Abstract
Silver nanoparticles (AgNPs) have been widely used in industrial, household, and healthcare-related products due to their excellent antimicrobial activity. With increased exposure of AgNPs to human beings, the risk of safety has attracted much attention from the public and scientists. In review of recent studies, we discuss the potential impact of AgNPs on individuals at the cell level. In detail, we highlight the main effects mediated by AgNPs on the cell, such as cell uptake and intracellular distribution, cytotoxicity, genotoxicity, and immunological responses, as well as some of the major factors that influence these effects in vivo and in vivo, such as dose, time, size, shape, surface chemistry, and cell type. At the end, we summarize the main influences on the cell and indicate the challenges in this field, which may be helpful for assessing the risk of AgNPs in future.
Keywords: Silver nanoparticles, cell effects, cytotoxicity, genotoxicity, immunological response, risk assessment
INTRODUCTION
With strong antimicrobial activity, silver nanoparticles (AgNPs) are widely used as one of major ingredients in industrial, daily life, and healthcare-related products.1 For example, AgNP-based products have been used in the surface coatings of washing machines, water purifiers, toys, and packaging materials. They have been also incorporated into textiles and some cosmetics, including sunscreen. Furthermore, they have been coated or embedded inside medical products, such as wound dressings, urinary catheters, surgical instruments, and bone prostheses.2 Their antimicrobial ability is attributed to the strong oxidative activity of AgNP surfaces and the release of silver ions to biological environments.3 Both factors are thought to trigger a series of negative effects on the structures and functions of cells, which finally induce cytotoxicity, genotoxicity, immunological responses, and even cell death.1,2 Nowadays, the possible adverse effects of AgNPs to both workers at manufacturing plants and consumers exposed to these products have generated greater attention between the public and scientists. Therefore, evaluation of the potential risks of AgNPs, especially their impacts on biological systems, from different aspects may help to facilitate the design of safer and more effective anti-microbial products in the future. Here, we review recently published results concerning the effects of AgNPs on the cell, possible mechanisms and main determinant factors thereof, and challenges in this field.
PREPARATION
In general, three strategies, including chemical, physical and biological reduction, have been used to prepare AgNPs.1 As a conventional method, chemical reduction involves a process in which a silver salt is dissolved in a liquid phase to react with a reducing agent, and then a suitable dispersant is used to facilitate a good dispersion compound. Common reduction agents include citrate, glucose, ethylene glycol, and sodium borohydride. For the physical reduction method, on the other hands, silver ions are reduced to AgNPs through a variety of physical methods including optical quantum reduction and microwave reduction. The biological reduction method, relying on the ability of bio-organisms to reduce ions to AgNPs, is considered being a green synthesis strategy because the major substrates and the reaction are mild. Importantly, some key physiochemical properties of AgNPs, like shapes and surface coating, can be precisely tunable. For example, the shape of AgNPs can be manipulated into spheres, cubes, triangles, rods and so on.4,5 Also, surface coating polymers, such as poly-(N-vinylpyrrolidone) (PVP) and small molecules like citrate and thiols, can provide functional groups on the nanoparticles to improve the dispersion in the aqueous phase.6,7
BIOLOGICAL EFFECTS OF SILVER NANOPARTICLES
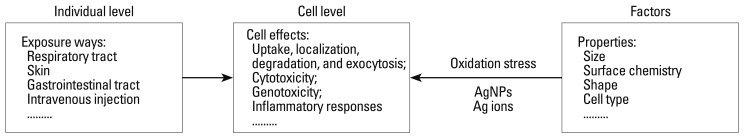
Risk evaluations of AgNPs are designed to test their biological effects, possible mechanisms, and efficient approaches to decrease their negative effects. Nanotoxicity majorly focuses on testing biological effects, and is critical to understanding mechanisms and to predicting potentially adverse effects of AgNPs for sustainable development thereof in the future. Here, we review recent research on the biological effects of AgNPs, mainly at the cell level (Fig. 1), and discuss the relevant mechanisms and challenges during AgNP development.
Fig. 1.
Potential effects of AgNPs on cells and the major factors that mediate these effects.
Effects on humans
AgNPs have been widely used as antimicrobial materials in foods, medical products, and coatings for industrial products. Factors like size, surface chemistry, methods of exposure, and exposure times are critical to determining their pathways of tissue distribution.2 For individuals, there are several possible ways to be exposed to AgNPs including dermal contact, oral administration (gastrointestinal tract), inhalation (respiratory tract), blood circulation (intravenous injection), etc.2,8 Through tail veins the injected AgNPs have a short circulation time and a broad tissue distribution in vivo.8,9 The liver is the major target organ, followed by the spleen, lungs, and kidneys, although the larger size AgNPs may accumulate more in the spleen than that in other organs. Interestingly, Ag concentrations in the blood remain at a high level up to 6 days post-injection, after that the concentration will be fallen, which suggests that AgNPs may be degraded and removed in a time-dependent manner.9 Furthermore, one study concerning the inhalation toxicity of AgNPs revealed that distribution to the lungs and liver induces inflammatory responses such as inflammatory cell infiltration and chronic alveolar inflammation.10 After inhalation exposure, AgNPs are likely deposited in olfactory mucosa and subsequently translocated to olfactory nerves,11 which may induce the impairment and dysfunction of brain cells and immunotoxicity.12 Despite similar exposure in the lungs, however, another study showed that AgNPs caused negligible impacts on the nasal cavity and lungs.13 Additionally, in regards to oral exposure to AgNPs, migration to the acidic environment of the gastrointestinal tract helps the dissolution of AgNPs into silver ions. Moreover, AgNPs affect the expression of biochemical markers of hepatotoxicity, such as serum alkaline phosphatase and cholesterol,14 as well as apoptosis and inflammation.15,16 Animals models with zebrafish, fruit flies, Caenorhabditis elegans, and Japanese medaka have been used to study the toxicity of AgNPs in vivo. In these studies, AgNPs reportedly induced development and reproduction abnormalities, and the high mortality was considered to be dependent on the exposed dose.17-19 Furthermore, reports on workers exposed to low doses of silver dust or soluble silver at threshold limit values showed no significant changes in health status.20 Notwithstanding, long-term exposure studies of higher doses are needed to reveal the potential risk of AgNPs on health. Additionally, the establishment of a safe range of exposure doses and evaluation standards for assessing AgNP safety is needed to protect workers and consumers.
Biochemical markers can be used to discover and predict the possible mechanisms and extent of AgNP nanotoxicity. Biochemical changes include the up-regulation of oxidative stress related genes, metallothionein mRNA expression, and elevated expression of heat shock protein 70 (hsp70).8 Currently, high throughput techniques utilizing genomics-based methods have been used to study the toxicity of AgNPs in vivo by screening for biomarkers;13 temporal-spatial imaging of AgNPs, and sensitive detection of key biochemical markers have proven to be essential paths in studying the risk of AgNPs.
Effects on cells
Compared to animal models, the research of NPs toxicity at the cell level is much simple and convenient. Below, we summarize the works on the potential toxicity of AgNPs at the cell level.
The transport of AgNPs inside the cell begins with cell membrane receptor recognition, internalization, and translocation, and ends with degradation, accumulation, or clearance by cells. For most cells, uptake of AgNPs via endocytosis is a time, dose, energy-dependent process, and the major target organelles are endosomes and lysosomes.21,22 For primary astrocytes, lung fibroblasts, and glioblastoma cells, macropinocytosis and clathrin-involved pathways are involved in the internalization of AgNPs.21,22 Macrophages internalize the agglomerates of AgNPs via actin-dependent endocytosis mediated by scavenger receptors.23 For monocytes, non-agglomerated AgNPs can be internalized via clathrin-dependent, actin-independent pathways.24 Internalized AgNPs can be found in mitochondria and the nucleus, which depends on the size and surface modification of NPs.25 Once internalized, intracellular AgNPs induce a series of effects including oxidative stress, impairment of the cell membrane, cell cycle rest, inflammatory responses, DNA damage and genotoxicity, chromosome aberration, and apoptosis.25-28
The AgNP exposure could induce the changes of cell shape, reduce cell viability, increase lactate dehydrogenase (LDH) release and finally result in cell apoptosis and necrosis.7,28 Cytotoxicity is a direct outcome due to oxidation stress caused by AgNPs and release of Ag ions. Electron spin resonance has indicated that the active surface of AgNPs can directly induce the generation of original free radicals, and the dissolution of AgNPs into Ag ions triggers the production of hydroxyl radicals in acidic endo/lysosomes.3 With high concentrations of AgNPs, the morphology of epithelial cells can change to become less polyhedral and more fusiform, shrunken, and rounded. The reason for this is that AgNPs elevate oxidative stress by decreasing glutathione (GSH) and superoxide dismutase (SOD) and increasing lipid peroxidation, which finally leads to apoptosis by increasing caspase-3 activity and DNA fragmentation.29 Moreover, internalized AgNPs can disrupt the integrity of the cell membrane, cause lysosomal swelling, and even rupture lysosomal membranes.26 AgNPs and released Ag ions prefer to interacting with thiol groups in reduced GSH and proteins, such as thioredoxin, SOD, and thioredoxin peroxidase. There are many molecules that contain thiols in the cytoplasm, cell membrane, and inner membrane of mitochondrion, which serve as targets of silver ions or AgNPs.28 Upon interaction of AgNPs with membrane proteins, AgNPs and Ag ions may evoke lipid peroxide and increase the permeation of cell membrane systems. The damage of the cell membrane leads to leakage of cytoplasmic contents, such as LDH, and eventual necrosis, while rupture of lysosomal membranes releases cathepsins into the cytoplasm, activating lysosome-mediated apoptosis. Furthermore, damage to mitochondria impairs electron transfer, inhibits adenosine triphosphate (ATP) synthesis, triggers oxidative stress, and activates mitochondrion-dependent apoptosis.26,29
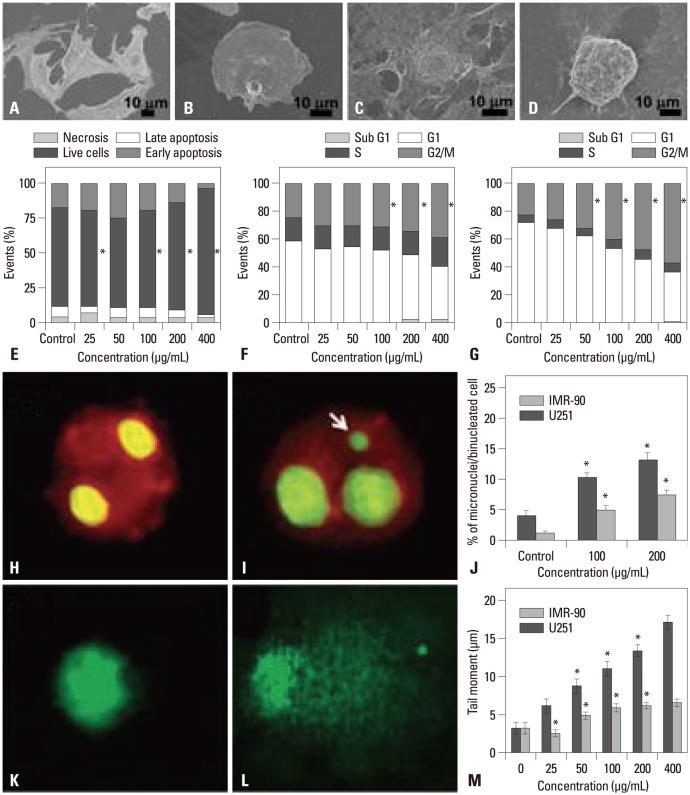
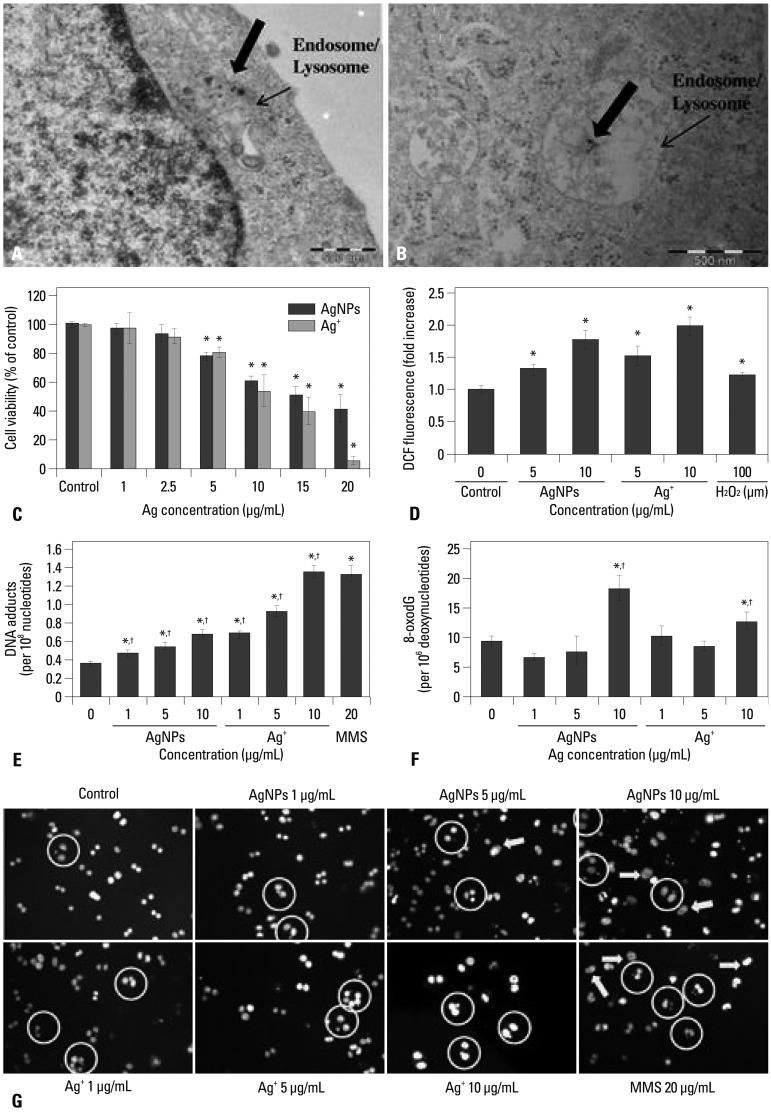
AgNPs are associated with genotoxicity as a result of damage to DNA and chromosomes from oxidation stress; AgNPs may also induce mutagenicity.30 Transmission electron microscopy images, together with elemental mapping of single cells, have revealed that AgNPs can translocate to the nucleus and cause a damage to DNA and chromosomes. Nuclear pore complexes in the nuclear envelope have a 9-10 nm in diameter, and they facilitate the transport of proteins in and out of the cell, including partly dissolved NPs. Upon diffusion into the cell, AgNPs can be deposited in the nucleus, and subsequent production of reactive oxygen species (ROS) directly triggers DNA damage and chromosomal abnormalities, according to comet and micronucleus assay (Fig. 2). As a result, the cell cycle is halted in the G2/M interphase and proliferation is inhibited. Finally, cells must choose whether to survive or to die at a later stage, by judging whether DNA repair pathways are unsuccessful or not.22,25 Another study showed that AgNPs at a low dose and chronic exposure also result in DNA damage and changes in the expression of carcinogenicity-correlated genes in the human hepatoma cell line HepG2. At low doses, although no significant cytotoxicity was recorded, the induced cell proliferation was observed. Nevertheless, a low dose of AgNPs, rather than Ag2CO3 (reflects the interaction of Ag ions with cells), can cause DNA damage and chromosomal aberrations (increase in micronuclei), which were reportedly attributed to "nano-size" effect and the release of Ag ions.31 Previously, the cytotoxicity and genotoxicity of bovine serum abumin (BSA)-coated AgNPs on Chinese hamster ovary cells, CHO-K1, were investigated, and revealed that both BSA-AgNPs alone and Ag ions can generate ROS that oxidize DNA to oxidative adducts, 8-oxodG, and induces the formation of micronuclei (Fig. 3).27
Fig. 2.
Cell effects induced by AgNPs depended on cell type. Lung fibroblast cells (IMR-90) and glioblastoma cells (U251) exposed to AgNPs at a low dose did not cause cytotoxicity, but could inhibit cell proliferation. AgNPs changed the morphology of both cells observed under environmental scanning electronic microscopes (A); however, they did not cause obvious cell death (IMR-90), as determined by Annexin V and PI assay (E): (A and B) Control IMR-90 cells and those exposed to AgNPs. (C and D) Control U251 cells and those exposed to AgNPs. Changes in cell cycle for U251 (F) and IMR-90 cells (G) exposed to AgNPs. Induced chromosomal aberrations in IMR-90 cells by 100 µg/mL of AgNPs determined by micronucleus analysis: control (H), AgNP-treated (I), the percentage of formed micronuclei in binucleated cells (J). Comet analysis to study DNA damage in U251 cells: control (K), AgNP-treated cells (L), and results of tail moment distances of DNA for both cells (M). *Represents p<0.05 compared with control. Adapted from Asharani, et al. BMC Cell Biol 2009;10:65.22 and AshaRani, et al. ACS Nano 2009;3:279-90.25
Fig. 3.
Cytotoxicity and genotoxicity analysis of BSA-coated AgNPs in the cell line CHO-K1. TEM images of CHO-K1 cells when treated with 10 µg/mL of AgNPs for 6 h (A) and 24 h (B). For cells treated with AgNPs and Ag+, changes in mitochondrial activity (C) by CCK-8 assay and intracellular ROS levels (D) that were labeled by DCFHDA fluorescence density and determined by flow cytometry. DNA adducts induced by AgNPs and Ag+ after 24 h exposure (E). Methylmethanesulphonate (MMS) was used as a positive control. DNA oxidative adduct, 8-oxodG, that can be induced by AgNPs and Ag+ after 24 h exposure (F). Fluorescence microscopic images of micronuclei induced by AgNPs and Ag+ after 24 h exposure (G). Statistical significant difference from control is expressed as *(p<0.05) and significant difference between AgNPs and Ag+ in the same amount of silver is expressed as †(p<0.05). Adapted from Jiang, et al. Toxicol Lett 2013;222:55-63.27
It has been reported that some nanomaterials can activate immunological responses.32 AgNPs can also trigger innate and adaptive inflammatory responses due to oxidation stress. Together with induced cytotoxicity, AgNPs can also rupture the lysosomal membranes of monocytes and promote the maturation and secretion of a key cytokine, IL-1β, related to immunological activation. Leakage of cathepsins from impaired lysosomes and efflux of K+ ions may contribute to the production of mitochondrial superoxide and hydrogen peroxide, as well as the formation of inflammasomes.26 AgNPs can also induce inflammation to microvessel endothelial cells of the blood brain barrier in a dose, time, and size-dependent manner. They can trigger cytotoxic responses and stimulate the expression of immune-related cytokines, such as interleukin IL-1β, IL-2, tumor necrosis factor TNF-α, and prostaglandin E2. The responses to AgNPs were demonstrated by the increasing permeability of biological barrier and the reducing integrity of endothelial cell monolayer.33
Key factors that mediate cellular effects of AgNPs
The cytotoxicity of AgNPs depends on time, dose, and temperature.21 Other factors such as size, surface coatings of AgNPs, and cell type are also strongly associated with cytotoxicity.
Size
AgNP size mediates cell responses, including uptake, cytotoxicity, ability to penetrate biological barriers, and immunological responses.33-36 As reported, both ROS generation and the degradation of AgNPs into ions depend on size. A recent study revealed that the size of PVP-coated AgNPs is negatively correlated with ROS level, apoptosis, and necrosis ratio, as well as the decrease of cell viability.35 The smaller AgNPs have stronger activity because of the large specific surface area regulating oxidation stress and the dissolution rate of AgNPs into ions depending on interfacial interaction.37,38 Furthermore, cell uptake of NPs largely depends on the size of NPs, which results in different concentrations of AgNPs inside the cell.39 The ability of AgNPs penetrating the biological barriers also depends on their size. Several human lung, stomach, breast, hepatocellular cells have been used to test the size effects on cellular activities, such as cell uptake, ROS levels, membrane integrity, cell cycle rest, and EC50, all of them were shown to be highly dependent on size.35,36 It was reported that AgNPs can induce strong damage and dysfunction of endothelial cells as well as increase of the permeability of the monolayer of microvascular endothelial cells in a size-dependent manner, producing strong inflammatory responses. The accumulation of smaller AgNPs in the cell causes cytotoxicity, changes in the morphology of endothelial cell monolayers, and promote cytokine release.33 AgNP size is one of an important factors for evoking an immunological state in monocytes. Smaller AgNPs (5 nm to 28 nm) can produce greater amounts of hydrogen peroxide and induce greater inflammasome formation because they can cause stronger leakage of cathepsins from lysosomes, induce more efflux of intracellular K+, and produce more superoxide in mitochondrial membranes.26
Surface chemistry
Surface chemistry can influence the interaction of AgNPs with cells. According to surface coatings, AgNPs can be conjugated by certain molecules to realize novel functions and to improve colloidal stability. Surface coating AgNPs can affect shape, aggregation, and dissolution ratio. The stability of the surface coatings influences the cytotoxicity of AgNPs. PVP-and citrate-coated AgNPs are, respectively, listed as the most and least stable NPs in OECD recommended media (chloride present).6 Citrate coatings can improve the stability of colloidal AgNPs and decrease their toxicity. Once citrate-coated AgNPs are dried in a powder, the surface citrate coating is destroyed, and they become pristine one but after re-dissolving they still cause obvious cytotoxicity. In contrast, PVP modification AgNPs maintains a good stability, and causes negligibly toxic effects on human skin HaCaT keratinocytes when the dried NP powder is re-dissolved into water.40 Previous works demonstrated that uncoated AgNPs significantly decreased cell viability in a time-and dose-dependent manner, while BSA-coated ones could reduce cytotoxicity.41 Reportedly, polysaccharide-coated AgNPs resulted in a stronger DNA damage than uncoated AgNPs did. Uncoated AgNPs prefer to agglomerating and may not translocate to the nucleus and mitochondria, whereas macromolecule coatings, such as polysaccharides and proteins, can increase the likelihood of entering into mitochondria and the nucleus, and these AgNPs can be distributed throughout the whole cell.41,42
Shape
Shape of AgNPs also plays important roles in the toxic and immunological effects. In previous works, human lung epithelial A549 cells were exposed to Ag nanowires (length of 1.5-25 µm; diameter of 100-160 nm), spherical AgNPs (30 nm), and Ag microparticles (<45 µm), producing distinct effects. It was found that Ag nanowires resulted in calcium influx, the strongest cytotoxicity (reduced cell viability and increased LDH release) and immunological responses (cyto-kine production and increased activation of NF-κB), whereas spherical Ag particles had negligible effects on cells. The possible reason was that the wires can directly contact with the cell surface rather than being internalized.43
Cell type
Considering the distribution of AgNPs in multiple tissues, recent studies have revealed that cell types can influence responses to AgNPs. When fibroblast cells (NIH3T3) and colon cancer epithelial cells (HCT116) were exposed to AgNPs, the two types of cells showed distinct responses. For the fibroblast cells, exposure to AgNPs resulted in high expression of ROS and c-Jun N-terminal kinases, which activate mitochondrial apoptotic pathways. However, the epithelial cells showed less of a response to AgNPs because the expression of anti-apoptotic protein bcl-2 can be activated to protect against apoptotic stimuli.44 Starch-coated AgNPs can cause different genotoxicities to fibroblast cells (IMR-90) and glioblastoma cells (U251). For both types of cells, AgNPs can diffuse into mitochondria and the nucleus, induce mitochondrial dysfunction, and increase the level of ROS, subsequently cause DNA damage, chromosomal aberrations, and cell cycle rest. However, fibroblast cells are more resistant to AgNPs, while the glioblastoma cells are more sensitive to AgNPs because fibroblast cells can recover from cell cycle arrest.25 Meanwhile, PVP-coated AgNPs do not induce obvious toxicity to primary cultured astrocytes, even they accumulate more AgNPs than lung cancer cells do.21 The reason is that the release of toxic Ag+ from internalized AgNPs was more slowly and most accumulated AgNPs in a non-toxic form in astrocytes. Similar reports revealed that NPs can produce distinct effects on normal cells from cancer cells because lysosomal membranes can endure different stimuli in two types of cells45 and the ability to counteract with and to recover from oxidative stress are quite distinct for two types of cells.46
The mechanism for the cellular effect of AgNPs
Oxidative stress leads to a series of cellular events, including reduced levels of GSH, elevated lipid peroxidation, inflammation, DNA damage, altered cell cycle and proliferation capacity, and apoptosis and necrosis in various cell culture models. The generation of ROS and release of silver ions are two dominant factors that mediate cell effects.
Generally speaking, it is difficult to distinguish the direct origins of AgNP induced-cell effects. AgNPs at a low dose (<1.0 µg/mL) are not enough to produce obvious cytotoxicity to hepatoma cells, HepG2, but cause damage to DNA and chromosomes by forcing cells to express a large number of DNA repair-related genes.31 With the aid of extensive gene expression analysis, AgNPs, Ag2CO3, and Ag ion inhibitor cysteine are used to reveal the nature of AgNP-induced cell effects. Results have demonstrated that both AgNPs alone as well as "ionic Ag ions" contribute to the DNA damage derived from oxidation stress. Ag ions mainly contribute to cytotoxic and stress associated effects. Nano-size alone has unique toxic effects on the cells, which suggests that both particles and dissolved ions can synergically influence cellular responses.
Ag ions play a role in catalyzing ROS production in the presence of oxygen species.31 Interestingly, AgNPs themselves can produce ROS and oxidative stress in vivo, as well as the process to release Ag ions.31 Electron spin resonance (ESR) spectroscopy has been used to study ROS generation in a simulated microenvironment, like cytoplasm or endo/lysosomes. According to a Fenton-like reaction, dispersed AgNPs can induce reactive oxygen species like hydroxyl radicals in the presence of hydrogen peroxide and an acidic environment. Hydrogen peroxide inside a cell at a low dose can accelerate the dissolution of AgNPs and produce much stronger oxidative stress.3
Some redox-related peptides and proteins, such as GSH, thioredoxin, and SOD, are known to mediate oxidative stress. Interactions of these antioxidant molecules with AgNPs or Ag ions can partly antagonize oxidative stimuli to reduce toxicity of the latter.5 However, excessive ROS may change their structure and function, losing their antioxidant ability.47 Ag ions prefer to bind to chlorides, inorganic sulfides, and thiol groups, but the interactions of AgNPs with proteins and the possible influences thereof on cells are largely unknown.
CONCLUSION AND PERSPECTIVE
AgNPs have emerged as a typical antimicrobial nanomaterial applied in industry, daily life, and healthcare. Due to the strong activity of AgNPs and release of Ag ions, the biological effects and safety thereof have attracted tremendous attentions from scientists. Both AgNPs and Ag ions can produce ROS and cause oxidative stress in cells at different levels: molecules, organelles, and the entire cell. AgNPs induce stronger oxidative damage to cell membrane and organelles, including lysosomes, mitochondria, and the nucleus, directly resulting in apoptosis or necrosis. Oxidative stress caused by AgNPs can trigger inflammatory responses, including the activation of innate immunity and increased permeability of endothelial cells. AgNPs at a non-cytotoxic dose may induce DNA damage, chromosomal abnormality, and possible mutagenicity. Several factors such as dose, exposure time, size, shape, surface chemistry, and cell types play important roles in mediating cellular responses.
Previous studies have revealed the biological effects of AgNPs. However, many challenges still exist in this field. It is important to understand the mechanisms of the biological effects of AgNPs and to predict the outcomes of AgNPs exposure in vivo. Nevertheless, building a proper cell model for studying the biological effects of AgNPs in vivo remains a challenge. Many parameters in artificial microenvironments thus should be fully considered and carefully controlled to reach a conclusion. In addition, major biomarkers should be screened under different conditions for evaluating the safety of AgNPs in future: dose, time, size, surface chemistry, and specific tissues. High throughput analysis, advanced nuclear analytical techniques, and omics-based techniques are necessary to resolve problems in this field.48,49 More importantly, for sustainable development of nanotechnology and safety, some measurements should be taken immediately to resolve the possible adverse effects of AgNPs to human beings.
ACKNOWLEDGEMENTS
This work was financially supported by the National Basic Research Program of China (2011CB933401, 2012CB 934000, and 2011BAD24B01), the National Natural Science Foundation of China (11205166 and 31070854), Beijing Natural Science Foundation (No.1112012), BIGC Key Project (No.23190113051), KM 201110015008 and PHR2011 0516, PHR201107145.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Chernousova S, Epple M. Silver as antibacterial agent: ion, nanoparticle, and metal. Angew Chem Int Ed Engl. 2013;52:1636–1653. doi: 10.1002/anie.201205923. [DOI] [PubMed] [Google Scholar]
- 2.Chen X, Schluesener HJ. Nanosilver: a nanoproduct in medical application. Toxicol Lett. 2008;176:1–12. doi: 10.1016/j.toxlet.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 3.He W, Zhou YT, Wamer WG, Boudreau MD, Yin JJ. Mechanisms of the pH dependent generation of hydroxyl radicals and oxygen induced by Ag nanoparticles. Biomaterials. 2012;33:7547–7555. doi: 10.1016/j.biomaterials.2012.06.076. [DOI] [PubMed] [Google Scholar]
- 4.Dickerson MB, Sandhage KH, Naik RR. Protein- and peptide-directed syntheses of inorganic materials. Chem Rev. 2008;108:4935–4978. doi: 10.1021/cr8002328. [DOI] [PubMed] [Google Scholar]
- 5.Eckhardt S, Brunetto PS, Gagnon J, Priebe M, Giese B, Fromm KM. Nanobio silver: its interactions with peptides and bacteria, and its uses in medicine. Chem Rev. 2013;113:4708–4754. doi: 10.1021/cr300288v. [DOI] [PubMed] [Google Scholar]
- 6.Tejamaya M, Römer I, Merrifield RC, Lead JR. Stability of citrate, PVP, and PEG coated silver nanoparticles in ecotoxicology media. Environ Sci Technol. 2012;46:7011–7017. doi: 10.1021/es2038596. [DOI] [PubMed] [Google Scholar]
- 7.Foldbjerg R, Olesen P, Hougaard M, Dang DA, Hoffmann HJ, Autrup H. PVP-coated silver nanoparticles and silver ions induce reactive oxygen species, apoptosis and necrosis in THP-1 monocytes. Toxicol Lett. 2009;190:156–162. doi: 10.1016/j.toxlet.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 8.Ahamed M, Alsalhi MS, Siddiqui MK. Silver nanoparticle applications and human health. Clin Chim Acta. 2010;411:1841–1848. doi: 10.1016/j.cca.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 9.Lankveld DP, Oomen AG, Krystek P, Neigh A, Troost-de Jong A, Noorlander CW, et al. The kinetics of the tissue distribution of silver nanoparticles of different sizes. Biomaterials. 2010;31:8350–8361. doi: 10.1016/j.biomaterials.2010.07.045. [DOI] [PubMed] [Google Scholar]
- 10.Hyun JS, Lee BS, Ryu HY, Sung JH, Chung KH, Yu IJ. Effects of repeated silver nanoparticles exposure on the histological structure and mucins of nasal respiratory mucosa in rats. Toxicol Lett. 2008;182:24–28. doi: 10.1016/j.toxlet.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Oberdörster G, Sharp Z, Atudorei V, Elder A, Gelein R, Kreyling W, et al. Translocation of inhaled ultrafine particles to the brain. Inhal Toxicol. 2004;16:437–445. doi: 10.1080/08958370490439597. [DOI] [PubMed] [Google Scholar]
- 12.Rahman MF, Wang J, Patterson TA, Saini UT, Robinson BL, Newport GD, et al. Expression of genes related to oxidative stress in the mouse brain after exposure to silver-25 nanoparticles. Toxicol Lett. 2009;187:15–21. doi: 10.1016/j.toxlet.2009.01.020. [DOI] [PubMed] [Google Scholar]
- 13.Lee HY, Choi YJ, Jung EJ, Yin HQ, Kwon JT, Kim JE, et al. Genomics-based screening of differentially expressed genes in the brains of mice exposed to silver nanoparticles via inhalation. J Nanopart Res. 2009;12:1567–1578. [Google Scholar]
- 14.Kim YS, Kim JS, Cho HS, Rha DS, Kim JM, Park JD, et al. Twenty-eight-day oral toxicity, genotoxicity, and gender-related tissue distribution of silver nanoparticles in Sprague-Dawley rats. Inhal Toxicol. 2008;20:575–583. doi: 10.1080/08958370701874663. [DOI] [PubMed] [Google Scholar]
- 15.Cha K, Hong HW, Choi YG, Lee MJ, Park JH, Chae HK, et al. Comparison of acute responses of mice livers to short-term exposure to nano-sized or micro-sized silver particles. Biotechnol Lett. 2008;30:1893–1899. doi: 10.1007/s10529-008-9786-2. [DOI] [PubMed] [Google Scholar]
- 16.Song KS, Sung JH, Ji JH, Lee JH, Lee JS, Ryu HR, et al. Recovery from silver-nanoparticle-exposure-induced lung inflammation and lung function changes in Sprague Dawley rats. Nanotoxicology. 2013;7:169–180. doi: 10.3109/17435390.2011.648223. [DOI] [PubMed] [Google Scholar]
- 17.Scown TM, Santos EM, Johnston BD, Gaiser B, Baalousha M, Mitov S, et al. Effects of aqueous exposure to silver nanoparticles of different sizes in rainbow trout. Toxicol Sci. 2010;115:521–534. doi: 10.1093/toxsci/kfq076. [DOI] [PubMed] [Google Scholar]
- 18.Lee KJ, Nallathamby PD, Browning LM, Osgood CJ, Xu XH. In vivo imaging of transport and biocompatibility of single silver nanoparticles in early development of zebrafish embryos. ACS Nano. 2007;1:133–143. doi: 10.1021/nn700048y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu Y, Zhou Q, Li H, Liu W, Wang T, Jiang G. Effects of silver nanoparticles on the development and histopathology biomarkers of Japanese medaka (Oryzias latipes) using the partial-life test. Aquat Toxicol. 2010;100:160–167. doi: 10.1016/j.aquatox.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 20.Lee JH, Mun J, Park JD, Yu IJ. A health surveillance case study on workers who manufacture silver nanomaterials. Nanotoxicology. 2012;6:667–669. doi: 10.3109/17435390.2011.600840. [DOI] [PubMed] [Google Scholar]
- 21.Luther EM, Koehler Y, Diendorf J, Epple M, Dringen R. Accumulation of silver nanoparticles by cultured primary brain astrocytes. Nanotechnology. 2011;22:375101. doi: 10.1088/0957-4484/22/37/375101. [DOI] [PubMed] [Google Scholar]
- 22.Asharani PV, Hande MP, Valiyaveettil S. Anti-proliferative activity of silver nanoparticles. BMC Cell Biol. 2009;10:65. doi: 10.1186/1471-2121-10-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh RP, Ramarao P. Cellular uptake, intracellular trafficking and cytotoxicity of silver nanoparticles. Toxicol Lett. 2012;213:249–259. doi: 10.1016/j.toxlet.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 24.Wang H, Wu L, Reinhard BM. Scavenger receptor mediated endocytosis of silver nanoparticles into J774A.1 macrophages is heterogeneous. ACS Nano. 2012;6:7122–7132. doi: 10.1021/nn302186n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.AshaRani PV, Low Kah Mun G, Hande MP, Valiyaveettil S. Cytotoxicity and genotoxicity of silver nanoparticles in human cells. ACS Nano. 2009;3:279–290. doi: 10.1021/nn800596w. [DOI] [PubMed] [Google Scholar]
- 26.Yang EJ, Kim S, Kim JS, Choi IH. Inflammasome formation and IL-1β release by human blood monocytes in response to silver nanoparticles. Biomaterials. 2012;33:6858–6867. doi: 10.1016/j.biomaterials.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 27.Jiang X, Foldbjerg R, Miclaus T, Wang L, Singh R, Hayashi Y, et al. Multi-platform genotoxicity analysis of silver nanoparticles in the model cell line CHO-K1. Toxicol Lett. 2013;222:55–63. doi: 10.1016/j.toxlet.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 28.Almofti MR, Ichikawa T, Yamashita K, Terada H, Shinohara Y. Silver ion induces a cyclosporine a-insensitive permeability transition in rat liver mitochondria and release of apoptogenic cytochrome C. J Biochem. 2003;134:43–49. doi: 10.1093/jb/mvg111. [DOI] [PubMed] [Google Scholar]
- 29.Arora S, Jain J, Rajwade JM, Paknikar KM. Cellular responses induced by silver nanoparticles: In vitro studies. Toxicol Lett. 2008;179:93–100. doi: 10.1016/j.toxlet.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 30.Kim YJ, Yang SI, Ryu JC. Cytotoxicity and genotoxicity of nano-silver in mammalian cell lines. Mol Cell Toxicol. 2010;6:119–125. [Google Scholar]
- 31.Kawata K, Osawa M, Okabe S. In vitro toxicity of silver nanoparticles at noncytotoxic doses to HepG2 human hepatoma cells. Environ Sci Technol. 2009;43:6046–6051. doi: 10.1021/es900754q. [DOI] [PubMed] [Google Scholar]
- 32.Jang J, Lim DH, Choi IH. The impact of nanomaterials in immune system. Immune Netw. 2010;10:85–91. doi: 10.4110/in.2010.10.3.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trickler WJ, Lantz SM, Murdock RC, Schrand AM, Robinson BL, Newport GD, et al. Silver nanoparticle induced blood-brain barrier inflammation and increased permeability in primary rat brain microvessel endothelial cells. Toxicol Sci. 2010;118:160–170. doi: 10.1093/toxsci/kfq244. [DOI] [PubMed] [Google Scholar]
- 34.Park J, Lim DH, Lim HJ, Kwon T, Choi JS, Jeong S, et al. Size dependent macrophage responses and toxicological effects of Ag nanoparticles. Chem Commun (Camb) 2011;47:4382–4384. doi: 10.1039/c1cc10357a. [DOI] [PubMed] [Google Scholar]
- 35.Li L, Sun J, Li X, Zhang Y, Wang Z, Wang C, et al. Controllable synthesis of monodispersed silver nanoparticles as standards for quantitative assessment of their cytotoxicity. Biomaterials. 2012;33:1714–1721. doi: 10.1016/j.biomaterials.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 36.Liu W, Wu Y, Wang C, Li HC, Wang T, Liao CY, et al. Impact of silver nanoparticles on human cells: effect of particle size. Nanotoxicology. 2010;4:319–330. doi: 10.3109/17435390.2010.483745. [DOI] [PubMed] [Google Scholar]
- 37.Kittler S, Greulich C, Diendorf J, Köller M, Epple M. Toxicity of silver nanoparticles increases during storage because of slow dissolution under release of silver ions. Chem Mater. 2010;22:4548–4554. [Google Scholar]
- 38.He D, Bligh MW, Waite TD. Effects of aggregate structure on the dissolution kinetics of citrate-stabilized silver nanoparticles. Environ Sci Technol. 2013;47:9148–9156. doi: 10.1021/es400391a. [DOI] [PubMed] [Google Scholar]
- 39.Jiang W, Kim BY, Rutka JT, Chan WC. Nanoparticle-mediated cellular response is size-dependent. Nat Nanotechnol. 2008;3:145–150. doi: 10.1038/nnano.2008.30. [DOI] [PubMed] [Google Scholar]
- 40.Lu W, Senapati D, Wang S, Tovmachenko O, Singh AK, Yu H, et al. Effect of Surface Coating on the Toxicity of Silver Nanomaterials on Human Skin Keratinocytes. Chem Phys Lett. 2010;487:92–96. doi: 10.1016/j.cplett.2010.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kittler S, Greulich C, Gebauer JS, Diendorf J, Treuel L, Ruiz L. The influence of proteins on the dispersability and cell-biological activity of silver nanoparticles. J Mater Chem. 2010;20:512–518. [Google Scholar]
- 42.Ahamed M, Karns M, Goodson M, Rowe J, Hussain SM, Schlager JJ, et al. DNA damage response to different surface chemistry of silver nanoparticles in mammalian cells. Toxicol Appl Pharmacol. 2008;233:404–410. doi: 10.1016/j.taap.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 43.Stoehr LC, Gonzalez E, Stampfl A, Casals E, Duschl A, Puntes V, et al. Shape matters: effects of silver nanospheres and wires on human alveolar epithelial cells. Part Fibre Toxicol. 2011;8:36. doi: 10.1186/1743-8977-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hsin YH, Chen CF, Huang S, Shih TS, Lai PS, Chueh PJ. The apoptotic effect of nanosilver is mediated by a ROS- and JNK-dependent mechanism involving the mitochondrial pathway in NIH3T3 cells. Toxicol Lett. 2008;179:130–139. doi: 10.1016/j.toxlet.2008.04.015. [DOI] [PubMed] [Google Scholar]
- 45.Wang L, Liu Y, Li W, Jiang X, Ji Y, Wu X, et al. Selective targeting of gold nanorods at the mitochondria of cancer cells: implications for cancer therapy. Nano Lett. 2011;11:772–780. doi: 10.1021/nl103992v. [DOI] [PubMed] [Google Scholar]
- 46.Zhang L, Wang L, Hu Y, Liu Z, Tian Y, Wu X, et al. Selective metabolic effects of gold nanorods on normal and cancer cells and their application in anticancer drug screening. Biomaterials. 2013;34:7117–7126. doi: 10.1016/j.biomaterials.2013.05.043. [DOI] [PubMed] [Google Scholar]
- 47.Choi J, Reipa V, Hitchins VM, Goering PL, Malinauskas RA. Physicochemical characterization and in vitro hemolysis evaluation of silver nanoparticles. Toxicol Sci. 2011;123:133–143. doi: 10.1093/toxsci/kfr149. [DOI] [PubMed] [Google Scholar]
- 48.Qu Y, Li W, Zhou Y, Liu X, Zhang L, Wang L, et al. Full assessment of fate and physiological behavior of quantum dots utilizing Caenorhabditis elegans as a model organism. Nano Lett. 2011;11:3174–3183. doi: 10.1021/nl201391e. [DOI] [PubMed] [Google Scholar]
- 49.Li YF, Chen C. Fate and toxicity of metallic and metal-containing nanoparticles for biomedical applications. Small. 2011;7:2965–2980. doi: 10.1002/smll.201101059. [DOI] [PubMed] [Google Scholar]