Abstract
Some of the most prevalent and debilitating pain conditions arise from the structures innervated by the trigeminal system (head, face, masticatory musculature, temporomandibular joint and associated structures). Orofacial pain (OFP) can arise from different regions and etiologies. Temporomandibular disorders (TMD) are the most prevalent orofacial pain conditions for which patients seek treatment. Temporomandibular disorders include a number of clinical problems that involve the masticatory musculature, the temporomandibular joint (TMJ) or both. Trigeminal neuropathic pain conditions can arise from injury secondary to dental procedures, infection, neoplasias, or disease or dysfunction of the peripheral and/or central nervous system. Neurovascular disorders, such as primary headaches, can present as chronic orofacial pain, such as in the case of facial migraine, where the pain is localized in the second and third division of the trigeminal nerve. Together, these disorders of the trigeminal system impact the quality of life of the sufferer dramatically. A multidisciplinary pain management approach should be considered for the optimal treatment of orofacial pain disorders including both non-pharmacological and pharmacological modalities.
Keywords: pain, orofacial, neuropathic, TMD, trigeminal, headache
Orofacial pain disorders
Orofacial pain disorders are highly prevalent and debilitating conditions involving the head, face, and neck. These conditions represent a challenge to the clinician since the orofacial region is complex and therefore, pain can arise from many sources. The clinician needs to have solid knowledge of the pain conditions that arise from these structures for proper diagnosis and a multidisciplinary approach of management is strongly recommended.
The orofacial pain classification as outlined by Okeson1,2 is divided into physical (Axis 1) and psychological (Axis 2) conditions. Physical conditions comprise temporomandibular disorders (TMD), which include disorders of the temporomandibular joint (TMJ) and disorders of the musculoskeletal structures (eg, masticatory muscles and cervical spine); neuropathic pains, which include episodic (eg, trigeminal neuralgia [TN]) and continuous (eg, peripheral/centralized mediated) pains and neurovascular disorders (eg, migraine). Psychological conditions include mood and anxiety disorders. This review focuses on the current perspectives in orofacial pain management, and only TMD, neuropathic pains, and headaches will be discussed. For a more comprehensive discussion about pathophysiology and diagnosis of the disorders depicted in this classification and other painful disorders arising from the head, face, and neck, other texts should be reviewed.
TMD
“TMD” defines a number of clinical problems that involve the masticatory musculature, the TMJ, and associated structures.3 TMD is considered to be a subclassification of musculoskeletal disorders1 and is the most prevalent condition for which patients seek treatment.4,5 The careful evaluation of these facial structures in conjunction with clinical symptoms is crucial in forming a proper differential diagnosis. The patient may present with jaw ache, earache, toothache, facial pain, and/or headache; however, the complaint may be as benign as general facial fullness or pressure. Treatment planning depend on various factors, including the chief complaint, medical history, presenting symptoms, examination, and diagnosis. In the past, TMD cases have sometimes been considered to be difficult to diagnose and problematic to treat; however, thanks to ongoing research in orofacial pain and pain management, clinicians are able to use a more standardized classification and better diagnostic and therapeutic methods to offer patients a wide range of treatment modalities with higher success rates.
Natural history and epidemiology of TMD
Most epidemiological studies clearly demonstrate that TMD symptoms are more commonly seen in women than in men,1 and that many symptoms seem to arise in adolescence or the early twenties and may continue intermittently, well into middle age; however, TMD symptomatology does get better with time, supporting a conservative management approach. In a study by Solberg et al,6 76% of subjects aged 18–25 years had one or more signs associated with TMD and 26% had at least one symptom associated with TMD. Of this group, only 10% had symptoms that were considered by the subjects to be severe enough to seek treatment. Rasmussen7 found that most cases of a clicking TMJ did not evolve into an open or closed locking state. Rasmussen noted that, in the natural progression of internal derangement, acute TMD symptoms lasted a mean of 5.5 years and that, although joint noises generally did not disappear, most painful and disabling symptoms subsided in time. Similar results were shown by Könönen et al, who followed 128 Finnish adults over 9 years, in whom the incidence of clicking increased with age.8 None of the patients, however, developed locking. In a more recent study, the presence of degenerative joint disorders was found to be the discriminating factor in two different age subgroups: patients with a mean age range of 52 years presented a prevalence of crepitus, while patients with a mean age range of 38 years did not.9
Disorders of the TMJ
Disorders of the TMJ are a result of a disc–condyle incoordination that influences the TMJ biomechanics. These disorders comprise the disc interference disorders or internal derangements, such as disc displacements with and without reduction, that can be asymptomatic or symptomatic due to inflammation (eg, capsulitis/synovitis). Disc displacements with reduction may present as a painful or non-painful click. Disc displacements without reduction may present with a painful limitation at opening. Retrodiscitis and TMJ subluxation may present symptomatology when the pain is a result of inflammation arising from the retrodiscal tissues or capsulitis or synovitis processes. Osteoarthritic changes can originate in the TMJ articular surfaces and, when they are influenced by a systemic disease, can become aggressive and progressive, such as in the case of polyarthritis.
Muscular disorders
Myalgia usually presents as a dull aching pain due to muscle injury or strain. It is commonly seen in acute forms, though, with continued muscle tension, can present for longer periods of time. Treatment may include, rest, hot or cold compresses, stretching exercises, and muscle relaxants. Myofascial pain (MFP) also presents as a dull, continuous aching pain that varies in intensity. MFP produces pain upon palpation that is local and may refer to other sites, as mapped out by Simons et al.10 MFP tends to be seen in muscle pain conditions of a more chronic nature, in which the tension is unremitting. Trigger points can often be seen in MFP and may be localized to a taut band of muscle. In addition, trigger points are associated with decreased muscle length and, when stimulated, can result in a local twitch response.11 Palpation of the trigger points should duplicate the patient’s pain complaint, thus confirming diagnosis. Blocking the source of the pain (ie, masseter muscle) by using a vapocoolant spray or local anesthetic injection can also provide a definitive diagnosis.
Myositis is a localized transient swelling involving the muscle and facial tissues.12 There tends to be increased pain with mandibular movement and localized tenderness, usually following injury or infection.
Patient evaluation
TMD assessment should include a general examination of the head and neck, a detailed examination of the masticatory muscles, an evaluation of the TMJs, an evaluation of mandibular range of motion (ROM), and a detailed intraoral examination.13
Evaluation of the TMJs and mandibular ROM
The evaluation of the TMJs includes examination for any signs of dysfunction or pain symptomatology. Fingertips are placed over the lateral and posterior aspects of the TMJs applying light but steady force and performed when the mandible is at rest/closed position and opening. Symptomatology reported in response to force applied to the lateral aspect of TMJs may be a sign of capsulitis/synovitis. Symptomatology reported in response of force applied to the posterior aspect of the condyle may be a sign of retrodiscitis or posterior capsulitis.
The clinician should be aware of joint sounds, which could present as clicks, pops, or crepitus.1 These sounds are evaluated with the help of a stethoscope placed in the TMJ area or sometimes perceived during palpation. Clicks and pops are commonly related to disc displacements with reduction and crepitation is commonly associated with osteoarthritic changes in the articular surfaces of the TMJ.14 Imaging of the TMJ may also be useful during examination. Moreover, it is very important to identify any TMJ restrictions. The clinician should view the patient’s opening and closing patterns to note any mandibular deviations. The evaluation of mandibular ROM consists of measuring comfort opening, active opening, passive opening, protrusion, and left and right lateral excursions with a millimeter ruler while noting the severity and location of pain with jaw movement. This can be particularly helpful in differentiating between joint and muscle pain. Comfort opening is determined by the patient opening as wide as possible without any pain, active opening is determined by the patient opening as wide as possible with pain, and passive opening is determined by the clinician gently stretching the patient presumably past active opening while noting a soft or hard end feel. A reasonably normal interincisal distance is approximately 40 mm, or the width of three of the patient’s fingers as a crude measure. Usually, with proper questioning, the patient will reliably reveal any recent limitations in ROM. The occurrence of TMJ clicking, crepitus, or jaw opening interferences with or without pain should also be noted at the initial examination. These baseline findings will aid in establishing the differential diagnosis and treatment options, as well as providing a comparison for future change in TMD symptoms.
Evaluation of the muscles of mastication
The muscles of mastication should be palpated bilaterally for firmness and tenderness, utilizing approximately 2–3 lbs of pressure,15 or the amount of pressure needed to cause blanching of the fingernail. Upon muscular palpation, the patient should be asked to report the severity of the tenderness, pain referral to multiple sites or single-site pain localization, and replication of the chief complaint upon palpation. It may be pertinent to ask the patient about their use of analgesics prior to palpation in order to account for reduced symptoms upon examination.
Management of TMD
Most of the time, patients will visit the clinician when pain and dysfunction, such as limitation of opening, episodes of joint locking (open lock/TMJ subluxation), pain with mandibular function (chewing), facial pain, or headache are present.
The treatment goals for TMD are decreasing pain, restoring normal ROM, and restoring normal masticatory and jaw function. Many TMDs can be cyclical and self-limiting, with periods of complete remission of symptoms.
In the case of disc-condyle incoordinations, studies suggest that for some patients even though they may be progressive (for example, a disc displacement with reduction may progress to a disc displacement without reduction), they are self limiting, suggesting an adaptation of the condition and with no significant disability.1,7,16,17 It is very important to emphasize that patients have no recurrence of symptoms with the use of conservative, reversible treatments,16,18 thus conservative treatment is the modality that needs to be used at all times. Initial treatment should therefore stress a conservative and reversible approach. Primary treatment options include home care (self-care program), medical care (non-surgical care), and surgical care.
Patient education: home care program
Home care should generally be the initial approach, at least as part of a more extensive treatment plan. The use of a home care program has proved to be effective in the management of TMD. It has been shown that patients have reported feeling less pain immediately after their initial patient education/counseling visit, perhaps as a consequence of an immediate reduction in stress/tension-related parafunctional activity.1,19 Patient education is a crucial aspect of home care and is one of the most subtle and underappreciated, yet effective, treatments for TMD. Therefore, informing and reassuring the patient regarding their condition and presenting symptoms may alleviate a great deal of anxiety and improve treatment outcomes.
A successful home care program consists of resting the masticatory muscles by limiting jaw movements, parafunctional habit modification, emphasizing a soft diet, and moist heat and/or ice therapy.20 Muscle rest may involve limited jaw activity (eg, reduced talking, chewing, yawning) for the treatment duration, and perhaps as a preventive measure, even after symptoms have resolved. Patients with disc displacement without reduction should be instructed to avoid any forceful attempt to open the mouth wider when the condition is acute and have explained to them that, with the care provided, the ROM will improve and return to normal.1 Restricting the mandibular movements as much as possible would facilitate healing and prevent further injury.20 This could be attained with a soft food diet, avoiding chewing gum and hard foods, and limitation of opening during yawning, as well as habit awareness, such as avoiding biting objects, clenching, or bruxing.1,3 Patients may have a diurnal (daytime) parafunctional habit (clenching, grinding, posturing) that is often not conscious, and this should be addressed to decrease sustained masticatory muscle contractions.21 Patient education and understanding of the physiological rest position (lips together, teeth apart) is imperative in reducing and eventually halting the daytime activity that contributes to the progression of TMD. If asked to pay attention to their jaw position over time, many patients will return for follow-up with the recognition that they are in fact engaging in some jaw activity that contributes to their symptoms. Additionally, suggesting habit-controlling cues may be helpful in reminding the patient throughout the day to check the position of their bite. As an example, saying the letter “N” throughout the day can remind the patient to unclench or discontinue grinding their teeth. A soft diet is also crucial for muscle and TMJ pain management so that the condition is not exacerbated while treatment is provided. Finally, a trial of moist heat and/or ice therapy overlying the painful areas of the face, head, and neck can be recommended. Moist heat tends to work better for muscle pain or tension by increasing circulation and relaxing involved muscles, and ice for TMJ capsulitis by reducing inflammatory symptoms.
Medical care (non-surgical)
Physical therapy
Instructing the patient to apply moist heat or cold compresses, or alternating both modalities, has been proven to be beneficial, since it stimulates analgesia and relaxation and may improve movement.12,22
Physical therapy is beneficial in restoring the normal function of the TMJ, muscles of mastication, and cervical muscles, as well as in reducing inflammation, promoting repair, and strength.22–24 Physical therapy can be performed by an experienced physical therapist3 or can be provided by a qualified clinician who is treating the TMJ disorder. Primary goals of the physical therapy component of treatment are to stretch chronically contracted and fatigued muscles, increase ROM, and reduce muscular trigger point activity.25 A number of exercises are commonly used to treat TMJ-associated muscle disorders, including N-stretch (placing the tip of the tongue on the roof of the mouth and stretching the jaw) (Figure 1); chin to chest (gently pulling the head forward, bringing the chin toward the chest); and head tilt (turning the head to one side and then tilting it posteriorly). These exercises must be done four to six times per day to be effective. In addition, the patient should use moist heat for 10–15 minutes followed by ethyl chloride spray prior to stretching the muscles. Vapocoolant spray provides a temporary anesthesia effect to the muscles so that a more intense stretch can be achieved without pain. The heat and cooling spray should be used for at least three of the six exercising sessions throughout the day. Patients can expect an even higher likelihood of treatment success if transcutaneous electrical nerve stimulation is added to a strict stretching regimen,26 and if biofeedback training is used as a cognitive behavioral procedure to teach the patient to maintain reduced muscular tension and pain.21,27
Figure 1.

Jaw N-stretch with vapocoolant spray.
Notes: The patient is instructed to place the tip of the tongue on the roof of the mouth just behind the frontal teeth (like saying the letter “N”) and to open – stretching the mandible while the spray is directed towards the face (masseter muscle region) in an upward motion.
Pharmacotherapy
Medications are an effective addition in managing the symptomatology of intracapsular disorders.1 Commonly used pharmacological agents for the treatment of TMJ disorders include analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), local anesthetics, oral and injectable corticosteroids, sodium hyaluronate injections, muscle relaxants, botulinum toxin injections, and antidepressants.12,28–30 The analgesics and corticosteroids are indicated for acute TMD pain; the NSAIDs, local anesthetics, and muscle relaxants are used for both acute and chronic conditions; and tricyclic antidepressants are usually used more for chronic TMD pain in association with tension-type headaches.28,31 Research demonstrating the efficacy of botulinum toxin for muscular disorders related to TMD is limited,32,33 although there is some data to support the benefit of using low concentrations and large injection volumes of botulinum toxin at multiple muscular sites.30
NSAIDs
NSAIDs are indicated for mild-to-moderate acute inflammatory conditions. Commonly used NSAIDs include ibuprofen and naproxen. NSAIDs should be used by the patient for a minimum of 2 weeks, with time-contingent usage as opposed to dosing based on the presence of pain.29 Long-term NSAID use is not recommended as long as the activity resulting in the inflammatory process can be reduced. In some chronic arthritic cases, the long-term use of NSAIDs, such as the COX-2 inhibitors, including celecoxib, may be considered; however, possible side effects, such as gastrointestinal upset, should be taken into account.
Local anesthetics
Local anesthetics are primarily used when a myofascial trigger point is present. Myofascial trigger points are usually detected in the mastication muscles, but can also be found in numerous other muscles, such as the splenius capitis and upper trapezius. Due to its low toxicity to muscles, 1% procaine (1 cc) is recommended, but 1% or 2% lidocaine is also commonly used.1,31 The trigger point injection technique involves locating the trigger point, which is usually found in a taut band of muscle, and needling the area.10 The patient should be instructed that the muscles may be sore for the first 48 hours after the injection, but should begin to improve thereafter. The efficacy of trigger point injections is highly variable and dependent, for the most part, on the patient’s compliance with a strict physical therapy regimen in conjunction with the injections. In addition, local anesthetics can be used to block the likely source of pain to confirm a diagnosis.
TMJ injections
Intracapsular injection of corticosteroids significantly reduces TMJ pain.34 It is indicated for acute and painful arthritic TMJ that has not responded to other modalities of treatment12 and when the joint is still acutely inflamed, such as in the case of polyarthritic disorders and in acute disc displacements without reduction.35–37 The use of triamcinolone or dexamethasone, in addition to 2% lidocaine without epinephrine, is generally used for TMJ injections (Figure 2). Tomograms of the TMJ or other radiographic studies are required prior to injecting into the joint space. It has been suggested in animal studies that steroid injections may increase osteoclastic activity.38 There is no evidence that a single steroid injection causes damage; however, multiple injections may do,39 therefore the quantity of steroid injections should be carefully considered due to the possibility of bone resorption in the site of injection.
Figure 2.

Temporomandibular joint injection.
Injections of sodium hyaluronate in osteoarthritis of the knee has shown improvement of symptoms;40 however, results for the management of TMD have been inconclusive and more studies are warranted.41,42
Muscle relaxants
Muscle relaxants may be prescribed for acute muscle tension associated with TMJ disorders.31 These are commonly taken at night before bed, due to possible associated drowsiness. Thus, for patients with poor sleep patterns, these drugs are particularly helpful in alleviating insomnia in addition to their muscle-pain preventive properties. A commonly used and effective muscle relaxant is cyclobenzaprine,43 started at lower dosages (5–10 mg) and taken 1–2 hours before bedtime.
Antidepressants
Tricyclic antidepressants like amitriptyline and nortriptyline may be used for more chronic MFP.21,31 In addition, they can be prescribed for the TMD patient who has tension-type headache (TTH), depression, poor sleep, and/or poor appetite. It is important to inform the patient that these medications are used in dosages that will not usually have anti-depressive effects when prescribed to treat muscle pain and/or headaches. Nortriptyline at usual doses of 10–30 mg and amitriptyline at doses of 10–25 mg should be gradually tapered up until the desired therapeutic effect is achieved or side effects develop, such as drowsiness, dry mouth, or weight gain. The tricyclic antidepressants have anti-nociceptive effects as well as maintaining the patient in deeper stages of sleep. Caution should be used in patients who have comorbid heart conditions, concurrent psychotropic use, and/or psychiatric illness, eg, bipolar disorder.44
Occlusal appliance therapy
Oral appliances (OAs) are processed acrylic devices that have been used for the management of TMD for years, with different designs. Studies have reported a reduction in TMD symptoms or at least sufficient evidence to justify their use for myalgia and arthralgia of the masticatory system.45–49 In an extensive review about the use of OAs and the management of TMD, it was concluded that OAs are still regarded as a useful adjunct therapy for some TMD cases.50
Stabilization appliances (flat plane splints) (Figure 3) are used for the purpose of equally distributing jaw parafunctional forces, reducing the forces placed on the masticatory muscles, and protecting the occlusal surfaces of the teeth from chronic nocturnal bruxing.51 For the case of nocturnal bruxism, OAs will protect the teeth from excessive tooth wear but may not stop parafunctional habits; they may, however, decrease the frequency, duration, and intensity of these habits.50,52,53 Usually, the patient is instructed to wear the splint only at night as long as parafunctional activity is controlled during the day with education and bite relation awareness, teaching the patient to be aware of when they are clenching their teeth during the day. The splint should cover all of the maxillary or mandibular teeth and have bilateral posterior contacts with little to no anterior contacts. The stabilization appliance should feel comfortable to the patient when fitted for the first time and be re-evaluated after 1 week. Adjustments should continue every 3–6 months due to changes that may result in the form and function of the splint due to chronic bruxing.
Figure 3.
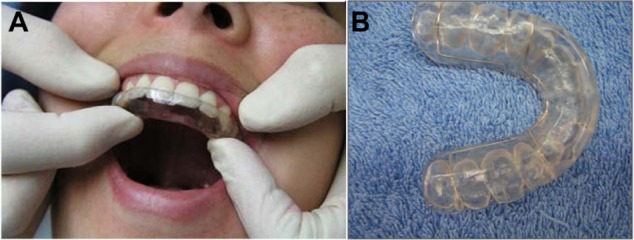
Maxillary stabilization splint.
Anterior repositioning splint prescription varies among clinicians, but it is usually used for the chronic intermittent closed-locking patient.51 With the possibility of permanent occlusal and bite changes with long-term use of repositioning appliances, short-term (6 weeks) use of this appliance is strongly recommended in addition to close monitoring. If bite changes start to develop, then the patient should be instructed to discontinue the use of the splint and the splint may need to be converted to a stabilization non-repositioning appliance. A few patients may experience increased pain with the use of a splint. In this case, the splint and the initial diagnosis should be re-evaluated and, if the pain persists, discontinuation of the splint is recommended.
In a systematic review and meta-analysis of randomized controlled trials, it was found that well-adjusted hard stabilization appliances are more effective in treating joint and muscle pain when compared with the use of no appliance, soft stabilization appliances, anterior bite appliances, and non-occluding appliances.50 Even though these OAs presented some evidence of reducing joint and muscle pains, the potential adverse events (eg, occlusal changes) were higher.49
Occlusal adjustment
There is not enough evidence to show that occlusal adjustments are useful in treating or preventing TMD.54 As a general rule, TMD should be treated in a conservative manner and occlusal adjustments are an irreversible modality.
Surgical care
TMJ surgery is only indicated when non-surgical therapy has been ineffective, and it is not indicated in patients who are asymptomatic or mildly symptomatic or as a preventive measure.55 Surgical recommendations, such as arthrocentesis and arthroscopy, depend on the degree of internal derangement as well as previous TMJ treatment history in addition to moderate-to-severe pain and disabling dysfunction.55 It is important to discourage patients from undergoing surgical procedures if physical medicine, pharmacological management, and splint therapy have not been attempted. Working closely with an oral and maxillofacial surgeon who has expertise in TMJ surgery is highly advisable in dealing with this particular group of patients.
Arthrocentesis is a conservative treatment that involves an intra-articular lavage with or without deposit of corticosteroids that is useful when there are intra-articular restrictions to movement, as in disc displacement without reduction.56 This procedure is often used with mandibular manipulation and is recommended for patients who have joint restrictions and for those individuals who have developed an acute or chronic closed lock.57
Arthroscopy is a closed surgical procedure that allows direct observation and sampling of joint tissue, useful in hypomobility due to joint derangement58 as well as fibrosis.59 It is performed mainly in the upper joint space and is utilized primarily for lysis and lavage but also for ablation of adhesions and biopsy.
Arthrotomy is an open surgical procedure that modifies joint anatomy, such as total or partial joint reconstruction or replacement, which is required for the patient who has advanced TMD that meets the surgical criteria and has been refractory to other modalities.12 It is used in cases of neoplasia, bony or fibrous ankylosis, severe chronic arthritis, and severe chronic dislocations.58 It is important to work closely with an experienced TMJ surgeon to assess the necessity of this procedure if other conservative treatments have not produced positive results.
Acupuncture and TMD
Acupuncture has been studied as a complementary and alternative medicine treatment modality for various orofacial pain disorders, mostly those of musculoskeletal origin. Acupuncture is a form of Traditional Chinese Medicine (TCM) that involves the stimulation of acupuncture points that are thought to stimulate the flow of energy believed to be blocked. It has been proposed that the reason why acupuncture research has not been as definitive about its benefits in pain treatment is because these studies often fail to include other treatments, such as herbal remedies and Qigong.60 A study that focused on TMD showed reductions in pain and, more importantly, a reduction in NSAID use in subjects who had been treated with traditional acupuncture.60 Further research compared TCM including acupuncture to specialty care that included self-care, patient education, occlusal splint therapy, physical therapy, and psychosocial counseling and found that the TCM arm had a significantly greater reduction in pain and psychosocially contributing factors.61 In addition, MFP, when teased apart from TMD, has been shown to benefit from acupuncture when compared to a sham acupuncture procedure.62 It is crucial to educate MFP patients about the difference between acupuncture and traditional trigger point injection therapy, as patients may confuse the two because of the similarity of the procedures. Acupuncture appears to be a beneficial treatment in conjunction with traditional therapies for TMD and perhaps as an alternative if pharmacological treatment is contraindicated.
Neuropathic pain
Basic and clinical research support that neuroplastic changes involving the peripheral and central nervous system as well as immune mechanisms are involved in the development and maintenance of chronic neuropathic pain.63 It has been estimated that the incidence of chronic orofacial neuropathic pain is five to ten per 100,000 people.64–66 Commonly, neuropathic pain conditions in the orofacial region are divided into episodic pain disorders, including trigeminal neuralgia (TN) and glossopharyngeal neuralgia, and continuous pain disorders that frequently result from deafferentation after injury in the peripheral and central nervous system, which is the case in neuromas and idiopathic trigeminal neuropathic pains such as atypical odontalgia (AO). There is considerable variability in prevalence, cause, and treatment of these disorders. More detailed reviews on neuropathic pains classification, etiology, and pathophysiology can be found elsewhere.12,67,68
There are still limited data in regard to the treatment of trigeminal neuropathic pain. Its management is based on the evidence associated with pain management in other parts of the body. Good reference guides are those by Dworkin et al69 and Zakrzewska.70
The use of anticonvulsant medications has shown to be effective in the management of trigeminal neuropathic pain, and they are the first-line treatment choice for the management of neuralgic type of pains.70–72 Tricyclic antidepressants and serotonin noradrenaline reuptake inhibitors, as well as topical medications such as capsaicin and lidocaine,70,73 are used for the more continuous type of pain, such as in the case of idiopathic trigeminal neuropathic pain, for example, in AO.74,75
Trigeminal neuralgia
TN is a chronic paroxysmal neuropathic pain condition that is described as a severe, lancinating, and electric-like unilateral pain. It is localized most often to the second and third distributions of the trigeminal nerve (V2 and V3) intraorally and extraorally and can present in both distributions at the same time. There is usually a trigger zone in the trigeminal distribution which, when stimulated, can result in an excruciatingly painful attack. The pain attacks last seconds to minutes and numerous pain episodes can be present daily. TN commonly goes through periods of remission where the pain can remit for months or even longer.12,66,76
The etiology of TN is often related to vascular compression77 that may result in focal demyelination.78 The superior cerebellar artery compression on the trigeminal root has been shown to be responsible for attacks of TN pain;79 however, nonvascular compression by a cerebellopontine angle neoplasm, such as acoustic neuromas, meningiomas, cholesteatomas, and neurofibromas, have also been shown to result in TN attacks.80,81 A cranial nerve exam can demonstrate other neural deficits that may be present due to a mass pressing on the trigeminal root. Therefore, magnetic resonance imaging (MRI) and computed tomography (CT) imaging of the brain should be requested in order to rule out any intracranial pathology.76 Furthermore, myelin loss due to multiple sclerosis has been shown to be a causative disorder related to the paroxysmal pain firing of TN attacks.82
Antiepileptic medications are the drugs of choice for the management of TN. Carbamazepine, oxcarbazepine, and gabapentin are commonly used as first-line medications.66,70 Carbamazepine, evaluated in a systematic review, has been shown to be the most effective treatment.71 If these medications are not effective, or if the therapeutic range cannot be achieved due to side effects, then doses should be lowered and second-line drugs, such as baclofen83 and lamotrigine,84 may be added to reduce the pain attacks. It is best to reduce the pain attacks completely with multiple medications if necessary. After achieving pain-free status and monitoring for pain attacks for a minimum of 3–6 months, a slow taper off of medication will demonstrate if the TN has gone into remission. If pain attacks recur, then pharmacologic management should immediately be reinstituted. If medications are no longer effective or if unmanageable side effects develop, then neurosurgical options, such as microvascular decompression or gamma knife radiosurgery, may be considered.85
Glossopharyngeal neuralgia
Glossopharyngeal neuralgia is a rare condition associated with pain in the area supplied by the glossopharyngeal nerve.86 Painful sites may include the nasopharynx, posterior part of the tongue, throat, tonsil, larynx, and ear. This disorder presents shooting paroxysms of pain that can occur multiple times a day with stimulation of the oropharyngeal region.87 Common triggers may include mechanical stimulation of the trigger zone as well as activities including chewing, swallowing, coughing, talking, and head movement. The painful episodes may continue for months and then spontaneously go into remission. Due to the proximity of the vagal sensory nerves, glossopharyngeal neuralgia may coincide with a cardiac dysrhythmia such as bradycardia, asystole, and syncope.88 Diagnosis may be confirmed by blocking the tonsillar and pharyngeal region with topical or local anesthetics. Imaging with a CT scan of the head and a brain MRI should be conducted to rule out pathology related to the nerve compression and possible oropharyngeal carcinoma. Pharmacologic treatment of glossopharyngeal neuralgia is similar to that for TN and may include the use of antiepileptic medications.89 If medication management fails, then surgical procedures may be considered, such as a microvascular decompression to remove pressure from the glossopharyngeal nerve, radiofrequency thermocoagulation, gamma knife radiosurgery, or rhizotomy.86,90
Peripheral trigeminal neuropathic pain
Peripheral neuropathic pain can arise as a result of a traumatic nerve injury resulting in chronic aching, continuous burning-like pain at the site of the injury.91 When a nerve injury occurs, the transected nerve will sometimes attempt to restore itself through axonal sprouting, resulting in a traumatic neuroma.92,93 Diagnosis can be made through tapping (Tinel’s sign) or lightly pressing on the suspected site of the neuroma. In addition, allodynia and hyperalgesia will often be present in the area of the nerve injury or adjacent to it.91 It is recommended to perform a diagnostic block of the painful site with topical anesthetic first (eg, benzocaine) followed by a somatic block with local anesthetic (eg, lidocaine injection).91 If either of these blocks reduce or alleviate the pain, then topical creams or ointments may be utilized to treat the pain. The use of topical medications for the management of neuropathic pain is a good modality that reduces potential side effects of the systemic route.73 Capsaicin is a common locally acting pharmacologic agent that can be utilized in cream or gel form, normally at a concentration ranging from 0.025%–0.05%95 mixed with benzocaine 20% and applied with the use of a stent that covers the affected area (neurosensory stent). Recently, 8% capsaicin has been approved in the US and Europe for application directly into the skin, and has proved to be effective in alleviating pain.95 In addition, compounding pharmacies can create a cream that may include analgesics/sedatives such as ketamine, NSAIDs such as diclofenac, anticonvulsant drugs such as gabapentin and carbamazepine, and tricyclic antidepressant medications such as nortriptyline and amitriptyline.73,96
Centralized trigeminal neuropathic pain
Prolonged stimulation of peripheral nociceptors may eventually lead to central neural changes.63,97 The pain in these cases is described as continuous, aching, and burning, with evidence of hyperalgesia and allodynia.98 Diagnostic local anesthetic blocking of the affected site usually does not alleviate the pain in centralized neuropathic pain, thus treatment is conducted with centrally acting systemic medications. Antiepileptic drugs, such as gabapentin and valproic acid, in combination with tricyclic antidepressants such as amitriptyline, may reduce pain,70 but often treatment of this condition is difficult.
Atypical odontalgia
AO is a centralized trigeminal neuropathy often localized in a tooth or tooth area that is frequently misdiagnosed, leading to unnecessary dental treatments in attempts to relieve the pain.75 AO is described as a persistent idiopathic pain that does not fulfill the diagnostic criteria for cranial neuralgias and which is not attributed to another disorder,99 and can be throbbing and burning in nature.12 The pharmacological management of AO may include topical and systemic medications. If the pain is localized to a peripheral origin and the diagnostic block gives an equivocal response but a decrease in pain, a topical medication can be used and a neurosensory stent can be fabricated. Systemic approaches, such as tricyclic antidepressants, calcium channel blockers (pregabalin and gabapentin), sodium channel blockers (carbamazepine), and antiepileptics such as topiramate, can be used for the management of this condition.69,74 The management of AO is very challenging, and a multidisciplinary approach is necessary, which should include orofacial pain specialists and neurologists in addition to psychiatric and psychological evaluations in order to identify comorbidities with depression and anxiety.74
Headache
Another source of nonodontogenic toothaches and orofacial pains may present as a disturbance of the trigeminovascular system. Migraine is commonly thought of as a headache that is unilateral and that causes pain behind the eye, neck, and cranium; however, migraine headaches can also present in the lower part of the face, particularly in the teeth.98–100 It is very important that the orofacial pain clinician is aware of the possibility of this localization in addition to the clinical features that a migraine presents to avoid misdiagnosis as an odontogenic toothache or other type of orofacial pain, leading to improper management.
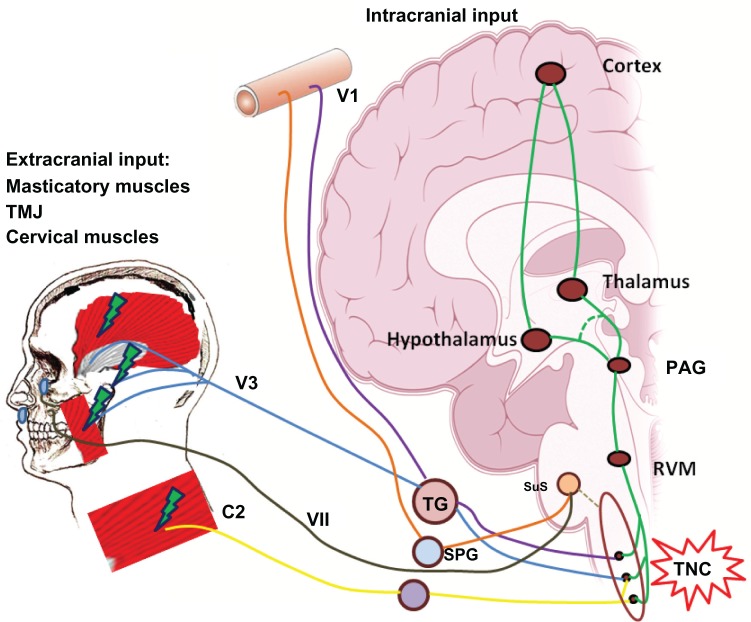
Primary headaches, such as migraine and TTH, are also disorders mediated by the trigeminal system that can be chronic and disabling, affecting over 15% of the US population at any one time and costing the US economy over $19.6 billion a year.102 Migraine is a primary disorder of the brain explained as a neurovascular disorder in which neural events result in meningeal blood vessel dilation, which results in further nociceptive activation of the trigeminovascular system.103 The pathophysiology of migraine is still not completely understood, but it is known that key anatomical peripheral and central structures are involved. The trigeminovascular system consists of the dura mater that surrounds the meninges and spinal cord, the dural meningeal blood vessels (cranial vasculature), and the innervations of these structures provided by the ophthalmic branch (V1) of the trigeminal nerve and its afferent connection to the trigeminal nucleus caudalis (TNC) in the central nervous system, in addition to a reflex connection from the trigeminal nucleus to the parasympathetic outflow to the cranial vasculature through the superior salivatory nucleus.103,104
The nociceptive (pain) information of these structures convey information to the TNC, brainstem, and higher processing centers.103 The TNC also receives cervical inputs. Stimulation of the dura mater extends to the C2 and C3 regions, and is collectively described as the trigeminocervical complex (TCC). This anatomical relationship may explain why a migraine headache can sometimes be felt in the neck area.105–107
Primary headaches, particularly migraine, are believed to involve activation and sensitization of the trigeminovascular system, specifically the afferent meningeal nociceptor projections to the ophthalmic division of the trigeminal nerve,108 and this is thought to cause the release of vasoactive neuropeptides such as substance P (SP), neurokinin A (NKA), and calcitonin gene-related peptide (CGRP), which is elevated during a chronic migraine attack.109 What drives the trigeminovascular activation is still not clear, but it has been hypothesized that a dysfunction within nuclei of the brainstem and diencephalon may contribute to activation of this system, thereby relaying nociceptive information to other central structures.103 Trigeminal nerve release of CGRP is known to aid in the process of neurogenic inflammation, facilitating pain transmission leading to allodynia and hyperalgesia.110–112 These nociceptive mediators will induce edema, mast cell activation, and further sensitization of the trigeminovascular system.113
Facial migraine
In the new International Classification of Headache Disorders 3rd edition (ICHD-3 beta version) in the comments to section 1.1 (“Migraine without aura”) facial migraine is mentioned as a subset of patients who present with the typical migraine headache, but localized in the face and not as a subtype.99 Facial migraine may follow the diagnostic criteria of migraine without aura (ICHD-3 1.1), which is described as a recurrent headache of moderate-to-severe intensity that lasts from 4–72 hours, with a pulsating quality, which is unilateral in location, aggravated by routine physical activity, and associated with nausea and/or phonophobia and photophobia.99
The ophthalmic division of the trigeminal nerve innervates most of the cranial structures: this could explain the reason why most migraine sufferers feel pain in the periorbital region and behind their eye. In facial migraine, however, the pain is localized in the lower part of the face. Migraine localized in the area of the maxillary branch distribution (V2) has been reported.101,114,115 V2 gives rise to the nervus meningeus medius, which innervates the dura mater of the anterior floor of the middle fossa, and this may explain the localization of the pain in the maxillary area. Migraine symptomatology localized on the V3 territory has also been reported,101,114,115 and this could be explained since it is well recognized that stimulation of the dura mater in animals during electrophysiological experiments, and in humans during neurosurgery, induces pain in any of the three divisions of the trigeminal nerve.101,116 More detailed reviews on migraine pathophysiology can be found elsewhere.103,117
Management
The management of migraine comprises pharmacological and nonpharmacological approaches. It is imperative that the treatment approach of migraine always includes a complete medical evaluation performed by the neurologist to rule out a secondary cause of the headache, such as systemic disease, tumors, or cerebrovascular abnormalities.
Nonpharmacological approaches
Patients need to be educated about the pain they are experiencing. When the pain is localized in the lower half of the face and/or in a tooth/teeth area (facial migraine), the patient should be assured that, even though the experienced pain may be severe and throbbing, it is not a toothache or related dental problem. This is extremely important since it will prevent unnecessary dental procedures due to misdiagnosis as odontogenic toothache or other orofacial pain.
Facial migraine is the same migraine headache described in the ICDH-3 (beta version) but with a different localization, therefore requiring that the same management protocol be followed. It is recommended to have the patient identify any trigger factors that may start the migraine attack. A good method by which the patient can provide this information is with the use of a pain diary, in which the patient keeps a record of the characteristics of the headache episodes along with the circumstances that made them appear. As soon as the patient can identify the possible triggers, then they are instructed to avoid or address them by, for example, a change in diet, sleep hygiene, or stress management. This is a great opportunity for the patient to realize that lifestyle changes may greatly influence their headaches and subsequently feel more in control of the disorder.
Other nonpharmacological methods that have proved useful for migraine and TTH are biofeedback, relaxation techniques, hypnosis, and psychological therapies.118,119
Pharmacological approaches
As described above, the TNC is a crucial anatomical relay center for conveying sensory information, predominantly nociceptive, coming from the orofacial region, the head and its cranial vasculature, to higher pain processing centers in the brain; in addition, it gives and receives projections from the superior salivatory nucleus and structures from the descending inhibitory system, such as the ventrolateral periaqueductal gray and rostral ventromedial medulla.103 These anatomical connections have positioned the TNC as a therapeutical target to potentially decrease or inhibit trigeminovascular nociceptive activation and further sensitization.120
The same medications used for the management of migraine are used for the management of facial migraine, since it is the same disorder and same pathophysiology but different headache localization (face). If the migraine attack occurs less than twice per month, then an abortive medication should be considered. If the migraine attack is more frequent, it is best managed with preventive medications.
Abortive medications
Abortive medications are the first line of treatment for the acute treatment of migraine. The use of NSAIDs, such as naproxen sodium and ibuprofen, has been shown to be probably effective in alleviating a headache attack;121 however, patients taking NSAIDs on a daily or regular basis are at risk of exacerbating their existent headache and developing medication overuse headaches.99
Ergotamine derivatives, such as dihydroergotamine (DHE), have been used for years for the treatment of moderate to severe migraine;122 however, triptans, because of their better tolerability and pharmacological specificity, have replaced ergotamine derivatives in the majority of cases.123 DHE is a 5-HT1B and 5-HT1D agonist,124 as well as acting at other receptors, and is useful in patients who have not responded to triptan therapy.122 DHE is available in intranasal125 and injectable preparations, the latter in particular being popularly used as an abortive agent in the emergency room.126
Serotonin 5-HT1B/1D receptor agonists (triptans), such as sumatriptan, are newer established medications for the acute treatment of migraine.127,128 Studies have shown that they affect neuronal activation, inhibiting the presynaptic release of CGRP at the TCC, and also act in the ventrolateral periaqueductal gray and the thalamus.103,129 5-HT1B/1D receptors are localized on the trigeminal ganglion in humans and rodents130–132 and at the level of the TNC in humans.133–135 5-HT1B receptors are localized on human intracranial arteries.133 Sumatriptan has been shown to prevent central sensitization of TCC neurons, but not abort central sensitization.136,137 This may explain why triptans are effective when they are taken at the first sign of a migraine.
In addition to oral dosing formulations, subcutaneous and intranasal formulations offer a fast onset of action and are a good alternative for patients who experience gastrointestinal effects. The different pharmacokinetics between triptans should be considered when choosing the appropriate one for a patient.
New combination preparations, such as sumatriptan with naproxen sodium, have shown additive effects in improving pain relief and migraine-associated symptoms, such as phonophobia, photophobia, and nausea, when compared with monotherapy, as well as good tolerability in the acute management of migraine.138,139
Triptans can induce cardiovascular and cerebrovascular effects because of their vasoconstrictor properties, therefore they are contraindicated in patients with disorders in these systems.140 However, new medications in development such as CGRP receptor antagonists, including oral telcagepant, have shown to be a good migraine abortive without the vascular effects.141 Evidence has shown that the 5-HT1F receptor is another promising new target in the treatment of migraine: lasmiditan, a 5-HT1F receptor agonist, has shown good clinical efficacy for acute migraine treatment in doubleblind placebo controlled trials.142,143
Preventives
Patients who have frequent migraine attacks, such as 15 headache days per month, can benefit from preventive therapy.99 The mechanism of action of the current preventive medications is not, however, well understood. Medications that have proven beneficial are beta adrenergic blockers such as propranolol and atenolol; calcium channel blockers such as verapamil and flunarizine; tricyclic antidepressants such as amitriptyline; serotonin antagonists such as methysergide; and antiepileptics such as topiramate and valproate.144
Newer treatment strategies have been shown to be promising. The use of botulinum toxin injections for migraine prophylaxis and the management of chronic migraine and TTH have been shown to be effective and well tolerated.145–148 In addition, neuromodulative procedures, such as occipital nerve stimulation approaches, have been shown to be effective in the management of refractory headaches such as chronic migraine and cluster headache in which pain-free periods (weeks) can be accomplished.149,150 More comprehensive reviews of preventive options for migraine can be found elsewhere.44,151
Tension type headache
TTH is the most common primary headache disorder in the general population.152 Its pathophysiology remains unclear, but peripheral and central mechanisms are likely to be involved. A model has been proposed in which interaction between the limbic system, the descending inhibitory system, and peripheral inputs, such as those coming from the intracranial vasculature and myofascial inputs, may result in TTH.153
The patient may describe the headache as a tight headband compressing their head with a dull, non-pulsating quality. The headache is bilateral with a mild-to-moderate intensity and will not worsen with routine physical activity. It can present as episodic attacks, but can evolve to a more chronic state.99 Sometimes the headache can be associated with pericranial tenderness. Muscles that are tender to palpation include the temporalis muscle and cervical muscles, such as the splenius, sternocleidomastoid, and upper trapezius muscles.99,154,155 Headache associated with myofascial trigger points can meet the criteria for episodic and chronic TTH.156,157 This is very important to note during examination, since treatment should be oriented to address the MFP condition. The use of physical therapy and trigger point injection therapy is useful.1
The management of TTH involves nonpharmacological and pharmacological approaches, as observed for migraine. Changes in lifestyle such as sleep hygiene, detection of triggers with a pain diary, as well as stress management and relaxation techniques, have been shown to be beneficial.118,158 Pharmacological approaches, such as the use of NSAIDs as well as tricyclic antidepressants in addition to botulinum toxin injections, have proved useful.145,146,159,160
Headache and TMD
It is known that headache and orofacial pain disorders, such as TMD, are highly prevalent conditions in the general population.161,162 Evidence suggests that a clinical comorbidity between primary headaches and TMD exists.163,164 Epidemiological studies have shown that TMD symptomatology is more common in patients with primary headaches such as migraine, episodic TTH, and chronic daily headache,163,164 where the prevalence of primary headache, particularly migraine, was increased in patients with TMD.165 In addition, patients with headache and orofacial pain disorders of musculoskeletal origin also present a higher disability impact.163 It can be hypothesized that extracranial trigeminal nociceptive inputs arising from the craniofacial structures as a result of a TMD may influence the activation of the trigeminovascular system, since these nociceptive inputs convey in TNC where intracranial inputs do. Existing TMD may, therefore, influence and/or exacerbate a headache disorder, and a headache disorder may exacerbate a TMD condition (Figure 4). It is very important, therefore, that, during treatment, such comorbidity is addressed. A relationship between the orofacial pain specialist and the neurologist (headache specialist) must be established, as management should be focused on addressing both, the headache and the TMD condition, since they considerably increase the prevalence of each other.163,164
Figure 4.
Relationship between temporomandibular disorders and headache.
Notes: Extracranial nociceptive inputs arising from craniofacial structures as a result of a temporomandibular disorder, as well as cervical input from the cervical muscles, may influence the activation of the trigeminovascular system. The commonality is that these nociceptive inputs converge on the TNC in the same way as do intracranial nociceptive inputs arising from the dural blood vessels and higher centers.
Abbreviations: C2, C2 region of the cervical spinal cord; PAG, ventrolateral periaqueductal gray; RVM, rostral ventromedial medulla; SPG, sphenopalatine ganglion; SuS, superior salivatory nucleus; TG, trigeminal ganglion; TMJ, temporomandibular joint; TNC, trigeminal nucleus caudalis; VII, facial nerve; VI, ophthalmic branch of the trigeminal nerve; V3, mandibular branch of the trigeminal nerve.
Trigeminal autonomic cephalalgias (TACs)
Cluster headache, paroxysmal hemicranias, and short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing are severe headaches that are not as common as migraine and that are characterized for their notorious parasympathetic autonomic symptoms.99,166 The typical localization of these headaches are the orbital, temporal or supraorbital regions but they can be present in the orofacial region such as in the mandible, TMJ, and dental areas. These headaches require neurological evaluation and management; therefore, it is of fundamental importance to make an appropriate differential diagnosis to avoid unnecessary dental treatments or being misdiagnosed as other types of orofacial pains of non neurovascular etiology. Detailed reviews of trigeminal autonomic cephalalgias and their treatment can be found elsewhere.166–168
Conclusion
Orofacial pain management can be challenging and the clinician should be aware of the different etiologies and characteristics of the diverse disorders of the orofacial region. The orofacial pain specialist has the experience and the knowledge to provide a correct diagnosis and management of these conditions. A multidisciplinary approach is ideal in the management of orofacial pain disorders.
Understanding the pain neurobiology of the trigeminal system is key to the development of better and safer therapeutics. It is necessary to stress the need for randomized controlled clinical trials that evaluate the efficacy of current and new therapies for the management of orofacial pains. New and exciting discoveries from the bench to the bedside will hopefully put an end to the burden of chronic orofacial pain conditions in the near future.
Acknowledgments
We thank Dr Simon Akerman for reviewing the draft of this manuscript.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Okeson JP. Bell’s Orofacial Pains. The Clinical Management of Orofacial Pain. 6th ed. Carol Stream, IL: Quintessence Publishing Co, Inc; 2005. [Google Scholar]
- 2.Okeson JP. The Classification of Orofacial Pains. Oral Maxillofac Surg Clin North Am. 2008;20(2):133–144. doi: 10.1016/j.coms.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 3.McNeill C. Temporomandibular Disorders: Guidelines for Classification, Assesment, and Management. 2nd ed. Chicago, IL: Quintessence Publishing Co, Inc; 1993. [Google Scholar]
- 4.Dworkin SF. Temporomandibular disorder (TMD) pain-related disability found related to depression, nonspecific physical symptoms, and pain duration at 3 international sites. J Evid Based Dent Pract. 2011;11(3):143–144. doi: 10.1016/j.jebdp.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Dworkin SF, Huggins KH, LeResche L, et al. Epidemiology of signs and symptoms in temporomandibular disorders: clinical signs in cases and controls. J Am Dent Assoc. 1990;120(3):273–281. doi: 10.14219/jada.archive.1990.0043. [DOI] [PubMed] [Google Scholar]
- 6.Solberg W, Woo M, Houston J. Prevalence of mandibular dysfunction in young adults. J Am Dent Assoc. 1979;98(1):25–34. doi: 10.14219/jada.archive.1979.0008. [DOI] [PubMed] [Google Scholar]
- 7.Rasmussen OC. Description of population and progress of symptoms in a longitudinal study of temporomandibular arthropathy. Scand J Dent Res. 1981;89(2):196–203. doi: 10.1111/j.1600-0722.1981.tb01671.x. [DOI] [PubMed] [Google Scholar]
- 8.Könönen M, Waltimo A, Nyström M. Does clicking in adolescence lead to painful temporomandibular joint locking? Lancet. 1996;347(9008):1080–1081. doi: 10.1016/s0140-6736(96)90280-9. [DOI] [PubMed] [Google Scholar]
- 9.Guarda-Nardini L, Piccotti F, Mogno G, Favero L, Manfredini D. Age-related differences in temporomandibular disorder diagnoses. Cranio. 2012;30(2):103–109. doi: 10.1179/crn.2012.015. [DOI] [PubMed] [Google Scholar]
- 10.Simons DG, Travel JG, Simons LS. Myofascial Pain and Dysfunction: The Trigger Point Manual. Upper Half of Body. 2nd ed. Atlanta, GA: Lippincott Williams & Wilkins; 1998. p. 1. [Google Scholar]
- 11.Sanitá PV, de Alencar Júnior FGP. Myofascial pain syndrome as a contributing factor in patients with chronic headaches. J Musculoskelet Pain. 2009;17(1):15–25. [Google Scholar]
- 12.de Leeuw R. Temporomandibular Disorders. In: de Leeuw R, editor. Orofacial Pain Guidelines for Assesment, Diagnosis and Management. 4th ed. Hanover Park, IL: Quintessence Publishing Co, Inc; 2008. pp. 158–176. (The American Academy of Orofacial Pain). [Google Scholar]
- 13.Clark GT, Seligman DA, Solberg WK, Pullinger AC. Guidelines for the examination and diagnosis of temporomandibular disorders. J Craniomandib Disord. 1989;3(1):7–14. [PubMed] [Google Scholar]
- 14.Bezuur JN, Habets LL, Jimenez Lopez V, Naeije M, Hansson TL. The recognition of craniomandibular disorders – a comparison between clinical and radiographic findings in eighty-nine subjects. J Oral Rehabil. 1988;15(3):215–221. doi: 10.1111/j.1365-2842.1988.tb00151.x. [DOI] [PubMed] [Google Scholar]
- 15.Ohrbach R, Gale EN. Pressure pain thresholds, clinical assessment, and differential diagnosis: reliability and validity in patients with myogenic pain. Pain. 1989;39(2):157–169. doi: 10.1016/0304-3959(89)90003-1. [DOI] [PubMed] [Google Scholar]
- 16.Mejersjö C, Carlsson GE. Long-term results of treatment for temporomandibular joint pain-dysfunction. J Prosthet Dent. 1983;49(6):809–815. doi: 10.1016/0022-3913(83)90355-4. [DOI] [PubMed] [Google Scholar]
- 17.Nickerson JW, Boering G. Natural course of osteoarthrosis as it relates to internal derangement of the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 1989;1:27–45. [Google Scholar]
- 18.Mejersjö C, Carlsson GE. Analysis of factors influencing the long-term effect of treatment of TMJ-pain dysfunction. J Oral Rehabil. 1984;11(3):289–297. doi: 10.1111/j.1365-2842.1984.tb00579.x. [DOI] [PubMed] [Google Scholar]
- 19.Riley JL, 3rd, Myers CD, Currie TP, et al. Self-care behaviors associated with myofascial temporomandibular disorder pain. J Orofac Pain. 2007;21(3):194–202. [PubMed] [Google Scholar]
- 20.Randolph CS, Greene CS, Moretti R, Forbes D, Perry HT. Conservative management of temporomandibular disorders: a posttreatment comparison between patients from a university clinic and from private practice. Am J Orthod Dentofacial Orthop. 1990;98(1):77–82. doi: 10.1016/0889-5406(90)70035-B. [DOI] [PubMed] [Google Scholar]
- 21.Graff-Radford SB. Myofascial pain: diagnosis and management. Curr Pain Headache Rep. 2004;8(6):463–467. doi: 10.1007/s11916-004-0068-y. [DOI] [PubMed] [Google Scholar]
- 22.Danzig WN, Van Dyke AR. Physical therapy as an adjunct to temporomandibular joint therapy. J Prosthet Dent. 1983;49(1):96–99. doi: 10.1016/0022-3913(83)90247-0. [DOI] [PubMed] [Google Scholar]
- 23.Kirk WS, Jr, Calabrese DK. Clinical evaluation of physical therapy in the management of internal derangement of the temporomandibular joint. J Oral Maxillofac Surg. 1989;47(2):113–119. doi: 10.1016/s0278-2391(89)80099-0. [DOI] [PubMed] [Google Scholar]
- 24.Clark GT, Adachi NY, Dornan MR. Physical medicine procedures affect temporomandibular disorders: a review. J Am Dent Assoc. 1990;121(1):151–162. doi: 10.14219/jada.archive.1990.0140. [DOI] [PubMed] [Google Scholar]
- 25.Carlson CR, Okeson JP, Falace DA, Nitz AJ, Anderson D. Stretch-based relaxation and the reduction of EMG activity among masticatory muscle pain patients. J Craniomandib Disord. 1991;5(3):205–212. [PubMed] [Google Scholar]
- 26.Rodrigues D, Siriani AO, Bérzin F. Effect of conventional TENS on pain and electromyographic activity of masticatory muscles in TMD patients. Braz Oral Res. 2004;18(4):290–295. doi: 10.1590/s1806-83242004000400003. [DOI] [PubMed] [Google Scholar]
- 27.Reeves JL. EMG-biofeedback reduction of tension headache: a cognitive skills-training approach. Biofeedback Self Regul. 1976;1(2):217–225. doi: 10.1007/BF00998588. [DOI] [PubMed] [Google Scholar]
- 28.Gangarosa L, Mahan PE. Pharmacologic management of TMD-MPDS. Ear Nose Throat J. 1982;61:670–678. [Google Scholar]
- 29.Gregg JM, Rugh JD. Pharmacological therapy. In: Mohl NDZ, George A, Carlsson, Gunnar E, Rugh, John D, editors. A Textbook of Occlusion. Chicago, IL: Quintessence; 1983. pp. 351–375. [Google Scholar]
- 30.Song PC, Schwartz J, Blitzer A. The emerging role of botulinum toxin in the treatment of temporomandibular disorders. Oral Dis. 2007;13(3):253–260. doi: 10.1111/j.1601-0825.2007.01352.x. [DOI] [PubMed] [Google Scholar]
- 31.Graff-Radford SB. Regional myofascial pain syndrome and headache: principles of diagnosis and management. Curr Pain Headache Rep. 2001;5(4):376–381. doi: 10.1007/s11916-001-0028-8. [DOI] [PubMed] [Google Scholar]
- 32.Ernberg M, Hedenberg-Magnusson B, List T, Svensson P. Efficacy of botulinum toxin type A for treatment of persistent myofascial TMD pain: a randomized, controlled, double-blind multicenter study. Pain. 2011;152(9):1988–1996. doi: 10.1016/j.pain.2011.03.036. [DOI] [PubMed] [Google Scholar]
- 33.Guarda-Nardini L, Stecco A, Stecco C, Masiero S, Manfredini D. Myofascial pain of the jaw muscles: comparison of short-term effectiveness of botulinum toxin injections and fascial manipulation technique. Cranio. 2012;30(2):95–102. doi: 10.1179/crn.2012.014. [DOI] [PubMed] [Google Scholar]
- 34.Wenneberg B, Kopp S, Gröndahl HG. Long-term effect of intra-articular injections of a glucocorticosteroid into the TMJ: a clinical and radiographic 8-year follow-up. J Craniomandib Disord. 1991;5(1):11–18. [PubMed] [Google Scholar]
- 35.Kopp S, Akerman S, Nilner M. Short-term effects of intra-articular sodium hyaluronate, glucocorticoid, and saline injections on rheumatoid arthritis of the temporomandibular joint. J Craniomandib Disord. 1991;5(4):231–238. [PubMed] [Google Scholar]
- 36.Samiee A, Sabzerou D, Edalatpajouh F, Clark GT, Ram S. Temporomandibular joint injection with corticosteroid and local anesthetic for limited mouth opening. J Oral Sci. 2011;53(3):321–325. doi: 10.2334/josnusd.53.321. [DOI] [PubMed] [Google Scholar]
- 37.Stoll ML, Good J, Sharpe T, et al. Intra-articular corticosteroid injections to the temporomandibular joints are safe and appear to be effective therapy in children with juvenile idiopathic arthritis. J Oral Maxillofac Surg. 2012;70(8):1802–1807. doi: 10.1016/j.joms.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 38.El-Hakim IE, Abdel-Hamid IS, Bader A. Tempromandibular joint (TMJ) response to intra-articular dexamethasone injection following mechanical arthropathy: a histological study in rats. Nt J Oral Maxillofac Surg. 2005;34(3):305–310. doi: 10.1016/j.ijom.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 39.Toller PA. Use and misuse of intra-articular corticosteroids in treatment of temporomandibular joint pain. Proc R Soc Med. 1977;70(7):461–463. doi: 10.1177/003591577707000704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Divine JG, Zazulak BT, Hewett TE. Viscosupplementation for knee osteoarthritis: a systematic review. Clin Orthop Relat Res. 2007;455:113–122. doi: 10.1097/BLO.0b013e31802f5421. [DOI] [PubMed] [Google Scholar]
- 41.Li XD, Shi ZD, Tian WD. An outcome analysis of two methods of intra-capsular injection of sodium hyaluronate for temporomandibular disorders. Hua Xi Kou Qiang Yi Xue Za Zhi. 2004;22(2):135–137. Chinese. [PubMed] [Google Scholar]
- 42.Manfredini D, Piccotti F, Guarda-Nardini L. Hyaluronic acid in the treatment of TMJ disorders: a systematic review of the literature. Cranio. 2010;28(3):166–176. doi: 10.1179/crn.2010.023. [DOI] [PubMed] [Google Scholar]
- 43.Herman CR, Schiffman EL, Look JO, Rindal DB. The effectiveness of adding pharmacologic treatment with clonazepam or cyclobenzaprine to patient education and self-care for the treatment of jaw pain upon awakening: a randomized clinical trial. J Orofac Pain. 2002;16(1):64–70. [PubMed] [Google Scholar]
- 44.Silberstein SD. Preventive migraine treatment. Neurol Clin. 2009;27(2):429–443. doi: 10.1016/j.ncl.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 45.Clark GT. A critical evaluation of orthopedic interocclusal appliance therapy: effectiveness for specific symptoms. J Am Dent Assoc. 1984;108(3):364–368. doi: 10.14219/jada.archive.1984.0002. [DOI] [PubMed] [Google Scholar]
- 46.Clark GT. A critical evaluation of orthopedic interocclusal appliance therapy: design, theory, and overall effectiveness. J Am Dent Assoc. 1984;108(3):359–364. doi: 10.14219/jada.archive.1984.0010. [DOI] [PubMed] [Google Scholar]
- 47.Tsuga K, Akagawa Y, Sakaguchi R, Tsuru H. A short-term evaluation of the effectiveness of stabilization-type occlusal splint therapy for specific symptoms of temporomandibular joint dysfunction syndrome. J Prosthet Dent. 1989;61(5):610–613. doi: 10.1016/0022-3913(89)90286-2. [DOI] [PubMed] [Google Scholar]
- 48.Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances. Evidence of their efficacy. J Am Dent Assoc. 2001;132(6):770–777. doi: 10.14219/jada.archive.2001.0274. [DOI] [PubMed] [Google Scholar]
- 49.Fricton J, Look JO, Wright E, et al. Systematic review and meta-analysis of randomized controlled trials evaluating intraoral orthopedic appliances for temporomandibular disorders. J Orofac Pain. 2010;24(3):237–254. [PubMed] [Google Scholar]
- 50.Klasser GD, Greene CS. Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(2):212–223. doi: 10.1016/j.tripleo.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 51.Fricton J. Myogenous temporomandibular disorders: diagnostic and management considerations. Dent Clin North Am. 2007;51(1):61–83. doi: 10.1016/j.cden.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 52.Clark GT, Beemsterboer PL, Solberg WK, Rugh JD. Nocturnal electromyographic evaluation of myofascial pain dysfunction in patients undergoing occlusal splint therapy. J Am Dent Assoc. 1979;99(4):607–611. doi: 10.14219/jada.archive.1979.0348. [DOI] [PubMed] [Google Scholar]
- 53.Dube C, Rompre PH, Manzini C, Guitard F, de Grandmont P, Lavigne GJ. Quantitative polygraphic controlled study on efficacy and safety of oral splint devices in tooth-grinding subjects. J Dent Res. 2004;83(5):398–403. doi: 10.1177/154405910408300509. [DOI] [PubMed] [Google Scholar]
- 54.Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular joint disorders. Cochrane Database Syst Rev. 2003;(1):CD003812. doi: 10.1002/14651858.CD003812. [DOI] [PubMed] [Google Scholar]
- 55.Parameters of care for oral and maxillofacial surgery. A guide for practice, monitoring and evaluation (AAOMS Parameters of Care-92). American Association of Oral and Maxillofacial Surgeons. J Oral Maxillofac Surg. 1992;50(7 Suppl 2):i–xvi. 1–174. [No authors listed] [PubMed] [Google Scholar]
- 56.Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49(11):1163–1167. doi: 10.1016/0278-2391(91)90409-f. discussion 1168–1170. [DOI] [PubMed] [Google Scholar]
- 57.Dimitroulis G, Dolwick MF, Martinez A. Temporomandibular joint arthrocentesis and lavage for the treatment of closed lock: a follow-up study. Br J Oral Maxillofac Surg. 1995;33(1):23–27. doi: 10.1016/0266-4356(95)90081-0. [DOI] [PubMed] [Google Scholar]
- 58.Buckley MJ, Merrill RG, Braun TW. Surgical management of internal derangement of the temporomandibular joint. J Oral Maxillofac Surg. 1993;51(1 Suppl 1):20–27. doi: 10.1016/0278-2391(93)90006-y. [DOI] [PubMed] [Google Scholar]
- 59.Blaustein D, Heffez L. Diagnostic arthroscopy of the temporomandibular joint. Part II. Arthroscopic findings of arthrographically diagnosed disk displacements. Oral Surg Oral Med Oral Pathol. 1988;65(2):135–141. doi: 10.1016/0030-4220(88)90153-3. [DOI] [PubMed] [Google Scholar]
- 60.Elder C, Ritenbaugh C, Aickin M, et al. Reductions in pain medication use associated with traditional Chinese medicine for chronic pain. Perm J. 2012;16(3):18–23. doi: 10.7812/tpp/12.967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ritenbaugh C, Hammerschlag R, Calabrese C, et al. A pilot whole systems clinical trial of traditional Chinese medicine and naturopathic medicine for the treatment of temporomandibular disorders. J Altern Complement Med. 2008;14(5):475–487. doi: 10.1089/acm.2007.0738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shen YF, Younger J, Goddard G, Mackey S. Randomized clinical trial of acupuncture for myofascial pain of the jaw muscles. J Orofac Pain. 2009;23(4):353–359. [PMC free article] [PubMed] [Google Scholar]
- 63.Romero-Reyes M, Graff-Radford S. Is there hope for chronic pain and headache? Headache. 2007;47(8):1262–1271. doi: 10.1111/j.1526-4610.2007.00909.x. [DOI] [PubMed] [Google Scholar]
- 64.Lipton JA, Ship JA, Larach-Robinson D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc. 1993;124(10):115–121. doi: 10.14219/jada.archive.1993.0200. [DOI] [PubMed] [Google Scholar]
- 65.Marbach JJ. Medically unexplained chronic orofacial pain. Temporomandibular pain and dysfunction syndrome, orofacial phantom pain, burning mouth syndrome, and trigeminal neuralgia. Med Clin North Am. 1999;83(3):691–710. doi: 10.1016/s0025-7125(05)70130-9. [DOI] [PubMed] [Google Scholar]
- 66.Kitt CA, Gruber K, Davis M, Woolf CJ, Levine JD. Trigeminal neuralgia: opportunities for research and treatment. Pain. 2000;85(1):3–7. doi: 10.1016/s0304-3959(99)00310-3. [DOI] [PubMed] [Google Scholar]
- 67.Sarlani E, Balciunas BA, Grace EG. Orofacial pain – Part I: assessment and management of musculoskeletal and neuropathic causes. AACN Clin Issues. 2005;16(3):333–346. doi: 10.1097/00044067-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 68.Sarlani E, Balciunas BA, Grace EG. Orofacial Pain – Part II: assessment and management of vascular, neurovascular, idiopathic, secondary, and psychogenic causes. AACN Clin Issues. 2005;16(3):347–358. doi: 10.1097/00044067-200507000-00008. [DOI] [PubMed] [Google Scholar]
- 69.Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85(Suppl 3):S3–S14. doi: 10.4065/mcp.2009.0649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zakrzewska JM. Medical management of trigeminal neuropathic pains. Expert Opin Pharmacother. 2010;11(8):1239–1254. doi: 10.1517/14656561003767449. [DOI] [PubMed] [Google Scholar]
- 71.Reisner L, Pettengill CA. The use of anticonvulsants in orofacial pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91(1):2–7. doi: 10.1067/moe.2001.111189. [DOI] [PubMed] [Google Scholar]
- 72.Martin WJ, Forouzanfar T. The efficacy of anticonvulsants on orofacial pain: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(5):627–633. doi: 10.1016/j.tripleo.2011.01.033. [DOI] [PubMed] [Google Scholar]
- 73.Bramwell BL. Bs Pharm Rph. Topical orofacial medications for neuropathic pain. Int J Pharm Compd. 2010;14(3):200–203. [PubMed] [Google Scholar]
- 74.Baad-Hansen L. Atypical odontalgia – pathophysiology and clinical management. J Oral Rehabil. 2008;35(1):1–11. doi: 10.1111/j.1365-2842.2007.01813.x. [DOI] [PubMed] [Google Scholar]
- 75.Patel SB, Boros AL, Kumar SK. Atypical odontalgia – an update. J Calif Dent Assoc. 2012;40(9):739–747. [PubMed] [Google Scholar]
- 76.Merrill RL, Graff-Radford SB. Trigeminal neuralgia: how to rule out the wrong treatment. J Am Dent Assoc. 1992;123(2):63–68. doi: 10.14219/jada.archive.1992.0047. [DOI] [PubMed] [Google Scholar]
- 77.Lutz J, Linn J, Mehrkens JH, et al. Trigeminal neuralgia due to neurovascular compression: high-spatial-resolution diffusiontensor imaging reveals microstructural neural changes. Radiology. 2011;258(2):524–530. doi: 10.1148/radiol.10100477. [DOI] [PubMed] [Google Scholar]
- 78.Jannetta PJ. Arterial compression of the trigeminal nerve at the pons in patients with trigeminal neuralgia. J Neurosurg. 1967;26(1:Suppl):159–162. doi: 10.3171/jns.1967.26.1part2.0159. [DOI] [PubMed] [Google Scholar]
- 79.Bakshi R, Lerner A, Fritz JV, Sambuchi GD. Vascular compression in trigeminal neuralgia shown by magnetic resonance imaging and magnetic resonance angiography image registration. Arch Neurol. 2001;58(8):1290–1291. doi: 10.1001/archneur.58.8.1290. [DOI] [PubMed] [Google Scholar]
- 80.Matsuka Y, Fort ET, Merrill RL. Trigeminal neuralgia due to an acoustic neuroma in the cerebellopontine angle. J Orofac Pain. 2000;14(2):147–151. [PubMed] [Google Scholar]
- 81.Feinerman DM, Goldberg MH. Acoustic neuroma appearing as trigeminal neuralgia. J Am Dent Assoc. 1994;125(8):1122–1125. doi: 10.14219/jada.archive.1994.0124. [DOI] [PubMed] [Google Scholar]
- 82.Jensen TS, Rasmussen P, Reske-Nielsen E. Association of trigeminal neuralgia with multiple sclerosis: clinical and pathological features. Acta Neurol Scand. 1982;65(3):182–189. doi: 10.1111/j.1600-0404.1982.tb03076.x. [DOI] [PubMed] [Google Scholar]
- 83.Fromm GH, Terrence CF, Chattha AS. Baclofen in the treatment of trigeminal neuralgia: Double-blind study and long-term follow-up. Ann Neurol. 1984;15(3):240–244. doi: 10.1002/ana.410150306. [DOI] [PubMed] [Google Scholar]
- 84.Zakrzewska JM, Chaudhry Z, Nurmikko TJ, Patton DW, Mullens EL. Lamotrigine (lamictal) in refractory trigeminal neuralgia: results from a double-blind placebo controlled crossover trial. Pain. 1997;73(2):223–230. doi: 10.1016/S0304-3959(97)00104-8. [DOI] [PubMed] [Google Scholar]
- 85.Obermann M. Treatment options in trigeminal neuralgia. Ther Adv Neurol Disord. 2010;3(2):107–115. doi: 10.1177/1756285609359317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Singh PM, Kaur M, Trikha A. An uncommonly common: glossopharyngeal neuralgia. Ann Indian Acad Neurol. 2013;16(1):1–8. doi: 10.4103/0972-2327.107662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986;3:S1–S226. [No authors listed] [PubMed] [Google Scholar]
- 88.Marks PV, Purchas SH. Life-threatening glossopharyngeal neuralgia. Aust N Z J Surg. 1992;62(8):660–661. [PubMed] [Google Scholar]
- 89.Katusic S, Williams DB, Beard CM, Bergstralh EJ, Kurland LT. Epidemiology and clinical features of idiopathic trigeminal neuralgia and glossopharyngeal neuralgia: similarities and differences, Rochester, Minnesota, 1945–1984. Neuroepidemiology. 1991;10(5–6):276–281. doi: 10.1159/000110284. [DOI] [PubMed] [Google Scholar]
- 90.Olds MJ, Woods CI, Winfield JA. Microvascular decompression in glossopharyngeal neuralgia. Am J Otol. 1995;16(3):326–330. [PubMed] [Google Scholar]
- 91.Merrill RL. Head and neck pain. Seminars in Anesthesia, Perioperative Medicine, and Pain. 1997;16(4):280–291. [Google Scholar]
- 92.Mathews GJOJ. Painful traumatic neuroma. Surg Clin North Am. 1972;52(5):1313–1324. doi: 10.1016/s0039-6109(16)39843-7. [DOI] [PubMed] [Google Scholar]
- 93.Lee EJ, Calcaterra TC, Zuckerbraun L. Traumatic neuromas of the head and neck. Ear Nose Throat J. 1998;77(8):670–674. [PubMed] [Google Scholar]
- 94.Derry S, Sven-Rice A, Cole P, Tan T, Moore RA. Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2013;2:CD007393. doi: 10.1002/14651858.CD007393.pub3. [DOI] [PubMed] [Google Scholar]
- 95.Anand P, Bley K. Topical capsaicin for pain management: therapeutic potential and mechanisms of action of the new high-concentration capsaicin 8% patch. Br J Anaesth. 2011;107(4):490–502. doi: 10.1093/bja/aer260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.H D, Wellish M, Gilden D. Topical ketamine treatment of postherpetic neuralgia. Neurology. 2003;60(8):1391. doi: 10.1212/01.wnl.0000055848.00032.39. [DOI] [PubMed] [Google Scholar]
- 97.Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10(9):895. doi: 10.1016/j.jpain.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Merrill RL. Orofacial pain mechanisms and their clinical application. Dent Clin North Am. 1997;41(2):167–188. [PubMed] [Google Scholar]
- 99.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders. Cephalalgia. (3rd ed) 2013;33(9):629–808. doi: 10.1177/0333102413485658. beta version. [DOI] [PubMed] [Google Scholar]
- 100.Peñarrocha M, Bandrés A, Peñarrocha M, Bagán JV. Lower-half facial migraine: a report of 11 cases. J Oral Maxillofac Surg. 2004;62(12):1453–1456. doi: 10.1016/j.joms.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 101.Daudia AT, Jones NS. Facial migraine in a rhinological setting. Clin Otolaryngol Allied Sci. 2002;27(6):521–525. doi: 10.1046/j.1365-2273.2002.00628.x. [DOI] [PubMed] [Google Scholar]
- 102.Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: results from the American Productivity Audit. J Occup Environ Med. 2003;45(12):1234–1246. doi: 10.1097/01.jom.0000099999.27348.78. [DOI] [PubMed] [Google Scholar]
- 103.Akerman S, Holland PR, Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci. 2011;12(10):570–584. doi: 10.1038/nrn3057. [DOI] [PubMed] [Google Scholar]
- 104.May A, Goadsby PJ. The trigeminovascular system in humans: pathophysiologic implications for primary headache syndromes of the neural influences on the cerebral circulation. J Cereb Blood Flow Metab. 1999;19(2):115–127. doi: 10.1097/00004647-199902000-00001. [DOI] [PubMed] [Google Scholar]
- 105.McNaughton FL, Feindel W. Innervation of intracranial structures: a reappraisal. In: Rose FC, editor. Physiological aspects of clinical neurology. Oxford: Blackwell Scientific; 1977. pp. 279–293. [Google Scholar]
- 106.Andreou AP, Summ O, Charbit AR, Romero-Reyes M, Goadsby PJ. Animal models of headache: from bedside to bench and back to bedside. Expert Rev Neurother. 2010;10(3):389–411. doi: 10.1586/ern.10.16. [DOI] [PubMed] [Google Scholar]
- 107.Bartsch T, Goadsby PJ. The trigeminocervical complex and migraine: current concepts and synthesis. Curr Pain Headache Rep. 2003;7(5):371–376. doi: 10.1007/s11916-003-0036-y. [DOI] [PubMed] [Google Scholar]
- 108.Goadsby PJ, Lipton RB, Ferrari MD. Migraine – current understanding and treatment. N Engl J Med. 2002;346(4):257–270. doi: 10.1056/NEJMra010917. [DOI] [PubMed] [Google Scholar]
- 109.Goadsby PJ, Edvinsson L, Ekman R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann Neurol. 1990;28(2):183–187. doi: 10.1002/ana.410280213. [DOI] [PubMed] [Google Scholar]
- 110.Goadsby PJ. Migraine, allodynia, sensitisation and all of that …. Eur Neurol. 2005;53(Suppl 1):10–16. doi: 10.1159/000085060. [DOI] [PubMed] [Google Scholar]
- 111.Burstein R, Levy D, Jakubowski M. Effects of sensitization of trigeminovascular neurons to triptan therapy during migraine. Rev Neurol (Paris) 2005;161(6–7):658–660. doi: 10.1016/s0035-3787(05)85109-4. [DOI] [PubMed] [Google Scholar]
- 112.Durham PL. Calcitonin gene-related peptide (CGRP) and migraine. Headache. 2006;46(Suppl 1):S3–S8. doi: 10.1111/j.1526-4610.2006.00483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Oshinsky ML. Insights from experimental studies into allodynia and its treatment. Curr Pain Headache Rep. 2006;10(3):225–230. doi: 10.1007/s11916-006-0050-y. [DOI] [PubMed] [Google Scholar]
- 114.Obermann M, Mueller D, Yoon MS, Pageler L, Diener H, Katsarava Z. Migraine with isolated facial pain: a diagnostic challenge. Cephalalgia. 2007;27(11):1278–1282. doi: 10.1111/j.1468-2982.2007.01413.x. [DOI] [PubMed] [Google Scholar]
- 115.Silberstein SD, Lipton RB, Dalessio DJ, editors. Wolff’s Headache And Other Head Pain. 7th ed. New York: Oxford University Press; 2001. pp. 478–479. [Google Scholar]
- 116.Benoliel R, Elishoov H, Sharav Y. Orofacial pain with vascular-type features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(5):506–512. doi: 10.1016/s1079-2104(97)90267-5. [DOI] [PubMed] [Google Scholar]
- 117.Bernstein C, Burstein R. Sensitization of the trigeminovascular pathway: perspective and implications to migraine pathophysiology. J Clin Neurol. 2012;8(2):89–99. doi: 10.3988/jcn.2012.8.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nicholson R, Buse DC, Andrasik F, Lipton RB. Nonpharmacologic treatments for migraine and tension-type headache: how to choose and when to use. Curr Treat Options Neurol. 2011;13(1):28–40. doi: 10.1007/s11940-010-0102-9. [DOI] [PubMed] [Google Scholar]
- 119.Pistoia F, Sacco S, Carolei A. Behavioral therapy for chronic migraine. Curr Pain Headache Rep. 2012;17(1):1–8. doi: 10.1007/s11916-012-0304-9. [DOI] [PubMed] [Google Scholar]
- 120.Akerman S, Romero-Reyes M. Insights into the pharmacological targeting of the trigeminocervical complex in the context of treatments of migraine. Expert Rev Neurother. 2013;13(9):1041–1059. doi: 10.1586/14737175.2013.827472. [DOI] [PubMed] [Google Scholar]
- 121.Holland S, Silberstein SD, Freitag F, Dodick DW, Argoff C, Ashman E, Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78(17):1346–1353. doi: 10.1212/WNL.0b013e3182535d0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Silberstein S, Kori S. Dihydroergotamine: a review of formulation approaches for the acute treatment of migraine. CNS Drugs. 2013;27(5):385–394. doi: 10.1007/s40263-013-0061-2. [DOI] [PubMed] [Google Scholar]
- 123.Sprenger T, Goadsby P. Migraine pathogenesis and state of pharmacological treatment options. BMC Med. 2009;7:71. doi: 10.1186/1741-7015-7-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Buzzi MG, Moskowitz MA. Evidence for 5-HT1B/1D receptors mediating the antimigraine effect of sumatriptan and dihydroergotamine. Cephalalgia. 1991;11(4):165–168. doi: 10.1046/j.1468-2982.1991.1104165.x. [DOI] [PubMed] [Google Scholar]
- 125.Rapoport A, Winner P. Nasal delivery of antimigraine drugs: clinical rationale and evidence base. Headache. 2006;46:S192–S201. doi: 10.1111/j.1526-4610.2006.00603.x. [DOI] [PubMed] [Google Scholar]
- 126.Carleton SC, Shesser RF, Pietrzak MP, et al. Double-blind, multicenter trial to compare the efficacy of intramuscular dihydroergotamine plus hydroxyzine versus intramuscular meperidine plus hydroxyzine for the emergency department treatment of acute migraine headache. Ann Emerg Med. 1998;32(2):129–138. doi: 10.1016/s0196-0644(98)70126-x. [DOI] [PubMed] [Google Scholar]
- 127.Treatment of migraine attacks with sumatriptan. The Subcutaneous Sumatriptan International Study Group. N Engl J Med. 1991;325(5):316–321. doi: 10.1056/NEJM199108013250504. [No authors listed] [DOI] [PubMed] [Google Scholar]
- 128.Humphrey PP, Feniuk W. Mode of action of the anti-migraine drug sumatriptan. Trends Pharmacol Sci. 1991;12(12):444–446. doi: 10.1016/0165-6147(91)90630-b. [DOI] [PubMed] [Google Scholar]
- 129.Shields KG, Goadsby PJ. Serotonin receptors modulate trigeminovascular responses in ventroposteromedial nucleus of thalamus: a migraine target? Neurobiol Dis. 2006;23(3):491–501. doi: 10.1016/j.nbd.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 130.Ma QP. Co-localization of 5-HT(1B/1D/1F) receptors and glutamate in trigeminal ganglia in rats. Neuroreport. 2001;12(8):1589–1591. doi: 10.1097/00001756-200106130-00015. [DOI] [PubMed] [Google Scholar]
- 131.Ma QP, Hill R, Sirinathsinghji D. Colocalization of CGRP with 5-HT1B/1D receptors and substance P in trigeminal ganglion neurons in rats. Eur J Neurosci. 2001;13(11):2099–2104. doi: 10.1046/j.0953-816x.2001.01586.x. [DOI] [PubMed] [Google Scholar]
- 132.Smith D, Shaw D, Hopkins R, et al. Development and characterisation of human 5-HT1B- or 5-HT1D-receptor specific antibodies as unique research tools. J Neurosci Methods. 1998;80(2):155–161. doi: 10.1016/s0165-0270(97)00209-4. [DOI] [PubMed] [Google Scholar]
- 133.Longmore J, Shaw D, Smith D, et al. Differential distribution of 5HT1D- and 5HT1B-immunoreactivity within the human trigemino-cerebrovascular system: implications for the discovery of new anti-migraine drugs. Cephalalgia. 1997;17(8):833–842. doi: 10.1046/j.1468-2982.1997.1708833.x. [DOI] [PubMed] [Google Scholar]
- 134.Smith D, Hill RG, Edvinsson L, Longmore J. An immunocytochemical investigation of human trigeminal nucleus caudalis: CGRP, substance P and 5-HT1D-receptor immunoreactivities are expressed by trigeminal sensory fibres. Cephalalgia. 2002;22(6):424–431. doi: 10.1046/j.1468-2982.2002.00378.x. [DOI] [PubMed] [Google Scholar]
- 135.Castro ME, Pascual J, Romón T, del Arco C, del Olmo E, Pazos A. Differential distribution of [3H]sumatriptan binding sites (5-HT1B, 5-HT1D and 5-HT1F receptors) in human brain: focus on brainstem and spinal cord. Neuropharmacology. 1997;36(4–5):535–542. doi: 10.1016/s0028-3908(97)00061-0. [DOI] [PubMed] [Google Scholar]
- 136.Levy D, Jakubowski M, Burstein R. Disruption of communication between peripheral and central trigeminovascular neurons mediates the antimigraine action of 5HT 1B/1D receptor agonists. Proc Natl Acad Sci U S A. 2004;101(12):4274–4279. doi: 10.1073/pnas.0306147101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Burstein R, Jakubowski M. Analgesic triptan action in an animal model of intracranial pain: a race against the development of central sensitization. Ann Neurol. 2004;55(1):27–36. doi: 10.1002/ana.10785. [DOI] [PubMed] [Google Scholar]
- 138.Smith TR, Sunshine A, Stark SR, Littlefield DE, Spruill SE, Alexander WJ. Sumatriptan and naproxen sodium for the acute treatment of migraine. Headache. 2005;45(8):983–991. doi: 10.1111/j.1526-4610.2005.05178.x. [DOI] [PubMed] [Google Scholar]
- 139.Mathew NT, Landy S, Stark S, et al. Fixed-dose sumatriptan and naproxen in poor responders to triptans with a short half-life. Headache. 2009;49(7):971–982. doi: 10.1111/j.1526-4610.2009.01458.x. [DOI] [PubMed] [Google Scholar]
- 140.Dodick D, Lipton RB, Martin V, et al. Triptan Cardiovascular Safety Expert Panel Consensus statement: cardiovascular safety profile of triptans (5-HT agonists) in the acute treatment of migraine. Headache. 2004;44(5):414–425. doi: 10.1111/j.1526-4610.2004.04078.x. [DOI] [PubMed] [Google Scholar]
- 141.Ho T, Ferrari M, Dodick D, et al. Efficacy and tolerability of MK-0974 (telcagepant), a new oral antagonist of calcitonin gene-related peptide receptor, compared with zolmitriptan for acute migraine: a randomised, placebo-controlled, parallel-treatment trial. Lancet. 2008;372:2115–2123. doi: 10.1016/S0140-6736(08)61626-8. [DOI] [PubMed] [Google Scholar]
- 142.Färkkilä M, Diener HC, Géraud G, et al. Efficacy and tolerability of lasmiditan, an oral 5-HT(1F) receptor agonist, for the acute treatment of migraine: a phase 2 randomised, placebo-controlled, parallel-group, dose-ranging study. Lancet Neurol. 2012;11(5):405–413. doi: 10.1016/S1474-4422(12)70047-9. [DOI] [PubMed] [Google Scholar]
- 143.Ferrari MD, Färkkilä M, Reuter U, et al. European COL-144 Investigators Acute treatment of migraine with the selective 5-HT1F receptor agonist lasmiditan – a randomised proof-of-concept trial. Cephalalgia. 2010;30(10):1170–1178. doi: 10.1177/0333102410375512. [DOI] [PubMed] [Google Scholar]
- 144.Lance JW, Goadsby PJ. Mechanism and Management of Headache. 7th ed. Philadelphia, PA: Elsevier Butterworth Heinemann; 2005. [Google Scholar]
- 145.Gady J, Ferneini EM. Botulinum toxin A and headache treatment. Conn Med. 2013;77(3):165–166. [PubMed] [Google Scholar]
- 146.Mathew NT, Frishberg BM, Gawel M, Dimitrova R, Gibson J, Turkel C, BOTOX CDH Study Group Botulinum toxin type A (BOTOX) for the prophylactic treatment of chronic daily headache: a randomized, double-blind, placebo-controlled trial. Headache. 2005;45(4):293–307. doi: 10.1111/j.1526-4610.2005.05066.x. [DOI] [PubMed] [Google Scholar]
- 147.Aurora SK, Gawel M, Brandes JL, Pokta S, Vandenburgh AM, BOTOX North American Episodic Migraine Study Group Botulinum toxin type a prophylactic treatment of episodic migraine: a randomized, double-blind, placebo-controlled exploratory study. Headache. 2007;47(4):486–499. doi: 10.1111/j.1526-4610.2006.00624.x. [DOI] [PubMed] [Google Scholar]
- 148.Dodick DW, Turkel CC, DeGryse RE, et al. PREEMPT Chronic Migraine Study Group Onabotulinumtoxin A for treatment of chronic migraine: pooled results from the double-blind, randomized, placebo-controlled phases of the PREEMPT clinical program. Headache. 2010;50(6):921–936. doi: 10.1111/j.1526-4610.2010.01678.x. [DOI] [PubMed] [Google Scholar]
- 149.Mueller O, Diener HC, Dammann P, et al. Occipital nerve stimulation for intractable chronic cluster headache or migraine: a critical analysis of direct treatment costs and complications. Cephalalgia. 2013 Jun 28; doi: 10.1177/0333102413493193. Epub. [DOI] [PubMed] [Google Scholar]
- 150.Silberstein SD, Dodick DW, Saper J, et al. Safety and efficacy of peripheral nerve stimulation of the occipital nerves for the management of chronic migraine: results from a randomized, multicenter, double-blinded, controlled study. Cephalalgia. 2012;32(16):1165–1179. doi: 10.1177/0333102412462642. [DOI] [PubMed] [Google Scholar]
- 151.Schurks M, Diener HC, Goadsby P. Update on the prophylaxis of migraine. Curr Treat Options Neurol. 2008;10(1):20–29. doi: 10.1007/s11940-008-0003-3. [DOI] [PubMed] [Google Scholar]
- 152.Rasmussen BK. Migraine and tension-type headache in a general population: precipitating factors, female hormones, sleep pattern and relation to lifestyle. Pain. 1993;53(1):65–72. doi: 10.1016/0304-3959(93)90057-V. [DOI] [PubMed] [Google Scholar]
- 153.Olesen J. Clinical and pathophysiological observations in migraine and tension-type headache explained by integration of vascular, supraspinal and myofascial inputs. Pain. 1991;46(2):125–132. doi: 10.1016/0304-3959(91)90066-7. [DOI] [PubMed] [Google Scholar]
- 154.Jensen R, Rasmussen BK, Pedersen B, Olesen J. Muscle tenderness and pressure pain thresholds in headache. A population study. Pain. 1993;52(2):193–199. doi: 10.1016/0304-3959(93)90131-8. [DOI] [PubMed] [Google Scholar]
- 155.Bendtsen L, Fernández-de-la-Peñas C. The role of muscles in tensiontype headache. Curr Pain Headache Rep. 2011;15(6):451–458. doi: 10.1007/s11916-011-0216-0. [DOI] [PubMed] [Google Scholar]
- 156.Fernández-de-Las-Peñas C, Alonso-Blanco C, Cuadrado ML, Pareja JA. Myofascial trigger points in the suboccipital muscles in episodic tension-type headache. Man Ther. 2006;11(3):225–230. doi: 10.1016/j.math.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 157.Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, Gerwin RD, Pareja JA. Myofascial trigger points and their relationship to headache clinical parameters in chronic tension-type headache. Headache. 2006;46(8):1264–1272. doi: 10.1111/j.1526-4610.2006.00440.x. [DOI] [PubMed] [Google Scholar]
- 158.Kaniecki RG. Tension-type headache. Continuum (Minneap Minn) 2012;18(4):823–834. doi: 10.1212/01.CON.0000418645.32032.32. [DOI] [PubMed] [Google Scholar]
- 159.Bendtsen L, Jensen R. Treating tension-type headache – an expert opinion. Expert Opin Pharmacother. 2011;12(7):1099–1109. doi: 10.1517/14656566.2011.548806. [DOI] [PubMed] [Google Scholar]
- 160.Bendtsen L, Evers S, Linde M, Mitsikostas DD, Sandrini G, Schoenen J; EFNS. EFNS guideline on the treatment of tension-type headache – report of an EFNS task force. Eur J Neurol. 2010;17(11):1318–1325. doi: 10.1111/j.1468-1331.2010.03070.x. [DOI] [PubMed] [Google Scholar]
- 161.Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–349. doi: 10.1212/01.wnl.0000252808.97649.21. [DOI] [PubMed] [Google Scholar]
- 162.LeResche L. Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. 1997;8(3):291–305. doi: 10.1177/10454411970080030401. [DOI] [PubMed] [Google Scholar]
- 163.Mitrirattanakul S, Merrill RL. Headache impact in patients with orofacial pain. J Am Dent Assoc. 2006;137(9):1267–1274. doi: 10.14219/jada.archive.2006.0385. [DOI] [PubMed] [Google Scholar]
- 164.Gonçalves DA, Bigal ME, Jales LC, Camparis CM, Speciali JG. Headache and symptoms of temporomandibular disorder: an epidemiological study. Headache. 2010;50(2):231–241. doi: 10.1111/j.1526-4610.2009.01511.x. [DOI] [PubMed] [Google Scholar]
- 165.Franco AL, Gonçalves DA, Castanharo SM, Speciali JG, Bigal ME, Camparis CM. Migraine is the most prevalent primary headache in individuals with temporomandibular disorders. J Orofac Pain. 2010;24(3):287–292. [PubMed] [Google Scholar]
- 166.Goadsby PJ, Cohen AS, Matharu MS. Trigeminal autonomic cephalalgias: diagnosis and treatment. Curr Neurol Neurosci Rep. 2007;7(2):117–125. doi: 10.1007/s11910-007-0006-6. [DOI] [PubMed] [Google Scholar]
- 167.Leone M, Bussone G. Pathophysiology of trigeminal autonomic cephalalgias. Lancet Neurol. 2009;8(8):755–764. doi: 10.1016/S1474-4422(09)70133-4. [DOI] [PubMed] [Google Scholar]
- 168.May A. Update on the diagnosis and management of trigemino-autonomic headaches. J Neurol. 2006;253(12):1525–1532. doi: 10.1007/s00415-006-0303-2. [DOI] [PubMed] [Google Scholar]