Abstract
Zygomycosis is an acute or chronic infection caused by several fungal agents belonging to the phylum Zygomycota. These are saprophytic fungi and are found ubiquitously in the environment. These are emerging highly opportunistic pathogenic organisms. Basidiobolus ranarum (B. haptosporus, B. meristoporus) is a fungus belonging to the order Entomophthorales under the family Zygomycota. Basidiobolomycosis is a predominantly subcutaneous infection involving the trunk and limbs in immunocompetent hosts. We hereby report a case of Basidiobolomycosis from the Department of Microbiology, Siddhartha Medical College, Vijayawada in a 6 month old child who presented to us with a painless swelling over her left knee following an insect bite.
Keywords: Basidiobolus ranarum, subcutaneous nodules, zygomycosis
INTRODUCTION
The class Zygomycetes includes two fungal orders: Mucorales and Entomophthorales, with extremely different pathogenic potentials. Mucorales affect only the immunocompromised patient causing mortality in excess of 60% in those affected, while entomophthorales, which include Basidiobolus and Conidiobolus genera, affect the immune competent individual, causing principally chronic infection of the subcutaneous tissue.[1]
The fungus Basidiobolus ranarum is present in soil, decaying vegetable matter, and the intestines of amphibians, reptiles, fish and insectivorous bats.[2]
The Zygomycetes represent relatively uncommon isolates in the clinical laboratory, reflecting either environmental contaminants or, less commonly, a clinical disease called zygomycosis.[3] Human disease with these organisms occurs predominantly in tropical regions. The disease is endemic in India and is more so concentrated in South India. Transmission occurs by implantation of spores via minor trauma such as insect bites or by inhalation of spores.[4] The organism may also be transmitted from soil and vegetation that is contaminated with animal feces. Iatrogenic infection has also been reported. They generally do not invade blood vessels and rarely disseminate. Occasional cases of disseminated and angioinvasive disease have recently been described, primarily in immunocompromised patients, suggesting a possible emerging role for this organism as an opportunist.
B. ranarum was described from animal and environmental sources as early as 1886. The first human case was reported in 1956 in a patient from Indonesia. Although, the organism is found world-wide, there are estimated to have been only a few 100 cases of infection. Basidiobolus infections have historically been limited to tropical and subtropical areas, occurring as a chronic subcutaneous mycosis of the trunk and extremities in immunocompetent hosts, primarily children and young adults.[5]
B. ranarum spends part of its life -cycle in the intestine of the agamid lizard and is liberated as spores and mycelia in the lizard excrement. The spores germinate, and the organism grows saprophytically on lizard droppings, from which it may be picked up by individuals with traumatic lesions. In addition to being isolated from insects and reptiles, Basidiobolus has been isolated from several mammalian species.
Here, we describe to you a case of basidiobolomycosis, which presented with a subcutaneous swelling over the knee in a 6 month-old infant.
CASE REPORT
A 6 month-old female child presented with the chief complaints of multiple painless swellings over her left knee for the past 4 months, which was insidious in onset and gradually progressive. The present illness was preceded by an insect bite 4 months ago following which she developed erythematous nodules, which have gradually progressed with ulceration. It was associated with low -grade fever for the first 10 days following the insect bite. Physical Examination revealed multiple nodules over the extensor aspect of left thigh and a single well- defined erythematous indurated non- tender nodule of size 3 cm × 4 cm with central ulceration with eschar formation present over the left knee. The swelling was firm in consistency with smooth and rounded edges. It was freely mobile over the underlying structure [Figures 1 and 2]. Bilateral inguinal lymphadenopathy was noted.
Figure 1.

Subcutaneous nodule over the left knee
Figure 2.

Satellite nodules
Routine investigations were carried out; complete blood picture-Haemoglobin -13.7 g%, Total leucocyte count -9,900 cell\cu.mm, Differential Count –Neutrophils -55%, Lymphocytes- 40%, Eosinophils - 4%, Monocytes - 1%, and Platelets-1.76 lakhs/cu.mm. Complete urine examination - urine was clear with 2-3 pus cells, 3-4 epithelial cells with no albumin and sugar. Human immuno-deficiency virus 1 and 2- non- reactive; and Liver Function Test -normal; X-ray left thigh– showed soft- tissue swelling. Microbiological investigations: On direct examination of the tissue specimen with 10% KOH showed fungal elements with broad aseptate hyphae. Growth on Sabourauds Dextrose Agar at 30°C showed flat creamy brown, furrowed colonies with pale reverse by 3 days [Figure 3]. After about a week, satellite colonies have developed and the colonies have turned brown in colour [Figure 4]. Lactophenol cotton blue wet mount demonstrated aseptate hyphae and smooth walled zygospores with characteristic conjugation beaks, which confirmed the fungus to be B. ranarum [Figure 5]. Histopathological report says sections of normal skin with subcutaneous tissue showing inflammatory granulomatous reaction with diffuse and dense infiltration by eosinophils, polymorphs, histiocytes, plasma cells, lymphocytes, and few multinucleated giant cells. The central fragments showed fragments of aseptate hyphae.
Figure 3.

Furrowed colonies at 3 days on Sabourads Dextrose Agar
Figure 4.
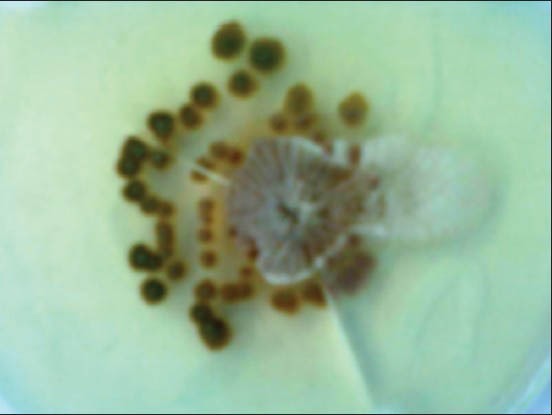
Growth at 10 days with brown pigmentation and satellite colonies
Figure 5.
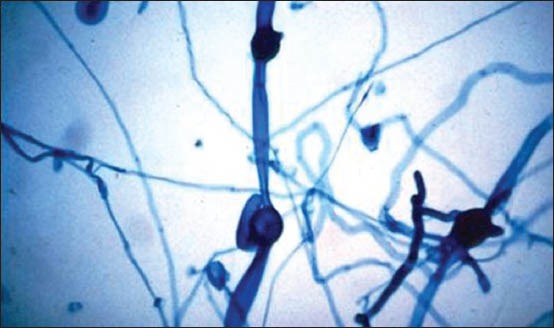
Lactophenol cotton blue preparation of the growth
Following the confirmation of the diagnosis as basidiobolomycosis by culture and microscopy, the patient was put on saturated solution of oral potassium iodide (KI) in milk. The initial dose was 5 drops (approximately 1 ml) thrice a day after meals followed by increase in dosage by 1 drop/dose until 40 drops/dose. Therapy was continued untill the signs of active disease have disappeared. Subsequently, the dosage has been decreased by 1 drop/dose until 5 drops were given, followed by discontinuation. Complete resolution of the lesions was seen by 8 weeks after initiation of treatment [Figure 6].
Figure 6.

Healed lesion
DISCUSSION
Basidiobolomycosis occurs predominantly in healthy individuals. B. ranarum typically causes a chronic infection of the peripheral or subcutaneous tissue, usually on the arms, trunk, and buttocks. The most common presentation for basidiobolomycosis is on the thighs and buttocks in a “bathing suit” distribution.[5] The infection is characterized by a hardened nodule, which expands and spreads locally. Although, the nodules will eventually ulcerate the overlying skin, dissemination usually does not occur. The nodular lesions contain inflammatory cellular material with many eosinophils, accounting for the associated erythema and warmth of the skin. The infection is slowly progressive without treatment but may heal spontaneously. B. ranarum has been reported to cause gastrointestinal infections, lymph node and muscle involvement apart from chronic granulomatous subcutaneous infection, but with a much lesser frequency.
Basidiobolus is relatively thermotolerant and is capable of growing, although, poorly, at 37°C, similar to the pathogenic Mucorales. It is hypothesized that thermotolerance is an important virulence factor for these organisms, allowing them to establish infections in vivo with those possessing growth capabilities above 37°C having the advantage of survival in the febrile patient.
The definitive diagnosis of basidiobolomycosis requires an excellent physical examination together with both pathologic and microbiologic evaluation, since basidiobolomycosis may resemble other infections, especially, other tropical infections, which present with subcutaneous lesions. Basidiobolus infection may resemble other fungal infections (pythiosis and sporotrichosis), parasitic infections (filarial elephantiasis and onchocerciasis), bacterial infections (Mycobacterium tuberculosis and Mycobacterium ulcerans), and other diseases, including Burkitt's lymphoma. While the direct examination may suggest the diagnosis, culture remains the “gold standard” for diagnosis.
Biopsy of subcutaneous tissue demonstrates broad, thin-walled hyphae together with acute and/or chronic inflammatory cell infiltrates. The mycelium of Basidiobolus is more septate than the hyphae of other zygomycetes. Hyphae are easily visualized with H and E stain. The organism does not typically invade the blood vessel and tissue; necrosis and tissue infarction are therefore not present.
Basidiobolus can be grown on standard mycology medium such as Sabouraud, potato dextrose, and cornmeal agars. Growth is moderately rapid at 30°C and less rapid at 37°C. Colonies are flat and furrowed, are yellowish to grayish on the surface with a pale reverse, and have a waxy texture. Satellite colonies sometimes form from the germination of ejected sporangioles. Colonies produce a musty odor.
After 7-10 days, the colony will be overgrown and the mycelia will contain masses of conidia, chlamydoconidia, and zygospores. Microscopically, colonies produce large vegetative hyphae (8-20 μm in diameter), which become increasingly septate with maturation. Basidiobolus produces two types of sporangiophores. Sporangiophores with inflated apices produce the single-spored sporangioles (ballistospores or conidia), measuring 7-15 by 6-12 μm in diameter. Conidia are ejected from the inflated, apical portion of the sporangiophore when the sub-conidial vesicle or swelling emits a stream of fluid that propels the conidium. This propulsion of conidia is a characteristic of the genus. Narrow sporangiophores with adhesive apices also produce single-spored sporangioles, however, these sporangioles are released passively. Sporangiospores may undergo cleavage to produce meristospores. They may also produce secondary sporangia.
In addition to culture, an infection with this agent may be diagnosed by detecting an immune response in an immunodiffusion test developed for the diagnosis of basidiobolomycosis.[6] This test has also been useful for monitoring infected patients. Serology has been useful in making a diagnosis of disease even in the absence of culture.
A discussion on the treatment of Basidiobolus infection must include a warning regarding prevention, since the organism has been introduced iatrogenically (via needle injection) and may be spread during diagnosis and treatment.
Pharmaceutical agents that have been used to successfully treat Basidiobolus infection include, most commonly KI, trimethoprim-sulfamethoxazole, amphotericin B, oral azoles, and KI combined with oral azoles. Treatment of Basidiobolus is not always successful, and no single drug has proved effective in the treatment of all cases of basidiobolomycosis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: A review of the clinical manifestations, diagnosis and treatment. Clin Microbiol Infect. 2004;10:31–47. doi: 10.1111/j.1470-9465.2004.00843.x. [DOI] [PubMed] [Google Scholar]
- 2.David H. Ellis: Ch 17-Subcutaneous zygomycosis. In: Topley and Wilson's: Microbiology and Microbial Infections– Medical Mycology. In: William G. Merz, Roderick J. Hay., editors. 10th ed. Paragraph 2. London: Hodder Arnold publishers; 2005. p. 348. [Google Scholar]
- 3.Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000;13:236–301. doi: 10.1128/cmr.13.2.236-301.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gugnani HC. A review of zygomycosis due to Basidiobolus ranarum. Eur J Epidemiol. 1999;15:923–9. doi: 10.1023/a:1007656818038. [DOI] [PubMed] [Google Scholar]
- 5.Jagadish Chander Textbook of Medical Mycology. 3rd ed. India – New Delhi: Mehta publishers; 2009. Jagadish Chander: Ch 25 – Zygomycosis; pp. 378–79. [Google Scholar]
- 6.Nemenqani D, Yaqoob N, Khoja H, Al Saif O, Amra NK, Amr SS. Gastrointestinal basidiobolomycosis: An unusual fungal infection mimicking colon cancer. [Last accessed 2013 Jan 31];Arch Pathol Lab Med. 2009 133:1938–42. doi: 10.5858/133.12.1938. Available from: http://www.archivesofpathology.org/doi/pdf/101043/1543-2165-133.12.1938 . [DOI] [PubMed] [Google Scholar]


