Abstract
Background and Objectives
The aims of this study were to evaluate the relationship between tinnitus and the level of anxiety and depression experienced by subjective tinnitus patients, and to determine the effect of the level of anxiety and depression to the results of tinnitus treatment.
Subjects and Methods
A total of 104 patients were included in this study. All the patients conducted Tinnitus Handicap Inventory (THI), Beck Depression Inventory (BDI), State Trait Anxiety Inventory 1, 2 (STAI 1, 2) to evaluate their psychometric properties. The subjective patterns of tinnitus before and after treatment were assessed through questionnaires.
Results
Significant correlation between THI scores and BDI, STAI 1, 2 scores were observed in the moderate and severe tinnitus group. The patients were classified into two groups depending on their THI scores, and also classified into two groups according to BDI, STAI 1, 2 results. Analysis of differences after treatment indicated significantly improved VAS scores after treatment in all groups.
Conclusions
The subjective level of tinnitus is significantly related with depression and anxiety symptoms when inconvenience caused by tinnitus was moderate or over. Assessments on tinnitus after treatment appeared to have improved significantly regardless of the severity of tinnitus, level of depression or anxiety disorder.
Keywords: Tinnitus, Depression, Anxiety disorder
Introduction
The number of patients with sensorineural hearing loss and tinnitus is rising due to the increase of average life expectancy, noise and stress, while the social significance of this issue has taken on greater importance. However, the mechanism and location of tinnitus have not been clearly identified yet and treating tinnitus is difficult. There is no treatment that could cure tinnitus in a short period. The association between the development of tinnitus and sensorineural hearing loss is well known, but no significance was discovered in the relationship between the hearing loss features and severity of tinnitus. The severity of tinnitus is known to be more closely related to neuropsychiatric factors or general health status than to auditory factors such as the degree of hearing loss and frequency or intensity of tinnitus.1)
Several studies have reported that there was a close relationship between tinnitus and stress, depression or anxiety disorders in tinnitus patients.2) These neuropsychiatric factors are recognized to be able to explain the severity of tinnitus; that is, the differences in various tinnitus features, but the relation between neuropsychiatric factors and the development of tinnitus is yet unclear. According to recent reports, neuropsychiatric factors such as depression or anxiety disorders are not direct causes of tinnitus but can be considered as related variables.3) Depression and anxiety disorders are most commonly known neuropsychiatric factors related to tinnitus and various study results have been reported. Most results were obtained through questionnaires, which present the association between tinnitus and symptoms of depression or anxiety although there are some differences in each report. However, these studies led to simple results that depressive or anxiety symptoms are accompanied in many tinnitus patients, and there are no research done worldwide on the correlation between these symptoms and the severity of tinnitus or how they affect treatment outcomes. In this study, we evaluated the features of depressive and anxiety symptoms accompanied in subjective tinnitus patients, and examined whether the severity of tinnitus and the degree of depressive or anxiety symptoms had a statistical relationship. Also, a subjective assessment was done after 6 months of drug therapy and modified tinnitus retraining therapy to examine any differences in treatment effect by tinnitus severity and by the degree of depressive or anxiety symptoms.
Subjects and Methods
Subjects
Patients who visited the otorhinolaryngology outpatient clinic of our hospital with a chief complaint of tinnitus and were diagnosed as subjective tinnitus from January 2009 to June 2010 were retrospectively investigated. Patients diagnosed as tinnitus due to a specific cause including acute external or middle ear disease, central disorders, cerebellopontine lesions or as objective tinnitus based on history taking, questionnaires, physical examination, hearing tests, and radiologic examinations were excluded. Patients who could not complete the questionnaire due to old age or cognitive disorders, and those who did not receive follow-up for over 6 months were excluded from the study. A total of 104 patients who were able to complete questionnaires after treatment over 6 months were selected as subjects for the final analysis.
Methods
Hearing test
Pure tone audiometry and speech audiometry were performed among all patients to check for hearing loss. Additional information on hearing was obtained through impedance audiometry, evoked otoacoustic emission test, and the auditory brainstem response test. Also, a tinnitogram was performed to confirm the loudness of tinnitus and frequency concordance.
Evaluation of tinnitus
The gender, age, prevalence period of tinnitus and its patterns were investigated and Visual Analog Scale (VAS) was used to evaluate subjective tinnitus patterns of individuals. Also, the Tinnitus Handicap Inventory (THI) which reliability and validity were proven through previous studies in Korea was used to assess tinnitus. Questionnaires on the tinnitus, depression and anxiety symptoms were performed at their first visit. The VAS was used to assess subjective features on tinnitus to analyze results before and after treatment.
Tinnitus questionnaires and VAS scores
Basic items such as the prevalence period, direction, number, and pattern of tinnitus were investigated. As for a subjective assessment on tinnitus, the loudness of tinnitus, awareness time, annoyance from tinnitus, and effect on life were rated as VAS scores in 10-point units.
THI
A Korean version THI was used to rate and measure subjective annoyance from tinnitus and to classify the degree of tinnitus by scores.4) It is composed of 25 items in total, with a functional subscale, emotional subscale, and catastrophic subscale. Each item is rated as 0 (none), 2 (sometimes), 4 (always) and the total score was calculated. Subjects were divided into two groups based on a THI score of 38. Those with less than 38 were designated as the mild tinnitus group while patients with a score of 38 or higher were classified as the moderate or more serious tinnitus group. Correlations with other variables were compared and significant differences in treatment outcomes were confirmed.
Evaluation of depressive symptoms
Evaluation on depressive symptoms was done by using the Korean version of the Beck Depression Inventory (BDI) which is composed of 21 items in total. BDI includes the emotional, cognitive, motive and physiological areas of depression and rates each item by a scale from 0 to 3 depending on the degree of symptoms. The sum of each item score of 0 to 9 is classified as normal, 10 to 15 as mild depression, 16 to 23 as moderate depression, and 24 to 63 as severe depression.
Evaluation of anxiety symptoms
State Trait Anxiety Inventory (STAI) 1 and 2 were used to assess the state and trait anxiety disorders. STAI 1 and 2 are each composed of 20 items, rating the anxiety symptoms by a scale from 0 to 4 points. STAI 1 presents the degree of state anxiety and evaluates the anxiety degree that changes depending on specific circumstances. STAI 2 indicates trait anxiety and shows the anxiety degree due to the tendency of each individual regardless of any specific situation. In STAI 1, a score of 52 or less is classified as normal, 53 to 56 as mild anxiety, 57 to 61 as moderate anxiety, and 62 or higher as severe anxiety. In STAI 2, a score of 54 or less is classified as normal, 55 to 58 as mild anxiety, 59 to 63 as moderate anxiety, and 64 or higher as severe anxiety.
Treatment
After completing history taking, examinations and questionnaires, modified tinnitus retraining therapy and drug therapy were done. The modified tinnitus retraining therapy was performed by one of the authors and included explanations on the mechanism of tinnitus clarified until today, general aspects of tinnitus, correlation between hearing tests, tinnitogram and tinnitus, results of questionnaires and other tests, general misconceptions about tinnitus, aggravating factors, and the general treatment process and prognosis. This therapy took about 10 minutes. The same contents were repetitively explained at follow-up every month at the outpatient clinic so that the patient could thoroughly understand tinnitus. As for drug therapy, medication for improving peripheral blood circulation such as ginko biloba agents (Ginnexin-F, SK Chemicals Life Science, Seongnam, Korea, 80 mg/T), Nicergolin (Sermion, Ildong Pharmaceutical Co, Seoul, Korea, 10 mg/T) and Sarpogrelate (Anplag, Yuhan Corporation, Seoul, Korea, 100 mg/T) were prescribed together for over 6 months. Antianxiety drugs were not used. Among 45 patients with sensorineural hearing loss accompanied, hearing aids were suggested to 19 patients with moderate or severe hearing loss and 4 patients of them actually used hearing aids. Noise avoidance and sound therapy using TV or radios were explained and attempted, but sound generators or tinnitus maskers were not applied. Follow-up on changes in tinnitus and hearing was done every month and hearing tests were performed again if necessary. In order to analyze treatment results after modified tinnitus retraining therapy and drug therapy for over 6 months, four items including loudness, awareness, annoyance, and effect on life were reevaluated by VAS scores. Results obtained before and after treatment were compared and analyzed.
Result analysis
Statistical analysis was done by using the SPSS 15.0 (SPSS Inc., Chicago, IL, USA) program. The Pearson bivariates correlation test was used to analyze correlations between variables, and a paired sample t-test was used to compare changes in VAS scores before and after treatment. The level of significance was set as 0.05 or less.
Results
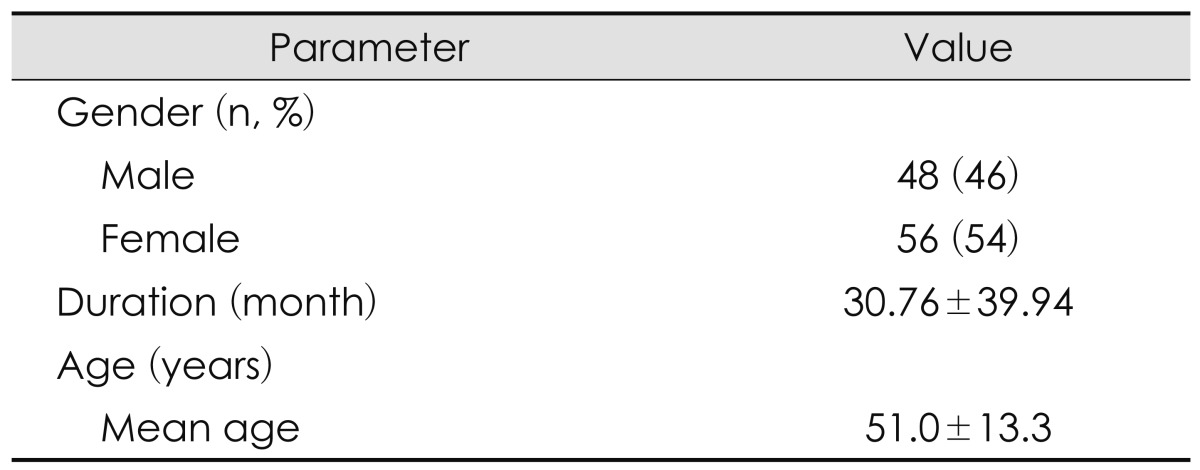
Among 104 tinnitus patients, 48 were men (46%) and 56 (54%) were women. The average age of subjects was 51.0 years (±13.2) and the average prevalence period of tinnitus was 30.7 months (Table 1).
Table 1.
Clinical characteristics of patients
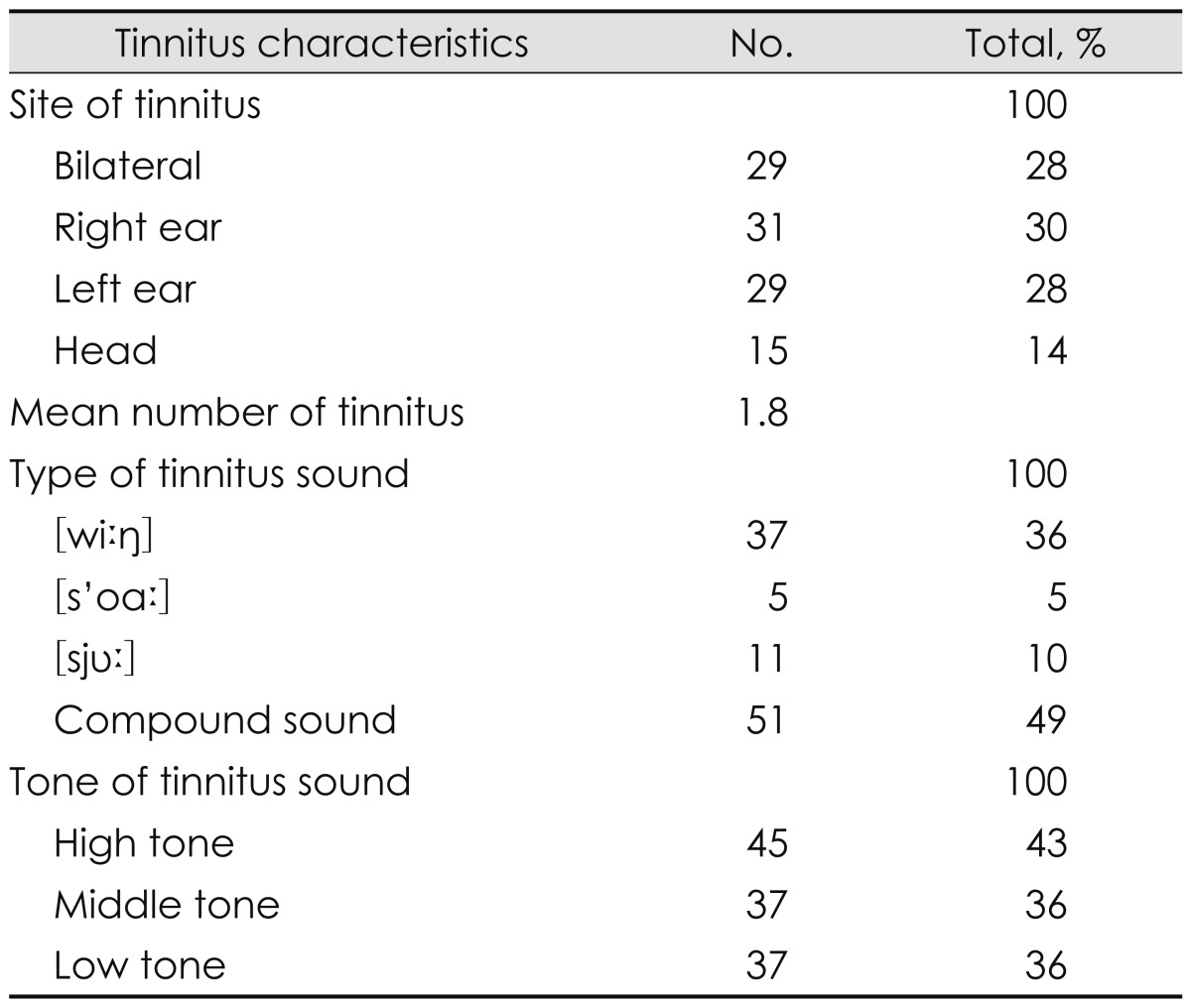
As for the location of tinnitus, 31 cases were in the right side (30%), 29 in the left (28%), and 29 in both sides (28%). The number of tinnitus noises was 1.8 in average. 63 patients heard one sound (61%), while 41 (39%) heard 2 or more sounds. 37 patients (36%) heard a 'whizzing' noise while 5 (5%) heard a 'whistling' sound, 11 (10%) heard a 'shush' sound, and 10 patients (10%) heard other types of sounds. As for the sound pitch, 45 patients complained high pitch sounds (43%) while 22 heard low pitch (21%), and 37 heard a middle pitch sound (36%)(Table 2).
Table 2.
Tinnitus characteristics of patients
Among the 104 patients, 59 (57%) showed normal hearing in the hearing test results. 45 patients (43%) appeared as sensorineural hearing loss with a pure tone audiometry threshold over 26 dB. 17 of these sensorineural hearing loss patients were unilateral (5 patients with right side hearing loss, 12 with left side hearing loss) while the remaining 28 patients showed bilateral hearing loss.
Correlations between variables before treatment
The average THI score was 40.1 (±24.1), and 49 patients (47%) appeared to have moderate or more serious tinnitus with a score over 38. The average BDI score was 11.4 (±8.2), and 27 patients appeared to be in a moderate or severe depressive state (26%). The average scores of STAI 1 and 2 were 44.5 (±10.9) and 42.6 (±9.6), respectively. The number of patients corresponding to mild or more serious anxiety level was 22 (21%) and 11 (11%), respectively (Table 3). There was a statistically significant correlation between THI and BDI scores, and between THI, STAI 1, and STAI 2 scores. The BDI, STAI 1 and STAI 2 scores also showed a statistically significant correlation. Age had no significant correlation with THI, STAI 1 and 2, but showed a statistically significant correlation with BDI. There was no statistical significance with the prevalence period of tinnitus and each variable. No significant correlation was observed with BDI, STAI 1 and STAI 2 in the mild tinnitus group with a THI scores lower than 38. However, the moderate or more serious tinnitus group showed a significant correlation with BDI, STAI 1, and STAI 2 (Table 4).
Table 3.
Mean and distribution of THI, BDI, STAI 1 and STAI 2
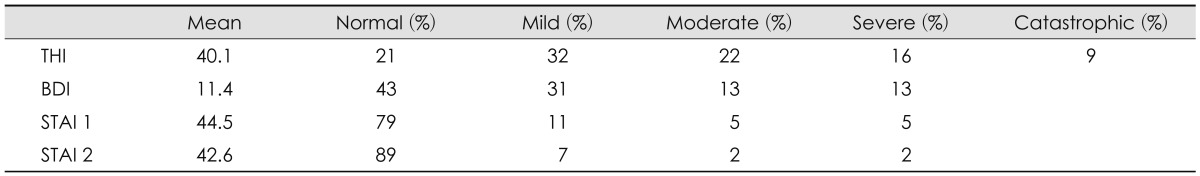
THI: Tinnitus Handicap Inventory, BDI: Beck Depression Inventory, STAI: State Trait Anxiety Inventory
Table 4.
Correlations between THI and BDI, STAI 1, STAI 2 (Pearson correlation test, *p<0.05)
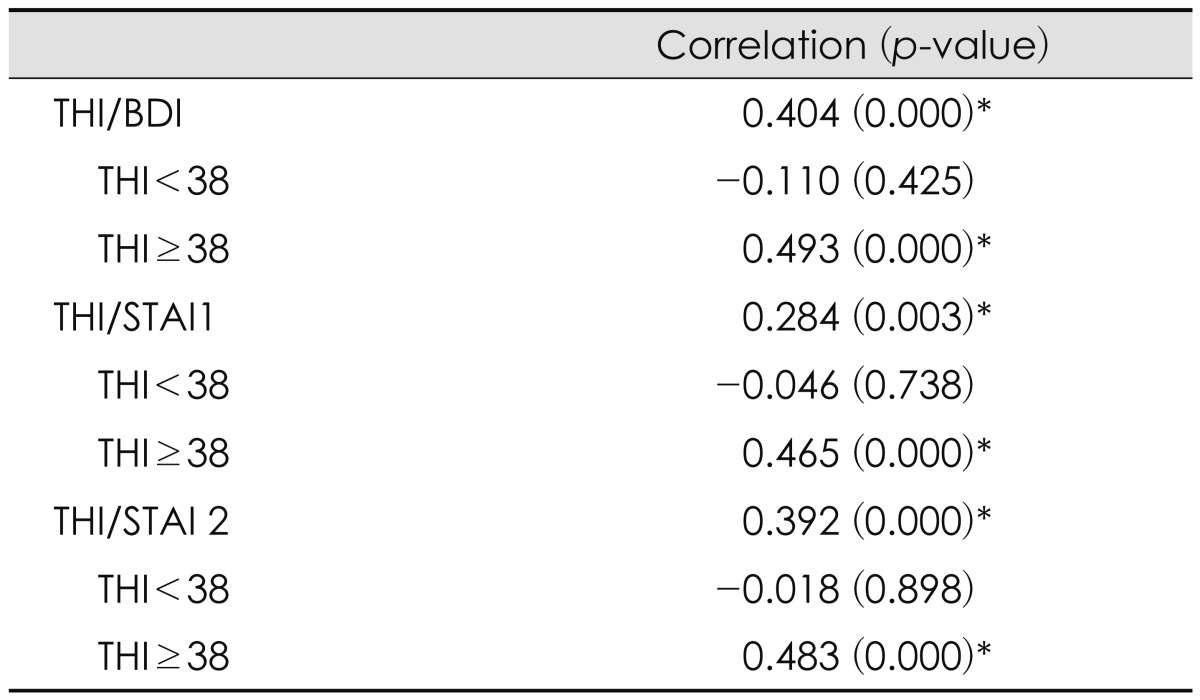
THI: Tinnitus Handicap Inventory, BDI: Beck Depression Inventory, STAI: State Trait Anxiety Inventory
THI appeared to have a statistically significant relation with all four items of VAS. VAS and STAI 2 had a statistically significant correlation only in the item of annoyance from tinnitus, while none was observed in the remaining three items. VAS, BDI, and STAI 1 all did not have any significant correlation (Table 5).
Table 5.
Correlations between VAS and THI, BDI, STAI 1, STAI 2 (Pearson correlation test, *p<0.05)
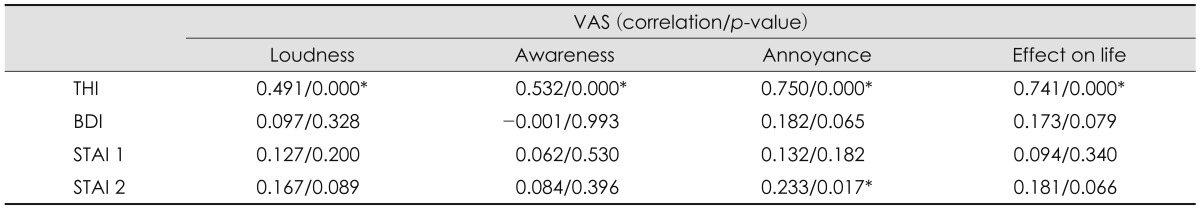
VAS: Visual Analogue Scale, THI: Tinnitus Handicap Inventory, BDI: Beck Depression Inventory, STAI: State Trait Anxiety Inventory
Changes in subjective evaluation on tinnitus before and after treatment
The score of loudness of tinnitus before treatment was 4.4±2.4, while the awareness time of tinnitus was 5.9±3.3, annoyance from tinnitus was 5.3±3.0, and the effect on life was 5.1±3.1. After treatment, these scores improved to 2.9±2.4, 3.6±3.4, 3.1±2.8, and 2.9±2.5, respectively. This difference was statistically significant (p<0.05). Changes in the subjective evaluation on tinnitus before and after treatment depending on THI scores were divided into the mild tinnitus group and the moderate or more serious tinnitus group. The loudness, awareness, annoyance, and effect on life of tinnitus showed significant improvements in the two groups. Also, an additional analysis was performed with the BDI standard set differently as 15 or lower and 16 or higher, but there was no difference between the two groups in these cases as well and all items appeared to have statistically significant improvements. STAI 1 and 2 were divided into the normal group and mild or more serious anxiety symptom group to compare changes in subjective evaluation on tinnitus before and after treatment. All items showed statistically significant improvements (Table 6).
Table 6.
Changes of visual analogue scale score in THI, BDI, STAI 1, STAI 2 after treatment (Paired t-test, all parameter show statistical significant)
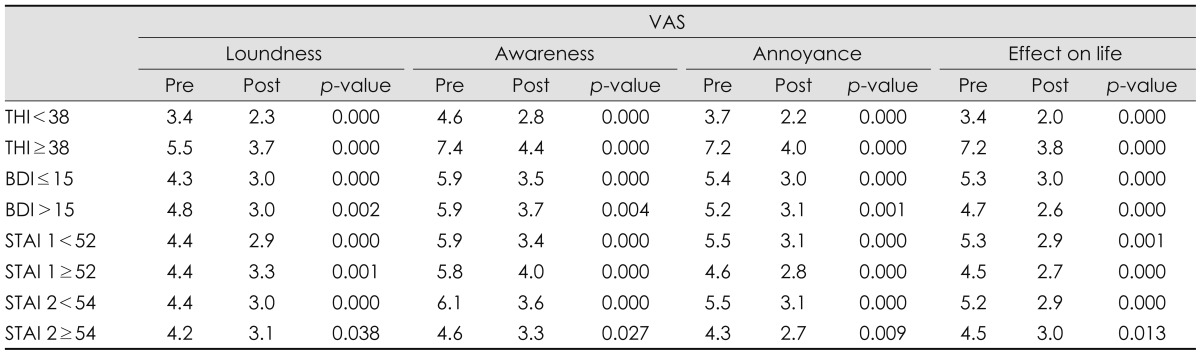
THI: Tinnitus Handicap Inventory, BDI: Beck Depression Inventory, STAI: State Trait Anxiety Inventory, Pre: pre-treatment, Post: post-treatment
Discussion
The ratio of depressive symptoms accompanied in tinnitus patients appears variously in reports, ranging in about 45-60% and anxiety symptoms are reported in about 19-45%.3,5) In this study, depressive symptoms were observed in 57% while state and trait anxiety symptoms showed in 21% and 11%, respectively which are similar to previous reports. According to the epidemiological survey of psychiatric illnesses in Korea by the Ministry of Health and Welfare in 2006, the prevalence of depression in Korea is reported as 2.1% and anxiety disorder as 3.2%. Previous reported that the prevalence of depression in adults is about 5% which increases to 10% when accompanied with other illnesses.6) The average BDI score in the depression group was 23.48 while it appeared as 8.43 in the group of ordinary people, based on the Korean version BDI study results.7) A score of 16 was presented as the standard for screening depression groups. When comparing this study with research results reported in Korea and foreign countries, it appears that depressive and anxiety symptoms are frequently accompanied in tinnitus patients. Compared to these study results, the high frequency of depression in tinnitus patients is similar to that in major chronic diseases and is inferred to negatively affect the quality of life of patients. However, the BDI cut-off score in the screening criteria has not been united yet and appears differently in each report. The reports above applied the cut-off score variously as well, from 10 to 14 respectively. The Korean version BDI study has presented a score of 16 as the standard for screening depression groups, and a study on the usefulness of BDI among the elderly population in Korea indicated that it would be appropriate to distinguish depression from normal in the aged by this score.8) 57% of the patients in this study applied to depression when analyzed by a cut-off score of 10 which was the standard for mild depression. Meanwhile, 26% of patients showed over a score of 16 which indicates moderate or severe depressive symptoms. From these results, we were able to identify a high rate of depressive symptoms accompanied.
The STAI which was used for evaluating anxiety disorders is also a standardized anxiety measurement tool most commonly used variously in clinical sites. In this study, trait anxiety and state anxiety were assessed separately in order to analyze the association between tinnitus and anxiety symptoms more. As a result, the prevalence of state anxiety and trait anxiety appeared as 21% and 11%, respectively, which were both higher than that of ordinary people. The percentage of state anxiety appeared higher than trait anxiety. Trait anxiety disorder indicates anxiety occurring depending on individual characteristic tendency regardless of the current situation. Thus, in this study where the prevalence of trait anxiety appeared higher than that in ordinary people, it could be interpreted that the characteristic anxiety level of individuals may be associated with the occurrence and appearance of tinnitus. Also, state anxiety presents the level of anxiety reflecting a certain situation in reality. The higher percentage of patients with state anxiety in this study shows that the level of anxiety symptoms may have been aggravated due to inappropriate emotions, stress or decline in concentration related to tinnitus. Put together, the level of existing characteristic anxiety in tinnitus patients is high and the current anxiety level increases from the occurrence of tinnitus. Therefore, the association between tinnitus and anxiety disorder should be considered as significant.
The annoyance from tinnitus assessed by THI and BDI, STAI values all showed a statistically significant correlation. Especially, a significant correlation was observed in the moderate or more serious tinnitus group with a THI score of over 38, but no relation was found in the mild tinnitus groups. From this, we were able to conclude that the level of depressive or anxiety symptoms was more serious when the annoyance from tinnitus was moderate or higher. Crocetti, et al.9) evaluated 108 tinnitus patients with questionnaires to examine the relationship between annoyance from tinnitus, depressive and anxiety symptoms, and reported the presence of a significant correlation. A close relationship was also reported between the intensity of tinnitus, stress, depression, and anxiety disorder in other studies.10-12) Antidepressants, antipsychotics and sedatives have been known to be partially effective in treating tinnitus, and some opinions have been reported that neuropsychological mediation is important in tinnitus treatment.5,13) This indicates the necessity of an approach and treatment to mental disorders such as depression or anxiety among tinnitus patients, especially if the annoyance from tinnitus assessed by THI is moderate or more serious.
No association between age and THI was observed in this study, but astatistically significant correlation appeared with BDI. The incidence of tinnitus is known to increase as sensorineural hearing loss worsens along with age. Considering several study results that the level of annoyance from tinnitus is more closely related to psychoneurotic factors including depression or overall health status than audiological factors, the result of this study that the age factor is unrelated to the severity of tinnitus seems to be reasonable. The frequency of depression increases due to several different social factors along with the increase of age. Since depression is associated with the development of tinnitus and the early discovery and treatment of depression are beneficial to treating tinnitus, evaluation on whether elderly tinnitus patients have depressive symptoms and early treatment acquires a significant meaning.14)
The prevalence of hearing loss and tinnitus increases along with age, but no correlation between age, gender, or the prevalence period of tinnitus and the annoyance from tinnitus is known.15) There was no correlation observed between the prevalence period and THI, BDI, and STAI 1, 2 in this study as well. A longer prevalence period does not always indicate a more serious level of annoyance from tinnitus, depression or anxiety. This may be the basis for the opinion that active treatment is required even in patients with a long prevalence period.
Treatments for tinnitus were variable. However, no single treatment can cure tinnitus in a short period. So various methods are being used in combination and the effects of each treatment are reported variously in studies.2) Currently, tinnitus retraining therapy is being held based on the neuropsychological model of tinnitus presented by Jastreboff16) Tinnitus retraining therapy is applied with several other methods in combination in most cases, since the same treatment outcomes do not appear in all patients in a short period. It also takes a long time for treatment effects to appear and continuous treatment for at least over 6 months is usually required. Modified tinnitus retraining therapy changed the original tinnitus retraining therapy by reducing theoriginal long counseling time, summarizing the major content of directive counseling within a relatively short time so that patients could overcome negative thoughts about tinnitus. A Korean study held among 43 tinnitus patients reported that the group which received medication with modified tinnitus retraining therapy in combination showed significant improvements in multiple items such as the loudness and awarenesstime of tinnitus, annoyance from tinnitus and effect on life due to tinnitus than the group which received combined drug therapy only.14) In this study, a subjective evaluation (loudness, awareness, annoyance, and effect on life) on tinnitus patients was done after providing 6 months of medication and modified tinnitus retraining therapy and all items showed statistically significant improvements. Thus, the modified tinnitus retraining therapy was confirmed as a useful treatment method for tinnitus patients. However, there was no difference depending on the level of annoyance, depressive and anxiety symptoms. The presence and degree of annoyance due to tinnitus, depressive and anxiety symptoms could not actually be factors that affect tinnitus treatment. However, there still is a possibility that patients who did not relatively experience any treatment effects while receiving 6 months of treatment may have been lost during follow-up, and subjective factors of patients might have been reflected in the result analysis since only the VAS questionnaire was used for evaluating treatment effects. Considering these possibilities, it is not clear whether these factors are influential to treatment outcomes. As we still lack an objective diagnosis tool and a standardized treatment method for tinnitus, clinical studies examining a larger number of patients for a long period and the development of tools for objectively assessing tinnitus may be necessary in order to investigate clear prognosis factors.
Conclusion
A statistically significant correlation with depressive and anxiety symptoms was observed in the moderate or more serious tinnitus group with a THI score of over 38. However, there was no significant correlation found in the mild tinnitus groups. Thus, it is considered that appropriate treatment along with evaluation on neuropsychiatric disorders such as depression and anxiety would be required if the severity of tinnitus appears as moderate or higher in the questionnaires. Assessments on tinnitus after treatment appeared to have improved significantly regardless of the severity of tinnitus, level of depression or anxiety disorder.
References
- 1.Zöger S, Svedlund J, Holgers KM. Relationship between tinnitus severity and psychiatric disorders. Psychosomatics. 2006;47:282–288. doi: 10.1176/appi.psy.47.4.282. [DOI] [PubMed] [Google Scholar]
- 2.Seidman MD, Standring RT, Dornhoffer JL. Tinnitus: current understanding and contemporary management. Curr Opin Otolaryngol Head Neck Surg. 2010;18:363–368. doi: 10.1097/MOO.0b013e32833c718d. [DOI] [PubMed] [Google Scholar]
- 3.Belli S, Belli H, Bahcebasi T, Ozcetin A, Alpay E, Ertem U. Assessment of psychopathological aspects and psychiatric comorbidities in patients affected by tinnitus. Eur Arch Otorhinolaryngol. 2008;265:279–285. doi: 10.1007/s00405-007-0440-8. [DOI] [PubMed] [Google Scholar]
- 4.Kim JH, Lee SY, Kim CH, Lim SL, Shin JN, Chung WH, et al. Reliability and validity of a Korean adaptation of the tinnitus handicap inventory. Korean J Otolaryngol-Head Neck Surg. 2002;45:328–334. [Google Scholar]
- 5.Reynolds P, Gardner D, Lee R. Tinnitus and psychological morbidity: a cross-sectional study to investigate psychological morbidity in tinnitus patients and its relationship with severity of symptoms and illness perceptions. Clin Otolaryngol Allied Sci. 2004;29:628–634. doi: 10.1111/j.1365-2273.2004.00879.x. [DOI] [PubMed] [Google Scholar]
- 6.Dobie RA, Sullivan MD. Antidepressant drugs and tinnitus. In: Vernon JA, editor. Tinnitus Treatment and Relief. 1st ed. Boston: Allyn and Bacon; 1998. pp. 43–51. [Google Scholar]
- 7.Lee YH, Song JY. A study of the reliability and the validity of the BDI, SDS, and MMPI-D scales. Korean J Clin Psychol. 1991;10:98–113. [Google Scholar]
- 8.Jo SA, Park MH, Jo I, Ryu SH, Han C. Usefulness of Beck Depression Inventory (BDI) in the Korean elderly population. Int J Geriatr Psychiatry. 2007;22:218–223. doi: 10.1002/gps.1664. [DOI] [PubMed] [Google Scholar]
- 9.Crocetti A, Forti S, Ambrosetti U, Bo LD. Questionnaires to evaluate anxiety and depressive levels in tinnitus patients. Otolaryngol Head Neck Surg. 2009;140:403–405. doi: 10.1016/j.otohns.2008.11.036. [DOI] [PubMed] [Google Scholar]
- 10.Lim JJ, Lu PK, Koh DS, Eng SP. Impact of tinnitus as measured by the Tinnitus Handicap Inventory among tinnitus sufferers in Singapore. Singapore Med J. 2010;51:551–557. [PubMed] [Google Scholar]
- 11.Auo HJ, Park KH, Yeo SW, Chang KH, Choi HG, Choi BJ, et al. Treatment response of modified tinnitus retraining therapy with medical therapy in the patients with tinnitus. Korean J Otorhinolaryngol-Head Neck Surg. 2009;52:648–654. [Google Scholar]
- 12.Zöger S, Svedlund J, Holgers KM. The Hospital Anxiety and Depression Scale (HAD) as a screening instrument in tinnitus evaluation. Int J Audiol. 2004;43:458–464. doi: 10.1080/14992020400050058. [DOI] [PubMed] [Google Scholar]
- 13.Fornaro M, Martino M. Tinnitus psychopharmacology: a comprehensive review of its pathomechanisms and management. Neuropsychiatr Dis Treat. 2010;6:209–218. doi: 10.2147/ndt.s10361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheline YI, Sanghavi M, Mintun MA, Gado MH. Depression duration but not age predicts hippocampal volume loss in medically healthy women with recurrent major depression. J Neurosci. 1999;19:5034–5043. doi: 10.1523/JNEUROSCI.19-12-05034.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pinto PC, Sanchez TG, Tomita S. The impact of gender, age and hearing loss on tinnitus severity. Braz J Otorhinolaryngol. 2010;76:18–24. doi: 10.1590/S1808-86942010000100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jastreboff PJ. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res. 1990;8:221–254. doi: 10.1016/0168-0102(90)90031-9. [DOI] [PubMed] [Google Scholar]


