Abstract
Background: A model of quality management called Strategic Collaborative Quality Management (SCQM) model was developed based on the quality management literature review, the findings of a survey on quality management assessment in healthcare organisations, semi-structured interviews with healthcare stakeholders, and a Delphi study on healthcare quality management experts. The purpose of this study was to verify the SCQM model.
Methods: The proposed model was further developed using feedback from thirty quality management experts using a Delphi method. Further, a guidebook for its implementation was prepared including a road map and performance measurement.
Results: The research led to the development of a context-specific model of quality management for healthcare organisations and a series of guidelines for its implementation.
Conclusion: A proper model of quality management should be developed and implemented properly in healthcare organisations to achieve business excellence.
Keywords: Strategic Quality Management, Healthcare Organisations, Modelling
Background
Total Quality Management (TQM) was not very successful in health sector (1–3). An ineffective TQM model, inappropriate TQM implementation methods and an inappropriate environment for implementing TQM were the main reasons for TQM failure in healthcare organisations (4). The failure of TQM in healthcare is due to the complexity of the healthcare systems, bureaucratic and highly departmentalised structure, multiple layers of authority, professional autonomy, and tensions between managers and professionals (5–7). Insufficient motivation for professionals to participate in TQM initiatives, the difficulties involved in evaluating the processes and outcomes, and a lack of market based competition were the major obstacles to TQM implementation in the health sector (8–10). Other barriers to successful TQM implementation in health sector were authoritative leadership, lack of top managers’ support, lack of employees’ involvement, lack of a plan for change, inadequate resources, lack of a quality-oriented culture, insufficient education and training, poor communication, and lack of customer focus (11–14).
TQM migrated into the health sector from the manufacturing sector of the economy during the 1980s. Professional healthcare organisations are very different from traditional industrial companies. The limited success of TQM in healthcare organisations led the author to search for a more viable solution, and as a result, the Strategic Collaborative Quality Management (SCQM) model was created (15).
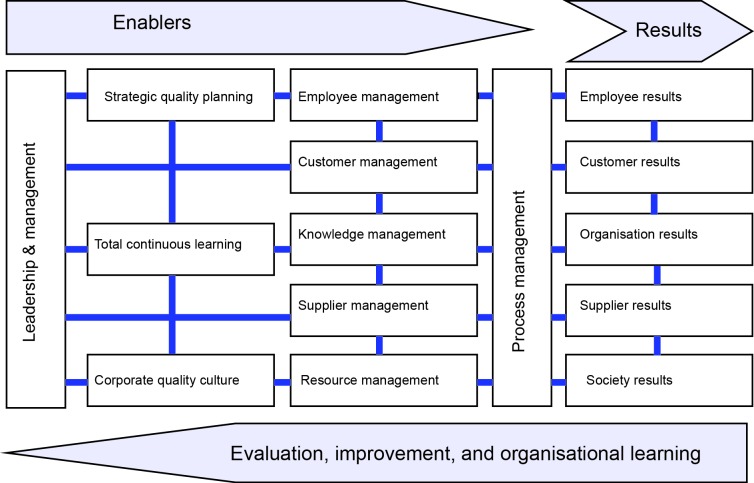
The SCQM model consists of 15 constructs, of which ten are enablers and five are results. The relationship among SCQM constructs is shown diagrammatically in Figure 1. The effectiveness of quality management arises from leadership and management efforts towards defining and communicating a strategic quality plan, and creating a learning organisation and a corporate quality culture to facilitate the management of employees, customers, suppliers, resources, knowledge and processes. An effective implementation of these practices supports the satisfaction of employees, customers, suppliers and society and improves organisational performance (15).
Figure 1.
A diagrammatic representation of the SCQM model
SCQM’s requirements are clear and well defined, unlike the vague descriptions and non-specific requirements of TQM (16,17). A clear definition of SCQM provides a common understanding of the concept. SCQM is an integrated system of principles, methods and best practices that provides a framework to strive for excellence by continuously improving organisational performance through leadership and management, strategic quality planning, corporate quality culture, total continuous learning, employees’ management, customer management, knowledge management, supplier management, resource management and process management.
The SCQM model is more comprehensive in terms of quality management constructs compared to other quality management models (e.g., ISO 9001, EFQM, and MBNQA). Constructs such as resource management and society results were either missing or covered under other constructs in the MBNQA model. Similarly, strategic quality planning and customer focus which enhance organisational performance, were either missing or covered under other constructs in the EFQM model. In contrast to the EFQM and MBNQA models, supplier management and supplier results are included as separate constructs in the SCQM framework. ISO 9000 contributes more in the areas of process management and quality data. Its contribution is much lower in the areas of leadership, human resource management and partnership development with suppliers (18).
TQM models such as EFQM and MBNQA give a low weighting to education and quality culture, while these constructs of quality management are very important in driving the organisation towards business excellence (19–20). The SCQM model highlights the importance of developing a culture of trust, creativity, empowerment, teamwork, cooperation and continuous improvement. SCQM emphasises the importance of organisational learning in developing a corporate quality culture, and sustainable quality improvement activities. SCQM also highlights the importance of providing education and training for customers and suppliers.
SCQM is a combination of strategic management, quality management and project management (Figure 2). SCQM integrates the principles of quality management into all the three steps of strategic management (i.e., Strategy formulation, strategy implementation and strategy evaluation). As a result, organisations formulate strategic quality goals and objectives, develop action plans, allocate resources, implement the action plans and evaluate the progress towards achieving strategic quality goals and objectives. In fact, SCQM considers continuous quality improvement into the process of formulating, implementing and evaluating strategic goals and objectives. The project management approach enhances the effectiveness and efficiency of action plans through planning, implementing, monitoring and controlling purposeful, well-defined and timely quality improvement projects. A project management approach helps to build a culture of quality and learning throughout the organisation.
Figure 2.

The SCQM model
There is no standard method for TQM implementation in an organisation. A lack of practical knowledge of methods and guidelines for TQM implementation was the main reason for TQM failure (21–24). EFQM and MBNQA models fail to offer practical methods for quality management implementation to achieve good outcomes. In contrast, road maps, techniques and methods for implementing SCQM are better defined. A well-defined model of quality management helps organisations implement quality management principles and practices effectively and efficiently. A coherent set of SCQM principles and methodology, guides managers and practitioners to define measure and control the quality of products or services.
SCQM involves changes in the structure, context (culture, values and political system) and processes of an organisation. The logic of structural, contextual and procedural changes seems to be the best sequence of activities for quality management implementation to reach the maximum result. Such a change provides lasting and significant positive results. Systems thinking, process mapping and process capability analysis in the SCQM model, help to identify opportunities to improve outcomes by improving structures and processes. Further, the SCQM’s approach to the change is fundamental, gradual and evolutionary. It considers a comprehensive change at individual, teams and organisational levels. In SCQM, the emphasis is on redesigning simpler, standardised and more effective processes, determining reasonable and achievable objectives for processes, and improving them continually and continuously until objectives are achieved. Employees using problem-solving techniques evaluate the ability of the processes to reduce variation and provide high quality and defect-free services. They plan for the desired situation and change the organisation accordingly. As a result, they would be more motivated and committed.
EFQM and ISO models provide generic guidelines that come from industry experience and do not specifically address all areas relevant to healthcare (25). Therefore, quality improvement is mainly limited to peripheral and administrative activities, rather than clinical procedures. Moeller believes that incorporating clinical standards in EFQM assessment model provides the potential to deliver high quality services (26). It encourages healthcare organisations to improve clinical procedures, rather than being limited to administrative activities. A healthcare version of MBNQA was developed on similar lines of the manufacturing industry. In this version, organisational performance results replaced the business results category and focus on patients and other stakeholders replaced the customer focus category (27).
The SCQM model does not aim to reduce professional autonomy in healthcare organisations. Managers and professionals work together as a team to improve core (clinical) and supportive (administrative) processes to meet predetermined standards and satisfy customers’ needs. The SCQM model integrates twelve management techniques to manage the organisation effectively and efficiently and to satisfy various stakeholders’ needs and expectations. SCQM using the main principles of Hoshin Kanri, Business process reengineering, Six sigma, Quality function deployment, Kizen, Clinical pathways and Balanced scorecard improves employees, customer and supplier satisfaction in healthcare sector. Clinical pathways as practice guidelines assist practitioners in defining, standardising and managing clinical processes and assuring quality care. These clinical pathways document the care plan and expected patient outcomes for a specific procedure or diagnosis within a given time frame (28).
The SCQM model is more result-oriented than TQM models. Unlike the MBNQA model, SCQM does include financial performance of the organisation. SCQM does not only focus on financial and operational performance indicators. It also looks at the impact of process improvement on employees, customers, suppliers and society. SCQM rests balanced emphasis on needs and legitimate expectations of various stakeholders. SCQM has a focus on effective collaboration with both internal and external customers. It aims to increase various stakeholders’ satisfaction and as a result, increase their commitment and loyalty to the organisation. SCQM emphasises a win-win relationship with not only customers, but also with employees and suppliers. The SCQM model highlights the importance of supplier results, while this construct of quality management is missing in EFQM or MBNQA models.
Methods
Purpose and objectives
The purpose of this study was to assess the internal validity of the proposed quality management model (SCQM). The study aimed to verify and develop further a quality management model for healthcare organisations, as well as a method for its implementation.
Method
This study utilised a three-round electronic contributory Delphi procedure with a panel of thirty quality management experts. Using an open questionnaire, the first draft of the conceptual, implementation and assessment models of SCQM was sent to quality management experts for review and comment. Experts’ suggestions were studied and considered in the second draft of the model. The second draft of the model was then sent to the participants for further comments. Results from round two were then used to develop the model further. Finally, the revised model was sent to the respondent group. So the panel members could express their comments on the revised SCQM model.
Instrument
An open questionnaire was used to evaluate the suitability of the proposed quality management framework for the healthcare sector. The questionnaire contained a cover letter that briefly explained the purpose of the study and the mechanisms to maintain confidentiality. The questionnaire consisted of two sections. The first section dealt with gathering participants’ general information. The second part of the questionnaire included questions in six areas: the constructs and sub-constructs of the model, the relationships between the constructs, the suitability of the proposed model for the health sector, the techniques for implementing the model, the implementation process and the assessment criteria. A literature review was carried out to develop the instrument (29–34).
Participants
Thirty experts from nine countries from both academia and the healthcare industry were invited to participate. They were professionals with expertise in quality management in healthcare and modeling. As described in Table 1 , 80% of the respondents were male. Respondents ranged in from 30 to 85 with a mean of 44.3 years (SD=12.47). On average, they had 12.9 (SD=10.1) years of experience in quality management. The majority had a doctoral degree (53.3 %).
Table 1. The demographic characteristics of Delphi panel experts .
| Demographic variables | Frequency (%) |
| Gender | |
| Male | 24 (80.0) |
| Female | 6 (20.0) |
| Age | |
| 30 to 39 years | 11 (36.7) |
| 40 to 49 years | 14 (46.7) |
| 50 years or older | 5 (16.7) |
| Work experience in quality management | |
| 5 to 10 years | 18 (60.0) |
| 11 to 15 years | 6 (20.0) |
| 16 to 20 years | 2 (6.7) |
| 21 to 25 years | 2 (6.7) |
| 26 to 30 years | 2 (6.6) |
| Education | |
| Bachelor of Science | 3 (10.0) |
| Master of Science | 9 (30.0) |
| Doctor of Medicine | 2 (6.7) |
| Doctor of Philosophy | 16 (53.3) |
| Occupation | |
| Academic | 10 (33.3) |
| Quality manager | 10 (33.3) |
| Hospital manager | 2 (6.7) |
| Quality management consultant | 8 (26.7) |
Results
Participants found the proposed quality management model comprehensive which considers the most important critical success factors of quality management implementation. “Overall, it is a comprehensive model.” (P15); “The above mentioned construct and sub-construct [of the model] include all the criteria to develop a successful [quality management] programme.” (P27); and “This is a nice schematic, incorporating the relevant factors in the process.”(P30)
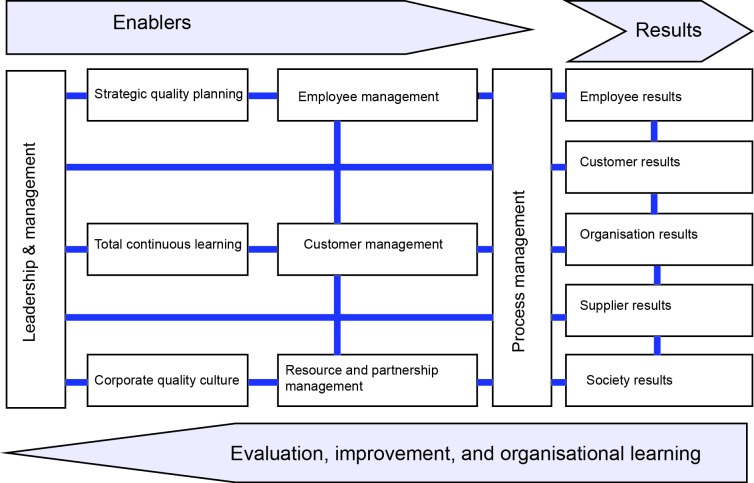
Participants were concerned mainly about the number of constructs in the model. “Your model is too complicated and complex. There are many variables in the model. I do not say it is wrong; rather, it is too complex. My recommendation is to narrow it down.” (P23) “This model is quite sophisticated. Therefore, you may encounter implementation barriers in organisations that have not focused their energies on understanding and managing their performance.” (P28) Therefore, the author reduced the number of constructs to thirteen. Resource management, knowledge management and supplier management constructs were merged together to form a new construct called “Resource and partnership management”.
All participants found the relationships between enablers and results in the proposed model clear and rational. “The model’s components are clear and flow from each other.” (P28) “This model is much clearer than the EFQM model.” (P19) “In my opinion, the constructs and their component sub-constructs are relevant.” (P26) “The relationship among them[model’s constructs]is rational.” (P2)
All participants agreed that the proposed model is applicable in the health sector: “I think that the proposed SCQM model is a comprehensive and feasible model that can be applied to managing clinical and service quality in healthcare organisations.” (P28) “Yes, in my opinion the model would be entirely applicable to healthcare organisations.” (P26) “This model is useful for healthcare organisations.” (P21) Nevertheless, some experts considered the model as generic and not specific for the health sector: “I think your model is a generic model. It is not developed specifically for the health sector.” (P4); “I do not think that the constructs of the model are health service-specific.” (P7) Although the principles, values and constructs of the model are universal and generic to manufacturing and service institutions, its application is context-specific.
Quality management experts found the model’s implementation techniques comprehensive and useful. “The techniques are comprehensive.” (P23 & 28) “The attempt to meld the principal features of various established techniques is innovative and worthy of being tested in the real world applications.” (P26) They were also concerned about the number of techniques and the time needed to use the model’s techniques. “Although the techniques are comprehensive, it takes time for an organisation to implement them completely and it would cost them a lot.” (P14) Although the model uses twelve techniques in a period of at least two years, these techniques will be used by different groups of people in an organisation. For example, managers use quality costing, benchmarking, Hoshin Kanri and balanced scorecard techniques to design the implementation plan and provide the required information for quality improvement activities. Employees mainly use a simple quality improvement technique to improve the quality of their services.
Experts evaluated the implementation of the model as logical. “The model follows a logical process as described by the normative change models.” (P28 & 14) Some experts were concerned about the degree of involvement by employees, particularly physicians, in the model. “The model implementation should be tailored to the needs of employees.” (P7); “The cooperation and collaboration of clinicians are critical. This is the management’s responsibility to get them involved in the quality management implementation.” (P30)
The model uses participative management techniques (e.g., employee Suggestion Scheme and quality improvement teams) which help engaging employees in the implementation process. Furthermore, the structural and procedural changes required by the model will stimulate employees’ participation. Moreover, the evaluation and auditing system in the model are designed in a way that encourages staff commitment and involvement in quality management activities.
Some participants raised the need to consider the role of external factors affecting SCQM implementation. “…The model is a bit internalised. Many aspects of quality are externalised through government agencies and regulations. Perhaps your model should recognise the influence of external agencies.” (P29); “The role of the external environment should be considered in the model.” (P4 & 6); and “Your model should consider external and contingency factors. You need to include the external environment in your model.” (P1) SCQM uses strategic quality planning which helps healthcare organisations investigate their internal and external environments. Therefore, as experts mentioned, institutional characteristics and external factors will be considered by the organisation in developing its SCQM implementation plan.
Discussion
SCQM provides a system of quality management with thirteen constructs, of which eight are enablers and five are results. The relationship among SCQM constructs is shown diagrammatically in Figure 3. The driver is leadership that develops a strategic quality plan, promotes continuous learning, shapes a corporate quality culture, and manages employees, customers and resources, which lead to excellence in overall organisational performance.
Figure 3.
A conceptual framework of SCQM model
In this study, SCQM is defined as follows: “An integrated system of principles, methods and best practices that provides a framework to strive for excellence by continuously improving the overall organisational performance (employee results, customer results, supplier results, society results and organisation results) through leadership and management, strategic quality planning, corporate quality culture, total continuous learning, employees management, customer management, resource and partnership management and process management.”
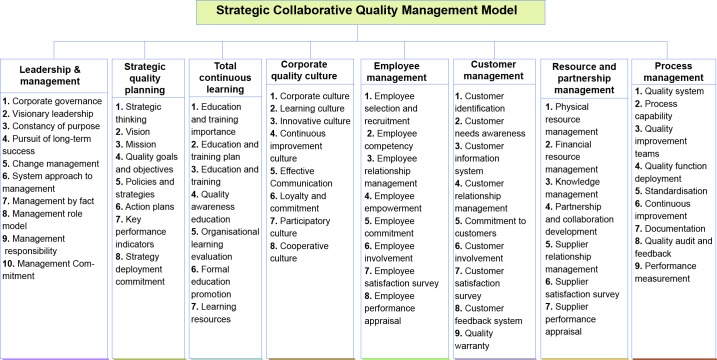
SCQM is implemented in an organisation through institutionalising a set of 67 practices that supports the SCQM core values and principles. SCQM practices are presented in Figure 4.
Figure 4.
SCQM implementation enablers
Organisational performance should be measured using a multi-dimensional approach in healthcare organisations due to the involvement of various stakeholders with different expectations. In the SCQM model, organisational performance measures are divided into five major categories and 15 sub-criteria (Figure 5.
Figure 5.
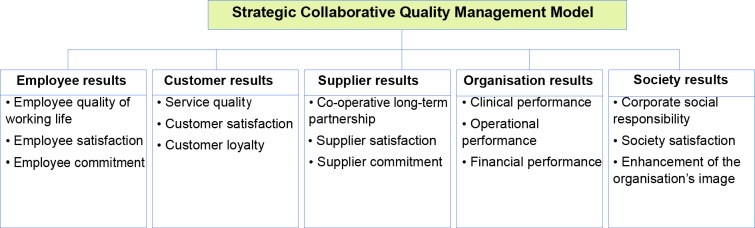
SCQM implementation results
The core values and basic principles of SCQM are the major components that guarantee its successful implementation. In order to gain the competitive advantages, the principles of SCQM should be fully understood by the entire organisation before their implementation. These core values and principles are summarised as follows:
Strategic focus: Emphasis on having a broad long-range perspective, vision, and awareness of the changes the external environment has on the organisation.
Systems view: Emphasis on analysis of the whole system producing/providing a product/service or influencing an output/outcome.
Goal-oriented: Emphasis on setting organisational goals and objectives and allocating resources to achieve goals and objectives.
Customer-centred: Emphasis on both internal and external customers’ satisfaction.
Fact-based: Emphasis on making decisions based on systematic analysis of relevant, accurate, reliable and objective data, information and knowledge.
Quality-driven: Emphasis on continuous improvement of processes and systems to support organisational goals and objectives.
Partnership-focused: Emphasis on co-operation and collaboration among people or organisations working together by sharing knowledge and technology and coordinating their activities to improve the quality of care.
People-led: Emphasis on employees, customers, suppliers and partners’ involvement in formulating, implementing and evaluating quality management programmes.
Learning-based: Emphasis on developing employees’ capabilities and enabling them to improve the quality of products/services continuously.
Balanced-measurement: Emphasis on employees, customers, suppliers and society’s satisfaction and organisational outcomes as performance measures.
To implement and gain the full potential of SCQM, its eight constructs and sixty seven practices must be implemented properly to make the greatest contribution to employees, customers, suppliers, society’s satisfaction and, finally, organisational performance. SCQM requires change in the structure, context and processes of an organisation. Creating necessary structures and assigning resources are needed to enable the change to occur and become institutionalised. SCQM also needs changes in an organisation’s culture, norms, values, political systems, decision-making processes and power sources. It requires changes in individual beliefs, attitudes and behaviours. Structural and contextual changes facilitate procedural changes, resulting in new working protocols and procedures which, in turn, result in improved quality and outcomes.
The complex nature of healthcare organisations needs a quality management programme to be practiced at four different levels: individuals, groups, organisation and surrounding environment levels (35) to achieve lasting change. Organisational change cannot occur without individual behavioural change. Initiating functional and cross-functional quality teams with enough authority, education and training, altering performance measurement and reward policies, and making specifications and requirements more explicit can help to change individuals’ behavior. At the work group level, teams should be empowered to define, manage and control the quality of their work. At the organisational level, quality management principles and values should be integrated into corporate goals and strategies, and the entire organisation must be mobilised in a systematic way to pursue corporate goals. The surrounding environment such as industry, local, national or even international society affects an individual organisation’s quality management effort. The external environment support can be through informal networking, collaboration for mutual gain, and transfer of successful practices. All four levels of change should be considered in order to maximise the probability of success.
The SCQM framework is based on three main elements: basic principles (e.g. quality culture), practices (e.g. learning culture, participative culture) and toolkits (techniques, tools and activities). The implementation of the principles and practices of SCQM are supported by techniques and tools to achieve business excellence ( Figure 6).
Figure 6.
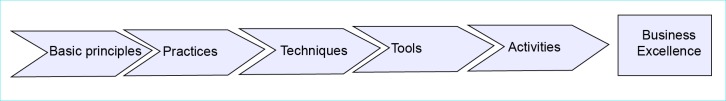
The logic of SCQM
Quality management techniques can be synergised to enhance the success of a quality management initiative (2). SCQM integrates the contents of twelve fundamental management techniques under a disciplined systematic approach focused on continuous improvement. These techniques include Quality costing, Benchmarking, Suggestion Scheme, the 5Ss, Total Productive Maintenance (TPM), Hoshin Kanri, Business Process Re-engineering (BPR), Kaizen (Continuous Quality Improvement), Clinical pathways, Six Sigma, Quality Function Deployment (QFD), Balanced Scorecard (BSC).
In the first year of implementation, the first six techniques should be implemented to develop organisational maturity and build up a culture of commitment, teamwork and discipline. In the second year of the model implementation, employees use a ten-step quality improvement approach to improve their work processes at functional and cross-functional levels. BPR, QFD, Clinical pathways, Six Sigma and Kaizen techniques are merged together in order to improve work processes based on customers’ needs, and reduce errors and mistakes rates.
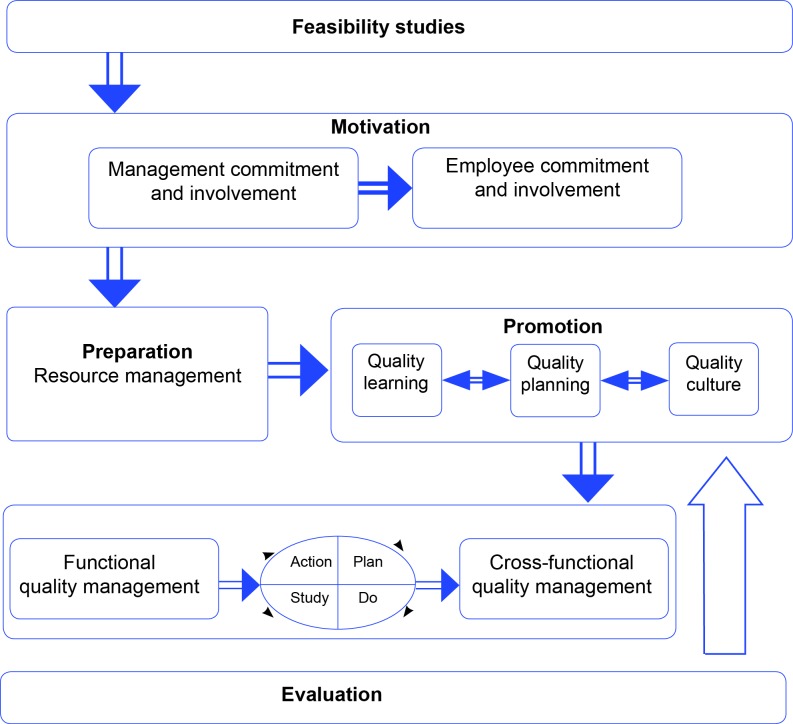
Implementation of the SCQM model consists of the following six phases: Feasibility studies, motivation, preparation, promotion, implementation and evaluation (Figure 7).
Figure 7.
A framework for implementing SCQM
Phase 0: feasibility studies
A preliminary step in SCQM implementation is to assess the current levels of organisational functioning to identify areas in need of change (Diagnostic Audit). This assessment measures the ability, readiness and the willingness of the organisation to quality management change. Organisational structures and cultures, predominant management style, communication, and managers’ and employees’ attitudes about quality improvement have a direct impact on the successful adoption of quality management practices and their sustenance over the long run. Feasibility studies help managers to develop appropriate strategies for implementing SCQM.
An organisation should be generally healthy before applying SCQM. If an organisation has significant problems such as an unstable funding base, poor management, deficient leadership, poor employee morale and serious tensions between managers and employees, SCQM implementation should be delayed until favourable conditions exist. It is likely that implementing SCQM at this time will result in even greater organisational problems.
Phase 1: motivation
An organisation’s willingness and ability to improve are necessary components of a change management programme. In this phase, the change agent must stimulate awareness towards quality management implementation. The objective of this phase is to demonstrate the responsibility of management and employees, and to ensure their commitment. Top management and the entire staff of an organisation must be committed to the improvement of quality in all aspects of their operations.
Quality costing and benchmarking techniques can be used in this phase to justify the need for quality improvement and encourage employees and managers to apply quality management to achieve competitive advantage. Quality costing also helps organisations to identify areas of poor quality and opportunities for improvement.
Phase 2: preparation (introduction)
Translating SCQM into practice requires the creation of a ‘quality structure’. SCQM proposes a five-tier quality structure, made up of a quality management council to plan and design the SCQM system, quality management department to develop quality management strategies, functional and cross-functional teams to implement SCQM within the organisation, quality steering committee to co-ordinate quality improvement initiatives, and quality audit team to evaluate quality management progress.
Phase 3: promotion
The most important phase in the implementation of SCQM is phase three. This is the phase in which the foundation for quality is built. The objectives of this phase are to develop a strategic quality plan for the organisation, to communicate strategic goals and objectives to employees, to develop employees’ knowledge, skills and capabilities, and to develop and sustain a culture of trust, teamwork and doing the right things right. The main aim of this phase is to enhance supportive constructs of SCQM (leadership and management, strategic quality planning, total continuous learning and corporate quality culture).
Hoshin Kanri and Balanced Scorecard are very useful techniques for operationalising strategic management in organisations. The main components of Hoshin Kanri and Balanced Scorecard are integrated to firstly categorise organisational goals into five strategic goals (i.e., goals related to employees, customers, suppliers, society and organisation) and secondly include continuous quality improvement into strategic goals, objectives, strategies, policies, action plans, measures and targets. This provides a balanced measure for evaluation and continuous organisational learning. Such a strategic framework creates a cause and effect chain that links performance measures with organisational strategic quality goals. In such a system, quality is not considered as a separate organisational goal. It is integrated in all organisational goals, objectives, strategies and action plans.
Suggestion Scheme, the 5Ss, and TPM are used in this phase to develop and sustain a quality culture emphasising transparency, honesty, trust, respect, effective communication, empowerment, learning, teamwork, co-ordination, innovation, customer focus and continuous improvement.
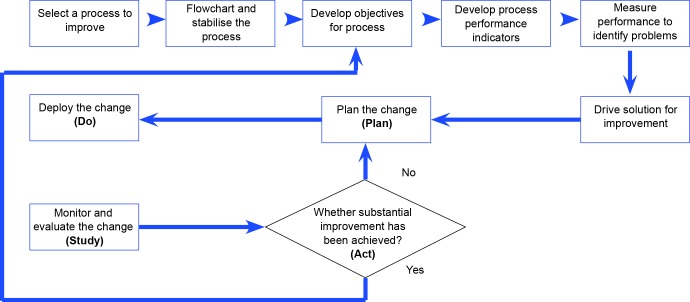
Phase 4: implementation (deployment and monitoring)
At this phase, organisation is in a position of improving processes to achieve customer satisfaction. The contents of BPR, Kaizen, Six Sigma, QFD and clinical pathways (applicable in clinical areas) techniques are integrated into a ten-step approach to process improvement. The ten-step method is a structured approach to problem solving and process improvement. It leads functional and cross-functional teams through a logical sequence of steps that requires a thorough analysis of the problem, its potential causes and possible solutions. It includes determining customer requirements, redefining and designing processes to reduce the variability and mistake rates, defining working standards and guidelines (protocols and procedures), and improving processes by using the PDSA cycle (Plan, Do, Study and Act cycle) to meet the needs of customers (both internal and external customers) effectively. The PDSA cycle describes a never-ending iterative process that is consistent with the philosophy of continuous improvement of SCQM.
Evidence-based practice is emphasised in process management activities to reduce errors and mistake rates. Tools like Pareto analysis, cause and effect analysis, the scatter diagram, check sheet, histogram, process control chart and affinity diagram can be used for process control and improvement. Figure 8 shows the ten-step approach to implementing and sustaining quality improvement activities.
Figure 8.
A ten-step approach for quality improvement
Phase 5: evaluation (development and improvement)
Evaluation and control are important components of SCQM implementation. The efficiency and effectiveness of the strategy and action plans must be monitored and adjustments made as needed. This phase emphasises a thorough self-assessment with input from employees, customers, suppliers and other stakeholders, as well as the organisation as a whole in order to see whether the stated objectives are achieved or not.
Self-assessment is a comprehensive, systematic and regular review of an organisation’s activities and results against the SCQM model. Such a formative evaluation determines the progress of SCQM implementation in the organisation and interventions and modifications needed. The SCQM model uses a 1,000-point scoring system, which can be used to assess the extent of the progress of SCQM in internal self-assessment or external accreditation (Table 2).
Table 2. Criteria and scores of SCQM model .
| Constructs | Sub-criteria | Delphi Panel’s score | Final score |
| Leadership and management | 10 | 107 | 100 |
| Strategic quality planning | 8 | 81 | 80 |
| Total continuous learning | 7 | 78 | 70 |
| Corporate quality culture | 8 | 77 | 80 |
| Employee management | 9 | 82 | 90 |
| Customer management | 9 | 86 | 90 |
| Resource and partnership management | 7 | 65 | 70 |
| Process management | 9 | 92 | 90 |
| Employee results | 3 | 68 | 80 |
| Customer results | 3 | 90 | 80 |
| Organisation results | 3 | 61 | 70 |
| Supplier results | 3 | 57 | 50 |
| Society results | 3 | 56 | 50 |
| Total Points | 82 | 1000 | 1000 |
Each of the thirteen constructs (criteria) of the SCQM model unpacks into 82 sub-criteria to assess the approach, deployment and results of the constructs within the organisation. The enablers have 67 sub-criteria used to assess the approach, deployment, and evaluation, while the results have 15 sub-criteria allowing a comparison of performances with other organisations. An assessment tool consisted of 300 questions (areas to address) was developed to evaluate an organisation’s progress in SCQM implementation. During the process of self-assessment, the strengths and weaknesses of addressed areas should be pointed out. The weak areas of the organisation’s SCQM implementation can be used to formulate improvement plans. Based on self-assessment, new areas can be selected for improvement, and so the cycle begins again. The results of self-assessment should be used for revising organisational goals and objectives. New strategies and action plans should be developed to meet revised organisational goals (formative evaluation).
The SCQM programme should also be evaluated at its completion. Therefore, management reviews of the SCQM programme must be carried out. Such a summative evaluation aims to determine the extent of achieving all the organisational goals and objectives, and the appropriateness of the SCQM programme through comparing key organisational performance indicators prior to the initiation of the SCQM programme and on its completion. Management review is necessary for addressing and correcting any problems indicated in the SCQM programme or its implementation and sustaining the quality management effort. Management reviews should be held at least once a year. There must be recognition and rewards for outstanding achievements to motivate good performance.
Four developmental stages can be considered for SCQM adoption and implementation in an organisation (Table 3). These include: orientation or awareness (stage 1), preparation (stage 2), experimentation (stage 3) and integration into organisational operations (stage 4).
Table 3. The developmental stage of the SCQM .
| Stages | Scores |
| 1. Orientation | <400 |
| 2. Preparation | 401–600 |
| 3. Experimentation | 601–800 |
| 4. Integration | 801–1000 |
Table 4 outlines briefly the SCQM Implementation. The timetable is designed for a small sized organisation. It changes based on the size of the organisation.
Table 4. The milestone in the SCQM programme implementation .
| Phases | Steps | Activity | Time (month) |
|
Phase 1
Motivation |
1 | Establish a common view that the change is needed | 1 |
| 2 | Outline the benefits of the SCQM programme for the organisation | 1 | |
| 3 | Ensure visible top managers’ commitment to quality management | 1 | |
| 4 | Ensure middle and operational managers’ commitment to quality management | 2&3 | |
| 5 | Ensure employees’ commitment and involvement to quality management | 2&3 | |
|
Phase 2
Introduction |
6 | Establish a quality management council | 4 |
| 7 | Establish a quality management department | 4 | |
| 8 | Establish functional and cross-functional quality teams | 4 | |
| 9 | Create a quality steering committee | 4 | |
| 10 | Establish internal quality audit team | 4 | |
|
Phase 3
Promotion |
11 | Analyse internal and external environments | 4–6 |
| 12 | Develop a corporate mission statement | 4–6 | |
| 13 | Develop a corporate vision statement | 4–6 | |
| 14 | Outline and clarify the guiding principles and values | 4–6 | |
| 15 | Set measurable corporate strategic goals and operational objectives | 4–6 | |
| 16 | Develop a comprehensive quality policy | 4–6 | |
| 17 | Ensure the commitment of the entire workforce to the vision, values and goals | 4–6 | |
| 18 | Develop effective strategies to achieve goals and operational objectives | 4–6 | |
| 19 | Identify key success factors for competitive advantages | 4–6 | |
| 20 | Develop policies and action plans | 4–6 | |
| 21 | Identify key performance indicators | 4–6 | |
| 22 | Making financial commitments | 4–6 | |
| 23 | Provide training and keep employees informed and get their feedback | From 6 | |
| 24 | Create a continuous improvement culture | From 6 | |
| 25 | Change the organisation’s structure in the line with the new culture | From 6 | |
|
Phase 4
Implementation |
26 | Identify and define the core and supporting processes | From 7 |
| 27 | Standardise and simplify the processes | From 7 | |
| 28 | Develop objectives for processes | From 7 | |
| 29 | Identify the key performance indicators for processes | From 7 | |
| 30 | Analyse the processes to identify opportunities for continuous improvement | From 7 | |
| 31 | Drive solution for substantial improvement | From 7 | |
| 32 | Plan the change | From 7 | |
| 33 | Deploy the plan | From 7 | |
| 34 | Study the effects of implementation | From 7 | |
| 35 | Act on the results and standardise the result | From 7 | |
|
Phase 5
Evaluation |
36 | Self-assessment | 12 |
| 37 | Develop quality goals, objectives and strategies based on self-assessment | 12 | |
| 38 | Implement quality goals, objectives and strategies | 12 | |
| 39 | Management review | 12 | |
| 40 | Recognition for achievement | 12 |
Conclusion
This study set out to develop and verify a model of quality management for healthcare organisations. A quality management model called SCQM was introduced using the findings of the fieldwork and the knowledge of the literature. The proposed model was further developed by using feedback from thirty quality management experts. Further, a guidebook for its implementation was prepared including a road map and performance measurement.
SCQM can overcome many of the pitfalls encountered in the implementation of TQM. SCQM offers a holistic and integrated approach, which can be applied to healthcare organisations to sustain the quality improvement efforts and thus to achieve organisational excellence. The proposed model establishes a link between strategic management, quality management and project management, which is considered helpful for any organisation to keep an edge over other organisations in this competitive environment.
SCQM provides a comprehensive triad of conceptual, implementation and assessment models. The SCQM conceptual model represents a set of core values and principles that focus on continuous quality improvement as a driving force in all functional areas and at all levels of the organisation. It is believed that the SCQM model is superior to the TQM models. SCQM combines principles of quality management with strategic management and project management. It includes creating the organisation’s long-range quality goals and objectives related to employees, customers, suppliers, society and organisation, developing strategies and action plans to achieve these objectives, adopting cultural change, and then allocating resources to implement the action plans. The ultimate goal of an SCQM initiative is to satisfy not only the customers, but also the employees, partners and suppliers.
Strategic management is essential to overall organisational success. Integrating quality management principles into the organisation’s strategies (strategic management) and project plans (project management) is the best way to ensure that quality management will be a way of life and an ongoing process. SCQM applies strategic change with an incremental approach that is suitable for healthcare organisations with complex processes and structures, and powerful political sub-cultures. The evolutionary nature of the change gives organisations enough time to adopt and adapt the SCQM model and improve processes gradually and continuously. It nurtures a quality culture by changing the dominant cultural variables and power relations within the organisation.
The SCQM implementation model represents the approach and sequence needed for implementing SCQM basic principles and practices. The SCQM model helps organisations to improve the quality of services continuously in a systematic way. The adoption of SCQM is dependent upon the needs and priorities of the organisation and the detail of its implementation may differ substantially. The approach to applying SCQM involves structural, cultural and procedural change. Changing structure and culture helps accelerate continuous quality improvement through procedural changes. The implementation of SCQM involves establishing quality infrastructure to include a quality management council, quality management department and quality improvement teams; developing quality goals as part of the strategic plan; adopting cultural change; and providing extensive quality-related training for all employees to manage quality through continuous improvement of well-designed processes. The logic of structural, contextual and procedural changes seems to be the best quality management implementation sequence to reach the result.
The SCQM framework is based on three main elements: basic principles, practices and toolkits. SCQM integrates the contents of fundamental management techniques under a disciplined systematic approach focused on continuous quality improvement to measure, improve and control the quality of healthcare services within a participatory framework. The main purpose of SCQM is to change the attitudes and skills of employees to do the right thing right the first time. SCQM places an emphasis on increased employee commitment, and involvement, co-operative relationship with suppliers and partners, regular measurement of the results and continuous improvement. SCQM as a strategic and planned effort enables healthcare organisations to improve their capacity to deliver efficient and effective services that are evidence-based, customer-oriented and outcome-focused.
The SCQM assessment model evaluates the approach, the implementation and the results of SCQM concepts and principles. The SCQM model is structured in 13 constructs including 82 sub-criteria and 300 questions (areas to address). Conducting assessments and using benchmarks allow organisations to assess their performance, determine the areas in need of improvement and continually improve the quality of their services.
It is hoped that the adoption of the SCQM model will offer healthcare organisations a fresh start on ‘how’ to implement a quality management programme holistically. The SCQM model represents a guide for healthcare organisations starting their quality management journey. The model serves to provide the essential requirements and the necessary actions that need to be taken by organisations to proceed with efficient and effective introduction and adoption of quality management.
Theoretical implications
This study contributes to the healthcare quality management theory especially with the absence of a context specific implementation road map. The study provides a conceptual model of implementing quality management in healthcare organisations.
Managerial implications
Managers will be able to use the proposed road map for implementing and maintaining quality management in healthcare organisations. Furthermore, a measure of quality management implementation in the health sector was developed. The development of such measure enables managers to evaluate the effectiveness of quality management interventions in enhancing organisational performance. The model can also be used as a tool for evaluating quality management maturity in an organisation.
Limitations and implications for future research
The development of the SCQM model in this study contributes to the healthcare quality management literature. However, this model needs to be validated and confirmed empirically. Quality management researchers and practitioners can measure its effectiveness by implementing its principles and practices in organisations to measure organisational performance.
Acknowledgments
The author gratefully acknowledges the reviewers for their constructive comments on earlier drafts of this paper. The author would also like to thank all quality management experts who took part in the study.
Ethical issues
This study was approved by ethics committee of Isfahan University of Medical Sciences in Iran.
Competing interests
The author declares that he has no competing interests.
Author’s contribution
AMM is the single author of the manuscript.
Citation: Mosadeghrad AM. Verification of a quality management theory: using a Delphi study. International Journal of Health Policy and Management 2013; 1: 261– 271.
References
- 1.Huq Z, Martin TN. Workforce cultural factors in TQM/CQI implementation in hospitals. Health Care Manage Rev. 2000;25:80–93. doi: 10.1097/00004010-200007000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Mosadeghrad AM. A survey of total quality management in Iran: Barriers to successful implementation in health care organisations. Leadersh Health Serv (Bradf Engl) 2005;18:xii–xxxiv. doi: 10.1108/13660750510611189. [DOI] [PubMed] [Google Scholar]
- 3.Theodorakioglou YD, Tsiotras GD. The need for the introduction of quality management into Greek health care. Total Quality Management. 2000;11:1153–65. [Google Scholar]
- 4.Mosadeghrad AM. Obstacles to TQM success in health care systems. Int J Health Care Qual Assur. 2013;26:147–73. doi: 10.1108/09526861311297352. [DOI] [PubMed] [Google Scholar]
- 5.Badrick T, Preston A. Influences on the implementation of TQM in health care organizations: professional bureaucracies, ownership and complexity. Aust Health Rev. 2001;24:166–75. doi: 10.1071/ah010166. [DOI] [PubMed] [Google Scholar]
- 6.Counte MA, Meurer S. Issues in the assessment of continuous quality improvement implementation in health care organizations. Int J Qual Health Care. 2001;13:197–207. doi: 10.1093/intqhc/13.3.197. [DOI] [PubMed] [Google Scholar]
- 7.Yang CC. The establishment of a TQM system for the health care industry. The TQM Magazine. 2003;15:93–8. [Google Scholar]
- 8.Hellstrom A, Lifvergren S, Quist J. Process management in healthcare: investigating why it’s easier said than done. Journal of Manufacturing Technology Management. 2010;21:499–511. [Google Scholar]
- 9.Nembhard IM, Alexander JA, Hoff TJ, Ramanujam R. Why does the quality of health care continue to lag? Insights from management research. Academy of Management Perspectives. 2009;23:24–42. [Google Scholar]
- 10.Ozturk AO, Swiss JE. Implementing management tools in Turkish public hospitals: the impact of culture, politics and role status. Public Adm Dev. 2008;28:138–48. [Google Scholar]
- 11.Abd-Manaf NH. Quality management in Malaysian public health care. Int J Health Care Qual Assur. 2005;18:204–16. doi: 10.1108/09526860510594767. [DOI] [PubMed] [Google Scholar]
- 12.Alexander JA, Weiner BJ, Shortell SM, Baker LC. Does quality improvement implementation affect hospital quality of care? Hosp Top. 2007;85:3–12. doi: 10.3200/HTPS.85.2.3-12. [DOI] [PubMed] [Google Scholar]
- 13.Withanachchi N, Handa Y, Karandagoda KKW, Pathirage PP, Tennakoon NCK, Pullaperuma DSP. TQM emphasizing 5-S principles: a breakthrough for chronic managerial constraints at public hospitals in developing countries. International Journal of Public Sector Management. 2007;20:168–77. [Google Scholar]
- 14.Mosadeghrad AM. The impact of organisational culture on the successful implementation of total quality management. The TQM Magazine. 2006;18:606–25. [Google Scholar]
- 15.Mosadeghrad AM. Towards a theory of quality management: an integration of strategic management, quality management and project management. International Journal of Modelling in Operations Management. 2012;2:89–118. [Google Scholar]
- 16.Godfrey G, Dale B, Marchington M, Wilkinson A. Control: a contested concept in TQM research. International Journal of Operations & Production Management. 1997;17:558–73. [Google Scholar]
- 17. Flood R. Beyond TQM. New York: John Wiley & Sons; 1993.
- 18.Gotzamani KD, Tsiotras GD. An empirical study of the ISO 9000 standards’ contribution towards total quality management. International Journal of Operations & Production Management. 2001;21:1326–42. [Google Scholar]
- 19. European Foundation for Quality Management, 2010. EFQM Excellence model [internet]. [cited 2013 October 1]. Available from: http://www.efqm.org/the-efqm-excellence-model.
- 20. NIST [homepage on the Internet]. [cited 2009 June 25]. Criteria for Performance Excellence, Baldrige National Quality Program. Available from: http://www.baldrige.nist.gov/PDF_files/2009_2010_Business_Nonprofit_Criteria.pdf.
- 21.Claver E, Tari JJ, Molina JF. Critical factors and results of quality management: an empirical study. Total Quality Management. 2003;14:91–118. [Google Scholar]
- 22.Hansson J, Klefsjo B. A core value model for implementing total quality management in small organisations. The TQM Magazine. 2003;15:71–81. [Google Scholar]
- 23.Seetharaman A, Sreenivasan J, Boon LP. Critical success factors of total quality management. Qual Quant. 2006;40:675–95. [Google Scholar]
- 24.Taylor WA, Wright GH. A longitudinal study of TQM implementation: Factors influencing success and failure. Omega. 2003;31:97–111. [Google Scholar]
- 25.Jennings K, Westfall F. A survey-based benchmarking approach for health care using the Baldridge quality criteria. Jt Comm J Qual Improv. 1994;20:500–9. doi: 10.1016/s1070-3241(16)30096-7. [DOI] [PubMed] [Google Scholar]
- 26.Moeller J. The EFQM Excellence ModelGerman experiences with the EFQM approach in health care. Int J Qual Health Care. 2001;13:45–9. doi: 10.1093/intqhc/13.1.45. [DOI] [PubMed] [Google Scholar]
- 27. NIST [homepage on the Internet]. [cited 2009 June 25]. Health Care Criteria for Performance Excellence, Baldrige National Quality Program. Available From: http://www.baldrige.nist.gov/PDF_files/2009_2010_HealthCare_Criteria.pdf.
- 28. Holloway NM. Medical-surgical care planning. Philadelphia: Lippincott Williams & Wilkins; 2004.
- 29.Baidoun S, Zairi M. A proposed model for TQM implementation in the Palestinian context. Total Quality Management and Business Excellence. 2003;14:1193–211. [Google Scholar]
- 30.Ghobadian A, Gallear D. TQM implementation: an empirical examination and proposed generic Model. Omega. 2001;29:343–59. [Google Scholar]
- 31.Jackson S. Successfully implementing total quality management tools within healthcare: What are the key actions? Int J Health Care Qual Assur. 2001;14:157–63. [Google Scholar]
- 32. Leebov W, Jean C, Ersoz CJ. The health care manager’s guide to continuous quality improvement. Lincoln: iUniverse; 2003.
- 33. Oakland JS. Total quality management: Text with cases. 3rd ed. Oxford: Butterworth-Heinemann; 2003.
- 34.Ruiz U, Simon J. Quality management in healthcare: a 20-year journey. Int J Health Care Qual Assur. 2004;17:323–33. doi: 10.1108/09526860410557570. [DOI] [PubMed] [Google Scholar]
- 35.Ferlie EB, Shortell SM. Improving the quality of health care in the United Kingdom and the United States: A framework for change. Milbank Q. 2001;79:281–315. doi: 10.1111/1468-0009.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]