Abstract
Age-related hearing loss (presbycusis) is characterized by an increased hearing threshold and poor speech understanding in a noisy environment, slowed central processing of acoustic information, and impaired localization of sound sources. Presbycusis seriously affects the older people's quality of life. Particularly, hearing loss in the elderly contributes to social isolation, depression, and loss of self-esteem. Current amplification methods related to auditory rehabilitation can provide improved communication ability to users. But, simple auditory rehabilitation is ineffective in managing the central auditory processing disorder and the psychosocial problem of presbycusis. The evaluation of central auditory processing disorder and psychosocial disorder in presbycusis should not be overlooked while providing auditory rehabilitation.
Keywords: Age-related hearing loss, Presbycusis, Cochlea, Inner ear, Auditory processing
Introduction
Age-related hearing loss (presbycusis) is described as a sensorineural hearing impairment caused by aging. Presbycusis is characterized by decreased speech understanding in a noisy environment, slowed central processing of acoustic information and impaired localization of sound sources, and natural deterioration in hearing. Patients who suffer from presbycusis encounter various difficulties in carrying out the activities of daily life. Age-related hearing loss occurs in elderly people in their 60s and in 50% of people in the over 70 age group.1)
The diagnosis of presbycusis is based on the medical history and physical examination. The ability to locate the sound source deteriorates in both ears of patients with presbycusis with a mild-to-moderate hearing loss in the high-frequency range. Presbycusis is usually diagnosed when patients meets the following criteria: symmetric increased hearing threshold, the absence of injury, use of ototoxic medications, history of ear disease and previous ear surgery, the presence of minimum conductive hearing loss (10 dB or lower), and aged 65 years or older.2)
According to the histological changes and the sites of degeneration in the cochlea identified by Schuknecht, presbycusis is divided into the following five types: sensory presbycusis, in which an abrupt change in the audiometric pattern is caused by the degeneration of hair cells; neural presbycusis, in which there is a downward sloping pattern on the audiogram and loss of cochlear nerve cells and central neural pathways; metabolic presbycusis, in which there is atrophy of the stria vascularis and a flat hearing curve on the audiogram; cochlear presbycusis, in which there is a gradual sloping pattern on the audiogram and there are no histological changes in organ of Corti and neural structure; mixed presbycusis, in which there is a combination of the symptoms of the other types of presbycusis.3) Once presbycusis is diagnosed based on medical history, physical examination and hearing test, it is classified into one of these five types for auditory rehabilitation. However, patients with presbycusis may have much difficulty of hearing in a noisy environment and decreased sound localization even when they have a normal threshold of hearing.4) The conventional hearing screening test such as pure-tone audiometry is not enough to measure the overall hearing ability. Also, successful rehabilitation of patients with presbycusis should not be judged only by an improvement in the hearing ability. Diverse screening methods are needed for variations of symptoms in patients with presbycusis.
To accurately measure the hearing ability of elderly people, it is crucial to identify the difficulties that they encounter during everyday life using proper assessment methods and to provide customized rehabilitation programs. The purpose of this study was to discuss the various assessment methods available to measure the hearing ability in patients with presbycusis and their difficulties in daily life.
Discussion
Medical history of hearing loss
Presbycusis may progress slowly, and the patients may not realize that their hearing ability is deteriorating. While taking the medical history of patients with presbycusis, it is important to identify the sounds which elderly people cannot understand as much as the sounds which elderly people cannot hear. It is also important to be aware of the fact that presbycusis is associated with depression and cognitive disorder in many cases. In such cases, treatment of concurrent conditions should also be considered. Risk factors for presbycusis that need to be assessed include exposure to noise, smoking, drug use, high blood pressure and family history of presbycusis. Previous history of working in noisy areas and exposure to noises like that of a gunshot may cause hearing loss in the higher frequency range, which in turn results in presbycusis in the entire frequency range. It is important to check if there are any otologic symptoms such as tinnitus and dizziness in order to ensure that presbycusis is not caused by other illnesses such as tumors around the auditory nerve.
Physical examination
Earwax should be removed before the inspection of the ear. Earwax can block the ear canal and can cause hearing loss in elderly people and impair the performance of the hearing aid. Therefore, earwax removal is important. In addition, presence of otorrhea should be assessed and the tympanic membranes should be carefully examined in patients with suspected presbycusis to determine whether concurrent conditions such as otitis media and cholesteatoma.
Hearing screening and testing
As hearing disorders progress very slowly, patients do not realize that their hearing ability is deteriorating. Hearing screening can be performed to detect presbycusis. For hearing screening, the whispered voice test is widely performed in outpatient clinic. In this test, the examiner stands behind the patient in order to prevent the patient from seeing the examiner at a distance of 6 inches and 2 feet from the ear, and whispers three different single-digit numbers while the external auditory canal of the other ear is occluded with his hand. Then the patient is asked to repeat the numbers that he/she heard. If a subject obtains a score of 50 or less on a 100-point scale, he/she is considered to have failed the whispered voice test, and a hearing loss of 30 dB can be expected.5) In addition, the tuning fork test is useful to determine whether hearing loss is caused by conductive or sensorineural impairment. The test is important for hearing screening of outpatient clinic.
Pure tone test
The pure tone test is an essential tool to diagnose and evaluate presbycusis. This test is the most important to assess the status of patients who are undergoing rehabilitation, including wearing the hearing devices. Test results provide very useful information for evaluating the outcomes of hearing rehabilitation. The accurate air conduction and bone conduction tests are included in the pure tone test. Elderly people may have difficulty in following the test instructions and they may feel exhausted as the test is time-consuming. Therefore, pre-test training is recommended.
Speech audiometry test
Patients with presbycusis may have a difficulty in listening and understanding what the other people are saying. Measuring the ability to hear and understand speech in patients with presbycusis is very important for selecting the appropriate treatment methods and interpreting the outcomes. Also, test results can be used for laying down the guidelines for hearing rehabilitation interventions and for assessing the difficulties encountered by the patients with hearing loss and their adaptability in the society. When compared with the pure tone test, the speech audiometry test is more complicated and extensive since it examines the physiological, linguistic and psychological aspects of speech, thereby making it crucial in patients with presbycusis.6)
Hearing in noise test (HINT)
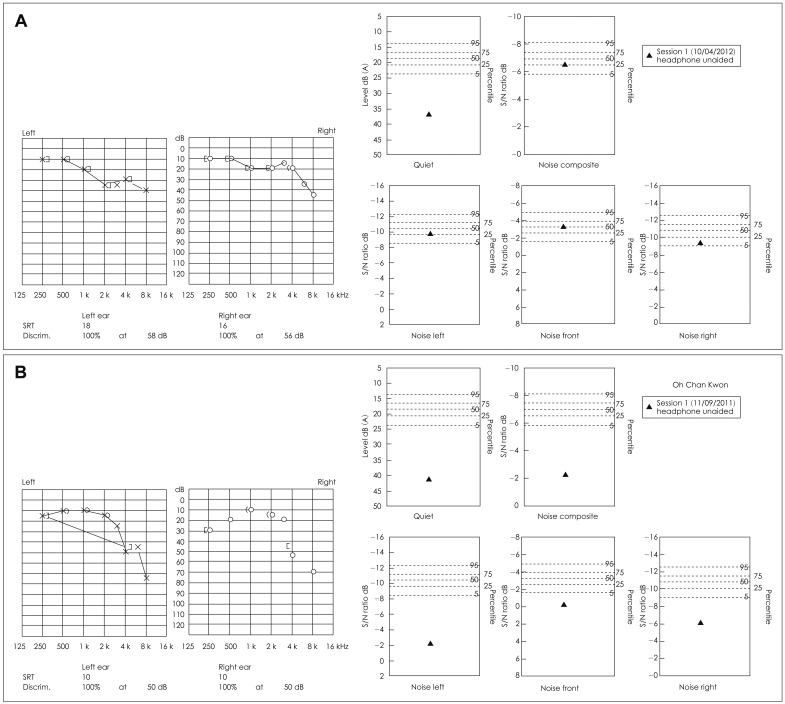
In patients with presbycusis, the ability to hear sounds and process speech is impaired as there is lack of coordination between the peripheral hearing organs and the brain. Conventional hearing tests such as the pure tone test do not accurately measure the hearing ability; and more importantly, these tests do not quantify the degree of difficulty which the patients with presbycusis encounter in their daily life.7) For an accurate hearing testing, the ability to recognize speech in noise needs to be measured. Hence, hearing in noise test (HINT), a modified version of speech audiometry test, was developed. HINT is designed to measure a person's ability to hear a brief conversational sentence in both quiet and noisy environments, and to compare the results with the standard (Fig. 1). The degree of hearing impairment in patients with presbycusis is quantified using a translated version of HINT, and the effects of hearing rehabilitation programs are assessed based on the results.8) However, more caution is required while applying this tool in rehabilitation, given that the HINT results can vary among patients with presbycusis despite the common results for the pure tone test.
Fig. 1.
Different results of HINTS between age-related hearing loss patients who have similar pure tone thresholds. A: 65 female, who have no difficulty having a conversation in noise environment. B: 63 male, who have severe difficulty having a conversation in noise environment. HINT: hearing in noise test.
Central auditory processing disorder (CAPD)
The central auditory processing disorder is defined as abnormal responses during auditory processing in the cerebral cortex where sound signals are delivered. As a result, there is an abnormal brain response to the sounds.9) The incidence of central auditory processing disorder (CAPD) is growing in patients with presbycusis who present with different symptoms. For example, the patient's hearing ability deteriorates in background noise even when their hearing level is normal. They may lose the ability to distinguish one sound from the other when they hear two sounds.4) The effects of conventional hearing rehabilitation methods were significantly lower in patients with presbycusis and CAPD. To assess CAPD, speech audiometry is usually performed in a noisy environment and the results are compared with those of the pure tone test. In addition, there is synthetic sentence identification with either an ipsilateral competing message (SSI-ICM) or contralateral competing message (SSI-CCM). SSI-ICM is known to offer a higher level of sensitivity.10,11) Frequency and duration pattern tests and dichotic tests were recently developed as new assessment tools for CAPD in South Korea. By using these tools, researchers can improve their understanding of cognitive disorders in patients with presbycusis.12)
Mental disorder test
Patients with hearing loss are prone to have mental disorders, depression, social stress, isolation and persecutory delusions.13,14) An earlier study suggested that 42% of patients with hearing loss needed psychological support and treatment, thereby signifying the need for measuring mental disorders in patients with presbycusis.15) The prevalence of depression and isolation is particularly high among patients with presbycusis. A translated version of the Beck Depression Inventory can be used for treatment of depression along with hearing rehabilitation. In developed countries, self-administered questionnaires are used to collect the information on hearing-related disabilities, and the collected data are quantified and applied to hearing rehabilitation.13,16) Translated versions of the Hearing Handicap Inventory for the Elderly (HHIE)17) and the HHIE-screening18) are used for evaluating mental disorders in patients with presbycusis.
Conclusion
The diagnosis of presbycusis is based on medical history, physical examination and hearing test. However, the typical approach of diagnosis of presbycusis followed by providing hearing aids and rehabilitation interventions does not guarantee that patients will be able to attend family and social life without any problems. To more accurately diagnose the condition of patients with presbycusis and to provide successful rehabilitation programs, CAPD and mental disorder tests should be performed along with the basic hearing tests. Any training program for the family members of patients can also be considered for improving the psychological wellbeing of patients with presbycusis.
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MEST)(2010-0023182).
References
- 1.Fransen E, Lemkens N, Van Laer L, Van Camp G. Age-related hearing impairment (ARHI): environmental risk factors and genetic prospects. Exp Gerontol. 2003;38:353–359. doi: 10.1016/s0531-5565(03)00032-9. [DOI] [PubMed] [Google Scholar]
- 2.Lowell SH, Paparella MM. Presbycusis: what is it? Laryngoscope. 1977;87(10 Pt 1):1710–1717. doi: 10.1288/00005537-197710000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Schuknecht HF. Further observations on the pathology of presbycusis. Arch Otolaryngol. 1964;80:369–382. doi: 10.1001/archotol.1964.00750040381003. [DOI] [PubMed] [Google Scholar]
- 4.Golding M, Taylor A, Cupples L, Mitchell P. Odds of demonstrating auditory processing abnormality in the average older adult: the Blue Mountains Hearing Study. Ear Hear. 2006;27:129–138. doi: 10.1097/01.aud.0000202328.19037.ff. [DOI] [PubMed] [Google Scholar]
- 5.Eekhof JA, de Bock GH, de Laat JA, Dap R, Schaapveld K, Springer MP. The whispered voice: the best test for screening for hearing impairment in general practice? Br J Gen Pract. 1996;46:473–474. [PMC free article] [PubMed] [Google Scholar]
- 6.Schubert K. [A new audiometer and results obtained with its use] Z Laryngol Rhinol Otol. 1951;30:11–26. [PubMed] [Google Scholar]
- 7.Guide for the evaluation of hearing handicap. JAMA. 1979;241:2055–2059. [PubMed] [Google Scholar]
- 8.Moon SK, Mun HA, Jung HK, Soli SD, Lee JH, Park K. Development of sentences for Korean Hearing in Noise Test (KHINT) Korean J Otolaryngol-Head Neck Surg. 2005;48:724–728. [Google Scholar]
- 9.Chung JW, Ahn JH. Central auditory processing disorder. Korean J Otolaryngol-Head Neck Surg. 2005;48:696–700. [Google Scholar]
- 10.Jerger J. Audiological findings in aging. Adv Otorhinolaryngol. 1973;20:115–124. [PubMed] [Google Scholar]
- 11.Gates GA, Karzon RK, Garcia P, Peterein J, Storandt M, Morris JC, et al. Auditory dysfunction in aging and senile dementia of the Alzheimer's type. Arch Neurol. 1995;52:626–634. doi: 10.1001/archneur.1995.00540300108020. [DOI] [PubMed] [Google Scholar]
- 12.Han MW, Ahn JH, Chung JW. The application of diagnostic tools of central auditory processing disorder and their normative value in each age group in Korean. Korean J Otorhinolaryngol-Head Neck Surg. 2008;51:694–698. [Google Scholar]
- 13.Rosen JK. Psychological and social aspects of the evaluation of acquired hearing impairment. Audiology. 1979;18:238–252. doi: 10.3109/00206097909081526. [DOI] [PubMed] [Google Scholar]
- 14.Jones EM, White AJ. Mental health and acquired hearing impairment: a review. Br J Audiol. 1990;24:3–9. doi: 10.3109/03005369009077837. [DOI] [PubMed] [Google Scholar]
- 15.McKenna L, Hallam RS, Hinchcliffe R. The prevalence of psychological disturbance in neurotology outpatients. Clin Otolaryngol Allied Sci. 1991;16:452–456. doi: 10.1111/j.1365-2273.1991.tb01038.x. [DOI] [PubMed] [Google Scholar]
- 16.Ventry IM, Weinstein BE. The hearing handicap inventory for the elderly: a new tool. Ear Hear. 1982;3:128–134. doi: 10.1097/00003446-198205000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Park SN, Han GC, Cho YS, Byun JY, Shin JE, Chu HS, et al. Standardization for a Korean version of hearing handicap inventory for the elderly. Korean J Otorhinolaryngol-Head Neck Surg. 2011;54:828–834. [Google Scholar]
- 18.Kim YS, Won CW, Kim BS, Choi HR, Kim SH, Kim JC, et al. Usability of HHIE S as a screening test of hearing imairment in the Korean elderly. J Korean Acad Fam Med. 2001;22:878–885. [Google Scholar]