incomplete or not available due to patient refusal or lack of attendance of follow-up visits. Additionally, nine x-rays (5.3 %) could not be evaluated due to the following reasons: rotation on the whole leg x-ray was incorrect (two), femoral head not on the leg length x-ray (one), flexion contracture >10° (three), extra-articular malalignment, whereas the pre-operative planning was not done for a neutral axis (two bowed femur, one posttraumatic malalignment after a fracture). This left a cohort of 150 evaluable knees. Demographic data for both groups can be found in Table 1.
Table 1.
Baseline demographics for SI group (156 knees) and PMCB group (150 knees)
| Variables | SI Group | PMCB Group |
|---|---|---|
| Mean age, years (range; SD) | 65.0 (41–93; 9.2) | 66.1 (26–88; 8.8) |
| Mean weight, kg (range; SD) | 85.9 (51–134; 17.9) | 92.6 (69–116; 13.7) |
| Mean height, cm (range; SD) | 168 (148–194; 9.3) | 171 (149–186; 8.8) |
| Mean BMI (range; SD) | 30.3 (20.2-42.1; 5.3) | 31.7 (25.6-44.2; 4.6) |
| Gender (n, %) | ||
| Male | 79 (50.6 %) | 95 (63.3 %) |
| Female | 77 (49.4 %) | 55 (36.7 %) |
| Operated side (n, %) | ||
| Left | 83 (53.8 %) | 68 (43 %) |
| Right | 73 (46.2 %) | 91 (57 %) |
| Diagnosis (n, %) | ||
| Varus OA | 127 (81.4 %) | 114 (71.7 %) |
| Valgus OA | 16 (10.3 %) | 20 (12.6 %) |
| Posttraumatic OA | 9 (5.8 %) | 15 (9.4 %) |
| Patellofemoral OA | 4 (2.6 %) | 10 (6.3 %) |
| Operative time, minutes (range; SD) | 51.1 (38–76; 7.2) | 50.9 (35–90; 10.0) |
All patients received a cemented Genesis II™ (Smith and Nephew, Memphis, TN) posterior-stabilized high-flexion prosthesis and were operated upon using a conventional medial parapatellar approach. In the PMCB group, patients received femoral components fabricated from an oxidized zirconium alloy (Oxinium™, Smith and Nephew, Memphis, TN), whereas those in the SI group had cobalt-chrome components. The knees of the patients in the PMCB group underwent a full-leg radiograph and MRI preoperatively.
The process by which the VISIONAIRE instrumentation is produced has been described in detail in other studies [11, 18, 31]. The surgeon’s preferences called for a 9-mm proximal resection, a posterior slope alignment of 3°, a varus/valgus alignment of 4–7° if there was no rotation in the x-rays or, if there was rotation due to malalignment or degenerative joint, 5° for varus knees and 7° for valgus knees.
Standing long-leg x-rays were performed pre- and postoperatively to ascertain all radiographic endpoints, which is part of the senior author’s routine care. An independent orthopaedic surgeon (K.D.) then performed radiographic measurements for the following endpoint: hip-knee-ankle angle (HKA), defined as the angle between the mechanical axis of the femur and the mechanical axis of the tibia, with both lines crossing at the center of the knee (Fig. 1a-b) The following were considered the ideal (i.e., normal or in-range) values for these radiographic measurements: 0° ± 3° varus/valgus for HKA. HKA was calculated as a mean for the entire patient cohort, and additionally patients outside the ±3° range were noted.
Fig. 1.
a-b: The hip-knee-ankle angle (HKA) was determined as the angle between the mechanical axis of the femur and the mechanical axis of the tibia. Both lines cross the center of the knee (red marked circle). In this preoperative image HKA value is 168.72° (a). The postoperative HKA value is 179.42° (b)
We used a non-parametric Fisher's exact test in the analysis of contingency tables. Descriptive analysis (mean ± standard deviation was done using Microsoft Excel (Microsoft Corporation, Seattle, USA) and IBM SPSS Statistics 18 (PASW 18, SPSS Inc., Chicago, IL, USA).
Results
Postoperative x-ray analysis occurred at a mean interval of 3.5 months (range, 2.5-3.5) in the SI group and 3.5 months (range, 2.5–3.5) for the PMCB group.
Patients in the PMCB group experienced a post-TKA neutral mechanical alignment outside ±3° of the ideal alignment of 180° HKA at a significantly lower rate than those in the SI group (p = 0.0031; Table 2; Fig. 2).
Table 2.
Mean hip-knee-ankle angle (HKA) findings for SI group (156 knees) and PMCB group (150 knees), including outliers beyond the ideal alignment of 180°
| Range of Alignment | ||||||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD (Range) | <177° | >183° | Outlier ±3° | |||||
| SI | PCMB | SI | PCMB | SI | PCMB | SI | PCMB | |
| HKA preop | 175.2 ± 6.3 (163–198) | 173.7 ± 3.9 (163.5–186.5) | 110 | 116 | 16 | 2 | 80.8 % | 78.7 % |
| HKA postop | 178.7 ± 2.5 (173.2–188) | 178.4 ± 1.5 (172.5–182.1) | 22 | 14 | 11 | 0 | 21.2 % | 9.3 % |
Fig. 2.
Range of knees falling ±3° outside of the ideal hip-knee-ankle angle (HKA) alignment of 180°, pre- and post-operatively
There were no intraoperative complications encountered in either group, and the specialized instrumentation used in the PMCB group was optimally fitted to all the patients’ individual anatomy and did not require any additional modifications.
Discussion
VISIONAIRE technology was designed to restore a neutral postoperative mechanical axis. By using pre-operative MRI data and full-length anterior/posterior radiographs to ascertain the current and planned mechanical axis, engineers are able to produce tibial and femoral resection guides fitted to the patient’s specific anatomy. This is the latest study to support the accuracy of this technology [12, 18, 31]. It also represents an update of an earlier analysis in which results for a smaller cohort (100 knees) operated with this technology were presented without a comparison cohort [12]. With the addition of 50 knees to the PMCB cohort, alignment outcomes continued to be highly positive, and the number of knees ±3° beyond the ideal alignment of 180° actually fell slightly from 11 % to the 9.3 % noted in the current analysis.
Although these results attest to the viability of PMCB technology, it was equally important for us to include a cohort of patients operated with standard instrumentation in order to more fully understand how these two different techniques impact frontal alignment. Indeed, as hypothesized there was a substantial difference in the number of knees ±3° beyond the ideal alignment (21.2 % for the SI group, 9.3 % for the PMCB group). Our rates with PMCB compare favorably to the average 10.2 % rate resulting from computer-assisted navigation in prior studies, and substantially improves on the 28.2 % rate encountered with conventional instrumentation [30].
An overview of studies reporting frontal plane alignment within this range for both conventional instrumentation and PMCB are provided in Tables 3 and 4. With 90.7 % of knees in the current analysis within the ideal range, our results can be considered amongst the best yet noted. They are in line with other studies of PSI which reported improved alignment [16, 30, 38]. Although it should be noted that other studies have failed to show a clear advantage for PSI technology [24, 32], and that one study with the technology employed in the current analysis observed only a fair rate of accuracy, with higher risk of error >3° in the sagittal plane [11], there does appear to be an overall trend for the superiority of these new technologies over earlier instrumentation methods.
Table 3.
An overview of published data using conventional instrumentation that reported total frontal knee alignment within ±3° of ideal
| Author, year | Method | Evaluation method | N | Percentage of knees within ±3° of ideal |
|---|---|---|---|---|
| Yau et al. 2008 [45] | Manual | postop x-ray | 52 | 75 |
| Stockl et al. 2004 [40] | Manual | postop x-ray | 32 | 94 |
| Hart et al. 2003 [17] | Manual | postop x-ray | 60 | 70 |
| Hart et al. 2003 [17] | Manual | postop x-ray | 60 | 93 |
| Matsumoto et al. 2004 [27] | Manual | postop x-ray | 30 | 67 |
| Tillett et al. 1988 [42] | Manual (IM) | postop x-ray | 25 | 92 |
| Tillett et al. 1988 [42] | Manual (IM) | postop x-ray | 25 | 92 |
| Tillett et al. 1988 [42] | Manual (EM) | postop x-ray | 25 | 80 |
| Tillett et al. 1988 [42] | Manual (EM) | postop x-ray | 25 | 80 |
| Decking et al., 2005 [13] | Manual | postop x-ray | 25 | 36 |
| Decking et al. 2005 [13] | Manual | postop x-ray | 25 | 68 |
| Kim et al. 2005 [23] | Manual | postop x-ray | 78 | 73 |
| Haaker et al. 2005 [15] | Manual | postop x-ray | 100 | 72 |
| Matziolis et al. 2007 [28] | Manual | CT scanner | 28 | 75 |
| Kim et al. 2007 [23] | Manual | postop x-ray | 100 | 82 |
| Chauhan et al. 2004 [7] | Manual | postop x-ray | 36 | 72 |
| Chin et al. 2005 [9] | Manual (IM) | postop x-ray | 30 | 63 |
| Chin et al. 2005 [9] | Manual (EM) | postop x-ray | 30 | 63 |
| Bathis et al. 2004 [3] | Manual | postop x-ray | 80 | 78 |
| Sparmann et al. 2003 [37] | Manual | postop x-ray | 120 | 87 |
| current study | Manual | postop x-ray | 156 | 79 |
Table 4.
An overview of published data using custom jigs that reported total frontal knee alignment within ±3° of ideal
| Author, year | Method (Manufacturer) | Evaluation method | N | Percentage of knees within ±3° of ideal |
|---|---|---|---|---|
| Koeck et al. 2011 [25] | iUni (Conformis) | postop x-ray | 32 | 100 |
| Yaffe et al. 2012 [44] | PSI (Zimmer) | postop x-ray | 95 | 83 |
| Chareancholvanich et al. 2013 [6] | PSI (Zimmer) | CT scanner, scout view | 40 | 97 |
| Daniilidis and Tibesku 2013 [12] | Visionaire (Smith & Nephew) | postop x-ray | 100 | 89 |
| Nam et al. 2013 [29] | Signature (Biomet) | postop x-ray | 41 | 71 |
| Bali et al. 2012 [1] | Visionaire (Smith & Nephew) | postop x-ray | 32 | 91 |
| Nunley et al. 2012 [32] | Signature (Biomet) | CT scanner, scout view | 50 | 82 |
| Nunley et al. 2012 [32] | OtisMed (Stryker) | CT scanner, scout view | 50 | 56 |
| Barrack et al. 2012 [2] | Signature (Biomet) | CT scanner, scout view | 100 | 69 |
| Ng et al. 2012 [30] | Signature (Biomet) | postop x-ray | 569 | 86 |
| Nunley et al. 2012 [32] | Signature (Biomet) | CT scanner, scout view | 57 | 74 |
| Johnson et al. 2011 [22] | Trumatch (DePuy) | postop x-ray | 35 | 72 |
| Spencer et al. 2009 [38] | OtisMed (Stryker) | CT scanner | 21 | 90 |
| Boonen et al. 2012 [5] | Signature (Biomet) | postop x-ray | 40 | 71 |
| Lustig et al. 2013 [26] | Visionaire (Smith & Nephew) | intraoperative navigation | 60 | 79 |
| current study | Visionaire (Smith & Nephew) | postop x-ray | 150 | 91 |
As highlighted in Table 4, there are several different evaluation methods employed in the assessment of frontal knee alignment in studies of custom jigs, including postoperative x-rays and intraoperative navigation. Studies of the VISIONAIRE that evaluated this endpoint with post-operative x-rays, including the current analysis, routinely reported approximately 90 % of knees within the ideal range of alignment [16, 41]. Conversely, the study that evaluated this endpoint with intraoperative navigation reported only 79 % of knees within this range [45]. It is possible that utilizing intraoperative navigation to measure front alignment may account for a 10 % increase in the number of knees reported with malalignment; however, this is outside the scope of the current analysis and should be addressed in a future study. Establishing the best method for measuring this endpoint will be essential for gauging the true value of this technology going forward.
There were no relevant intraoperative issues arising from the use of PMCB in the 150 patients treated in this group throughout the study. This is in line with earlier studies with this technology, which also reported no intraoperative complications to date [11, 18, 31].
There are several limitations to the current analysis that must be taken into account when analyzing these results. Firstly, although a control arm was offered as means of a comparison, there were notable differences in the demographics between the two groups (e.g., more male patients in the PMCB group). It is possible that these factors influenced the overall results. Secondly, this study exclusively deals with radiographic outcomes. Expanding the outcomes to other important aspects of TKA such as pain, stiffness, and range of motion would have provided important further data with which to compare these two separate strategies. PSI has also been shown to shorten surgical steps and operative times, reduce the burden for surgical instrumentation, and lessen adverse outcomes such as blood loss, infection, and systematic fat emboli [16, 19, 24, 31, 38]. Therefore, the proposed utility of this technology should not be limited to radiographic aspects. Thirdly, it must be noted that the operating surgeon undertakes approximately 550 knee replacements annually and it is possible that this high level of experience positively influenced the results. The learning curve for beginner surgeons has been shown to be acceptably low with computer-assisted navigation systems, with the exception of a general increase in operative and tourniquet times during initial cases [14, 21, 34]. Another limitation of the present study is that we did not perform a power-analysis. Additional research is required, however, to ascertain whether less-experienced surgeons would encounter a similar learning curve with this particular PSI technology. Furthermore, it should be noted that the costs for using the PMCB technology are higher than with conventional methods.
In conclusion, PMCB technology proved superior to conventional instrumentation in achieving a neutral mechanical axis following TKA. As this is an update of an earlier study [12], in which data from 50 additional patients were available, these results also reconfirm the earlier conclusion that this specific technology is effective in addressing the issue of malalignment. Further follow-up will be needed to ascertain the long-term impact of these findings.
Acknowledgements
The authors wish to thank the medical assistants Ms. Christina Andrusiak, Ms. Sandra Schaefer, and Ms. Evi Schwarz for the collection of radiographic and patient data and Mr Robert Gartner for his assistance in the measurements. Smith & Nephew provided a medical writer (John Watson) who proofread and edited the manuscript for grammar and issues related to English language.
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. C.O.T is a paid teaching consultant to Smith & Nephew. The authors declare that there are no other potential conflicts of interest in connection with this paper.
References
- 1.Bali K, Walker P, Bruce W. Custom-fit total knee arthroplasty: our initial experience in 32 knees. J Arthroplasty. 2012;27:1149–1154. doi: 10.1016/j.arth.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Ruh EL, Williams BM, Ford AD, Foreman K, Nunley RM. Patient specific cutting blocks are currently of no proven value. J Bone Joint Surg Br. 2012;94(11 Suppl A):95–99. doi: 10.1302/0301-620X.94B11.30834. [DOI] [PubMed] [Google Scholar]
- 3.Bathis H, Perlick L, Tingart M, Luring C, Zurakowski D, Grifka J. Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86:682–687. doi: 10.1302/0301-620X.86B5.14927. [DOI] [PubMed] [Google Scholar]
- 4.Bjorgul K, Novicoff WM, Saleh KJ. Evaluating comorbidities in total hip and knee arthroplasty: available instruments. J Orthop Traumatol. 2010;11:203–209. doi: 10.1007/s10195-010-0115-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boonen B, Schotanus MG, Kort NP. Preliminary experience with the patient-specific templating total knee arthroplasty. Acta Orthop. 2012;83:387–393. doi: 10.3109/17453674.2012.711700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chareancholvanich K, Narkbunnam R, Pornrattanamaneewong C. A prospective randomised controlled study of patient-specific cutting guides compared with conventional instrumentation in total knee replacement. Bone Joint J. 2013;95-B:354–359. doi: 10.1302/0301-620X.95B3.29903. [DOI] [PubMed] [Google Scholar]
- 7.Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg Br. 2004;86:372–377. doi: 10.1302/0301-620X.86B3.14643. [DOI] [PubMed] [Google Scholar]
- 8.Cheng T, Pan XY, Mao X, Zhang GY, Zhang XL. Little clinical advantage of computer-assisted navigation over conventional instrumentation in primary total knee arthroplasty at early follow-up. Knee. 2012;19:237–245. doi: 10.1016/j.knee.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Chin PL, Yang KY, Yeo SJ, Lo NN. Randomized control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthroplasty. 2005;20:618–626. doi: 10.1016/j.arth.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Collier MB, Engh CA, Jr, McAuley JP, Engh GA. Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. J Bone Joint Surg Am. 2007;89:1306–1314. doi: 10.2106/JBJS.F.00667. [DOI] [PubMed] [Google Scholar]
- 11.Conteduca F, Iorio R, Mazza D, Caperna L, Bolle G, Argento G, Ferretti A. Are MRI-based, patient matched cutting jigs as accurate as the tibial guides? Int Orthop. 2012;36:1589–1593. doi: 10.1007/s00264-012-1522-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daniilidis K, Tibesku CO. Frontal plane alignment after total knee arthroplasty using patient-specific instruments. Int Orthop. 2013;37:45–50. doi: 10.1007/s00264-012-1732-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Decking R, Markmann Y, Fuchs J, Puhl W, Scharf HP. Leg axis after computer-navigated total knee arthroplasty: a prospective randomized trial comparing computer-navigated and manual implantation. J Arthroplasty. 2005;20:282–288. doi: 10.1016/j.arth.2004.09.047. [DOI] [PubMed] [Google Scholar]
- 14.Drummond M, Barbieri M, Cook J, Glick HA, Lis J, Malik F, Reed SD, Rutten F, Sculpher M, Severens J. Transferability of economic evaluations across jurisdictions: ISPOR Good Research Practices Task Force report. Value Health. 2009;12:409–418. doi: 10.1111/j.1524-4733.2008.00489.x. [DOI] [PubMed] [Google Scholar]
- 15.Haaker RG, Stockheim M, Kamp M, Proff G, Breitenfelder J, Ottersbach A. Computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res. 2005;433:152–159. doi: 10.1097/01.blo.0000150564.31880.c4. [DOI] [PubMed] [Google Scholar]
- 16.Hafez MA, Chelule KL, Seedhom BB, Sherman KP. Computer-assisted total knee arthroplasty using patient-specific templating. Clin Orthop Relat Res. 2006;444:184–192. doi: 10.1097/01.blo.0000201148.06454.ef. [DOI] [PubMed] [Google Scholar]
- 17.Hart R, Janecek M, Chaker A, Bucek P. Total knee arthroplasty implanted with and without kinematic navigation. Int Orthop. 2003;27:366–369. doi: 10.1007/s00264-003-0501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heyse TJ, Tibesku CO. Improved femoral component rotation in TKA using patient-specific instrumentation. Knee. 2012 doi: 10.1016/j.knee.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 19.Howell SM, Kuznik K, Hull ML, Siston RA. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. 2008;31:857–863. doi: 10.3928/01477447-20080901-15. [DOI] [PubMed] [Google Scholar]
- 20.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 21.Jenny JY, Miehlke RK, Giurea A. Learning curve in navigated total knee replacement. A multi-centre study comparing experienced and beginner centres. Knee. 2008;15:80–84. doi: 10.1016/j.knee.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 22.Johnson DR. The benefits of customized patient instrumentation to lower-volume joint replacement surgeons: results from practice. Am J Orthop (Belle Mead NJ) 2011;40(11 Suppl):13–16. [PubMed] [Google Scholar]
- 23.Kim YH, Kim JS, Yoon SH. Alignment and orientation of the components in total knee replacement with and without navigation support: a prospective, randomised study. J Bone Joint Surg Br. 2007;89:471–476. doi: 10.1302/0301-620X.89B4.18878. [DOI] [PubMed] [Google Scholar]
- 24.Klatt BA, Goyal N, Austin MS, Hozack WJ. Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. J Arthroplasty. 2008;23:26–29. doi: 10.1016/j.arth.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Koeck FX, Beckmann J, Luring C, Rath B, Grifka J, Basad E. Evaluation of implant position and knee alignment after patient-specific unicompartmental knee arthroplasty. Knee. 2011;18:294–299. doi: 10.1016/j.knee.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 26.Lustig S, Scholes CJ, Oussedik SI, Kinzel V, Coolican MR, Parker DA. Unsatisfactory accuracy as determined by computer navigation of VISIONAIRE patient-specific instrumentation for total knee arthroplasty. J Arthroplasty. 2013;28:469–473. doi: 10.1016/j.arth.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 27.Matsumoto T, Tsumura N, Kurosaka M, Muratsu H, Kuroda R, Ishimoto K, Tsujimoto K, Shiba R, Yoshiya S. Prosthetic alignment and sizing in computer-assisted total knee arthroplasty. Int Orthop. 2004;28:282–285. doi: 10.1007/s00264-004-0562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007;89:236–243. doi: 10.2106/JBJS.F.00386. [DOI] [PubMed] [Google Scholar]
- 29.Nam D, Maher PA, Rebolledo BJ, Nawabi DH, McLawhorn AS, Pearle AD. Patient specific cutting guides versus an imageless, computer-assisted surgery system in total knee arthroplasty. Knee. 2013 doi: 10.1016/j.knee.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 30.Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV., Jr Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012;470:99–107. doi: 10.1007/s11999-011-1996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Noble JW, Jr, Moore CA, Liu N. The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplasty. 2012;27:153–155. doi: 10.1016/j.arth.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 32.Nunley RM, Ellison BS, Zhu J, Ruh EL, Howell SM, Barrack RL. Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin Orthop Relat Res. 2012;470:895–902. doi: 10.1007/s11999-011-2222-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 34.Sampath SA, Voon SH, Sangster M, Davies H. The statistical relationship between varus deformity, surgeon's experience, BMI and tourniquet time for computer assisted total knee replacements. Knee. 2009;16:121–124. doi: 10.1016/j.knee.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 35.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Sikorski JM. Alignment in total knee replacement. J Bone Joint Surg Br. 2008;90:1121–1127. doi: 10.1302/0301-620X.90B9.20793. [DOI] [PubMed] [Google Scholar]
- 37.Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A. Positioning of total knee arthroplasty with and without navigation support. A prospective, randomised study. J Bone Joint Surg Br. 2003;85:830–835. [PubMed] [Google Scholar]
- 38.Spencer BA, Mont MA, McGrath MS, Boyd B, Mitrick MF. Initial experience with custom-fit total knee replacement: intra-operative events and long-leg coronal alignment. Int Orthop. 2009;33:1571–1575. doi: 10.1007/s00264-008-0693-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Srivastava A, Lee GY, Steklov N, Colwell CW, Jr, Ezzet KA, D'Lima DD. Effect of tibial component varus on wear in total knee arthroplasty. Knee. 2012;19:560–563. doi: 10.1016/j.knee.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 40.Stockl B, Nogler M, Rosiek R, Fischer M, Krismer M, Kessler O. Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2004;426:180–186. doi: 10.1097/01.blo.0000136835.40566.d9. [DOI] [PubMed] [Google Scholar]
- 41.Stulberg SD, Loan P, Sarin V. Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am. 2002;84-A(Suppl 2):90–98. [PubMed] [Google Scholar]
- 42.Tillett ED, Engh GA, Petersen T. A comparative study of extramedullary and intramedullary alignment systems in total knee arthroplasty. Clin Orthop Relat Res. 1988;230:176–181. [PubMed] [Google Scholar]
- 43.Werner FW, Ayers DC, Maletsky LP, Rullkoetter PJ. The effect of valgus/varus malalignment on load distribution in total knee replacements. J Biomech. 2005;38:349–355. doi: 10.1016/j.jbiomech.2004.02.024. [DOI] [PubMed] [Google Scholar]
- 44.Yaffe MA, Patel A, Mc Coy BW, Luo M, Cayo M, Ghate R, Stulberg SD. Component sizing in total knee arthroplasty: patient-specific guides vs. computer-assisted navigation. Biomed Tech (Berl) 2012;57:277–282. doi: 10.1515/bmt-2011-0093. [DOI] [PubMed] [Google Scholar]
- 45.Yau WP, Chiu KY, Zuo JL, Tang WM, Ng TP. Computer navigation did not improve alignment in a lower-volume total knee practice. Clin Orthop Relat Res. 2008;466:935–945. doi: 10.1007/s11999-008-0144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]