Sir,
Treatment of acne scars is a dilemma both for the treating physician and the patient as no oral or topical medicine works and it is associated with emotional and psychological stress. Acne scars are classified into three different types: Atrophic, hypertrophic, or keloidal. Atrophic scars are the most common type of acne scars. They have been further classified into three types as described by Jacob et al.[1] into ice-pick scars, rolling scars, and boxcar scars. Most of the patients with atrophic acne scars have more than one type of scars.
Various treatment modalities like punch excision and elevation, subcision, chemical peeling using various strengths of TCA, micro-needling, ablative, non-ablative lasers and fillers either singly or in combinations have been described in literature with varying results. Most of these procedures require costly equipment and materials and not affordable by many people.
Subcision or subcutaneous incision-less surgery is a term coined by Orentreich and Orentreich[2] in 1995 as the treatment option for atrophic acne scars. Here hypodermic 18 no. needle is used to break the fibrotic strands that tethered the scars to the underlying tissues leading to uplifting of scars. Combining subcision with other scar revision techniques or repeated subcisions may be beneficial to the patients.[3] TCA chemical reconstruction of skin scars (CROSS)[4] is another useful method for treatment of atrophic acne scars. It involves focal application of 50-100% of TCA with a wooden applicator on the base of an atrophic scar, which causes precipitation of proteins and coagulative necrosis of cells in the epidermis. There is necrosis of collagen in the papillary and upper reticular dermis. Healing is rapid because of sparing of adjacent normal tissues and adnexal structures. So there is reorganization of dermal structural elements and increase in collagen content that leads to filling of the atrophic scar.
While going through the literature, we found that different studies have used subcision and CROSS TCA alone or in combination with other techniques as well as their comparative studies but we did not find any study combining these two techniques together to the best of our knowledge. Encouraged by that, we combined subcision and TCA cross in all types of scars as subsicion breaks the dermal tethering of the scar tissue and TCA will remodel the collagen underneath the scar which treats the basic pathology of the scar to some extent.
In our study, 10 female patients between the age group of 20-35 years of skin type 4 and 5 with atrophic acne scars on the face were randomly selected. Most of the patients had more than one type of atrophic scars of grade 4 severity as described by Goodman.[5] In all the patients, there were no active acne lesions and none of them were on oral isotretinoin 3 months prior to inclusion in our study. Patients with keloidal tendencies, bleeding diathesis, and history of recurrent herpes simplex were excluded. Complete hemogram, random blood sugar levels, and viral markers were done in all the patients. Written consent after explaining the risks and benefits of treatment was taken from all the patients along with pre-/post-procedure photographs. Subcision followed by 50% TCA CROSS was done at 4 weeks interval for three sessions. Patients were followed-up monthly for improvement in scars up to 6 months.
Priming was done 2 weeks prior to the treatment with 2% hydroquinone and tretinoin 0.025% cream at night and sunscreen more than 30 sun protection factor (SPF) was given in the morning. Procedure was carried out after application of topical anesthetic cream for 45 min followed by infiltration of 2% Xylocaine with normal saline under aseptic conditions. A no. 18 hypodermic needle attached to a syringe was introduced horizontally underneath each scar and was moved back and forth till the snapping sound was heard. We used no. 18 hypodermic needle because it is cheap and easily available. Homeostasis was maintained by pressure. We cleaned the entire area with normal saline which was followed immediately by 50% TCA with the tip of a toothpick by pressing hard on the entire area of depressed atrophic acne scars irrespective of the type of scar and frosting was taken as the end point, antibiotic cream was applied, and patient was sent home. Patient was advised to apply antibiotic cream twice daily followed by sunscreen in the morning. Erythema, edema, and crusting lasted for 7-10 days in all the patients to varying severity. After 10 days, the patient was advised to apply azelaic acid 20% cream at night.
Results were evaluated on the basis of global scar grading system, visual improvement by photographs and patient satisfaction. The global acne scarring classification is a four-category qualitative system by Goodman[5] based on scar morphology and ease of masking by makeup or normal hair patterns. Grade 1 means macular scarring only, Grade 2 is mild atrophy, which is not visible beyond 50 cm and can be easily masked by makeup, Grade 3 is moderate atrophy obvious at social distance not easily masked by makeup while Grade 4 is severe atrophy.
Percentages in improvement were calculated as a combination of the three parameters, i.e. global scar grading system by Goodman, visual improvement by photographs showing the change in the grade and patient satisfaction, which was assessed by giving a questionnaire to the patient where they had to rate their improvement on 0-10 point scale.
Excellent >70%
Good 50-70%
Fair 30-50%
Poor <30%
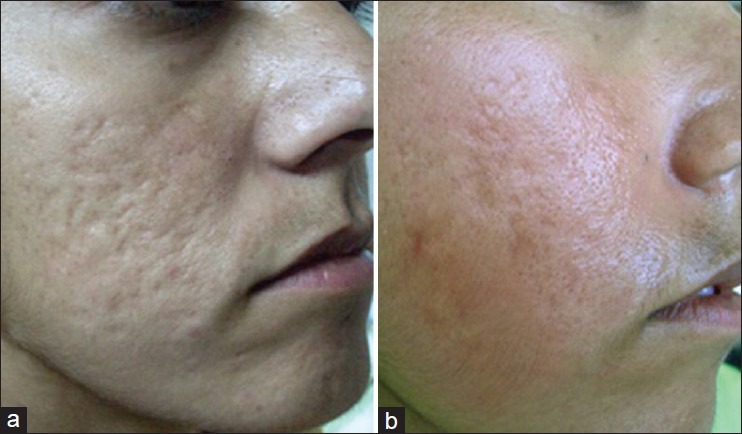
We labeled results as excellent when there was a two-grade change in the scars observed by the dermatologist both by grading system, photographs, and patient rated his improvement as more than 7 [Figures 1 and 3].
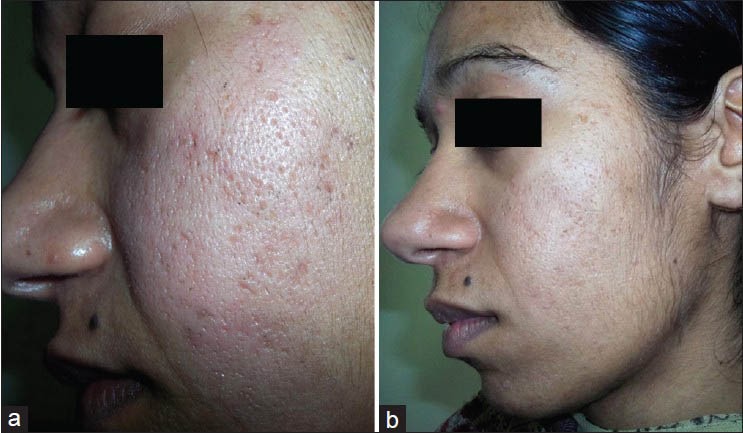
Results were taken as good when there was one-grade improvement in acne scars observed by the dermatologist both by grading system, photographs, and patient rated his improvement as 5, 6, or 7 [Figure 2].
Results were taken as fair when there was improvement in acne scars observed by the dermatologist by photographs only and patient rated his improvement as 3, 4, or 5.
Results were taken as poor when there was no improvement in acne scars observed by the dermatologist either by photographs or by grading system but it was only subjective improvement as told by the patient when they rated it between 1 and 3.
Figure 1.
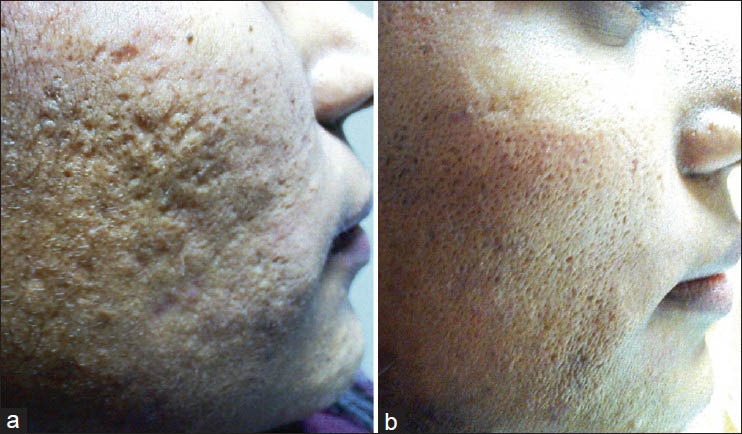
Sites involved right cheek. (a) Post-acne scars mostly ice pick, boxcars and few roller scars. (b) Decrease in number and depth of scars
Figure 3.
Site involved is left cheek and left temple. (a) Many ice pick scars and a few boxcars and very few rolling scars. (b) Decrease in depth and size of scars
Figure 2.
Sited involved right cheek. (a) Multiple post-acne ice pick and roller scars. (b) Decrease in size and depth of all the scars
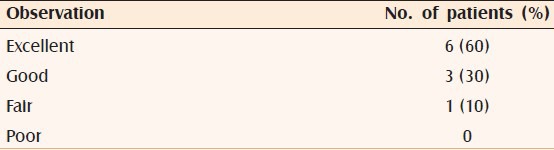
In all the patients, scar grading improved from grade 4 to grade 2 and results were graded excellent, good, and fair in 6, 3, and 1 patients respectively [Table 1]. Although in various studies best results with CROSS TCA are seen in ice-pick scars but since in our study we combined it with subcision, results were equally good even in rolling scars and boxcars scars. Post-inflammatory hyperpigmentation was transient in three patients, which persisted for 15-20 days post-procedure, which further decreased over the time period with 20% azelaic acid and in one case, the mild hyperpigmentation persisted even at the end of 6 months in spite of the best efforts for reasons not known. The patients were also happy with the results except for the one where hyperpigmentation persisted. Although the procedure has a downtime in the form of erythema, edema, and crusting, it is comparable to all other resurfacing procedures and the problem of post-inflammatory hyperpigmentation can be judiciously tackled with the proper and repeated use of sunscreens and lightening agents. Each procedure when done individually has downtime of few days. So, we tried to reduce it by combining the two procedures. Hence, it can be concluded that subcision combined with TCA CROSS is a simple, safe, and cost-effective procedure, which does not require any specialized or costly equipments or materials or any special training and can be performed as an out-patient-department procedure by any budding dermatologist.
Table 1.
Showing results
REFERENCES
- 1.Jacob CI, Dover JS, Kaminer MS. Acne scarring: A classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109–17. doi: 10.1067/mjd.2001.113451. [DOI] [PubMed] [Google Scholar]
- 2.Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21:543–9. doi: 10.1111/j.1524-4725.1995.tb00259.x. [DOI] [PubMed] [Google Scholar]
- 3.Alam M, Omura N, Kaminer MS. Subcision for acne scarring: Technique and outcomes in 40 patients. Dermatol Surg. 2005;31:310–7. doi: 10.1111/j.1524-4725.2005.31080. [DOI] [PubMed] [Google Scholar]
- 4.Lee JB, Chung WG, Kwahck H, Lee KH. Focal treatment of acne scars with trichloroacetic acid: Chemical reconstruction of skin scars method. Dermatol Surg. 2002;28:1017–21. doi: 10.1046/j.1524-4725.2002.02095.x. [DOI] [PubMed] [Google Scholar]
- 5.Goodman GJ, Baron JA. Postacne scarring: A qualitative global scarring grading system. Dermatol Surg. 2006;32:1458–66. doi: 10.1111/j.1524-4725.2006.32354.x. [DOI] [PubMed] [Google Scholar]


