Summary
Transient osteoporosis is a relatively rare condition of unknown etiology that causes temporary bone loss. The syndrome is characterized by self-limited course and spontaneous resolution after 6 to 12 months. The pathogenesis of transient osteoporosis is not fully understood but several hypotheses that have been proposed include trauma, neurovascular dysfunction and transient hyperemia. Clinical manifestations include sudden onset of pain in the hip that usually worsens with weight bearing and leads to functional disability involving the affected extremity. Radiographs are frequently unremarkable, but may reveal periarticular osteopenia 3–6 weeks after the onset of clinical symptoms. There is no radiographic evidence of demineralization during the early phase of syndrome, as a result advanced imaging is required. Magnetic resonance imaging is the most sensitive and predictable test for an early diagnosis and monitoring of disease progression.
Keywords: transient osteoporosis, hip joint, MRI, bone marrow edema
Background
Transient osteoporosis of the hip is a relatively rare disorder characterized by loss of bone tissue in the proximal femur. Hip joint is the most common location of the disease, although it may also involve the knee, ankle or foot bones. Self-limited nature of the disease is characteristic with complete relief of symptoms occurring after 6–12 months [1–4]. Transient osteoporosis usually occurs in middle-aged men and women in the third trimester of pregnancy or immediately after birth [2,5,6]. The first reported case of the disease described in 1959, concerned pregnant women. Pathogenesis is still unclear. One of the original hypotheses concerning pathophysiology included impaired venous outflow and local congestion caused by an increase in intramedullary pressure [7]. Other reports suggest that the condition is caused by microdamage, which results in a temporary stimulation of bone resorption [1]. In case of pregnant women, parathyroid hormone-related protein (PTHrP) is considered to play an important role in the pathogenesis [8].
Symptoms and Treatment
The disorder develops in 3 stages. The initial symptom consists of a sudden hip pain radiating to the groin, buttocks or thigh. The pain increases upon bearing weight on the affected limb and gradually restricts movement. Reduction in passive and active movement of the hip is observed on physical examination. The hip is tender on palpation. The second stage involves demineralization of the head, neck and intertrochanteric region of the femur, without narrowing of joint space, visualized on an x-ray. Therapeutic window is characterized by the presence of pain with no abnormalities visible on an x-ray. During this period, diagnosis can be made with magnetic resonance imaging, which can be used to identify transient osteoporosis in as little as 48 hours from the onset of symptoms [1,2]. Computed tomography is not routinely used to detect the condition, although it was suggested by some publications for its early detection of trabecular bone fractures and reduction in the density of the femur [9]. The final stage consists of a full and concurrent resolution of clinical and radiological symptoms.
Transient osteoporosis is treated conservatively with limited weight bearing on the affected limb, thigh muscle strengthening exercises, range of motion exercises and analgesics. The main purpose of this approach is to prevent the development of microtrauma and fatigue fractures [10,11]. Some physicians recommend bisphosphonates for symptom relief [12,13].
Magnetic Resonance Imaging
Transient osteoporosis of the hip can only be recognized after more aggressive and irreversible diseases with similar clinical symptoms have been excluded. Differential diagnosis includes stress fractures, regional migratory osteoporosis, complex regional pain syndrome (Sudeck’s syndrome), primary bone tumors, metastases to the femur, infectious, reactive, or rheumatoid arthritis, osteomyelitis, sickle cell anemia, leukemia and avascular bone necrosis. Magnetic resonance imaging is an essential diagnostic tool that can differentiate between these states.
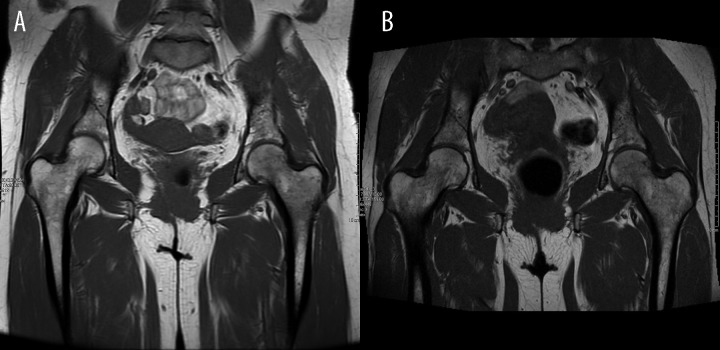
All of these disease entities may be accompanied by edema of the bone marrow presenting on an MRI as low signal intensity on T1-weighted imaging (Figure 1A), T1-weighted TSE (Figure 1B) and high intensity on T2-weighted (Figure 2A), TIRM (Figure 2B) and STIR sequences (Figure 3), and increased intensity after administration of a paramagnetic contrast [14–22]. The absence of additional focal lesions in the subchondral bone is a very sensitive and specific sign of transient osteoporosis that differentiates it from chronic conditions. Additionally, T2-weighted imaging may reveal hip joint effusion which commonly accompanies this disorder [21].
Figure 1.
(A, B) Transient osteoporosis of the hip in T1-weighted and T1-weighted Turbo Spin Echo imaging.
Figure 2.
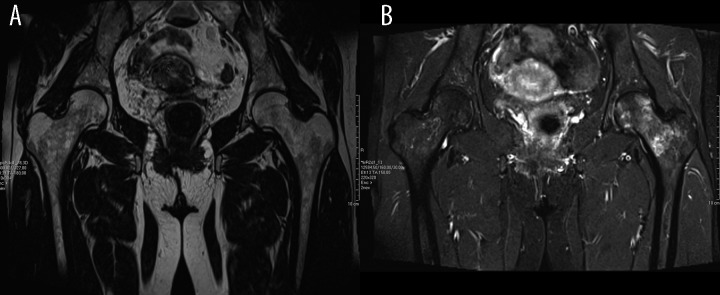
(A, B) Coronal T2-weighted and TIRM sequence images of patient with transient osteoporosis of the hip.
Figure 3.
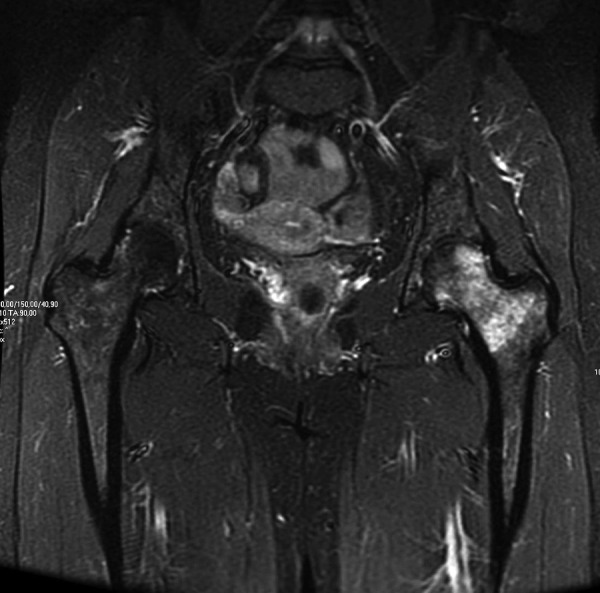
Coronal STIR sequence reveals edema of the bone marrow as high signal intensity.
Thickening of the medial cortex of the femoral neck and a fracture line with weak signal that may result from the weakened bone structure due to transient osteoporosis are characteristic findings in stress fracture imaging. In case of differentiation with complex regional pain syndrome, focus should be shifted to additional changes, such as skin atrophy, sensorimotor impairment and contractures [14].
Differentiation between transient osteoporosis and necrosis of the femoral bone poses the greatest diagnostic challenge. In the early stages, symptoms of both diseases are identical and affect similar age group of patients. Alcohol abuse, steroid therapy, sickle cell anemia, systemic lupus erythematosus and rheumatoid arthritis are the risk factors for the necrosis of the femoral head and are present in most cases. T1-weighted imaging shows very early changes involving the surrounding area of the necrotic bone ring of the fibrous connective tissue with a weak signal. In contrast to transient osteoporosis, bone marrow edema does not occur in the early stages of femoral necrosis. However, it presents in more advanced stages of necrosis and correlates with fracture of the femoral head and progression of pain, although according to some authors it is a weak prognostic factor [23–26].
There is an increasing number of case reports concerning transient osteoporosis of the hip available in the literature. Therefore, it is important to take it into account when forming the differential diagnosis of hip pain. Magnetic resonance imageing is the most important test that will distinguish this condition from other pathologies.
Precise analysis of images with a narrow field of view and a large sensor allows for a correct diagnosis at an early stage of the disease.
References
- 1.Korompilias AY, Karantanas AH, Lykissas M, et al. Transient osteoporosis. J Am Acad Orthop Surg. 2008;16:480–89. doi: 10.5435/00124635-200808000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Van Wagenen K, Pritchard P, Taylor JA. Transient osteoporosis of the hip: A case report. J Can Chiropr Assoc. 2013;57(2):116–22. [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen I, Melamed E, Lipkin A, et al. Transient osteoporosis of pregnancy complicated by a pathologic subcapital hip fracture. J Trauma. 2007;62:1281–83. doi: 10.1097/01.ta.0000198206.60286.2f. [DOI] [PubMed] [Google Scholar]
- 4.Chowdhury FU, Robinson P, Grainger AJ, et al. Transient regional osteoporosis: a rare cause of foot and ankle pain. Foot Ankle Surg. 2006;12:79–83. [Google Scholar]
- 5.Ma FY, Falkenberg M. Case reports: transient osteoporosis of the hip: an atypical case. Clin Orthop Relat Res. 2006;445:245–49. doi: 10.1097/01.blo.0000201154.44572.d2. [DOI] [PubMed] [Google Scholar]
- 6.Pai WC, Lin CY, Kao MJ, et al. Transient osteoporosis of the hip during pregnancy: a case report. Tw J Phys Med Rehabil. 2009;37:131–37. [Google Scholar]
- 7.Hofmann S, Engel A, Neuhold A, et al. Bone-marrow edema syndrome and transient osteoporosis of the hip: An MRI-controlled study of treatment by core decompression. J Bone Joint Surg Br. 1993;75:210–16. doi: 10.1302/0301-620X.75B2.8444939. [DOI] [PubMed] [Google Scholar]
- 8.Funk JL, Shoback DM, Genant HK. Transient osteoporosis of the hip in pregnancy: natural history of changes in bone mineral density. Clin Endocrinol (Oxf) 1995;43:373–82. doi: 10.1111/j.1365-2265.1995.tb02046.x. [DOI] [PubMed] [Google Scholar]
- 9.Kim YL, Nam KW, Yoo JJ, et al. CT evidence for subchondral trabecular injury of the femoral head in transient osteoporosis of the hip: a case report. J Korean Med Sci. 2010;25:192–95. doi: 10.3346/jkms.2010.25.1.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diwanji SR, Cho YJ, Xin ZF, Yoon TR. Conservative treatment for transient osteoporosis of the hip in middle – aged women. Singapore Med J. 2008;49(1):e17. [PubMed] [Google Scholar]
- 11.Lakhanpal S, Ginsburg WW, Luthra HS, et al. Transient regional osteoporosis. A study of 56 cases and review of the literature. Ann Intern Med. 1987;106:444–50. doi: 10.7326/0003-4819-106-3-444. [DOI] [PubMed] [Google Scholar]
- 12.Seok H, Kim YT, Kim SH, et al. Treatment of transient osteoporosis of the hip with intravenous zoledronate – a case report. Ann Rehabil Med. 2011;35(3):432–35. doi: 10.5535/arm.2011.35.3.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emad Y, Ragab Y, El-Shaarawy N, et al. Transient osteoporosis of the hip, complete resolution after treatment with alendronate as observed by MRI description of eight cases and review of the literature. Clin Rheumatol. 2012;31(11):1641–47. doi: 10.1007/s10067-012-2060-y. [DOI] [PubMed] [Google Scholar]
- 14.Gemmel F, Van Der Veen HC, Van Schelven WD, et al. Multi-modality imaging of transient osteoporosis of the hip. Acta Orthop Belg. 2012;78(5):619–27. [PubMed] [Google Scholar]
- 15.Wilson AJ, Murphy WA, Hardy DC, et al. Transient osteoporosis: transient bone marrow edema? Radiology. 1988;167:757–60. doi: 10.1148/radiology.167.3.3363136. [DOI] [PubMed] [Google Scholar]
- 16.Ragab Y, Emad Y, Abou-Zeid A. Bone marrow edema syndromes of the hip: MRI features in different hip disorders. Clin Rheumatol. 2008;27:475–82. doi: 10.1007/s10067-007-0731-x. [DOI] [PubMed] [Google Scholar]
- 17.Vande Berg BC, Lecouvet FE, Koutaissoff S, et al. Bone marrow edema of the femoral head and transient osteoporosis of the hip. Eur J Radiol. 2008;67(1):68–77. doi: 10.1016/j.ejrad.2008.01.061. [DOI] [PubMed] [Google Scholar]
- 18.Bloem JL. Transient osteoporosis of the hip: MR imaging. Radiology. 1988;167(3):753–55. doi: 10.1148/radiology.167.3.3363135. [DOI] [PubMed] [Google Scholar]
- 19.Karantanas AH. Acute bone marrow edema of the hip: role of MR imaging. Eur Radiol. 2007;17:2225–36. doi: 10.1007/s00330-007-0591-4. [DOI] [PubMed] [Google Scholar]
- 20.James SL, Hughes RJ, Ali KE, et al. MRI of bone marrow oedema associated with focal bone lesions. Clin Radiol. 2006;61:1003–9. doi: 10.1016/j.crad.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 21.Vande Berg B, Lecouvet F, Koutaïssoff S, et al. Transient bone marrow edema of the hip. J Radiol. 2011;92(6):557–66. doi: 10.1016/j.jradio.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 22.Ma FY, Falkenberg M. Case reports: transient osteoporosis of the hip: an atypical case. Clin Orthop Relat Res. 2006;445:245–49. doi: 10.1097/01.blo.0000201154.44572.d2. [DOI] [PubMed] [Google Scholar]
- 23.Vande Berg BC, Malghem JJ, Lecouvet FE, et al. Idiopathic bone marrow edema lesions of the femoral head: predictive value of MR imaging findings. Radiology. 1999;212(2):527–35. doi: 10.1148/radiology.212.2.r99au03527. [DOI] [PubMed] [Google Scholar]
- 24.Ito H, Matsuno T, Minami A. Relationship between bone marrow edema and development of symptoms in patients with osteonecrosis of the femoral head. Am J Roentgenol. 2006;186:1761–70. doi: 10.2214/AJR.05.0086. [DOI] [PubMed] [Google Scholar]
- 25.Kim YM, Oh HC, Kim HJ. The pattern of bone marrow oedema on MRI in osteonecrosis of the femoral head. J Bone Joint Surg Br. 2000;82(6):837–41. doi: 10.1302/0301-620x.82b6.10740. [DOI] [PubMed] [Google Scholar]
- 26.Fernandez-Canton G. From bone marrow edema to osteonecrosis. New concepts. Reumatol Clin. 2009;5(5):223–27. doi: 10.1016/j.reuma.2008.02.004. [DOI] [PubMed] [Google Scholar]