Abstract
Patient: Male, 43
Final Diagnosis: Neurofibromatosis
Symptoms: Hip pain
Medication: —
Clinical Procedure: —
Specialty: Orthopedics and Traumatology
Objective:
Rare disease
Background:
Neurofibromatosis type 1 is a disease known for orthopedic manifestations such as spine deformities, congenital pseudarthrosis of the tibia and other bony dysplasias; joint dislocations are rare. Joint arthritis caused by neurofibromatosis, with a stable hip, has never been reported in the English literature before.
Case Report:
A 43-year-old man diagnosed with neurofibromatosis type 1 (NF-1) presented with hip pain of 5 years duration, with no history of trauma and no clinical or radiological signs of dislocation. He had classical clinical and radiological signs of hip arthritis, with acetabular erosions and femoral head arthritis. The patient was treated with total hip arthroplasty metal-on-metal (MoM).
Conclusions:
Hip arthritis alone without subluxation or dislocation due to NF-1 is an extremely rare presentation. This is the first reported presentation and provisional treatment with total hip arthroplasty.
MeSH Keywords: Arthritis, Arthroplasty, Replacement, Hip, Neurofibromatosis 1
Background
Neurofibromatosis is a disease first described by the German pathologist Frederick von Recklinghausen in 1882 [1], hence the other name for it is Recklinghausen’s disease. It is an autosomal-dominant genetic defect, with an incidence of 1 in 3000 world-wide. NF-1 is the most common type [2] Other less frequent types include neurofibromatosis type 2 (NF-2) and a very rare subtype of NF-1 called segmental neurofibromatosis, but these are not related to orthopedic manifestations [3]. Diagnosis criteria were defined in 1986 by the National Institutes of Health [4]. Spine abnormalities, congenital pseudarthrosis of the tibia, metabolic bone disorders, and disturbed growth patterns are all know orthopedic manifestations of NF-1.
Case Report
We present the case of a 43-year-old man diagnosed with neurofibromatosis type 1 who presented to our institute complaining of severe left hip pain, which had been affecting his daily life for the past 5 years. Physical examination revealed no swelling, but he had limited range of motion in the hip, with a positive Trendelenburg gait on the same side. Neurological examination was within normal limits. Walking distance was limited to 50 m because of pain. Radiologic examination showed severe hip arthritis with no subluxation, complicated by protrusio acetabuli (PA) according to the method of Gusis et al for measuring PA [5] (Figures 1 and 2). The patient had a leg length discrepancy of 2 cm. Due to the limitation of activity this diseased hip was causing, he was planned for total hip arthroplasty. Pre-operative planning focused on addressing any acetabular deficiency intraoperatively, addressing the PA, having a stable prosthesis, and addressing the leg-length discrepancy. This required us to prepare acetabular cages, bulk allografts, morselized bone graft, and acetabular augments. Pre-operative planning for the femoral side included preparing multiple neck offsets, narrow stems, and a modular stem. We used a direct lateral hip approach (Hardinge). Intra-operatively, no neurofibromas or soft-tissue masses were seen. The femoral head was deformed, which necessitated an in situ neck osteotomy to remove the head. We used a non-cemented metal-on-metal prosthesis (M2a-Magnum™ Biomet, Warsaw, IN, USA) size 64 mm tantalum shell. The fixation was secure and no screw augmentation was required. The head size was 32 mm, the femoral stem was 16, and a −3 neck offset was used. Post-operatively, the patient was allowed to engage in immediate weight-bearing with hip precaution. Two-year post-operative images are shown in Figure 3A and 3B. A 2-year follow-up showed no clinical or radiological signs of loosening. Regarding his physical activity at 2 years after surgery, he was able to walk without pain and climb stairs, but no objective quality of life (QoL) tool was available at the time of assessment.
Figure 1.

AP pelvis x-ray showing arthritic left hip.
Figure 2.

3D reconstruction computerized tomography showing an arthritic left hip.
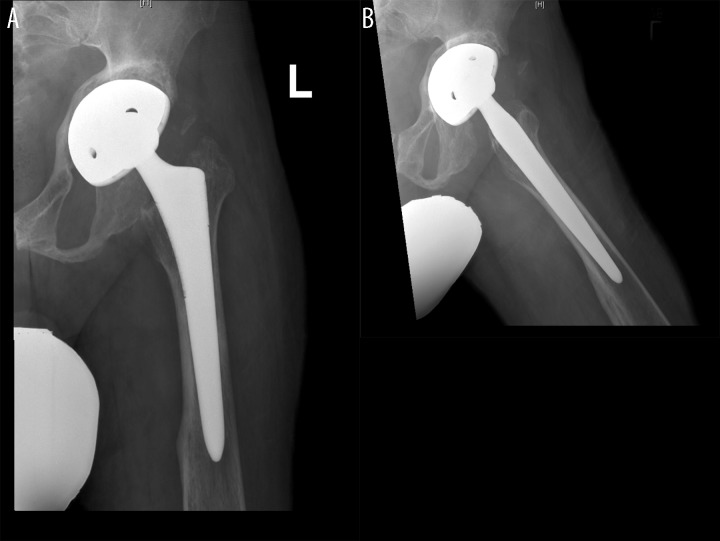
Figure 3.
(A, B) Two year follow up x-rays showing the prostheses in a stable position with no sign of radiological loosening.
Discussion
Hip dislocation due to NF-1 is thought to be associated with plexiform neurofibromas (either intra-articular or surrounding the hip joint) and is a rare complication of the disease, only reported 9 times [6–8]. All cases had bony changes in terms of erosions, acetablular dysplasia, or coxa valga [7]. Other factors include muscle imbalance caused by spinal tumors [9]. Only 1 case was reported in the English literature as a dislocation without evidence of intra-articular neurofibromas, by Odent et al. [7]. To our knowledge, arthritis secondary to NF-1 with a stable hip has never been reported in the literature. Unlike the previous 9 case reports, arthritis is accompanied by subluxation or dislocation and intra-articular neurofibromas; unlike this case, which presented with arthritis alone.
Mandell et al. [10] reported a rate of 21% of PA compared to 9% in the control group and was the first to report this skeletal abnormality; 13% of the NF-1 patients had PA that was more progressive. Total hip arthroplasty in such cases becomes challenging due to possible abductor weakness or the loss of sensory protection at the hip, as hypothesized by Phillips et al. [11], risking hip dislocation. This may lead surgeons to use constrained hips, as suggested by Odent et al. [7], with no idea about the long-term results of such prosthesis use. Tangsataporn et al. [8] reported good results with 1-year follow-up using a trochanteric advancement technique and a trabeculated metal shell with a 36-mm head with a post-operative abduction splint for 6 weeks. In our case, there was structural deformity in the acetabulum, and the radiographs resembled post-traumatic arthritis. In such cases, augments or bulk allograft may be required and larger heads improve stability.
Conclusions
Hip arthritis alone due to NF-1 is extremely rare and hip; arthroplasty is a valid option and should be planned carefully, considering the nature of the neurofibromatosis. Here, we present the first case report of hip arthritis without subluxation, dislocation, or intra-articular neurofibromas.
References:
- 1.Crump T. Translation of case reports in Ueber die multiplen Fibrome der Haut und ihre Beziehung zu den multiplen Neuromen by F. v. Recklinghausen. Adv Neurol. 1981;29:259–75. [PubMed] [Google Scholar]
- 2.Friedman JM. Epidemiology of neurofibromatosis type 1. Am J Med Genet. 1999;89(1):1–6. [PubMed] [Google Scholar]
- 3.Feldman DS, Jordan C, Fonseca L. Orthopaedic manifestations of neurofibromatosis type 1. J Am Acad Orthop Surg. 2010;18(6):346–57. doi: 10.5435/00124635-201006000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Stumpf D, Alksne J, Annegers J, et al. Neurofibromatosis. Conference statement. National institutes of health consensus development conference. Arch Neurol. 1988;45(5):575–78. [PubMed] [Google Scholar]
- 5.Gusis SE, Babini JC, Garay SM, et al. Evaluation of the measurement methods for protrusio acetabuli in normal children. Skeletal Radiol. 1990;19(4):279–82. doi: 10.1007/BF00191672. [DOI] [PubMed] [Google Scholar]
- 6.Galbraith JG, Butler JS, Harty JA. Recurrent spontaneous hip dislocation in a patient with neurofibromatosis type 1: a case report. J Med Case Rep. 2011;5:106. doi: 10.1186/1752-1947-5-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Odent T, Ranger P, Aarabi M, et al. Total hip arthroplasty in a patient with neurofibromatosis type I and recurrent spontaneous hip dislocation. Can J Surg. 2004;47(3):219–20. [PMC free article] [PubMed] [Google Scholar]
- 8.Tangsataporn S, Shakib A, Kuzyk PR, et al. Secondary Hip Osteoarthritis due to Neurofibroma Treated with Total Hip Replacement. Case Rep Orthop. 2012;2012:173921. doi: 10.1155/2012/173921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haga N, Nakamura S, Taniguchi K, Iwaya T. Pathologic dislocation of the hip in von Recklinghausen’s disease: a report of two cases. J Pediatr Orthop. 1994;14(5):674–76. doi: 10.1097/01241398-199409000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Mandell GA, Harcke HT, Scott CI, et al. Protrusio acetabuli in neurofibromatosis: nondysplastic and dysplastic forms. Neurosurgery. 1992;30(4):552–56. doi: 10.1227/00006123-199204000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Phillips JE, McMaster MJ. Pathological dislocation of the hip in neurofibromatosis. J R Coll Surg Edinb. 1987;32(3):180–82. [PubMed] [Google Scholar]