Abstract
Epidermodysplasia verruciformis (EV) is a rare, inherited disorder that predisposes patients to widespread human papillomavirus (HPV) infection and cutaneous squamous cell carcinomas. There is still no definitive therapeutic modality for EV. A 24 year old male patient with EV was treated with oral zinc sulphate, one of the cheapest and safe immuno-modulator available as therapeutic agent with satisfactory result.
Keywords: Epidermodysplasia verruciformis, wart, zinc
INTRODUCTION
Epidermodysplasia verruciformis (EV) is most commonly inherited in an autosomal recessive manner, although sporadic, sex-linked, and autosomal dominant inheritance has been described.[1] The disease is characterized by chronic infection with human papilloma virus HPV types 3, 5, 8, 9, 10, 12, 14, 17, 20, 21, 23, 25, 28, 38, 47, 49. Widespread skin eruptions of flat to papillomatous, wartlike lesions and reddish brown pigmented plaques on the trunk, extremities and the face are typical.[1] Malignant skin tumor especially squamous cell carcinoma develops in 30-70% patients, most commonly on sun exposed areas starting between the ages of 20 and 40 years.[1]
CASE REPORT
A 24-year-old male presented in our out-patient department with complaints of multiple asymptomatic raised warty lesions on the face and extremities since 4 years of age and multiple asymptomatic light colored flat lesions on the trunk and axilla since 4 years of age. These lesions had appeared over a period of time and were progressively increasing in number, size and area of involvement.
He also had an asymptomatic non-healing ulcer in the right first web space for the last 1 year. Initially, it was small but over past 3 months it progressively increased in size. Mucocutaneous examination revealed multiple dark colored warty papules and plaques over the face, neck and extremities [Figures 1-3]. Multiple hypopigmented macules like those of pityriasis versicolor were present predominantly in bilateral axilla, upper back and shoulders. An ulcer of size 6-7 cm was present in first web space of the right hand [Figure 2]. It was non-tender, firm in consistency and the surface showed hemorrhagic crusting with rolled out margins.
Figure 1.

Response of oral Zn therapy on the face
Figure 3.

Response of oral Zn therapy on the lower extremities
Figure 2.

Response of oral Zn therapy on the upper extremities
Hematological, renal, hepatic biochemical parameters and chest X-ray were normal. X-ray of the right hand showed soft-tissue shadows in first web space with no bony involvement. MRI of right hand showed ill-defined heterogeneous lesion in the first web space of right hand (2.4 × 2.8 × 3.3), involving the lumbricals and palmar interossei on the lateral aspect and closely averting flexor digitorum superficialis tendon.
Skin biopsy from the warty lesion present on the extensor surface of right forearm revealed hyperkeratosis, irregular acanthosis, and an enlarged vacuolated cells suggestive of koilocytes. These histopathological features were consistent with EV [Figure 4]. Histopathological examination from the margin of ulcer present on the right first web space showed multiple dysplastic cells and was consistent with well differentiated squamous cell carcinoma. Rest of the metastatic work up was within normal limit.
Figure 4.
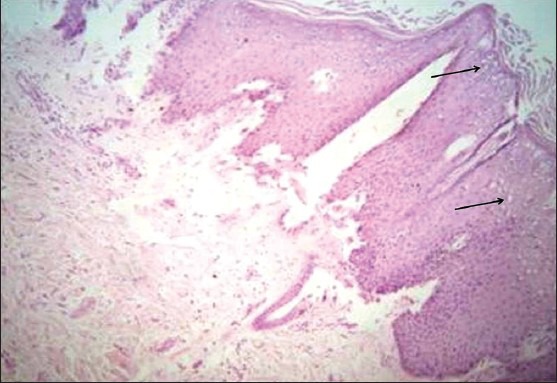
Histopathological examination shows hyperkeratosis, irregular acanthosis and koilocytes (black arrows) (H and E, ×400)
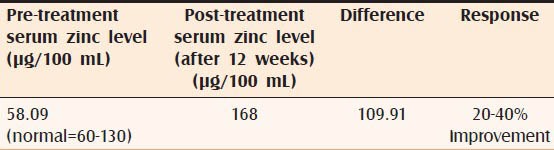
With all above findings the diagnosis of EV with squamous cell carcinoma of right hand was made. The patient was started on oral zinc sulphate 550 mg/day (10 mg/kg) for twelve weeks and followed-up for the next 6 months. Serum zinc level prior to starting zinc therapy was 58.09 μg/100 mL [Table 1] and on completion of treatment it was 168 μg/100 mL (difference 168 - 58.09 = 109.91) [Table 1]. The main outcome measured was complete clearance of verrucae at 12 weeks as observed on digital photographs taken by the physician delivering the treatment at baseline and 12 weeks. Complete clearance of verrucae was defined as the restoration of normal skin upon close inspection, as assessed by the physician [Figures 1-3].
Table 1.
Serological and clinical response after oral zinc therapy
The squamous cell carcinoma of right hand was removed after surgical consultation. No side-effects were reported by patient during the therapy and in the follow-up period.
DISCUSSION
The pathophysiology of EV is linked to defective cell-mediated immunity, with elucidation of mutations in EVER1 (Epidermodysplasia Verruciformis Enhancing Region) and EVER2 genes.[2,3] Although, the role of EVER1 and EVER2 genes in the pathogenesis of EV remains unclear, one hypothesis is that they are involved in the control of HPV infection within keratinocytes, or they play a role in the immune response to the infection itself.[4] Intracellular zinc homeostasis regulated by a complex of EVER proteins and zinc transporter proteins may play a role in inhibiting EV-HPV (Epidermodysplasia Verruciformis-Human Papilloma Virus) expression, especially EVER2 was found to inhibit free zinc influx to nucleoli. Keratinocytes with a mutated EVER2 grew faster than wild-type keratinocytes.[4] However, an estimated 25% of patients with EV lack mutations in EVER1 and EVER2, with the genetic defect in these patients not yet elucidated.[5]
Because HPV infection is non-lytic, antigen presentation occurs very slowly. HPV infection does not induce inflammatory cytokines therefore, therapeutic options aimed at modulating the immune system and facilitating the production of cytokines have been proposed.[6]
Morbidity and mortality associated with EV may be avoided by early recognition of the disease, sun avoidance, monitoring by a dermatologist, and treatment of premalignant and malignant lesions.
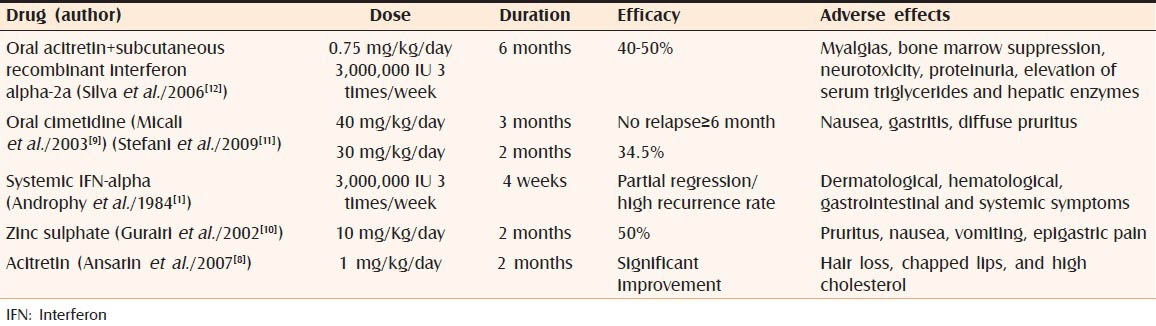
Medical management for EV includes topical imiquimod and 5-fluorouracil, systemic retinoids, interferon-alpha, cimetidine, zinc, and combination therapy [Table 2].[1,7,8,9,10,11,12]
Table 2.
Comparison in between various therapeutic modalities in epidermodysplasia verruciformis
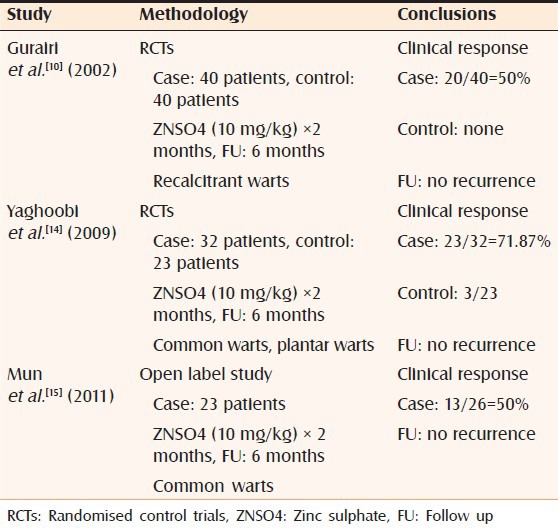
Oral zinc had been used by many authors either alone as well as in combination therapy with satisfactory to good results [Tables 2 and 3].[1,7,8,9,10,11,12] Prescribing zinc is due to its immunomodulatory effects. Zinc is a micronutrient that is necessary for the normal functioning of cells. More importantly, this element modulates DNA and RNA related enzymes and is also involved in many immunologic processes. Kitamura et al.[13] proposed that toll-like receptors mediated regulation of zinc homeostasis which influences dendritic cell function.[13] Zinc may be administered as acetate, gluconate or sulphate, but the latter seems to be better tolerated. One 100 mg capsule of zinc sulphate has 22.5 mg of elemental zinc. Normal plasma levels of zinc are 70-110 μg/dl.[13]
Table 3.
Zinc therapy in warts and epidermodysplasia verruciformis
In this patient, with oral zinc sulphate we got the fairly satisfactory results as warty lesions on the extremities were flattened more as compared to facial lesions in the range of 20-40%. Area wise clearance rate was 20% on face, 30% proximal upper extremities, 35% distal upper extremities, 35% proximal lower extremities and 40% distal lower extremities. There was no improvement in the pityriasis versicolor like hypopigmented lesions on the axilla and upper back. No side-effects were recorded during the therapy and follow-up period.
So far studies conducted on zinc in multiple or recalcitrant warts and EV showed response rate from 50% to 70% without any recurrence after 6 months of follow up [Table 3].[10,14,15] In present case, response rate was from 20% to 40% without any recurrence after 6 months.
We concluded that zinc therapy had a role in treatment of EV but in previous studies the response rate was much higher (50-70%) as compared to our observation (20-40%). The higher response rates of 50-70% were obtained in cases of recalcitrant common warts where the HPV types and pathophysiology involved are different from that in epidermodysplasia verruciformis EDV. This may be a reason of lower response rate with zinc therapy in our case but still more clinical trials are required to evaluate the actual response rate with zinc therapy in EV.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Androphy EJ, Dvoretzky I, Lowy DR. X-linked inheritance of epidermodysplasia verruciformis. Genetic and virologic studies of a kindred. Arch Dermatol. 1985;121:864–8. [PubMed] [Google Scholar]
- 2.Gober MD, Rady PL, He Q, Tucker SB, Tyring SK, Gaspari AA. Novel homozygous frameshift mutation of EVER1 gene in an epidermodysplasia verruciformis patient. J Invest Dermatol. 2007;127:817–20. doi: 10.1038/sj.jid.5700641. [DOI] [PubMed] [Google Scholar]
- 3.Sun XK, Chen JF, Xu AE. A homozygous nonsense mutation in the EVER2 gene leads to epidermodysplasia verruciformis. Clin Exp Dermatol. 2005;30:573–4. doi: 10.1111/j.1365-2230.2005.01858.x. [DOI] [PubMed] [Google Scholar]
- 4.Lazarczyk M, Pons C, Mendoza JA, Cassonnet P, Jacob Y, Favre M. Regulation of cellular zinc balance as a potential mechanism of EVER-mediated protection against pathogenesis by cutaneous oncogenic human papillomaviruses. J Exp Med. 2008;205:35–42. doi: 10.1084/jem.20071311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDermott DF, Gammon B, Snijders PJ, Mbata I, Phifer B, Howland Hartley A, et al. Autosomal dominant epidermodysplasia verruciformis lacking a known EVER1 or EVER2 mutation. Pediatr Dermatol. 2009;26:306–10. doi: 10.1111/j.1525-1470.2008.00853.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parton AM, Sommerville RG. The treatment of plantar verrucae by triggering cell-mediated immunity. Br J Pod Med. 1994;131:883–6. [Google Scholar]
- 7.Heratizadeh A, Völker B, Kupsch E, Wichmann K, Kapp A, Werfel T. Successful symptomatic treatment of epidermodysplasia verruciformis with imiquimod 5% cream. Hautarzt. 2010;61:1052–5. doi: 10.1007/s00105-010-1998-4. [DOI] [PubMed] [Google Scholar]
- 8.Ansarin H, Tajziehchi L, Shaianfar N. A case of epidermodysplasia verruciformis with squamous cell carcinomas on non-sun-exposed areas of skin. Arch Iran Med. 2007;10:261–3. [PubMed] [Google Scholar]
- 9.Micali G, Nasca MR, Dall’Oglio F, Musumeci ML. Cimetidine therapy for epidermodysplasia verruciformis. J Am Acad Dermatol. 2003;48:S9–10. doi: 10.1067/mjd.2003.111. [DOI] [PubMed] [Google Scholar]
- 10.Al-Gurairi FT, Al-Waiz M, Sharquie KE. Oral zinc sulphate in the treatment of recalcitrant viral warts: Randomized placebo-controlled clinical trial. Br J Dermatol. 2002;146:423–31. doi: 10.1046/j.1365-2133.2002.04617.x. [DOI] [PubMed] [Google Scholar]
- 11.Stefani M, Bottino G, Fontenelle E, Azulay DR. Efficacy comparison between cimetidine and zinc sulphate in the treatment of multiple and recalcitrant warts. An Bras Dermatol. 2009;84:23–9. doi: 10.1590/s0365-05962009000100003. [DOI] [PubMed] [Google Scholar]
- 12.Silva CS, Ramos RO, Pires MC, Sittart JAS. Epidermodysplasia verruciformis: Combined treatment with acitretin and interferon alpha-2a. An Bras Dermatol. 2006;81:595–7. [Google Scholar]
- 13.Kitamura H, Morikawa H, Kamon H, Iguchi M, Hojyo S, Fukada T, et al. Toll-like receptor-mediated regulation of zinc homeostasis influences dendritic cell function. Nat Immunol. 2006;7:971–7. doi: 10.1038/ni1373. [DOI] [PubMed] [Google Scholar]
- 14.Yaghoobi R, Sadighha A, Baktash D. Evaluation of oral zinc sulfate effect on recalcitrant multiple viral warts: A randomized placebo-controlled clinical trial. J Am Acad Dermatol. 2009;60:706–8. doi: 10.1016/j.jaad.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 15.Mun JH, Kim SH, Jung DS, Ko HC, Kim BS, Kwon KS, et al. Oral zinc sulfate treatment for viral warts: An open-label study. J Dermatol. 2011;38:541–5. doi: 10.1111/j.1346-8138.2010.01056.x. [DOI] [PubMed] [Google Scholar]


