Abstract
Purpose
Emergence agitation (EA) is frequently observed in children undergoing general anaesthesia. This study tested whether the addition of an intra-operative low-dose infusion of dexmedetomidine to fentanyl treatment reduced the incidence of emergence delirium following desflurane anesthesia in children undergoing strabismus surgery.
Materials and Methods
A total of 96 children (1-5 years old) undergoing strabismus surgery were enrolled. Anaesthesia was induced with propofol and maintained with desflurane. After induction, fentanyl (1 µg/kg) was administered to all children. During surgery, patients were infused with 0.2 µg/(kg·h)-1 dexmedetomidine (Group FD, n=47) or normal saline (Group F, n=47). Postoperative objective pain score (OPS), Paediatric Agitation and Emergence Delirium (PAED) score, and EA score were documented every 10 minutes in the post-anaesthesia care unit.
Results
There were no significant differences between the two groups in demographic characteristics and haemodynamic changes. The mean values of maximum EA, maximum PAED, and maximum OPS score were significantly lower in Group FD than in Group F at 0, 10, and 20 minutes after arrival at the post-anaesthesia care unit (p<0.001). The frequency of fentanyl rescue was lower in Group FD than in Group F (p<0.001). The incidence of severe EA was significantly lower in Group FD than in Group F (12.8% vs. 74.5%, p<0.001).
Conclusion
Intra-operative low-dose infusion of dexmedetomidine in addition to fentanyl reduces EA following desflurane anaesthesia in children undergoing strabismus surgeries.
Keywords: Dexmedetomidine, emergence agitation, objective pain score, pediatrics
INTRODUCTION
Emergence delirium (ED) and emergence agitation (EA) are common phenomenon in paediatric patients undergoing general anaesthesia by inhalation agents. The incidence of ED or EA was reported to range from 18% to 80%.1,2 Agitated behaviour associated with ED can delay discharge from the post-anaesthesia care unit (PACU), decrease parent and caregiver satisfaction, and increase the overall cost to the institution.3 Risk factors for development of ED include preschool age, previous surgery, adaptability, ophthalmology or otorhinolaryngology procedure, and inhalation agents associated with fast emergence.1,4
Strabismus surgery is one of the most common ophthalmologic operations in children under 5 years old and can be associated with moderate postoperative pain caused by the conjunctiva5 and a high incidence of EA (40-86%).6-9 As this procedure commonly elicits the oculo-cardiac reflex (OCR) by traction on extraocular muscles and their adnexa or by application of sudden pressure to the eye or orbit, arrhythmias such as bradycardia are frequently encountered during the procedure. Therefore, anaesthetic strategies for strabismus surgery in paediatric patients include prevention of haemodynamic instability as well as reduction of postoperative pain and EA.
Desflurane is known to allow faster recovery than any other inhalation agent.10-12 However, it can be associated with a higher incidence of EA,10,11,13 which may negate the advantage of rapid emergence.11,14 Recently, dexmedetomidine has been reported to prevent EA in paediatric patients.14-16 However, there are few data related to the effect of dexmedetomidine on EA following general anaesthesia with desflurane. Therefore, we designed this prospective randomised double-blind controlled study to investigate whether intraoperative continuous infusion of low-dose dexmedetomidine (0.2 µg/kg/h) could reduce the incidence of EA without deterioration of haemodynamics and delay emergence in paediatric patients undergoing strabismus surgeries who were anaesthetised with desflurane.
MATERIALS AND METHODS
After obtaining approval from the Internal Review Board of Severance Hospital (4-2011-0466) and registering this study at www.ClinicalTrials.gov (ref. number: NCT01512355), written informed consent was obtained from the parents of the children. Ninety-six children aged 1-5 years with an American society of Anesthegiologists physical status classification system (ASA) between I-II who were undergoing strabismus surgery were enrolled from September 2011 to March 2012. Exclusion criteria included lack of consent, mental retardation, developmental delay, history of allergies, neurological or psychiatric illness that may be associated with improper communication, any kind of cardiac conduction disorder, and any previous cardiovascular disease. Patients were randomized into two groups, the fentanyl group (Group F) and the fentanyl plus dexmedetomidine group (Group FD), by computer-generated random numbers in a double blinded fashion. The random number sequence was generated by an internet site program (http://www.random.org). During the induction period, cooperation of the children was rated on a four-point cooperation on induction scale, where 1=sleeping/calm, 2=awake/calm, 3=awake/anxious, and 4=very anxious/combative.17
Anaesthesia was induced with propofol (3 mg/kg) and rocuronium (0.3 mg/kg). Children were intubated and mechanically ventilated. Anaesthesia was maintained using desflurane with 50% air/O2. End tidal carbon dioxide was maintained between 30 and 35 mm Hg. After the induction, fentanyl (1 µg/kg) was administered to children in both groups. Patients in Group FD received continuous infusion with 0.2 µg/(kg·h)-1 dexmedetomidine (Precedex®, Hospira Inc, Rocky Mount, NC, USA; diluted with normal saline to a concentration of 2 µg/mL). For patients in Group F, an equivalent volume of normal saline [0.1 mL/(kg·h)-1] was continuously infused during surgery. The same investigator prepared all syringes containing drugs. All the evaluations and records were taken by a blinded observer outside the study. The bispectral index score (BIS VISTA™, Aspect Medical System Inc., MA, USA) was monitored during the surgery. The inhalation agent was titrated to maintain the bispectral index score between 40 and 60, and the baseline haemodynamic changes were kept within a 20% range. The concentration and age-adjusted minimal alveolar concentration of exhaled anaesthetic was monitored using an infrared analyser (Drager Primus®; Draeger Medical AG & Co KGaA, Luebeck, Germany). Intraoperative heart rate (HR), blood pressure (BP), haemoglobin oxygen saturation, bispectral index score, and end tidal desflurane concentration were recorded every 5 minutes from the start of infusion. Ondansetron and dexamethasone were administered intravenously for the prevention of postoperative nausea and vomiting. At the conclusion of the procedure, local anaesthetic eye drops containing 0.5% proparacaine (Alcaine, S.A. ALCON-COUVREUR N.V., Purrs, Belgium) were applied to the surgical site by an ophthalmologist for postoperative pain control, and infusion of the study drug and administration of desflurane were discontinued. Oral suction was performed and reversal agents (glycopyrrolate 0.004 mg/kg and neostigmine 0.02 mg/kg) were administered after confirming neuromuscular function had returned using train-of-four peripheral nerve stimulation. The patient's trachea was extubated after recovery of the cough and gag reflex, grimace, and purposeful movement. The time from discontinuation of anaesthetics to recovery of spontaneous respiration, eye opening on verbal command, and extubation was recorded.
After confirmation of regular respiration and stable vital signs, each child was transported to the PACU and observed until fully awake. After arrival at the PACU all children were reunited with their parents. Oxygen saturation by pulse oxymetry, electrocardiography, and non-invasive BP measurements every 5 minutes were monitored between the operating room and the PACU. In addition, post-operative pain and EA were evaluated immediately after surgery by the objective pain score (OPS),18 Paediatric Agitation Emergence Delirium (PAED) scale,19 and EA 5-point scale as described by Cole, et al.,20 and subsequently recorded every 10 minutes in the PACU by a well-trained PACU nurse who was blinded to this study.
The PAED scale is composed of five items: eye contact with caregiver, purposeful action, awareness of surroundings, restlessness, and inconsolability. Our patients could not open their eyes due to postoperative pain; therefore, we modified the item 'eye contact with caregiver' to 'responsiveness to their parents'. Each item was scored by five grades (0-4) according to its degree, and the scores of each item were summed to obtain the total PAED scale score. The EA scale consists of five grades (1=sleeping, 2=awake and calm, 3=irritable and crying, 4=inconsolable and crying, and 5=severe restlessness and thrashing). According to the PACU protocol, patients with severe EA (EA score ≥4) or severe pain (OPS >8) were treated with intravenous fentanyl (0.5 µg/kg). The frequency of additional fentanyl use was compared between the two groups. Children with a score of 8 according to the Post-Anaesthetic Discharge Scoring System (PODSS)21 were discharged from PACU.
At postoperative 24 hours, a blinded investigator interviewed the patients' parents via telephone and evaluated their daily activity over the last 24 hours and the previous night's sleep quality using a 3-point scale as follows: resumption of normal activity, 0=normal activity, 1=depressed but performed normal daily activities, and 2=irritable and could not perform normal activities; sleep quality, 0=slept well, 1=woke up crying in the night, and 2=intermittent sleep.
Severe EA was defined as an EA score of 4 and above. A power analysis (80% power at a 0.05 level of significance) indicated that 45 subjects were required per group to show that dexmedetomidine infusion could reduce the incidence of EA by 50%.22 The number of patients recruited was increased by 10% to account for possible dropouts.
Statistical analysis was performed using PASW Statistics 18 (SPSS Inc., Chicago, IL, USA) or SAS software 9.2 (SAS Inc., Cary, NC, USA). All data were reported as mean±SD or percentage. Parametric data were analysed using an unpaired Student's t-test. Ordinal data were analysed using the Mann-Whitney ranked sum test. Nominal data were analysed using either the chi-square or Fisher's exact test. A linear mixed model was used for sequential variables (OPS scale, PAED scale, EA scale, and PODSS scale). The optimal cut-off point of maximum OPS score and maximum PAED score in relation to an EA score of 4 and above was chosen using the receiver operating characteristic (ROC) curve and Youden's index (sensitivity+specificity-1). The best discriminative accuracy corresponds to the area under the curve. After applying the new cut-off value, we compared the incidence of severe emergence agitation between the two groups. p<0.05 was considered statistically significant.
RESULTS
Among the 96 patients enrolled in this study two patients were excluded, one due to operation delay and the other due to agenesis of kidney. The remaining patients were divided randomly between Group F and Group FD (n=47 per group).
There were no significant differences between the two groups with respect to patient's demographic data, cooperation on induction scale, and the duration of surgery and anaesthesia. Two patients in Group FD had history of asthma and were classified as ASA class II (Table 1). Intraoperative bispectral index score and age-adjusted minimal alveolar concentration were comparable between the two groups.
Table 1.
Patient Demographics and Duration of Surgery and Anaesthesia

ASA, American Society of Anesthesiologists physical status classification system; CIS, Cooperation on Induction Scale1 where 1=excellent (unafraid, cooperative, and accepts mask readily), 2=good (slight fear of mask but easily calmed), 3=moderate fear, not calmed with reassurance), 4=poor (terrified, crying, and agitated).
Values are given as mean±SD or number of patients.
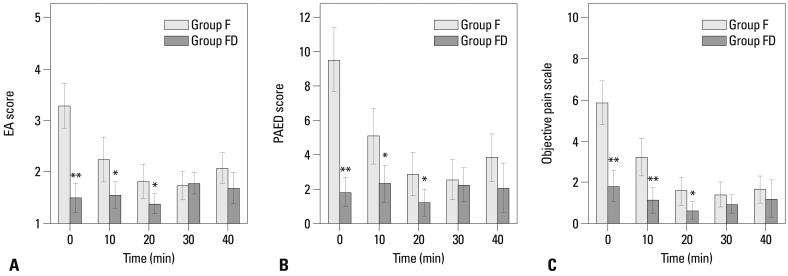
The means of maximum EA, maximum PAED, and maximum OPS score were significantly lower in Group FD than in Group F at 0, 10, and 20 minutes after arrival at PACU (Fig. 1). The maximum OPS and the frequency of fentanyl rescue were lower in Group FD than in Group F. The mean maximum OPS was 3.8 and 6.4 in group FD and group F, respectively (p<0.001). Five (10.6%) children in group FD required fentanyl rescue, compared with 24 (51.1%) children in group F (p<0.001).
Fig. 1.
Postoperative emergence agitation and objective pain score in post-anesthesia care unit. (A) EA score, emergence agitation 5 point scale, (B) PAED score, Pediatric Anesthesia Emergence Delirium score and (C) objective pain scale. *p<0.05 compared with Group F. **p<0.01 compared with Group F. EA, emergence agitation.
The mean maximum EA and maximum PAED scores were lower in group FD (p=0.001) (Table 2). The percentage of patients with EA scores of 4 and above was significantly lower in Group FD than in Group F (14.9% vs. 70.2%, p<0.001). The mean maximum PAED score was also significantly lower in Group FD than in Group F (9.0±4.5 vs. 11.5±4.1, p=0.001).
Table 2.
Postoperative Pain and Severe Emergence Agitation
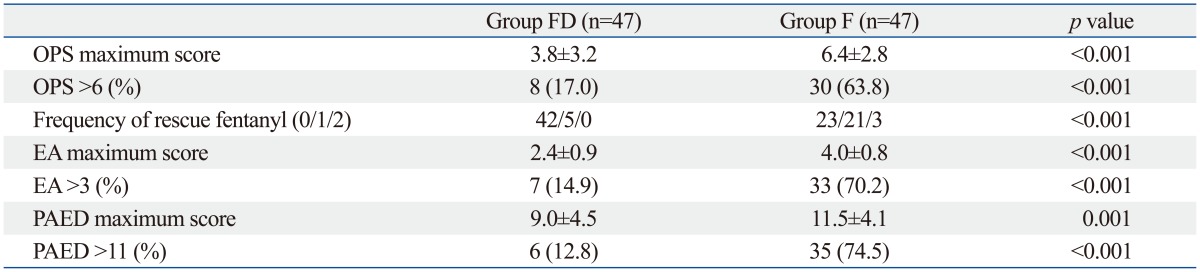
EA, emergence agitation score; OPS, objective pain score; PAED, Paediatric Agitation and Emergence Delirium.
Values are expressed as number of patients (percentage). The maximum EA, OPS and PAED scores are expressed as mean±SD.
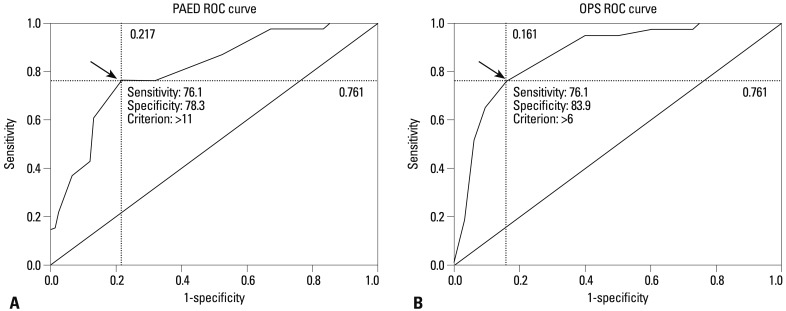
We performed a ROC curve analysis for the PAED scale and the OPS scale to define the cut-off points of severe EA, defined as a 5-point EA score of 4 and above and identified cut-off values that maximised sensitivity and specificity based on the ROC analysis. Thresholds of 11 for PAED and 6 for OPS were the best discriminators of severe EA.
The area under the ROC curve for PAED >11 was 0.77, with a sensitivity of 0.76 and specificity of 0.78 (Fig. 2A). The area under the ROC curve for an OPS >6 was 0.80, with sensitivity of 0.76 and specificity of 0.84 (Fig. 2B). When we classified severe EA as a PAED score >11, the incidence of severe EA was significantly lower in Group FD than in Group F (12.8% vs. 74.5%, p<0.001). We also compared the ROC curves of PAED scale and OPS scale by the Delong method. There was no significant difference between PAED and OPS scales in predicting severe EA (p=0.562).
Fig. 2.
Receiver operating characteristic (ROC) curve of PAED (A) and OPS score (B) for prediction of severe emergence agitation (EA≥4). Arrows indicate cut-off values. PAED, Paediatric Agitation Emergence Delirium; OPS, objective pain score.
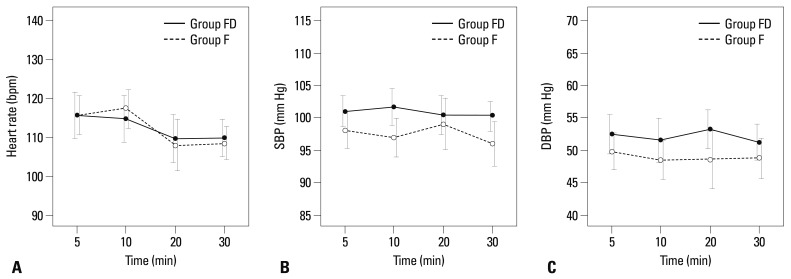
Haemodynamic instability did not occur in any of the patients and vital signs remained within 20% of baseline in all patients. HR, systolic blood pressure, and diastolic blood pressure were similar in both groups (Fig. 3).
Fig. 3.
Intra-operative haemodynamic data. (A) Heart rate, (B) systolic blood pressure and (C) diastolic blood pressure.
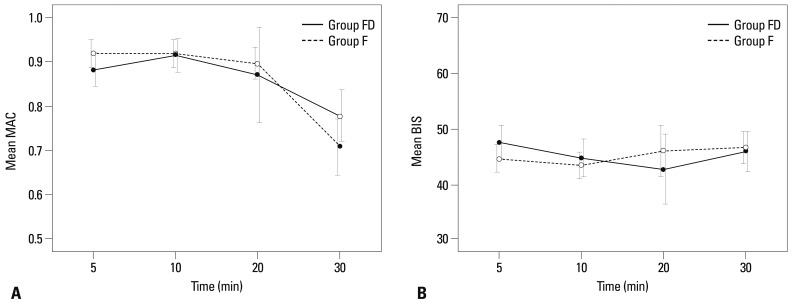
The intra-operative value of minimal alveolar concentration and bispectral index score were not different between the two groups (Fig. 4). When self-respiration (eye opening and extubation) occurred minimal alveolar concentration and bispectral index score values of the two groups were not different. Furthermore, there were no significant differences between groups with respect to the duration of emergence (Table 3).
Fig. 4.
Intra-operative sequential comparison of the changes in the age-adjusted minimum alveolar concentration of desflurane (A) and the bispectral index (B) between the two groups. MAC, minimal alveolar concentration; BIS, bispectral index score.
Table 3.
Recovery Profiles
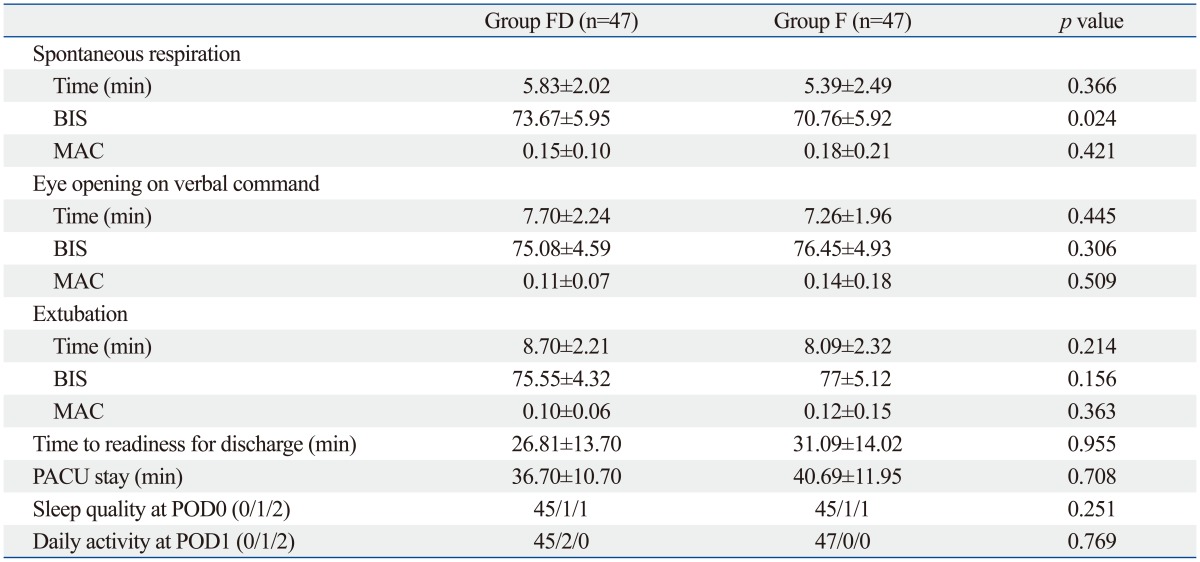
BIS, bispectral index score; MAC, minimal alveolar concentration; PACU, post-anaesthesia care unit; POD, postoperative day; PODSS, Post-Anaesthetic Discharge Scoring System.
Values given are mean±SD. Time to readiness for discharge means time from arrival at the PACU to achieving PODSS score of 8. Sleep quality on the night of operation (POD0): 0=slept well, 1=woke up crying in the night, 2=slept fitfully. Resumption of normal activity: 0=normal activity, 1=depressed but performed normal daily activities, 2=irritable and could not perform normal activity.
There was no statistical difference in the incidence of postoperative respiratory complications between the two groups. One desaturation event (haemoglobin oxygen saturation <95%) and one bronchospasm occurred in Group FD, but none occured in Group F.
There were no serious complications or significant differences in the 24-hours post-operative daily activities and sleep quality assessed by telephone interview with the patients' parents (Table 3).
DISCUSSION
Results of our study indicate that continuous intra-operative infusion of low-dose dexmedetomidine (0.2 µg/kg/h) can reduce the incidence of EA following desflurane anaesthesia in paediatric patients undergoing strabismus surgery. Furthermore, low-dose dexmedetomidine reduced postoperative pain without any haemodynamic compromise or delay of emergence.
Our primary outcome was the incidence of severe EA. When we defined severe EA as a 5-point EA score of 4 and above, low-dose dexmedetomidine reduced the incidence of severe EA by 79% compared with the saline control (14.9% vs. 70.2%, p<0.001) (Table 2). Previous studies reported a higher incidence of severe EA (up to 80%) after desflurane anaesthesia.1 Several studies report that 2.5 µg/kg fentanyl is effective in reducing severe EA without delay of emergence following desflurane anaesthesia in patients undergoing adenoidectomy or tonsillectomy.23,24 However, in our preliminary study, 2.5 µg/kg fentanyl delayed extubation time and PACU stay in children undergoing strabismus surgery despite a potent reduction of EA. Our data demonstrated that 1.0 µg/kg fentanyl and 0.2 µg/kg/h dexmedetomidine reduced the incidence of EA to the same level as 2.5 µg/kg fentanyl based on the previous study (7-24%)23,24 without delay of emergence. Many factors are associated with EA such as anaesthetic agents, rapid emergence from anaesthesia, the type of surgery, pain, preoperative anxiety and non-familiar environment.25,26 So far, the specific factors surrounding EA have been vague. EA in paediatric patients have complex causes. However, a strong connection between postoperative pain and EA has been supported by many studies.5,27-30 Postoperative satisfactory pain control is required to prevent EA, administration of 1.0 µg/kg fentanyl and local anaesthetic eye drops are considered to be enough for pain control in paediatric patients undergoing strabismus surgery. Recent meta-analysis reported propofol, pain prevention, ketamine and alpha 2-adrenergic receptor agonists appear to be effective to prevent EA.25 However, the superior drug among all of those drugs is not clear. Combined use of these agents and diversifying the routes of administration might be effective in reducing possible side effects.
A reliable, valid, and simple rating scale to measure postoperative EA in children is very important when taking care of paediatric patients in PACU. Although there are various assessment tools for evaluating EA, none is sufficiently specific and sensitive to assess children's behaviour upon emergence.4 We simultaneously used two assessment tools of emergence behaviour, PAED and OPS, and compared the incidence of severe EA based on the cut-off values of PAED and OPS score as well as the maximum PAED and OPS scores.31 Our data revealed that low-dose dexmedetomidine significantly reduced both the maximum scores and the incidence of EA based on the cut-off values of PAED and OPS. Furthermore, our study showed that PAED scoring and OPS scoring are equally able to predict severe EA.
The PAED scale developed by Sikich and Lerman19 consisting of five psychometric items for evaluating ED in paediatric patients is known to be reliable and has been validated.32,33 Sikich and Lerman19 defined true EA as a child who received pain killer post-operatively and negative EA as a child who did not. They reported that for a PAED score of 10 and above, the sensitivity was 0.64, the specificity was 0.86, and area under the ROC curve was 0.77. However, the cut-off value of PAED to determine severe EA has been inconsistently reported to range from 8 to 16.31,33,34 When we considered true EA as a 5-point EA of 4 and above, the threshold of PAED score to discriminate severe EA was 11.
The OPS scale has been used to assess pain in many studies with paediatric patients.11,14,22,35-37 In preschool aged paediatric patients it is not easy to distinguish pain from agitation. The OPS scale includes haemodynamic change, emotional factors (crying, agitation, and movement), and localisation of pain. For preschool children, many parts of this scale overlap the parameters of the PAED scale. Low-dose dexmedetomidine significantly reduced the OPS score and the frequency of rescue fentanyl use (Fig. 1, Table 3). Fig. 1 also shows that the OPS scoring pattern after arrival at PACU was very similar to that of the PAED scale, consistent with a previous study.22 Dexmedetomidine actually exerts an analgesic effect; therefore, it could reduce postoperative opioid use and the incidence of opioid-related complications such as pruritus, nausea, and respiratory depression.30,38 Because we applied fentanyl after induction and eye drops containing local anaesthetics at the end of surgery for postoperative pain control, the high OPS score upon arrival at PACU may reflect psychiatric properties. In this respect dexmedetomidine appears to exert not only an analgesic effect, but also an anxiolytic and sedative effect.
In our study, low-dose continuous infusion of dexmedetomidine without a loading dose did not affect haemodynamic changes during the perioperative phase. Intraoperative HR, systolic blood pressure, and diastolic blood pressure were not different between the two groups (Fig. 3). This result is consistent with a previous study.14 As the haemodynamic effects of dexmedetomidine are similar to those of 2 other alpha agonists, dexmedetomidine produces a dose-dependent decrease in HR and blood pressure.39 Deutsch and Tobias40 reported that an intravenous administration of 0.5 µg/kg of dexmedetomidine over 5 minutes caused an approximate 10% and 25% reduction in blood pressure and HR, respectively, in paediatric patients undergoing general anaesthesia. In addition, Patel, et al.22 reported that mean HR and mean systolic blood pressure were significantly reduced after administration of 0.7 µg/kg/h dexmedetomidine following a 2 µg/kg loading dose. We were concerned about the haemodynamic effects of dexmedetomidine, thus we reduced the infusion dose to almost one third of the recommended dose and without an initial loading dose. Despite the relatively low dose used in our study, we found that 0.2 µg/(kg·h)-1 was sufficient to prevent postoperative severe EA in paediatric patients without compromising haemodynamics. Although a higher dose of dexmedetomidine might further reduce the incidence of EA, it may also cause delay emergence and excessive haemodynamic changes which may mask an OCR. However, a previous study reported that premedication with a single bolus injection of dexmedetomidine (0.5 µg/kg) prevented OCR in paediatric patients undergoing strabismus surgery under general anaesthesia.7
Because we did not compare the incidence of OCR between the two groups, we could not evaluate the influence of the haemodynamic effects of dexmedetomidine on OCR. Our study merely shows there was no significant difference in haemodynamic effects resulting from continuous intraoperative infusion of 0.2 µg/(kg·h)-1 dexmedetomidine. None of our patients required atropine to treat bradycardia resulting from either OCR or dexmedetomidine.
Guler, et al.42 and Patel, et al.22 reported that a 0.5 µg/(kg·h)-1 of dexmedetomidine reduced agitation in paediatric tonsillectomy, but the emergence time was 2 minutes longer in the dexmedetomidine group compared with the control group. These delayed emergence could be explained by the administration time and total dose of dexmedetomidine. Considering the drug-onset time, administration of dexmedetomidine 5 minutes before the end of surgery35 could cause delayed awakening. In our study, the total infusion time was approximately 20 minutes and total dose of the drug was approximately 0.1 µg/kg. This is a relatively small dose, about one-fourth of that used in the previous studies. This low-dose dexmedetomidine infusion can facilitate rapid emergence as reflected by the extubation time, response on verbal command, PACU stay, and time to readiness for discharge (Table 3).
The major limitation of this study is the small number of patients recruited who underwent strabismus surgeries. More extensive randomized studies should be performed to determine the optimum dose of dexmedetomidine to prevent EA in paediatric patients in different types of surgery, which could affect the incidence of EA. Therefore, the dose of dexmedetomidine of this study might be modified according to the type of surgical procedure. Further studies are needed to evaluate the optimum dose of dexmedetomidine for variable types of surgery. Despite the small sample size, statistical power of our primary outcome was over 0.8 for each parameter and significant differences were found between Group FD and Group F. Limited to strabismus surgery, we demonstrated the preventive effect of dexmedetomidine. Further studies are required to evaluate the dexmedetomidine's effect on OCR. As mentioned above, we did not compare the incidence of OCR between the two groups. Nevertheless, our results show that low dose continuous infusion of dexmedetomidine without a loading dose did not induce hemodynamic change. Based on this result, a low dose infusion of dexmedetomidine might not affect the incidence of OCR.
In conclusion, intraoperative continuous infusion of low-dose dexmedetomidine [0.2 µg/(kg·h)-1] can reduce emergence agitation following desflurane anaesthesia without haemodynamic compromise or delayed awakening in paediatric patients undergoing strabismus surgery.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Voepel-Lewis T, Malviya S, Tait AR. A prospective cohort study of emergence agitation in the pediatric postanesthesia care unit. Anesth Analg. 2003;96:1625–1630. doi: 10.1213/01.ANE.0000062522.21048.61. [DOI] [PubMed] [Google Scholar]
- 2.Grundmann U, Uth M, Eichner A, Wilhelm W, Larsen R. Total in travenous anaesthesia with propofol and remifentanil in paediatric patients: a comparison with a desflurane-nitrous oxide inhalation anaesthesia. Acta Anaesthesiol Scand. 1998;42:845–850. doi: 10.1111/j.1399-6576.1998.tb05332.x. [DOI] [PubMed] [Google Scholar]
- 3.Dexter F, Macario A, Manberg PJ, Lubarsky DA. Computer simulation to determine how rapid anesthetic recovery protocols to decrease the time for emergence or increase the phase I postanesthesia care unit bypass rate affect staffing of an ambulatory surgery center. Anesth Analg. 1999;88:1053–1063. doi: 10.1097/00000539-199905000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Vlajkovic GP, Sindjelic RP. Emergence delirium in children: many questions, few answers. Anesth Analg. 2007;104:84–91. doi: 10.1213/01.ane.0000250914.91881.a8. [DOI] [PubMed] [Google Scholar]
- 5.Finley GA, McGrath PJ, Forward SP, McNeill G, Fitzgerald P. Parents' management of children's pain following 'minor' surgery. Pain. 1996;64:83–87. doi: 10.1016/0304-3959(95)00091-7. [DOI] [PubMed] [Google Scholar]
- 6.Mizrak A, Erbagci I, Arici T, Ozcan I, Ganidagli S, Tatar G, et al. Ketamine versus propofol for strabismus surgery in children. Clin Ophthalmol. 2010;4:673–679. doi: 10.2147/opth.s11336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mizrak A, Erbagci I, Arici T, Avci N, Ganidagli S, Oner U. Dexmedetomidine use during strabismus surgery in agitated children. Med Princ Pract. 2011;20:427–432. doi: 10.1159/000324554. [DOI] [PubMed] [Google Scholar]
- 8.Jung HJ, Kim JB, Im KS, Oh SH, Lee JM. Effect of ketamine versus thiopental sodium anesthetic induction and a small dose of fentanyl on emergence agitation after sevoflurane anesthesia in children undergoing brief ophthalmic surgery. Korean J Anesthesiol. 2010;58:148–152. doi: 10.4097/kjae.2010.58.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aouad MT, Yazbeck-Karam VG, Nasr VG, El-Khatib MF, Kanazi GE, Bleik JH. A single dose of propofol at the end of surgery for the prevention of emergence agitation in children undergoing strabismus surgery during sevoflurane anesthesia. Anesthesiology. 2007;107:733–738. doi: 10.1097/01.anes.0000287009.46896.a7. [DOI] [PubMed] [Google Scholar]
- 10.White PF, Tang J, Wender RH, Yumul R, Stokes OJ, Sloninsky A, et al. Desflurane versus sevoflurane for maintenance of outpatient anesthesia: the effect on early versus late recovery and perioperative coughing. Anesth Analg. 2009;109:387–393. doi: 10.1213/ane.0b013e3181adc21a. [DOI] [PubMed] [Google Scholar]
- 11.Welborn LG, Hannallah RS, Norden JM, Ruttimann UE, Callan CM. Comparison of emergence and recovery characteristics of sevoflurane, desflurane, and halothane in pediatric ambulatory patients. Anesth Analg. 1996;83:917–920. doi: 10.1097/00000539-199611000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Wachtel RE, Dexter F, Epstein RH, Ledolter J. Meta-analysis of desflurane and propofol average times and variability in times to extubation and following commands. Can J Anaesth. 2011;58:714–724. doi: 10.1007/s12630-011-9519-1. [DOI] [PubMed] [Google Scholar]
- 13.Davis PJ, Cohen IT, McGowan FX, Jr, Latta K. Recovery characteristics of desflurane versus halothane for maintenance of anesthesia in pediatric ambulatory patients. Anesthesiology. 1994;80:298–302. doi: 10.1097/00000542-199402000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Shukry M, Clyde MC, Kalarickal PL, Ramadhyani U. Does dexmedetomidine prevent emergence delirium in children after sevoflurane-based general anesthesia? Paediatr Anaesth. 2005;15:1098–1104. doi: 10.1111/j.1460-9592.2005.01660.x. [DOI] [PubMed] [Google Scholar]
- 15.Singh R, Kharbanda M, Sood N, Mahajan V, Chatterji C. Comparative evaluation of incidence of emergence agitation and post-operative recovery profile in paediatric patients after isoflurane, sevoflurane and desflurane anaesthesia. Indian J Anaesth. 2012;56:156–161. doi: 10.4103/0019-5049.96325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Isik B, Arslan M, Tunga AD, Kurtipek O. Dexmedetomidine decreases emergence agitation in pediatric patients after sevoflurane anesthesia without surgery. Paediatr Anaesth. 2006;16:748–753. doi: 10.1111/j.1460-9592.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- 17.Weldon BC, Watcha MF, White PF. Oral midazolam in children: effect of time and adjunctive therapy. Anesth Analg. 1992;75:51–55. doi: 10.1213/00000539-199207000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Hannallah RS, Broadman LM, Belman AB, Abramowitz MD, Epstein BS. Comparison of caudal and ilioinguinal/iliohypogastric nerve blocks for control of post-orchiopexy pain in pediatric ambulatory surgery. Anesthesiology. 1987;66:832–834. doi: 10.1097/00000542-198706000-00023. [DOI] [PubMed] [Google Scholar]
- 19.Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004;100:1138–1145. doi: 10.1097/00000542-200405000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Cole JW, Murray DJ, McAllister JD, Hirshberg GE. Emergence behaviour in children: defining the incidence of excitement and agitation following anaesthesia. Paediatr Anaesth. 2002;12:442–447. doi: 10.1046/j.1460-9592.2002.00868.x. [DOI] [PubMed] [Google Scholar]
- 21.Chung F, Chan VW, Ong D. A post-anesthetic discharge scoring system for home readiness after ambulatory surgery. J Clin Anesth. 1995;7:500–506. doi: 10.1016/0952-8180(95)00130-a. [DOI] [PubMed] [Google Scholar]
- 22.Patel A, Davidson M, Tran MC, Quraishi H, Schoenberg C, Sant M, et al. Dexmedetomidine infusion for analgesia and prevention of emergence agitation in children with obstructive sleep apnea syndrome undergoing tonsillectomy and adenoidectomy. Anesth Analg. 2010;111:1004–1010. doi: 10.1213/ANE.0b013e3181ee82fa. [DOI] [PubMed] [Google Scholar]
- 23.Cohen IT, Finkel JC, Hannallah RS, Hummer KA, Patel KM. The effect of fentanyl on the emergence characteristics after desflurane or sevoflurane anesthesia in children. Anesth Analg. 2002;94:1178–1181. doi: 10.1097/00000539-200205000-00023. [DOI] [PubMed] [Google Scholar]
- 24.Demirbilek S, Togal T, Cicek M, Aslan U, Sizanli E, Ersoy MO. Effects of fentanyl on the incidence of emergence agitation in children receiving desflurane or sevoflurane anaesthesia. Eur J Anaesthesiol. 2004;21:538–542. doi: 10.1017/s0265021504007069. [DOI] [PubMed] [Google Scholar]
- 25.Dahmani S, Stany I, Brasher C, Lejeune C, Bruneau B, Wood C, et al. Pharmacological prevention of sevoflurane- and desflurane-related emergence agitation in children: a meta-analysis of published studies. Br J Anaesth. 2010;104:216–223. doi: 10.1093/bja/aep376. [DOI] [PubMed] [Google Scholar]
- 26.Kim MS, Moon BE, Kim H, Lee JR. Comparison of propofol and fentanyl administered at the end of anaesthesia for prevention of emergence agitation after sevoflurane anaesthesia in children. Br J Anaesth. 2013;110:274–280. doi: 10.1093/bja/aes382. [DOI] [PubMed] [Google Scholar]
- 27.Davis PJ, Greenberg JA, Gendelman M, Fertal K. Recovery characteristics of sevoflurane and halothane in preschool-aged children undergoing bilateral myringotomy and pressure equalization tube insertion. Anesth Analg. 1999;88:34–38. doi: 10.1097/00000539-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Cravero JP, Beach M, Thyr B, Whalen K. The effect of small dose fentanyl on the emergence characteristics of pediatric patients after sevoflurane anesthesia without surgery. Anesth Analg. 2003;97:364–367. doi: 10.1213/01.ANE.0000070227.78670.43. [DOI] [PubMed] [Google Scholar]
- 29.Finkel JC, Cohen IT, Hannallah RS, Patel KM, Kim MS, Hummer KA, et al. The effect of intranasal fentanyl on the emergence characteristics after sevoflurane anesthesia in children undergoing surgery for bilateral myringotomy tube placement. Anesth Analg. 2001;92:1164–1168. doi: 10.1097/00000539-200105000-00016. [DOI] [PubMed] [Google Scholar]
- 30.Messerer B, Gutmann A, Weinberg A, Sandner-Kiesling A. Implementation of a standardized pain management in a pediatric surgery unit. Pediatr Surg Int. 2010;26:879–889. doi: 10.1007/s00383-010-2642-1. [DOI] [PubMed] [Google Scholar]
- 31.Bong CL, Ng AS. Evaluation of emergence delirium in Asian children using the Pediatric Anesthesia Emergence Delirium Scale. Paediatr Anaesth. 2009;19:593–600. doi: 10.1111/j.1460-9592.2009.03024.x. [DOI] [PubMed] [Google Scholar]
- 32.Blankespoor RJ, Janssen NJ, Wolters AM, Van Os J, Schieveld JN. Post-hoc revision of the pediatric anesthesia emergence delirium rating scale: clinical improvement of a bedside-tool? Minerva Anestesiol. 2012;78:896–900. [PubMed] [Google Scholar]
- 33.Janssen NJ, Tan EY, Staal M, Janssen EP, Leroy PL, Lousberg R, et al. On the utility of diagnostic instruments for pediatric delirium in critical illness: an evaluation of the Pediatric Anesthesia Emergence Delirium Scale, the Delirium Rating Scale 88, and the Delirium Rating Scale-Revised R-98. Intensive Care Med. 2011;37:1331–1337. doi: 10.1007/s00134-011-2244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen J, Li W, Hu X, Wang D. Emergence agitation after cataract surgery in children: a comparison of midazolam, propofol and ketamine. Paediatr Anaesth. 2010;20:873–879. doi: 10.1111/j.1460-9592.2010.03375.x. [DOI] [PubMed] [Google Scholar]
- 35.Erdil F, Demirbilek S, Begec Z, Ozturk E, Ulger MH, Ersoy MO. The effects of dexmedetomidine and fentanyl on emergence characteristics after adenoidectomy in children. Anaesth Intensive Care. 2009;37:571–576. doi: 10.1177/0310057X0903700405. [DOI] [PubMed] [Google Scholar]
- 36.Saadawy I, Boker A, Elshahawy MA, Almazrooa A, Melibary S, Abdellatif AA, et al. Effect of dexmedetomidine on the characteristics of bupivacaine in a caudal block in pediatrics. Acta Anaesthesiol Scand. 2009;53:251–256. doi: 10.1111/j.1399-6576.2008.01818.x. [DOI] [PubMed] [Google Scholar]
- 37.Akin A, Bayram A, Esmaoglu A, Tosun Z, Aksu R, Altuntas R, et al. Dexmedetomidine vs midazolam for premedication of pediatric patients undergoing anesthesia. Paediatr Anaesth. 2012;22:871–876. doi: 10.1111/j.1460-9592.2012.03802.x. [DOI] [PubMed] [Google Scholar]
- 38.Tufanogullari B, White PF, Peixoto MP, Kianpour D, Lacour T, Griffin J, et al. Dexmedetomidine infusion during laparoscopic bariatric surgery: the effect on recovery outcome variables. Anesth Analg. 2008;106:1741–1748. doi: 10.1213/ane.0b013e318172c47c. [DOI] [PubMed] [Google Scholar]
- 39.Bhana N, Goa KL, McClellan KJ. Dexmedetomidine. Drugs. 2000;59:263–268. doi: 10.2165/00003495-200059020-00012. [DOI] [PubMed] [Google Scholar]
- 40.Deutsch E, Tobias JD. Hemodynamic and respiratory changes following dexmedetomidine administration during general anesthesia: sevoflurane vs desflurane. Paediatr Anaesth. 2007;17:438–444. doi: 10.1111/j.1460-9592.2006.02139.x. [DOI] [PubMed] [Google Scholar]
- 41.Braun U, Feise J, Mühlendyck H. Is there a cholinergic and an adrenergic phase of the oculocardiac reflex during strabismus surgery? Acta Anaesthesiol Scand. 1993;37:390–395. doi: 10.1111/j.1399-6576.1993.tb03735.x. [DOI] [PubMed] [Google Scholar]
- 42.Guler G, Akin A, Tosun Z, Ors S, Esmaoglu A, Boyaci A. Single-dose dexmedetomidine reduces agitation and provides smooth extubation after pediatric adenotonsillectomy. Paediatr Anaesth. 2005;15:762–766. doi: 10.1111/j.1460-9592.2004.01541.x. [DOI] [PubMed] [Google Scholar]