Abstract
The more consistently someone records their food intake the more likely they are to lose weight. We hypothesized that subjects who kept track via their preferred method would demonstrate higher adherence and therefore improved outcomes compared to those who used a non-preferred method. Participants were randomly assigned to use a paper, PDA, or Web-based diary and classified as “Preferred” if they used their preferred method and “Non-Preferred” if they did not. Days adherent to diary use were collected for 12 weeks. Weight, % body fat, waist circumference, and self-efficacy scores were measured at baseline, 6 and 12 weeks. Thirty nine participants completed the 12 week study. Fifty nine percent were male. The mean age was 35 and mean baseline BMI was 33 kg/m2 (±3.5). Forty four % (n=17) used their “Preferred” diary method and 56% (n=22) did not. Participants who used their preferred diary were more adherent to recording both food intake (64.2% vs. 43.4%, p=.015) and exercise (60.6% vs. 31.2%, p=.001). Though no difference was seen between groups on weight management outcomes, these results suggest that diary preference affects adherence to diary use.
Keywords: Choice, Preference, Weight management, Self-monitoring, Diaries, Adherence, Self-efficacy
1. Introduction
Poor clinical and behavioral outcomes are often the result of poor adherence to therapeutic and behavioral regimens. Research suggests that treatment outcomes may be improved if patients perceive greater control over their treatment choice (Legg England & Evans, 1992). It is well described in education literature that providing choice can be a powerful instructional strategy (Seibert, 2008). According to the self-determination theory (Deci & Ryan, 2000), choice should be relevant to the students’ interest and goals (autonomy support), not be too numerous or complex (competence support), and be congruent with their cultural values (relatedness support) (Katz & Assor, 2007). A meta-analysis of 41 studies that tested the effect of providing choice on intrinsic motivation found when individuals are allowed to affirm their sense of autonomy through choice they experience enhanced motivation, persistence, performance and production (Patall, Cooper, & Robinson, 2008). Therefore providing choices may be an important tool to promote adherence. Providing patients with a choice of medication (Montgomery, Harding, & Fahey, 2001; Protheroe, Fahey, Montgomery, & Peters, 2000; Qaseem, Snow, Denberg, Forciea, & Owens, 2008; Reginster, Rabenda, & Neuprez, 2006; Rennie, Bothamley, Engova, & Bates, 2007), diet (Burke, Choo et al., 2006; Lutes et al., 2008), and treatment modalities for cervical neoplasia (Hartz & Fenaughty, 2001), insomnia (Vincent & Lionberg, 2001), and depression (Dwight-Johnson, Unutzer, Sherbourne, Tang, & Wells, 2001) have resulted in mixed outcomes. However most of the findings suggest the need for further research is needed in this area. To date, no research has been published exploring the effect of food/exercise diary choice on weight management adherence patterns and outcomes.
Currently the three most common ways to self-monitor energy intake and expenditure are: Paper diary, hand-held electronic diary (PDA) and Web-based diary. Maintaining detailed records on specific behaviors, is considered one of the most essential features of behavior therapy (Baker & Kirschenbaum, 1993; Berkel, Poston, Reeves, & Foreyt, 2005; Fabricatore, 2007; Shay, 2008) and consistent self-monitoring has been associated with improved adherence to dietary measures,(Schnoll & Zimmerman, 2001; Yancy & Boan, 2006) although accuracy is generally poor (Goris, Westerterp-Plantenga, & Westerterp, 2000; Livingstone & Black, 2003; Schaefer et al., 2000; Stone, Shiffman, Schwartz, Broderick, & Hufford, 2003). Because a positive effect is also seen without accurate recording (Blundell & Gillett, 2001; Boutelle & Kirschenbaum, 1998; Boutelle, Kirschenbaum, Baker, & Mitchell, 1999; Goris et al., 2000; Guare et al., 1989; Hollis et al., 2008; Kruger, Blanck, & Gillespie, 2006; Rosenthal & Marx, 1983; Sandifer & Buchanan, 1983; Sperduto, Thompson, & O’Brien, 1986; Stalonas & Kirschenbaum, 1985), it is likely that accuracy is not as important as consistently focusing attention on the behavior (Helsel, Jakicic, & Otto, 2007). The more consistently individuals self-monitor their daily energy balance the more weight they lose(Baker & Kirschenbaum, 1993; Boutelle & Kirschenbaum, 1998; Burke et al., 2008; Helsel et al., 2007; Hollis et al., 2008; Wadden et al., 2005) Unfortunately low adherence rates due to the tedious nature of keeping a detailed food diary is well known (Baker & Kirschenbaum, 1993; Burke, Sereika et al., 2006). One contributing factor to low adherence rates may be the lack of choice in the type of food/exercise diary used. Weight management programs generally instruct all attendees to use the same type of diary. Because individuals often have different learning styles they may have different diary prefer ences. For example, some individuals prefer to use a Web-based diary while others prefer a paper diary or a portable electronic device such as a personal digital assistant (PDA). Of the three methods, the PDA diary provides both portable access to nutrition and exercise information and rapid computerized data entry. The paper diary is portable but not automated and the Web-based diaries provide rapid computerized data entry but are not particularly portable. The purpose of this article is to report the findings on food/exercise diary preference in relation to adherence patterns, self-efficacy and change in body composition. We hypothesized that subjects who kept records via a preferred method would demonstrate higher adherence and therefore improved outcomes compared to those who used a non preferred method.
2. Methods
Prior to randomization, each participant was asked what diary they would prefer to use. Participants were then randomly assigned to use a paper and pencil, PDA, or Web-based diary for energy self monitoring. After using their assigned diary for 12 weeks, participants were again asked which diary they preferred to use. For the purpose of this analysis, participants were classified as “Preferred” or “Non Preferred” based on whether or not they used the diary they preferred for the 12 weeks of the study. The Preferred group consisted of participants who reported using the diary they preferred at the end of 12 weeks and the Non-preferred group consisted of participants who reported that they did not use the diary method they preferred at the end of 12 weeks.
2.1. Participants
All study participants were active duty military members with a BMI≥25.0 kg/m2. According to the 2003 Institute of Medicine report on military weight management, the epidemic of overweight and obesity has become a major threat to the long-term welfare and readiness of the United States (U.S.) military forces (IOM, 2004) Results from the National Quality Management Project in 2002 found Navy active duty to have the highest obesity rates (19.3%) of all the military services (NQMP, 2003). As of 2006, failure to meet the Navy’s Physical Readiness Program standards three times over four years is grounds for mandatory separation(“OPNAVINST 6110.1H CH-1, 2006). All Navy active duty are required to complete the Navy Physical Fitness Assessment (PFA) and a Body Composition Assessment (BCA) every 6 months (OPNAV Instruction 6110.1H, 2005). Service members who do not pass the BCA are required to read and complete the Navy Nutrition and Weight Control Self-Study Guide (NAVPERS 15602A, 1996) and establish a healthy diet or attend ShipShape, the Bureau of Medicine and Surgery (BUMED)-approved weight management program for the Navy and Marine Corps (http://www-nehc.mednavy.mil/HP/Shipshape/Overview.htm). All participants had to be enrolled in the 8-week ShipShape Navy weight management program with no planned travel away from the area for greater than 2 weeks over the 12 week study period.
2.2. Study setting
The study took place at a large east coast naval hospital as part of the ShipShape weight management program. ShipShape consists of eight sessions: (1) Orientation; (2) Guidelines for Success; (3) Nutrition Facts and Fallacies; (4) Move your Body; (5) Making Healthy Choices; (6) Building Your Support Team & Listening to Your Body’s Language; (7) Stress Management & Emotional Eating; and (8) Long-term success. The sessions last 90 min and are taught once a week. Subjects are instructed to record their energy intake and expenditure using a paper diary and to maintain a total energy balance of 1200–1500 kcal/day for women and 1800–2000 kcal/day for men in order to achieve an overall weight loss goal of 1 to 2 lb (0.45 kg–0.9 kg) per week and, due to health reasons, never go below 800 kcal in a day and spread a days worth of kilocalories over several small meals. Over the study timeframe, three different ShipShape instructors taught the 8-week course. Two of the instructors were registered dietitians and one was a health educator. The class materials and lectures were the same for all three instructors and for all sessions. IRB approval was obtained from the Principal Investigator’s (PI) University IRB and the Navy IRB prior to subject contact. Initial contact of potential study participants was made by the PI during the first ShipShape class of each cycle. Recruitment for the study began in January 2007 and ended in August 2008.
2.3. Procedure
The length of the study was 12 weeks. All the ShipShape attendees were given an overview of the study at baseline including a detailed description of each of the diaries, the types of body composition measurements, the questionnaires and the number of study visits. Attendees were also told that ShipShape instructs everyone to keep track of their food intake and exercise using a paper diary. To avoid any possible labeling or bias effect, the purpose of the study was described as a way to evaluate the paper diary, the PDA diary and the Web-based diary in order to determine if one type of diary will work better to help ShipShape attendees keep track of their daily food intake and exercise. They were told that if they agreed to be in the study they would not have a choice as to which diary they used and that the study required each participant to track their energy intake and expenditure for 12 weeks; 6 weeks while attending ShipShape and 6 weeks on their own. Participants who agreed to participate in the study were asked to read and sign the informed consent. Each participant was then randomly assigned to one of the three diary groups. The sample was stratified by gender and women and men were randomized separately. Participants were asked to write their initials onto a piece of paper. The papers were collected and divided into two groups: male and female. The papers from each group were placed into separate hats and as the participant initials were selected they were randomly assigned a diary method.
Each participant was given instructions on how to record their food, beverage and exercise using their assigned diary. They were also provided with a detailed handout with the same information. Participants were instructed as follows. Exercise: Participants were to record all structured physical activity. For days that they chose not to participate in structured exercise they were instructed to enter 10 min of walking to account for their daily activity. Days in which participants recorded at least one structured exercise activity or 10 min of walking were considered adherent days for monitoring energy output. Food and Beverage: Days in which participants recorded at least 2 food or beverage entries that totaled greater than or equal to 800 kcal were considered adherent days for monitoring energy intake (this definition was based on the instruction ShipShape attendees received: never go below 800 kcal in a day and spread a days worth of kilocalories over several small meals). Each participant was instructed to record in their diaries for a total of 84 days (12 weeks). Each week for weeks 1–6 and at week 12, study participants were asked to fill out a Diary Questionnaire designed to assess the average timing for recording the food and exercise information and to inquire if they had difficulties using their diary and if other diary methods were employed. Participants were instructed to make their diary entries as close to the time of the activity as possible. Participants who reported entering information right before the activity, right after the activity, or 1–3 h after the activity were considered adherent to entering information close to the time of the activity. Those who selected other options (e.g., at the end of the day, the next day) were considered non-adherent.
Participants were asked to formally start tracking their energy intake and expenditure after the second ShipShape class as the first two weeks were used to gain familiarity with their assigned diary. Participants were also asked to bring in their diary reports to each class and on the last study visit at Week 12. For the paper diary group, this report was the actual diary; for the Web-based diary group, a printout of the diary records was obtained by the PI who had administrative oversight of the Web-based group; and for the PDA diary group, the information was stored in the PDA which was transcribed onto paper during class by the PI and associate investigators. Each participant’s diary information was collected weekly for 6 weeks which corresponded to the ShipShape program and then once at week 12 to reflect the activity for weeks 7–12 during which the participants were on their own without weekly sessions. Copies of the diary information during the weeks participants attended Shipshape were given to the instructor so feedback and dietary recommendations could be provided, a standard practice for all ShipShape attendees. At the follow-up session (week 12), participants were asked to fill out a Follow-up Questionnaire which asked them to evaluate their assigned diary.
2.4. Intervention
The intervention for this study is the self-monitoring method: (1) paper diary, (2) Web-based diary, and (3) PDA diary. All of the diaries were purchased from one company: Calorie King (http://www.calorieking.com, Family Health Network, Costa Mesa, CA). Each method provided the participants with the same detailed nutrition information (a database containing the USDA nutrient values of more than 45,000 food and beverage items including restaurant food) eliminating the bias of one diary method providing more information than another. The paper diary group received a pocket-sized paper diary, a 302 page pocket-sized paperback containing the calorie, fat and carbohydrate information found in the PDA and Web software and a laminated card listing common exercises and the number of kilocalories expended with 30 min of activity based on a target bodyweight of either: 150,175, or 200 lb. The Web diary group and the PDA diary group received the nutrition and exercise information from the diary software. The Web diary group received a membership to the Calorie King on-line weight management and exercise program that could be accessed through any computer with Internet service. The PDA diary group received a Tungsten/e2 Palm™ with the Calorie King Palm OS program installed.
2.5. Measurements
Once the informed consent had been signed and witnessed, anthropometric measures were obtained. These include body weight, estimated % body fat and waist circumference. All participants were measured on the same digital Seca™ scale without shoes. The estimated % body fat was obtained from a bioelectrical impedance assessment (BIA) using the Tanita® BF 350 bioelectrical impedance machine. Weight was validated at week 0, 6 and 12 when two weights were obtained (1) with the digital Seca™ scale and (2) with the Tanita® BF 350 bioelectrical impedance machine. Waist circumference was measured using a Gulick II tape measure with the participant standing and the tape measure at the level of the umbilicus at normal minimal inspiration(NHLBI, 2000). Height was based on self-report of their official military record. Body Mass Index was calculated by dividing a subject’s weight in kilograms by the square of his/her height in meters (kilograms per meter squared)(NHLBI, 2000).
2.6. Questionnaires
In addition to the weekly Diary Questionnaire and the 12 week Follow-up Questionnaire, the participants were asked to fill out a demographic questionnaire at baseline and the Weight Efficacy LifeStyle (WEL) questionnaire at baseline, week 6 and week 12. The demographic questionnaire contained questions related to age, gender, race, ethnicity, prior attempts at weight loss and a question asking participants to select the diary they would like to use if they were given a choice.
The Weight Efficacy Life-Style (WEL) questionnaire (WEL), developed by Clark, Abrams, Niaura, Eaton, & Rossi (Clark, Abrams, Niaura, Eaton, & Rossi, 1991; Wolff & Clark, 2001), was designed to measure self-efficacy in relation to weight management and has been frequently used to evaluate self-efficacy as an outcome measure (Clark, Cargill, Medeiros, & Pera, 1996; Dutton, Martin, Rhode, & Brantley, 2004; Pinto, Clark, Cruess, Szymanski, & Pera, 1999; Wolff & Clark, 2001). The WEL is a 20-item Likert scale that consists of a total score and five situational factors. The total score and each factor is a continuous variable; the higher the score (maximum 180), the higher the level of self-efficacy. The WEL demonstrates high reliability with an internal consistency ranging from 0.76 to 0.90 (Clark et al., 1991; Clark et al., 1996). The WEL has not been used in the military population, which has a higher proportion of men then most weight management programs. The internal consistency coefficient (Cronbach’s α) for this sample was 0.92 at baseline and 0.93 at weeks 6 and 0.80 at week 12.
2.7. Statistical analysis
Statistical Package for the Social Scientist (SPSS) version 16.0 version for Windows (SPSS, Inc., Chicago, IL) was used for all analyses. Chi-square (for categorical dependent measures) and one-way ANOVAs (for continuous dependent measures) were used to evaluate baseline group differences. Independent t-tests were used to evaluate baseline group differences between 12 week-completers and non-completers and between the Preference group and Non-Preference group. Repeated measures (RM) ANOVAs were performed on the following outcome measures: change in weight (kg), estimated % body fat, waist circumference (inches), self-efficacy score (WEL) and number of days entered food/exercise information from baseline to week 6 and from baseline to week 12. Type of diary (paper, web, or PDA) was treated as the between subject factor and time the within-subject factor. If significant differences were found between groups for any outcome analyzed, post-hoc testing was performed. If the assumptions of ANOVA were not met then appropriate non-parametric tests were performed. All p-values were based on a 2-tailed test with alpha set at the .025 significance level to account for familywise alpha inflation that can occur from doing multiple comparisons. Correlation analyses were performed to examine relationships between number of days recording food intake and weight loss and number of days recording exercise and weight loss. An analysis of adherence patterns to timing of data entry was also conducted, as well as a review of the narrative data.
3. Results
3.1. Sample
A total of 73 participants were enrolled into the study, with 39 finishing the study through 12 weeks, resulting in a completion rate of 53%. The primary reasons for participant dropout were inability to attend ShipShape as originally planned (n=19), unanticipated deployments/transfers (n=5), and pregnancy (n=2). Completers (n=39) were compared to dropouts (n=34) on demographic variables to ascertain if there was differential attrition. The participant demographics and characteristics, including random assignment to diary preference, were not statistically significantly different between the 12 week completers and the drop-outs, lending support to the hypothesis that there was no differential attrition from the study.
3.2. Diary preference
Of the 39 participants who completed the study, 12 (31%) were randomly assigned the diary they preferred and 27 (69%) were not. The baseline diary preferences were as follows: 13 (33%) Paper-pencil, 13 (33%) PDA, and 13 (33%) Web-based diary. At week 12 the diary preferences changed to the following: 10 (26%) Paper-pencil, 14 (36%) PDA, and 15 (38%) Web-based diary. For the purpose of this analysis, participants were classified as “Preferred” or “Non-Preferred” based on whether or not they used a diary they preferred to use at the end of 12 weeks. See Fig. 1. Participant demographics and characteristics were statistically significantly different between the Preferred-group and Non-Preferred group for baseline BMI (p=.003) with the Preferred-group having a higher average BMI (34.8, SD=3.5 vs. 31.7, SD=2.7). There was also a statistically significant difference in the number of prior weight loss attempts where 59% of the Preferred-group reported greater than 6 weight loss attempts and only 9% of the Non-Preferred-group reported greater then 6 weight loss attempts (χ=13.0, p=.011). The remaining demographics and baseline characteristics were not statistically significantly different between the groups. See Table 1 for baseline characteristics, body composition, and WEL score.
Fig. 1.
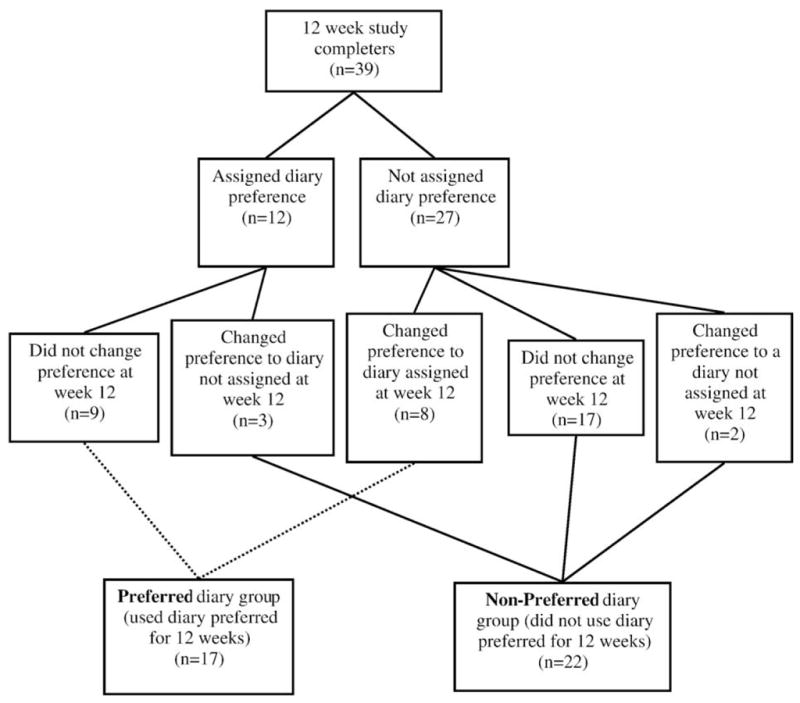
Preference vs. non-preference group assignment.
Table 1.
Description of study participants by group and overall using either percent and sample size [% (n)] or mean ± SD.
| Pref (N=17) | Non-Pref (N=22) | Overall (N=39) | |
|---|---|---|---|
| Demographics % (n) | |||
| Gender (male) | 65% (11) | 54% (12) | 59% (23) |
| Race (white) | 53% (9) | 63% (14) | 59% (23) |
| Ethnicity (non-Hispanic) | 88% (15) | 90% (20) | 90% (35) |
| Rank (enlisted) | 70% (12) | 72% (16) | 72% (28) |
| Education (HS/GED only) | 35% (6) | 55% (12) | 46% (18) |
| Housing (off-base) | 88% (15) | 86% (19) | 87% (34) |
| Marital Status (married) | 59% (10) | 50% (11) | 54% (21) |
| Age mean (±SD) | 35.00 (±7) | 35.60 (±11) | 35.33 (±9.3) |
| Health Patterns % (n) | |||
| Weight problem (Yes as child) | 35% (6) | 27% (6) | 31% (12) |
| Weight problem (Yes family) | 59% (10) | 77% (17) | 70% (27) |
| Prior wt loss attempts | |||
| None | 6% (1) | 4% (1) | 5% (2) |
| ≤6 attempts | 35% (6)a | 86% (19)a | 64% (25) |
| >6 attempts | 59% (10)a | 9% (2)a | 31%(12) |
| Days eat out per week | |||
| None | 12% (2) | 5% (1) | 7% (3) |
| 1–3 per wk | 71% (12) | 73% (16) | 72% (28) |
| 4–7 per wk | 6% (1) | 18% (4) | 13% (5) |
| >7 per wk | 12% (2) | 4% (1) | 7% (3) |
| Health | |||
| Excellent/very good | 35% (6) | 41% (9) | 38% (15) |
| Fair/poor | 59% (10) | 59% (13) | 59%(23) |
| Outcome measures mean (±SD) | |||
| BMI | 34.8 (±3.5)b | 31.7 (±2.7)b | 33.0 (±3.4) |
| % Body fat | 35.6 (±7.5) | 34.5 (±7.1) | 34.9 (±7.3) |
| Waist circumference | 42.6 (±5) | 39.8 (±3.5) | 41.0 (±4.4) |
| WEL score | 117.2 (±27.6) | 114.2 (±32.1) | 115.5 (±29.9) |
Pearson chi-square p<.025.
t-test p<.025.
3.3. Body composition
A mixed between–within subjects analysis of variance was conducted to assess the impact of diary preference on participants’ weight, estimated % body fat (BF), and waist circumference from baseline to week 6 and baseline to week 12. There was no significant interaction between diary preference and time for any of the three variables (F(2,36)=.10, p=.90 for weight, F(2,36)=.92, p=.40 for % BF, and F (2,36)=1.8, p=.18 for waist circumference). There was a substantial main effect for time for all body composition measures (p≤.001) with the sample as a whole showing a decrease in weight, estimated %BF, and waist circumference from baseline to 6 weeks and from baseline to 12 weeks. However, the majority of weight loss took place by week 6 during the class. When participants were not attending the weekly weight management classes (week 7–week 12), there was no change in body composition for weight loss (−0.3 kg, p=.34), % BF (−0.5%, p=. 17), or waist circumference, (−0.6 inches, p=.04). Overall at week 12 subjects as a whole demonstrated a significant decrease in weight (−2.8 kg., p<.001), waist circumference (−2.2 in., p<.001) and estimated percent body fat (−1.6%, p<.001). The omnibus main effect comparing those who used the diary they preferred compared to those who did not was not significant for a difference between groups on change in weight (F (1,37)=.029, p=.87), % BF (F(1,37)=1.3, p=.26), or waist circumference (F(1,37)=1.1, p=.30) at week 6 nor at week 12 suggesting no difference in the effect of diary preference on changes in body composition. See Table 2 for a description of change in weight, body fat and waist circumference.
Table 2.
Change in body composition and self-efficacy (WEL) scores from baseline to 6 weeks, 6 weeks to 12 weeks, and baseline to 12 weeks given as means ± SD.
| Interval change | Pref (N=17) | Non-Pref (N=22) | Overall (N=39) |
|---|---|---|---|
| Weight (kg) | |||
| Baseline to 6 wks | −2.3±2.5 | −2.5±2.8 | −2.4±2.7 |
| 6 wks to 12 wks | −0.4±2.4 | −0.3±1.2 | −0.3±2.2 |
| Total (0–12 wks) | −2.7±3.9 | −2.8±3.9 | −2.7±3.9 |
| Body fat (%) | |||
| Baseline to 6 wks | −0.6±1.7 | −1.5±2.0 | −1.1±1.9 |
| 6 wks to 12 wks | −0.6±2.0 | −0.4±2.3 | −0.5±2.1 |
| Total (0–12 wks) | −1.2±2.3 | −1.9±2.8 | −1.6±2.6 |
| Waist circumference (inches) | |||
| Baseline to 6 wks | −1.1±1.3 | −2.0±1.9 | −1.6±1.7 |
| 6 wks to 12 wks | −1.0±2.3 | −0.3±1.5 | −0.6±1.9 |
| Total (0–12 wks) | −2.1±2.4 | −2.3±2.2 | −2.2±2.2 |
| Total WEL score | |||
| Baseline to 6 wks | +17.6±23.2 | +29.0±28.2 | +24.0±26.5 |
| 6 wks to 12 wks | −2.7±19.9 | +0.3±18.9 | −1.0±19.1 |
| Total (0–12 wks) | +14.9±24.7 | +29.3±24.6 | +23.0±25.4 |
p<.025 between baseline and week 6 and baseline and week 12 for all comparisons.
p>.05 between 6 wks to 12 wks.
p>.05 for all between group comparisons.
3.4. Self-efficacy
Both groups reported fairly high baseline total WEL scores. Out of a possible score of 180 (the higher the score the higher the level of self-efficacy) the average baseline score was 115, SD=30 (Median=121). A mixed between–within subjects analysis of variance was conducted to assess the impact of diary preference on participants total WEL score from baseline to week 6 and baseline to week 12. There was no significant interaction between diary preference and time (F(2,36)= 1.6, p=.21). There was a substantial main effect for time (F(2,36)=17.4, p<.001) with an overall increase in WEL score from baseline to 6 weeks and from baseline to 12 weeks. However, when participants were not attending the weekly weight management classes (week 7–week 12), there was no significant increase in WEL scores (p=.70). See change in WEL scores in Table 2. The main effect comparing the two groups was not significant for change in WEL score at week 6 and week 12 (F(1,37)=2.9, p=.10) suggesting no difference in the effect of diary preference on self-efficacy. There was no significant correlation between change in WEL score and change in weight in the first 6 weeks when most weight loss occurred (r=.077, p=.64).
3.5. Adherence patterns
For those who completed the 84-day study (12 weeks), the average number of days participants adhered to using the diary to enter food items was 44 days, SD=23 (Median=41) and to enter exercise information was 37 days, SD=24 (Median=37). A mixed between–within subjects analysis of variance was conducted to assess the impact of diary preference on participant diary entry adherence from week 1 to week 6 and week 7 to week 12. There was no significant interaction between diary preference and time for either food entries (F(1,37)=.77, p=.38) or exercise entries (F(1,37)=1.4, p=.24). There was a substantial main effect for time (p<.001) with both groups showing a decrease in food and exercise entries over time (Table 3). The main effect comparing the two groups was significant for food entries (F(1,37)=6.3, p=.02) and for exercise entries (F(1,37)=12.8, p=.001) suggesting the group using the diary they preferred made significantly greater number of food and exercise entries with the greatest difference occurring in the last 6 weeks when participants were not attending the weekly weight management classes. See change in adherence patterns in Table 3.
Table 3.
Percentage of participants adherent to diary entry and timing of diary entry by group and overall.
| Adherence variable | Pref (%) | Non-Pref (%) | Overall (%) | |
|---|---|---|---|---|
| Food report | % days adherent to entry | |||
| Week 1–6 | 79 | 63 | 70 | |
| Week 7–12 | 49 | 25 | 36 | |
| Total week 1–12 | 64a | 43a | 52 | |
| % of time adherent to entry timing | ||||
| Week 1–6 | 71 | 41 | 54 | |
| Week 7–12 | 47a | 9a | 26 | |
| Exercise report | % days adherent to entry | |||
| Week 1–6 | 73a | 50a | 60 | |
| Week 7–12 | 47a | 15a | 29 | |
| Total week 1–12 | 60a | 32a | 44 | |
| % of time adherent to entry timing | ||||
| Week 1–6 | 65 | 32 | 46 | |
| Week 7–12 | 47a | 5a | 23 | |
p<.025 between baseline and week 6 and baseline and week 12 for all comparisons.
p<.025 between week 1–6 and week 7–12 for all comparisons.
Note:
Sample size varies as weeks class not attended data on diary entry timing not collected.
Adherent food entry day=At least 2 food or beverage entries that totaled >800 kcal.
Adherent exercise entry day=At least one exercise or lack of exercise event recorded.
Adherent timing of food/exercise entry=Right before or within 3 h after.
p<.025 between groups.
The relationship between the total number of days adherent to recording food intake into the diaries and weight loss from week 0–week 6 and week 0–week 12 demonstrated a moderate negative correlation between the weight change and recording food intake (r=−.40, p=0.013 week 6 and r=−.37, p=0.021 week 12). The relationship between the total number of days adherent to recording exercise into the diaries and total weight change from week 0–week 6 and week 0–week 12 demonstrated a small correlation between variables without significance (r=−.27, p=0.10 at week 6 and r=−.27, p=0.10 at week 12). No significant correlation was found with the number of days entered food/exercise over the last 6 weeks and weight change at week 12 (r=−.24, p=0.071 food and r=−.27, p=0.09 exercise).
Based on the self-reported information in the week 1–6 Food Diary Questionnaires, 54% of the participants reported that for the majority of the time they entered their food items close to the time of consumption (adherent food entry timing), and 46% recorded their exercise close to the time of the activity (adherent exercise entry timing). Data from the final Food Diary Questionnaires which captured diary entry patterns over the last 6 weeks of the study, showed a significant decrease in these percentages with a statistically significant difference between groups (9% adherent food entry timing as compared to 47%, χ=9.26, p=.002, and 5% adherent exercise timing as compared to 47%, χ=11.3, p=.001) suggesting greater adherent diary entry timing in the group who used the diary they preferred for the last 6 weeks of the study when they were not attending the weight management class. See adherence data in Table 3.
3.6. Comparisons between the three diary methods
Analyses between the three diary methods were also performed. No statistically significant differences were found. The data are presented in Table 4 for base line demographics, body composition and WEL scores; Table 5 for changes in body composition and WEL scores; and Table 6 for differences in adherence patterns.
Table 4.
Description of study participants by dairy method and overall using either percent and sample size [% (n)] or mean ± SD.
| Paper-pencil (n=13) | PDA (n=14) | Web (n=12) | Overall (N=39) | |
|---|---|---|---|---|
| Demographics | ||||
| Gender (male) | 54% (7) | 50% (7) | 75% (9) | 59% (23) |
| Race (white) | 61% (8) | 64% (9) | 50% (6) | 59% (23) |
| Ethnicity (non-Hispanic) | 100% (13) | 93% (13) | 75% (9) | 90% (35) |
| Rank (enlisted) | 69% (9) | 71% (10) | 75% (9) | 72% (28) |
| Education (HS/GED only) | 46% (6) | 57% (8) | 33% (4) | 46% (18) |
| Housing (off-base) | 85% (11) | 93% (13) | 83% (10) | 87% (33) |
| Marital status (married) | 38% (5) | 57% (8) | 67% (8) | 54% (21) |
| Age (mean ± SD) | 36.5±9.63 | 34.00±8.51 | 35.67±10.52 | 35.33±9.3 |
| Health patterns | ||||
| Weight problem (yes as child) | 38% (5) | 43% (6) | 8% (1) | 31% (12) |
| Weight problem (yes family) | 77% (10) | 71% (10) | 58% (7) | 70% (27) |
| Prior wt loss attempts | ||||
| None | 8% (1) | 7% (1) | 0 | 5% (2) |
| ≤6 attempts | 61% (8) | 64% (9) | 67% (8) | 64% (25) |
| >6 attempts | 31% (4) | 29% (4) | 33% (4) | 31%(12) |
| Days eat out per week | ||||
| None | 8% (1) | 7% (1) | 8% (1) | 7% (3) |
| 1–3 per wk | 54% (7) | 93% (13) | 67% (8) | 72% (28) |
| 4–7 per wk | 23% (3) | 0 | 17% (2) | 13% (5) |
| >7 per wk | 15% (2) | 0 | 8% (1) | 7% (3) |
| Health | ||||
| Excellent/very good | 46% (6) | 21% (3) | 50% (6) | 38% (15) |
| Fair/poor | 54% (7) | 77% (11) | 42% (5) | 59%(23) |
| Outcome measures | ||||
| BMI | 32.3±3.0 | 33.9±3.5 | 32.8±3.6 | 33.0±3.5 |
| % Body fat | 36.3±8.1 | 36.4±7.5 | 31.9±5.5 | 34.9±7.3 |
| Waist circumference | 41.0±4.2 | 40.9±4.9 | 41.3±4.5 | 41.0±4.4 |
| WEL score | 121.5±32.4 | 110.7±27.2 | 114.6±31.6 | 115.5±29.9 |
All pairwise comparisons p>.05.
Table 5.
Change in body composition and self-efficacy (WEL) scores from baseline to 6 weeks and baseline to 12 weeks given as means ± SD between diary methods.
| Interval change | Paper-pencil (n=13) | PDA (n=14) | Web (n=12) | Overall (N=39) |
|---|---|---|---|---|
| Weight (kg) | ||||
| Baseline to 6 wks | −2.7±2.9 | −2.4±2.8 | −2.2±2.5 | −2.4±2.7 |
| 6 wks to 12 wks | −0.2±2.6 | −0.5±2.0 | −0.2±2.0 | −0.3±2.2 |
| Total (0–12 wks) | −3.0±3.6 | −2.9±4.3 | −2.4±4.0 | −2.8±3.9 |
| Body fat (%) | ||||
| Baseline to 6wks | −1.1±2.5 | −1.0±1.9 | −1.3±1.3 | −1.1±1.9 |
| 6 wks to 12 wks | −0.9±2.5 | −0.6±1.8 | +0.2±1.9 | −0.5±2.1 |
| Total (0–12 wks) | −2.0±2.9 | −1.6±2.2 | −1.1±2.7 | −1.6±2.6 |
| Waist circumference (inches) | ||||
| Baseline to 6 wks | −1.6±2.1 | −1.6±1.7 | −1.6±1.3 | −1.6±1.7 |
| 6 wks to 12 wks | −1.4±2.4 | −0.3±1.3 | −0.2±1.6 | −0.6±1.9 |
| Total (0–12 wks) | −3.0±1.8 | −1.9±2.6 | −1.7±2.1 | −2.2±2.2 |
| Total WEL score | ||||
| Baseline to 6 wks | +23.6±25.9 | +27.0±31.3 | +21.0±22.6 | +24.0±26.5 |
| 6 wks to 12 wks | +1.4±16.5 | −0.6±21.5 | −4.0±20.0 | −1.0±19.1 |
| Total (0–12 wks) | +25.0±22.9 | +26.4±31.8 | +17.0±19.9 | +23.0±25.4 |
p>.05 for all pairwise comparisons between groups.
p<.025 between baseline and week 6 and baseline and week 12.
p>.05 between 6 wks to 12 wks.
Table 6.
Percentage of participants adherent to diary entry and timing of diary entry by dairy method group and overall.
| Adherence variable | Paper-pencil (%) | PDA (%) | WEB (%) | Overall (%) | |
|---|---|---|---|---|---|
| Food report | % days adherent to entry | ||||
| Week 1–6 | 74 | 78 | 56 | 70 | |
| Week 7–12 | 47 | 36 | 24 | 36 | |
| % of time adherent to entry timing | |||||
| Week 1–6 | 54 | 64 | 42 | 54 | |
| Week 7–12 | 31 | 14 | 33 | 26 | |
| Exercise report | % days adherent to entry | ||||
| Week 1–6 | 62 | 65 | 54 | 60 | |
| Week 7–12 | 28 | 35 | 24 | 29 | |
| % of time adherent to entry timing | |||||
| Week 1–6 | 46 | 57 | 33 | 46 | |
| Week 7–12 | 23 | 21 | 25 | 23 | |
Note:
Sample size varies — for weeks class not attended, data on diary entry timing not collected.
Adherent food entry day=At least 2 food or beverage entries that totaled ≥800 kcal.
Adherent timing of food/exercise entry=Right before or within 3 h after.
Adherent exercise entry day=At least one exercise or lack of exercise event recorded.
4. Discussion
The study did not find a difference in weight management outcomes, self-efficacy and adherence patterns between participants who used different diary methods to self-monitor energy intake and expenditure. However, this study provides data that suggests that diary preference has an affect on adherence to diary use. We hypothesized that subjects who kept records using a preferred diary method (Preferred-group) would demonstrate higher adherence and therefore improved outcomes compared to those who used a non-preferred method (Non-Preferred-group). Though no difference in self-efficacy scores and weight management outcomes was seen between the Preferred-group and the Non-preferred-group, there was a significantly greater number of diary entries made by the Preferred-group with the greatest difference occurring in the last 6 weeks when participants were not attending the weekly weight management classes. In addition, the Preferred-group reported a greater number of entries at or near the time of the food intake and/or activity. There was also a negative correlation between weight loss and the number of days food intake was recorded. This finding is consistent with the literature (Baker & Kirschenbaum, 1993; Boutelle & Kirschenbaum, 1998; Burke et al., 2008; Helsel et al., 2007; Hollis et al., 2008), and further reinforces why self-monitoring is considered the cornerstone of behavior therapy (Baker & Kirschenbaum, 1993; Berkel et al., 2005).
The study had several limitations. Generalizability to other populations may be limited because the sample included only active duty military personnel, 59% of whom were male. Military personnel attending weight management programs differ from the general population in that they tend to have larger numbers of men and a primary reason for attending is often the threat of job loss if fitness and body composition requirements set by the military are not met. In addition, military personnel are often required by their command to attend a weight management program when they exceed body composition standards. This is unlike the civilian population who typically attend weight management programs voluntarily. This may have been a major contributing factor to the non-significance found between the Preferred group and the Non-Preferred group in weight management outcomes. Most of the participants had an urgent need to lose weight before then next Navy fitness test. Therefore despite which diary they used most of the participants lost weight while attending ShipShape. Unfortunately data past the 12 week study was not collected to assess sustainability of this weight loss. A difference in weight loss between the Preference group and the Non-preference group may have been seen if this study had been conducted in a civilian weight management population where the motivation to lose weight is generally not the same for all attendees and often not as urgent.
The number of days participants adhered to recording food intake in their diaries was actually greater than reported in the study. Meal skipping and eating disorders are also common among active duty members who are trying to lose weight prior to taking their fitness tests (Harrow, Cordoves, & Hulette, 2006; Warner et al., 2007). Many diary entries in this study had missing meals and/or showed total daily energy intakes of less then 800 kcal. Adherence rates to diary food entries would have been higher if an adherent day for entering food intake was not defined as at least 2 entries totaling ≥800 kcal based on Shipshape instruction not to consume less then this amount in a day.
The small sample of 12 week completers increased the risk of a Type II error. However the estimated power based on change in weight at 12 weeks (Partial Eta Squared=0.03) was very low indicating that it is unlikely that an effect seen from even a larger sample would have resulted in a clinically meaningful difference in weight loss.
Another limitation of the study was the lack of an electronic time–date stamp for each diary entry. Timely recoding improves accuracy (Burke et al., 2008). Data on timing of diary entry for this study relied on a weekly self-reported average for week 1–6 and the overall average for week 7–12. It is well known that recall is poor and it is preferable to collect data recorded in real time (Burke et al., 2008; Shiffman, Hufford, & Paty, 2001). In studies using paper diaries, subjects often do not consistently complete their diary entries as required but rather fill them out in batches after the fact (“parking lot compliance”) (Hufford, Stone, Shiffman, Schwartz, & Broderick, 2002). Because none of the electronic methods for this study provided a date–time stamp of the entry, and all of the diary data was collected at the end of each week (week 1–6) and at the end of week 12 (week 7–12), the potential for “parking lot compliance” was most likely equal across all groups.
In summary, this study provides support that providing attendees of a weight management program a choice of diary method may improve adherence patterns. It is well described in education literature that providing choice can be a powerful instructional and motivational strategy (Patall et al., 2008; Seibert, 2008). Offering choices, such as the type of diary to use to self-monitor, may be an important motivational tool in weight management programs. The number of times a choice can be made should not be restricted to one. Several of the study participants in this study changed their diary preference over a 12 week timeframe; therefore it may be important to encourage individuals to try different diary methods until they find one method or a combination of methods (e.g. paper-pencil diary plus a web-based diary) that works best for them.
5. Conclusion
Though no difference was seen between groups on outcomes in this study, these results suggest that diary preference affects adherence to recording of entries with increased adherence patterns seen with participants who used the diary they preferred. Further study is suggested given that there are a number of diary options available; providing individuals with a choice may improve adherence which, in turn, may improve weight management outcomes.
Acknowledgments
Role of funding sources
This study was supported financially by a student research allotment from the National Naval Medical Center, Department of Graduate Research and Education (GEAR), Bethesda, Maryland.
We gratefully acknowledge Virginia Giroux, and Dianne Paraoan for their assistance on this project.
Footnotes
Conflict of interest
The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy or position of Uniformed Services University of Health Sciences, the Department of Defense, nor the U.S. Government.
No relationship exists between any of the authors and any commercial entity or product mentioned in this article that might represent a conflict of interest. No inducements have been made by any commercial entity to submit the manuscript for publication.
Contributors
Dr. Shay designed the study and wrote the protocol. Dr. Seibert provided editorial and content support as well as summaries of previous research studies. Dr. Watts conducted the statistical analysis. Dr. Pagliara assisted in generating the data. All authors have approved the final manuscript.
References
- Baker RC, Kirschenbaum DS. Self-monitoring may be necessary for successful weight control. Behavior Therapy. 1993;24:377–394. [Google Scholar]
- Berkel LA, Poston WS, Reeves RS, Foreyt JP. Behavioral interventions for obesity. Journal of the American Dietetic Association. 2005;105(5 Suppl 1):S35–S43. doi: 10.1016/j.jada.2005.02.031. [DOI] [PubMed] [Google Scholar]
- Blundell JE, Gillett A. Control of food intake in the obese. Obesity Research. 2001;9(Suppl 4):263S–270S. doi: 10.1038/oby.2001.129. [DOI] [PubMed] [Google Scholar]
- Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vital component of successful weight control. Obesity Research. 1998;6(3):219–224. doi: 10.1002/j.1550-8528.1998.tb00340.x. [DOI] [PubMed] [Google Scholar]
- Boutelle KN, Kirschenbaum DS, Baker RC, Mitchell ME. How can obese weight controllers minimize weight gain during the high risk holiday season? By self-monitoring very consistently. Health Psychology. 1999;18(4):364–368. doi: 10.1037//0278-6133.18.4.364. [DOI] [PubMed] [Google Scholar]
- Burke LE, Choo J, Music E, Warziski M, Styn MA, Kim Y, Sevick MA. PREFER study: a randomized clinical trial testing treatment preference and two dietary options in behavioral weight management—Rationale, design and baseline characteristics. Contemporary Clinical Trials. 2006;27(1):34–48. doi: 10.1016/j.cct.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Burke LE, Sereika S, Choo J, Warziski M, Music E, Styn M, Novak J, Stone A. Ancillary study to the PREFER trial: a descriptive study of participants’ patterns of self-monitoring—Rationale, design and preliminary experiences. Contemporary Clinical Trials. 2006;27(1):23–33. doi: 10.1016/j.cct.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Burke LE, Sereika SM, Music E, Warziski M, Styn MA, Stone A. Using instrumented paper diaries to document self-monitoring patterns in weight loss. Contemporary Clinical Trials. 2008;29(2):182–193. doi: 10.1016/j.cct.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. Journal of Consulting Clinical Psychology. 1991;59(5):739–744. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- Clark MM, Cargill BR, Medeiros ML, Pera V. Changes in self-efficacy following obesity treatment. Obesity Research. 1996;4(2):179–181. doi: 10.1002/j.1550-8528.1996.tb00531.x. [DOI] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. The ‘what’ and ‘why’ of goal pursuit: Human needs and the self determination theory of behavior. Psychology Inquiry. 2000;11:227–268. [Google Scholar]
- Dutton GR, Martin PD, Rhode PC, Brantley PJ. Use of the weight efficacy lifestyle questionnaire with African American women: Validation and extension of previous findings. Eating Behaviors. 2004;5(4):375–384. doi: 10.1016/j.eatbeh.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Dwight-Johnson M, Unutzer J, Sherbourne C, Tang L, Wells KB. Can quality improvement programs for depression in primary care address patient preferences for treatment? Medical Care. 2001;39(9):934–944. doi: 10.1097/00005650-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Fabricatore AN. Behavior therapy and cognitive-behavioral therapy of obesity: Is there a difference? Journal of the American Dietetic Association. 2007;107(1):92–99. doi: 10.1016/j.jada.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Goris AH, Westerterp-Plantenga MS, Westerterp KR. Undereating and underrecording of habitual food intake in obese men: Selective underreporting of fat intake. American Journal of Clinical Nutrition. 2000;71(1):130–134. doi: 10.1093/ajcn/71.1.130. [DOI] [PubMed] [Google Scholar]
- Guare JC, Wing RR, Marcus MD, Epstein LH, Burton LR, Gooding WE. Analysis of changes in eating behavior and weight loss in type II diabetic patients. Which behaviors to change. Diabetes Care. 1989;12(7):500–503. doi: 10.2337/diacare.12.7.500. [DOI] [PubMed] [Google Scholar]
- Harrow JJ, Cordoves RI, Hulette RB. Attitudes toward intentional weight loss and dietary behavior among U.S. Army reserve soldiers during annual training. Military Medicine. 2006;171(7):678–683. doi: 10.7205/milmed.171.7.678. [DOI] [PubMed] [Google Scholar]
- Hartz LE, Fenaughty AM. Management choice and adherence to follow-up after colposcopy in women with cervical intraepithelial neoplasia 1. Obstetrics and Gynecology. 2001;98(4):674–679. doi: 10.1016/s0029-7844(01)01526-5. [DOI] [PubMed] [Google Scholar]
- Helsel DL, Jakicic JM, Otto AD. Comparison of techniques for self-monitoring eating and exercise behaviors on weight loss in a correspondence-based intervention. Journal of the American Dietetic Association. 2007;107(10):1807–1810. doi: 10.1016/j.jada.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Hollis JF, Gullion CM, Stevens VJ, Brantley PJ, Appel LJ, Ard JD, Champagne CM, Dalcin A, Erlinger TP, Funk K, Laferriere D, Lin PH, Loria CM, Samuel-Hodge C, Vollmer WM, Svetkey LP. Weight loss during the intensive intervention phase of the weight-loss maintenance trial. American Journal of Preventive Medicine. 2008;35(2):118–126. doi: 10.1016/j.amepre.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hufford MR, Stone AA, Shiffman S, Schwartz JE, Broderick JE. Paper vs. electronic diaries: Compliance and subject evaluations. Applied Clinical Trials. 2002;(August):38–43. [Google Scholar]
- IOM. Committee on Military Nutrition Research Food and Nutrition Board. Washington, D.C: The National Academies Press; 2004. Institute of Medicine of the National Academies: Weight management: state of the science and opportunities for military programs: Subcommittee on military weight management. [PubMed] [Google Scholar]
- Katz I, Assor A. When choice motivates and when it does not. Educational Psychology Review. 2007;19:429–442. [Google Scholar]
- Kruger J, Blanck HM, Gillespie C. Dietary and physical activity behaviors among adults successful at weight loss maintenance. International Journal Behavioral Nutrition and Physical Activity. 2006;3(1):17. doi: 10.1186/1479-5868-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legg England S, Evans J. Patients’ choices and perceptions after an invitation to participate in treatment decisions. Social Science Medicine. 1992;34(11):1217–1225. doi: 10.1016/0277-9536(92)90314-g. [DOI] [PubMed] [Google Scholar]
- Livingstone MB, Black AE. Markers of the validity of reported energy intake. Journal of Nutrition. 2003;133(Suppl 3):895S–920S. doi: 10.1093/jn/133.3.895S. [DOI] [PubMed] [Google Scholar]
- Lutes LD, Winett RA, Barger SD, Wojcik JR, Herbert WG, Nickols-Richardson SM, Anderson ES. Small changes in nutrition and physical activity promote weight loss and maintenance: 3-month evidence from the ASPIRE randomized trial. Annals of Behavioral Medicine. 2008;35(3):351–357. doi: 10.1007/s12160-008-9033-z. [DOI] [PubMed] [Google Scholar]
- Montgomery AA, Harding J, Fahey T. Shared decision making in hypertension: The impact of patient preferences on treatment choice. Family Practitioner. 2001;18(3):309–313. doi: 10.1093/fampra/18.3.309. [DOI] [PubMed] [Google Scholar]
- NAVPERS 15602A (1996). In D.o. t. Navy (Ed.).
- NHLBI. The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: National Heart, Lung, and Blood Institute. 2000. [Google Scholar]
- NQMP. A National Quality Management Program Special Report: Prevalence of Obesity: NQMP. 2003. [Google Scholar]
- OPNAV Instruction 6110.1H (2005). In D. o. t. Navy (Ed.).
- OPNAVINST 6110.1H CH-1 (2006). In D. o. t. Navy (Ed.).
- Patall EA, Cooper H, Robinson JC. The effects of choice on intrinsic motivation and related outcomes: A meta-analysis of research findings. Psychology Bulletin. 2008;134(2):270–300. doi: 10.1037/0033-2909.134.2.270. [DOI] [PubMed] [Google Scholar]
- Pinto BM, Clark MM, Cruess DG, Szymanski L, Pera V. Changes in self-efficacy and decisional balance for exercise among obese women in a weight management program. Obesity Research. 1999;7(3):288–292. doi: 10.1002/j.1550-8528.1999.tb00408.x. [DOI] [PubMed] [Google Scholar]
- Protheroe J, Fahey T, Montgomery AA, Peters TJ. The impact of patients’ preferences on the treatment of atrial fibrillation: Observational study of patient based decision analysis. Bmj. 2000;320(7246):1380–1384. doi: 10.1136/bmj.320.7246.1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qaseem A, Snow V, Denberg TD, Forciea MA, Owens DK. Using second-generation antidepressants to treat depressive disorders: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine. 2008;149(10):725–733. doi: 10.7326/0003-4819-149-10-200811180-00007. [DOI] [PubMed] [Google Scholar]
- Reginster JY, Rabenda V, Neuprez A. Adherence, patient preference and dosing frequency: Understanding the relationship. Bone. 2006;38(4 Suppl 1):S2–6. doi: 10.1016/j.bone.2006.01.150. [DOI] [PubMed] [Google Scholar]
- Rennie TW, Bothamley GH, Engova D, Bates IP. Patient choice promotes adherence in preventive treatment for latent tuberculosis. European Respiratory Journal. 2007;30(4):728–735. doi: 10.1183/09031936.00034007. [DOI] [PubMed] [Google Scholar]
- Rosenthal BS, Marx RD. Determinants of initial relapse among dieters. Obesity and Bariatric Medicine. 1983;10:94–97. [Google Scholar]
- Sandifer BA, Buchanan WL. Relationships between adherence and in behavioral weight reduction programs. Behavior Therapy. 1983;16:1–14. [Google Scholar]
- Schaefer EJ, Augustin JL, Schaefer MM, Rasmussen H, Ordovas JM, Dallal GE, Dwyer JT. Lack of efficacy of a food-frequency questionnaire in assessing dietary macronutrient intakes in subjects consuming diets of known composition. American Journal of Clinical Nutrition. 2000;71(3):746–751. doi: 10.1093/ajcn/71.3.746. [DOI] [PubMed] [Google Scholar]
- Schnoll R, Zimmerman BJ. Self-regulation training enhances dietary self-efficacy and dietary fiber consumption. Journal of the American Dietetic Association. 2001;101(9):1006–1011. doi: 10.1016/S0002-8223(01)00249-8. [DOI] [PubMed] [Google Scholar]
- Seibert DC. Secrets to creating effective and interesting educational experiences: Tips and suggestions for clinical educators. Journal of Genetic Counseling. 2008;17(2):152–160. doi: 10.1007/s10897-007-9141-0. [DOI] [PubMed] [Google Scholar]
- Shay LE. Self-monitoring and weight management. Online Journal of Nursing Informatics. 2008;12(1) [Google Scholar]
- Shiffman S, Hufford MR, Paty J. Subject experience diaries in clinical research, Part 1: The patient experience movement. Applied Clinical Trials. 2001:1–6. [Google Scholar]
- Sperduto WA, Thompson HS, O’Brien RM. The effect of target behavior monitoring on weight loss and completion rate in a behavior modification program for weight reduction. Addictive Behaviors. 1986;11(3):337–340. doi: 10.1016/0306-4603(86)90060-2. [DOI] [PubMed] [Google Scholar]
- Stalonas PM, Kirschenbaum DS. Behavioral treatment for obesity: Eating habits revisited. Behavior Therapy. 1985;16:1–14. [Google Scholar]
- Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient compliance with paper and electronic diaries. Controlled Clinical Trials. 2003;24(2):182–199. doi: 10.1016/s0197-2456(02)00320-3. [DOI] [PubMed] [Google Scholar]
- Vincent N, Lionberg C. Treatment preference and patient satisfaction in chronic insomnia. Sleep. 2001;24(4):411–417. doi: 10.1093/sleep/24.4.411. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK, Hesson LA, Osei SY, Kaplan R, Stunkard AJ. Randomized trial of lifestyle modification and pharmacotherapy for obesity. New England Journal of Medicine. 2005;353(20):2111–2120. doi: 10.1056/NEJMoa050156. [DOI] [PubMed] [Google Scholar]
- Warner C, Warner C, Matuszak T, Rachal J, Flynn J, Grieger TA. Disordered eating in entry-level military personnel. Military Medicine. 2007;172(2):147–151. doi: 10.7205/milmed.172.2.147. [DOI] [PubMed] [Google Scholar]
- Wolff GE, Clark MM. Changes in eating self-efficacy and body image following cognitive-behavioral group therapy for binge eating disorder: A clinical study. Eating Behaviors. 2001;2(2):97–104. doi: 10.1016/s1471-0153(01)00021-6. [DOI] [PubMed] [Google Scholar]
- Yancy William S, Jr, Boan J. Adherence to diet recommendations. In: Bosworth HB, Oddone EZ, Weinberger M, editors. Patient Treatment Adherence: Concepts, Interventions, and Measurement. New Jersey: Lawrence Erlbaum Associates; 2006. pp. 95–116. [Google Scholar]


