Abstract
Objectives
Subthreshold Depression (StD) is common in older adults and is associated with poor self-rated health. However, the impact of StD on broader indicators of successful aging, such as positive psychological constructs, cognitive functioning, or quality of well-being, has not been assessed. We compared persons with scores above and below a predetermined threshold on the Center for Epidemiological Studies Scale for Depression (CESD) to non-depressed persons (ND) on measures of multiple domains associated with successful aging.
Design
Cross sectional survey-based psychological assessments.
Participants
1,979 community-dwelling older women participating in the Women’s Health Initiative study.
Measurements
ND was defined as a CESD score below 8, StD as a score between 8 and 15, and CESD Depression (CD) as a score of 16 or above. The study questionnaire consisted of multiple self-reported measures of positive psychological functioning (e.g., optimism, resilience), cognitive functioning and complaints, and quality of well-being. We also obtained a history of diagnosis, treatment, and hospitalization related to mental health problems.
Results
20.2% of women met CES-D criteria for StD and 7% for CD. Women with StD had worse self-rated successful aging, worse physical and emotional functioning, lower optimism, more negative attitudes toward aging, lower personal mastery and self-efficacy, and greater anxiety and hostility than ND women, but scored better on all these measures than women with CD. StD subjects also had higher self-reported rates of previous diagnosis, treatment, and hospitalization for mental health problems than the ND group. StD subjects with depressed mood and/or anhedonia were largely similar to those without these symptoms.
Conclusions
Mild-moderate levels of depressive symptoms that likely fall under a general category of StD were common, and were associated with worse functioning on virtually every component of successful aging that we examined. StD represents a clinical entity that may affect the longitudinal course of successful aging for large numbers of persons and is a potential target for clinical intervention.
Introduction
Among older adults, clinically significant depressive symptoms manifest more commonly in forms that do not meet criteria for major depressive disorder (MDD) (1). In various studies, these nonmajor forms of depression have been labeled as ‘subthreshold depression’ (StD) (2;3) ‘subsyndromal depression’ (4;5), or ‘minor depression’ (1). The prevalence of such nonmajor forms of depression varies across studies, depending upon sampling methods and diagnostic criteria used; community point prevalence estimates among older adults range from 8.8% (6) to 21.3% (7). Presence of nonmajor types of depression is associated with increased healthcare utilization, risk of future MDD, suicide, and disability (e.g., more days in bed, worse general well-being, and more activity limitations) (3;8–10). Studies focusing on older adults with nonmajor depression have also shown its association with declines in overall functioning and health (e.g. poor psychosocial functional status, high medical burden, low global and domain-specific quality of life) (1;11–13). However, the relationship between depressive symptoms and other indicators of health and well-being in later life, as would be subsumed under the framework of successful aging (e.g., personal control, optimism) have not been examined. We (14), and others (15;16) have reported that absence of depression is a significant predictor of self-rated successful aging. However, the relationship of nonmajor forms of depression to a broad spectrum of measures of successful aging has not been studied.
There has been some variability in operationalization and nomenclature of nonmajor forms of depression in previous studies. Judd and colleagues (4), defined the term ‘subsyndromal depression’ to describe presence of two or more current symptoms of depression present most of the time for a period of at least 2 weeks in persons not meeting criteria for dysthymic disorder, major depression, or minor depressive disorder. In subsequent studies, they have broadened this definition to include persons who had just one or more symptoms of depression (9). This definition implies that depressed mood and anhedonia (the “Criterion A” symptoms from DSM-IV-TR (17) criteria for MDD) are not necessary for diagnosing subsyndromal depression. On the other hand, some studies have required some level of Criterion A symptoms in their definitions of subsyndromal depression (12;18). Lyness and colleagues (12) have demonstrated that among persons with various definitions of ‘subsyndromal depression’, presence of Criterion A symptoms (depressed mood and anhedonia) were associated with a negative impact on functioning. In studying associations between nonmajor depression and outcomes related to successful aging, it would thus be useful to assess whether there is a difference in findings based on whether the definitions include Criterion A symptoms (i.e. meet criteria for minor depression). To understand the utility of these classification strategies, cross-validation against other measures of health and well-being is needed. In addition, among older adults with MDD, utilization of mental healthcare is lower than that among younger adults (19).
There is no single consensus definition of successful aging (16). Several reviews of the literature have identified a variety of components believed to be important to this concept. The most commonly employed criteria for successful aging include an absence of physical disease and disability, as well as preserved cognitive functioning (16). Interestingly, emotional and psychological aspects of successful aging have not received as much attention. However, integrating results from previous research, there are several psychological aspects believed to be important in facilitating successful aging, such as mastery, self-efficacy, and resilience (20). Yet, a notable deficit in past research on successful aging relates to a measurement of self-perceived successful aging. Given the potential impact of depressive symptoms on various psychological measures including self-rated successful aging, an examination of the impact of major and nonmajor forms of depression on successful aging seems warranted.
In this study we assessed depressive symptoms using the Center for Epidemiological Studies Depression scale (CESD) - a self-rated measure of depressive symptoms (described in the Methods section). The terms MDD and ‘subsyndromal depression’ are established clinical entities with clearly defined diagnostic criteria. Since our evaluation of depression is based on a scale and not clinical assessment, we use the term ‘CESD depression’ (CD) as a proxy for MDD and subthreshold depression (StD) as a proxy for ‘subsyndromal depression’ in this paper. These terms have previously been used to label depressive syndromes assessed by CESD (2;21). We measure prevalence of StD and its association with measures related to successful aging identified in previous work (16), in a community-dwelling sample of older women enrolled at the San Diego site of the NIH-funded Women’s Health Initiative (WHI) study. Next, we compared women with StD and CD, and non-depressed (ND) women on these measures as well as on reported history of diagnosis, medication or other treatment, and hospitalization for a mental or emotional problem. Finally, in the StD group, we explored differences between women with depressed mood and/or anhedonia and those without either of these symptoms. Our a priori hypotheses were that: (1) On measures of successful aging, persons with StD would score worse than the ND group, but better than those with CD. (2) A greater proportion of the StD group would report past diagnosis, treatment (including medications), and hospitalization related to mental health problems than the ND group.
Methods
Participants and Procedures
Study participants came from the San Diego clinical center of the WHI, a large NIH-funded multi-center study of the predictors of morbidity and mortality among post-menopausal women (22) who were followed for an average of seven years between 1994 and 2005. A detailed description of the WHI methodology is available in prior publications (23). In general, potential subjects were excluded if they did not plan to reside in the area for at least 3 years, had medical conditions predictive of survival less than 3 years, or had complicating conditions such as substance use disorders. The WHI investigation included an observational study (OS) and three separate clinical trials (CTs), involving hormone replacement therapy, dietary modification, and calcium/vitamin D supplementation
At their final study visit, San Diego WHI subjects were invited to participate in a study of successful aging. To enroll, women were either consented at their final clinic visit (for CT participants) or mailed the questionnaire and consent form (for OS participants). The following analysis is based on a sample of 1,979 English-speaking women who returned the surveys with a signed consent form and were ≥ 60 years old. Of these respondents, 1,089 were enrolled in the OS and 890 were enrolled in one of the CTs.
This study was approved by the Institutional Review Board of the University of California, San Diego. All study participants provided a written informed consent.
Data Collection
Demographics
Apart from the participants’ age (current at the time of survey), other demographic information including educational attainment, marital status, and ethnicity was obtained from the baseline (enrollment) visit of the WHI study (between 1994 and 1998).
Measures of depression
Depression was measured using the Center for Epidemiological Studies Scale for Depression (CES-D) (24). Based on previous reports in literature (25) we defined probable StD as a score between 8 and 15 on the CES-D, and probable CD as a score of ≥ 16. CD as defined by a CES-D cutoff of ≥ 16 has been shown to correspond adequately with a clinical diagnosis of MDD (23). As a proxy for depressed mood and anhedonia, we developed an index of ‘recent depression’ and ‘reduced enjoyment of life’ based on specific CESD items. Recent depression was defined as ‘experiencing depressed mood’ 3–4 times a week or more often. And reduced enjoyment of life was defined as reporting of ‘enjoyment of life’ 1–2 times a week or less frequently.
Measures related to Successful Aging
The survey questionnaire on successful aging used in this study was a slightly revised version of the one we used in an earlier investigation of resilience in older women in San Diego County (20). Briefly, participants rated their own level of successful aging on a 10-point Likert scale, with 1 being least successful and 10 most successful (14). Physical and mental health-related functioning and quality of life were measured using the MOS-RAND SF-36 scale (26). Attitude toward aging, personal mastery, and self-efficacy were evaluated with the Philadelphia Geriatric Morale Scale (PGMS) (27), Personal Mastery Scale (28) and Self-Efficacy Scale (29), respectively. Optimism was assessed using the Life Orientation scale (30), and resilience with the Connor-Davidson Resilience Scale (CD-RISC) (31). We employed the Cognitive Failures Questionnaire (CFQ) (32) and Cognitive Assessment Screening Test (CAST) (33) to evaluate subjective complaints and test-based cognitive performance (respectively), and subscales of the Brief Symptom Inventory (BSI) (34) to assess anxiety and hostility.
History and management of mental/emotional problems
History of diagnosis or management of mental health problems was evaluated using four self-report Yes/No items, asking if the participant had ever been “diagnosed with a mental or emotional problem”, ever been “in treatment with a mental health professional”, ever been “prescribed medication for a mental or emotional problem”, or ever been “hospitalized for such a problem.”
Statistical Analysis
Demographic data were compared across the subgroups defined by depression status through the use of F-tests for continuous data and chi-square tests for categorical data. We also examined depression status differences in self-reported diagnosis, treatment, medication, and hospitalization history by performing chi-square tests. We used Fisher exact tests when the usual asymptotic conditions for chi-square distribution were not met. Results for all 5 demographic variables and for all 4 diagnosis/treatment variables were separately Bonferroni-adjusted to control for multiple comparisons. Pairwise chi-square tests were performed on the diagnosis/treatment variables if significant differences were found on the full contingency table.
We performed univariate ANOVAs with the 13 successful aging-related outcome measures as dependent variables and with depression classification (ND, StD, and CD) as the independent variable. Because the data were not normally distributed (as determined by Shapiro-Wilk tests (35) we employed Kruskal-Wallis (K-W) ANOVAs, with follow-up Mann-Whitney (M-W) U tests for pairwise comparisons if there was a significant difference in outcomes across the three depression classifications. Results of significance for the 13 ANOVAs were Bonferroni-adjusted to control for multiple comparisons.
Finally, we explored differences in successful aging related measures between StD participants with and without depressed mood or reduced enjoyment of life. This was done through M-W U tests with these two StD categories as the independent variable. As before, results were Bonferroni-corrected.
All analyses were performed in the R statistical language, (R Version 2.6.2).
Results
The study sample consisted of 1,979 women aged 60–91 years (mean=73, Std Dev=7.4). Over four-fifths (84%) of the participants had completed high school, and 43% had at least some college education. Most of the participants (91%) were Caucasian, and 63% were married. Sixty-six percent had a mean annual household income of $35,000 or greater. Overall, 401 women (20.3%) met our criteria for StD, and 137 (7%) for CD (Table 1). StD and CD groups were older than the ND group; the three groups did not differ significantly in the level of education, average household income, ethnicity, or marital status. 389 (19.1%) of the 1,979 women did not have CESD scores as some or all CESD items were missing. We performed sensitivity analyses by multiple-imputation of these missing items (36) and fitting the ANOVA models on successful aging-related measures for each imputation. As these additions resulted in little change from the analyses of complete responders only, we report results for the complete responders only below.
TABLE 1.
Comparison of No Depression (ND), Subthreshold Depression (StD), and CESD Depression (CD) Groups on Demographic Variables
| Variable | Subject Group | χ2/F | Df | p | ||
|---|---|---|---|---|---|---|
| Non Depressed (ND) N=1,081 |
Subthreshold Depression (StD) N=401 |
Clinical Depression (CD) N=137 |
||||
| Age (Mean) in years * | 72.1 | 73.8 | 73.7 | F=9.4 | 2,1616 | <0.001 |
| Education + | χ2=15.5 | 8 | 0.05X | |||
| No high school diploma | 20 (2%) | 11 (3%) | 6 (4%) | |||
| High school diploma/GED | 114 (11%) | 41 (10%) | 17 (12%) | |||
| Some college | 446 (41%) | 174 (44%) | 68 (50%) | |||
| College graduate/Baccalaureate | 112 (10%) | 53(13%) | 10 (7%) | |||
| Some post graduate education | 385 (36%) | 120 (30%) | 36 (26%) | |||
| Missing Information a | 4 (<1%) | 2 (<1%) | 0 (0%) | |||
| Annual Household Income + | χ2=17.1 | 8 | 0.03 X | |||
| <=$20,000 | 104 (10%) | 51 (13%) | 25 (18%) | |||
| $20,000 – $34,999 | 217 (20%) | 70 (18%) | 33 (24%) | |||
| $35,000 – $49,999 | 218 (20%) | 85 (21%) | 29 (21%) | |||
| $50,000 – $74,999 | 276 (26%) | 91 (23%) | 24 (18%) | |||
| ≥ $75,000 | 230 (21%) | 80 (20%) | 22 (16%) | |||
| Missing Information a | 36 (3%) | 24 (6%) | 4 (3%) | |||
| Race/Ethnicity + | χ2=0.6 | 2 | 0.73 | |||
| White | 990 (92%) | 357 (89%) | 124 (91%) | |||
| Non-White | 68 (6%) | 29 (7%) | 10 (7%) | |||
| Missing Information a | 23 (2%) | 15 (4%) | 3 (2%) | |||
| Marital status + | χ2=14.6 | 8 | 0.07 | |||
| Married | 653 (60%) | 253 (64%) | 73 (53%) | |||
| Widowed | 152 (14%) | 69 (17%) | 27 (20%) | |||
| Live-in relationship | 20 (2%) | 10 (3%) | 4 (3%) | |||
| Divorced | 221 (20%) | 55 (14%) | 28 (20%) | |||
| Never married | 32 (3%) | 9 (2%) | 5 (4%) | |||
| Missing Information a | 3 (<1%) | 5 (1%) | 0 (0%) | |||
For continuous variables, descriptive values are means (standard deviation) and the test statistic is F.
For categorical variables, descriptive values are sample counts (N (with %)) and the test statistic is χ2
Persons with missing information were not included in the Chi-square analyses.
Comparison is not significant after Bonferroni correction.
K-W ANOVAs demonstrated significant differences at the Bonferroni-corrected .05-level among the 3 groups for comparisons on all measures of successful aging as well as measures of cognitive function, anxiety, and hostility (Table 2) with the exception of CAST. Follow-up M-W U-tests (Table 2) showed that, compared to the ND group, StD subjects had lower self-rated successful aging, lower physical and mental health composite scores on the MOS SF-36, less positive attitudes toward aging on the PGMS, lower scores for resilience (CD-RISC), self-efficacy, personal mastery, and optimism (Life Orientation scale), as well as a greater number of cognitive complaints on the CFQ and lower scores on the CAST. StD subjects also had higher scores on the BSI anxiety and hostility scales than ND subjects. In comparison to the CD group, however, the StD group had higher self-rated successful aging, higher scores on the SF36, PGMS, CD-RISC, Self Efficacy Scale, Personal Mastery scale and Life Orientation scale, and lower scores on the CFQ, and the anxiety and hostility subscales of the BSI. Cohen’s D estimates for comparing ND and StD groups ranged from .24 to .71 (median .52), estimates comparing ND and CD groups ranged from .31 to 1.95 (median 1.16), and for comparing StD to CD groups ranged from .10 to 1.19 (median .57).
Table 2.
Comparison of No Depression (ND), Subthreshold Depression (StD), and CESD Depression (CD) Groups on Measures Related to Successful Aging
| Measure (possible range) |
ND N=1,081 |
StD N=401 |
CD N=137 |
ND:StD:CD | ND:StD | ND: CD | StD: CD |
|---|---|---|---|---|---|---|---|
| Mean (Std dev) |
Mean (Std dev) |
Mean (Std dev) |
K-W: χ2 (2 df) |
t | M-W: U | MW: U | |
| Self rated successful aging (1–10) a | 8.5 (1.1) | 7.9 (1.3) | 6.7 (2.0) | 92.4* | −4.29 * | 36728* | 11551* |
| SF36 - Physical functioning (1–100) a | 45.4 (10.7) | 40.7 (11.4) | 37.7 (12.5) | 55.9* | −7.32 * | 32807* | 10160 |
| SF36 - Mental/emotional functioning (1–100) a | 58.9 (4.6) | 55.1 (7.2) | 45.0 (10.5) | 164.9* | −12.09 * | 41570* | 13573* |
| SF36 - Social functioning (1–100) a | 94.0 (12.9) | 85.6 (18.8) | 66.7 (25.7) | 147.7* | −9.70 * | 38404* | 12258* |
| Attitude toward Aging (PGMS) (0–5) a | 4.2 (1.0) | 3.4 (1.8) | 2.4 (1.7) | 130.7* | −12.05 * | 38050* | 11361* |
| Personal Mastery: PMS (7–28) a | 15.8 (3.3) | 13.9 (3.0) | 11.7 (3.3) | 126.7* | 10.61* | 7867* | 5305* |
| Self-Efficacy: SES (8–32) a | 25.0 (3.0) | 23.6 (2.9) | 22.0 (2.7) | 71.7* | −8.10 * | 35399* | 10930* |
| Optimism: LOS (6–30) a | 25.1 (2.9) | 23.5 (3.1) | 21.2 (3.6) | 102.2* | −9.42 * | 38607* | 12348* |
| Resilience: CD-RISC (0–100)a | 79.1 (11.1) | 71.7 (12.5) | 63.4 (14.7) | 113.4* | −10.01 * | 36986* | 10916* |
| Cognition: CFQ (20–100) b | 24.1 (8.0) | 28.7 (7.8) | 33.5 (10.1) | 102.9* | 9.60 * | 10871* | 6401* |
| Cognition: CAST ( 0–21) a | 18.8 (2.0) | 18.3 (2.3) | 18.0 (2.5) | 7.9 | −3.87 * | 25976 | 8611 |
| BSI Anxiety Scale (0–24) b | 0.8 (1.3) | 1.8 (2.4) | 4.2 (4.6) | 81.3* | 9.81 * | 12184* | 6116* |
| BSI Hostility Scale (0–20) b | 0.6 (1.0) | 1.2 (1.6) | 1.9 (2.1) | 69.5* | 7.93 * | 12572* | 6346* |
p<0.004
Higher scores indicate better functioning
Higher scores indicate worse functioning
Non Depressed (ND) = CESD <8
Subthreshold Depression (StD) = CESD between 8 and 15
CESD Depression (CD) = CESD ≥16
Abbreviations:
K-W = Kruskal-Wallis χ2 test
M-W = Mann-Whitney U test
CES-D = Center for Epidemiological Studies Scale for Depression;
PGMS = Philadelphia Geriatric Morale Scale; PMS = Personal Mastery Scale;
LOS = Life orientation Scale; CD-RISC = Connor Davidson Resilience Scale;
CFQ = Cognitive Failures Questionnaire; CAST = Cognitive Assessment Screening Test;
BSI = Brief Symptom Inventory
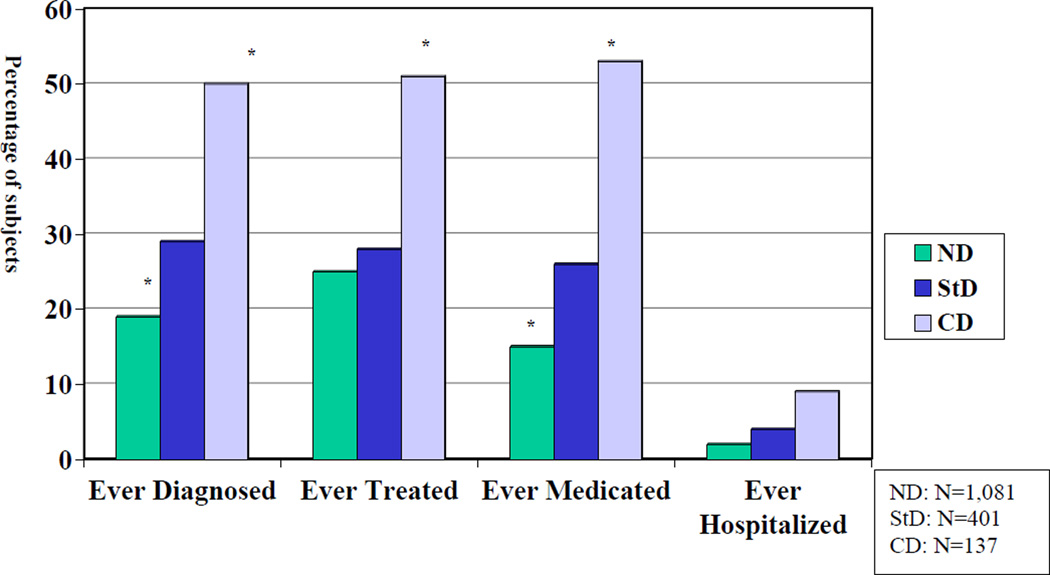
In terms of diagnosis and management of mental or emotional problems (Figure 1), all 4 measures were significantly different across the three subgroups after Bonferroni adjustment (diagnosis: χ2=70.5, df=2,p<.001; treatment ever: χ2=32.0,df=2,p<.001; medication ever χ2=107.9, df=2,p<.001; and hospitalization ever: χ2=21.3,df=2,p<.001). Post-hoc pairwise tests showed that a higher percentage of the StD group reported a history of diagnosis (χ2=16.6,df=1,p<.001) and medication prescription (χ2=20.2, df=1,p<.001) than the ND group. However, the percentages of the CD group reporting positive history for all of these measures were higher than those in the StD group (see Figure 1). (diagnosis ever: χ2=18.9,df=1,p<.001; treatment ever: χ2=17.7,df=1,p<.001; medication ever: χ2=32.3,df=1,p<.001; and hospitalization ever: χ2=3,3,df=1,p=.07).
Figure 1. History of Diagnosis/Treatment/Hospitalization for Mental or Emotional Problem.
* p <0.001 in comparison to StD group
Chi-square tests were used for all comparisons
df = 1 for all comparisons.
Within the StD group we compared the women with versus without recent depression and reduced enjoyment of life. Of the 401 persons in the StD group, 307 (77%) had not experienced either symptom while 94 (23%) reported recent depression or reduced enjoyment of life or both. Persons with either/both of these symptoms had significantly higher scores on the CD-RISC (M-W U=7465, p=0.001) and CAST (M-W U=16829, p=0.007, p=0.003) than those without either symptom. The groups did not differ on other measures.
Discussion
In this study, StD was nearly three times more prevalent (20.2%) than CD (7%) in a large sample of community-dwelling older women. This prevalence of StD is within the range of 8.8% (6) to 21.3% (7) reported in published studies of point prevalence among community-dwelling samples, but near the higher end. This relatively high prevalence may be due, in part, to our definition of StD (using an intermediate score on the CES-D) as well as the inclusion of only female participants. Previous studies among older adults have consistently reported a preponderance of women compared to men meeting different definitions of StD (2;6;37;38).
We confirmed our hypothesis that women with StD would have worse scores on measures of successful aging than ND subjects, but better scores than those with CD. Notably, women with StD scored worse on nearly all of the measures related to successful aging than those with ND, but better than those with CD. Our findings are consistent with the results reported by previous investigators (4) regarding greater functional disability among persons with StD compared to the ND group, but add to the literature by including previously unreported important outcomes related to the association of StD with worse performance on a broad spectrum of domains associated with of successful aging. Although there is no consensus definition of successful aging, its components in previous research have included positive psychological traits (e.g., optimism, resilience), high cognitive resources, and emotional well-being (16;39). While we cannot rule out the negative response biases produced by depression on self-report measures, our findings suggest that even low levels of depression seem to have a marked and diffuse impact on a variety of indicators of successful aging. Independent associations between low optimism and cardiac mortality (40), as well as worse attitudes toward aging and poorer functional health/will to live (41;42) have been identified. The extent to which depressive symptoms moderate these relationships should be a focus of further study.
StD was associated with higher historical self-reported rates of diagnosis, medication use, and hospitalization for mental/emotional problems than the rates among ND subjects but lower rates than in subjects with CD. Therefore, our results support the external validity of StD, and also support the concept of depression as an illness existing on a spectrum, insofar as StD was associated with impairments intermediate between those seen in ND and CD.
Finally, although there were differences on measures of cognition and resilience between the two groups, the majority of comparisons between these groups did not yield significant differences, which is consistent with a recent report of more similarities than differences when comparing three different definitions of subsyndromal depression (12). This finding highlights the importance of clinical management of even mild depression spectrum disorders in late life (43).
The adverse outcomes in functioning and successful aging among women with StD (compared to those with ND), in conjunction with lower use of mental healthcare among women with StD (compared to those with CD) have clinical relevance. While women with StD are more disabled and aging less successfully than those without depressive symptoms, there seems to be a lack of adequate recognition and treatment of this condition. In vigilant detection and clinical management of StD there may exist an opportunity to reduce morbidity and enhance the prospect of successful aging. Other researchers (25;44) have demonstrated how underlying StD may complicate outcomes in a variety of psychiatric disorders, but our findings suggest that this issue is not confined merely to persons with identified mental illness, and warrants increased recognition of StD among older adults in primary care settings.
There are several limitations to this investigation. All of our subjects were women, most of whom were Caucasian, and the median level of educational attainment was relatively high. Furthermore, the study was cross-sectional, and thus, any conclusions about the impact of StD on domains related to successful aging are likely to be confounded by cohort effects and characteristics of sample collection. The study design also limits our ability to comment on causal relationships between depressive symptoms and domains of successful aging. Future longitudinal study would be needed to determine whether StD predicts functional decline or visa versa. Another study limitation is that the history of diagnosis and management of mental and emotional problems was based on self-report, and not corroborated by review of records or examination, leading to a possibility of recall bias. Similarly, the independent variables in our study were also measured by self-report, which may be biased by social desirability (45). On the other hand, our large sample size and use of published measures are strengths of this investigation. While our categorization of CD and StD was based on CES-D scores and not diagnostic interviews, several previous authors have reliably measured StD and other forms of minor depression using cut-off scores on depression rating scales, in lieu of structured interview-based clinical diagnosis (12;25;46). While some participants might have been categorized differently in clinical interviews than they were on the basis of CES-D scores, the overall message is still consistent with the notion that depressive symptomatology exists on a spectrum, and that even persons with depressive symptoms who do not meet the criteria for CD are often disabled and distressed, and require increased clinical attention.
In summary, even mild-moderate levels of depressive symptoms that likely fall under a general category of StD were associated with worse functioning on virtually every component of successful aging that we examined. Given the high prevalence of StD in comparison to CD, and the historically low rates of detection and treatment of even late-life MDD in primary care settings (47), StD represents an entity that merits clinical vigilance and may be a possible target for improving longitudinal course of successful aging.
Acknowledgments
This work was supported, in part, by the Sam and Rose Stein Institute for Research on Aging, John A. Hartford Foundation's Center of Excellence in Geriatric Psychiatry, National Institute of Mental Health grants (MH071536, T32 MH019934-12 and P30 MH080002-01), and by the Department of Veterans Affairs.
We thank Shahrokh Golshan, Ph.D., Ian Fellows, M.S., and Rebecca Daly for their invaluable assistance with the data management and analysis.
References
- 1.Lyness JM. Naturalistic outcomes of minor subsyndromal depression in older primary care patients. Int J Geriatr Psychiatry. 2008;23:773–781. doi: 10.1002/gps.1982. [DOI] [PubMed] [Google Scholar]
- 2.Hybels C, Blazer D, Pieper C. Toward a threshold for subthreshold depression: An analysis of correlates of depression by severity of symptoms using data from an elderly community survey. Gerontologist. 2001;41:357–365. doi: 10.1093/geront/41.3.357. [DOI] [PubMed] [Google Scholar]
- 3.Judd LL, Schettler PJ, Akiskal HS. The prevalence, clinical relevance, and public health significance of subthreshold depressions. Psychiatr Clin North Am. 2002;25:685–698. doi: 10.1016/s0193-953x(02)00026-6. [DOI] [PubMed] [Google Scholar]
- 4.Judd LL, Rapaport MH, Paulus MP, et al. Subsyndromal symptomatic depression: a new mood disorder? J Clin Psychiatry. 1994;55(Suppl):18–28. [PubMed] [Google Scholar]
- 5.Cohen CI, Magai C, Yaffee R, et al. Racial differences in syndromal and subsyndromal depression in an older urban population. Psychiatr Serv. 2005;56:1556–1563. doi: 10.1176/appi.ps.56.12.1556. [DOI] [PubMed] [Google Scholar]
- 6.Chen CS, Chong MY, Tsang HY. Clinically significant non-major depression in a community-dwelling elderly population: epidemiological findings. Int J Geriatr Psychiatry. 2007;22:557–562. doi: 10.1002/gps.1714. [DOI] [PubMed] [Google Scholar]
- 7.Schoevers RA, Smit F, Deeg DJ, et al. Prevention of late-life depression in primary care: do we know where to begin? Am J Psychiatry. 2006;163:1611–1621. doi: 10.1176/ajp.2006.163.9.1611. [DOI] [PubMed] [Google Scholar]
- 8.Judd LL. Adverse outcome of subsyndromal and syndromal levels of depressive symptom severity. Psychosom Med. 2000;62:472–473. doi: 10.1097/00006842-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Judd LL, Akiskal HS, Maser JD, et al. A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Arch Gen Psychiatry. 1998;55:694–700. doi: 10.1001/archpsyc.55.8.694. [DOI] [PubMed] [Google Scholar]
- 10.Lyness JM, King DA, Cox C, et al. The importance of subsyndromal depression in older primary care patients: Prevalence and associated functional disability. Journal of American Geriatric Society. 1999;47:647–652. doi: 10.1111/j.1532-5415.1999.tb01584.x. [DOI] [PubMed] [Google Scholar]
- 11.Lyness JM, Heo M, Datto CJ, et al. Outcomes of minor subsyndromal depression among elderly patients in primary care settings. Ann Intern Med. 2006;144:496–504. doi: 10.7326/0003-4819-144-7-200604040-00008. [DOI] [PubMed] [Google Scholar]
- 12.Lyness JM, Kim J, Tang W, et al. The clinical significance of subsyndromal depression in older primary care patients. Am J Geriatr Psychiatry. 2007;15:214–223. doi: 10.1097/01.JGP.0000235763.50230.83. [DOI] [PubMed] [Google Scholar]
- 13.Chachamovich E, Fleck M, Laidlaw K, et al. Impact of major depression and subsyndromal symptoms on quality of life and attitudes toward aging in an international sample of older adults. Gerontologist. 2008;48:593–602. doi: 10.1093/geront/48.5.593. [DOI] [PubMed] [Google Scholar]
- 14.Montross LP, Depp C, Daly J, et al. Correlates of self-rated successful aging among community-dwelling older adults. Am J Geriatr Psychiatry. 2006;14:43–51. doi: 10.1097/01.JGP.0000192489.43179.31. [DOI] [PubMed] [Google Scholar]
- 15.Ko KJ, Berg CA, Butner J, et al. Profiles of successful aging in middle-aged and older adult married couples. Psychol Aging. 2007;22:705–718. doi: 10.1037/0882-7974.22.4.705. [DOI] [PubMed] [Google Scholar]
- 16.Depp CA, Jeste DV. Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. Am J Geriatr Psychiatry. 2006;14:6–20. doi: 10.1097/01.JGP.0000192501.03069.bc. [DOI] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- 18.McAvay GJ, Bruce ML, Raue PJ, et al. Depression in elderly homecare patients: patient versus informant reports. Psychol Med. 2004;34:1507–1517. doi: 10.1017/s0033291704002582. [DOI] [PubMed] [Google Scholar]
- 19.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 20.Lamond AJ, Depp CA, Allison M, et al. Measurement and predictors of resilience among community-dwelling older women. J Psychiatr Res. 2008 Apr 30; doi: 10.1016/j.jpsychires.2008.03.007. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hybels CF, Pieper CF, Blazer DG. The complex relationship between depressive symptoms and functional limitations in community-dwelling older adults: the impact of subthreshold depression. Psychol Med. 2009;9:1–12. doi: 10.1017/S0033291709005650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Langer RD, White E, Lewis CE, et al. The Women's Health Initiative Observational Study: baseline characteristics of participants and reliability of baseline measures. Ann Epidemiol. 2003;13:S107–S121. doi: 10.1016/s1047-2797(03)00047-4. [DOI] [PubMed] [Google Scholar]
- 23.The Women's Health Initiative Study Group. Design of the Women's Health Initiative clinical trial and observational study. Control Clin Trials. 1998;19:61–109. doi: 10.1016/s0197-2456(97)00078-0. [DOI] [PubMed] [Google Scholar]
- 24.Weissman MM, Sholomskas D, Pottenger M, et al. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 25.Diwan S, Bankole A, Vahia I, et al. Depression in older adults with schizophrenia spectrum disorder: prevalence and associated factors. Am J Geriatr Psychiatry. 2007;15:991–998. doi: 10.1097/JGP.0b013e31815ae34b. [DOI] [PubMed] [Google Scholar]
- 26.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 27.Lawton MP. The Philadelphia Geriatric Center Morale Scale: a revision. J Gerontol. 1975;30:85–89. doi: 10.1093/geronj/30.1.85. [DOI] [PubMed] [Google Scholar]
- 28.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19:200–231. [PubMed] [Google Scholar]
- 29.Sherer M, Maddux JE, Mercadente B, et al. The self-efficacy scale: construction and validation. Psychol Rep. 1982;51:663–671. [Google Scholar]
- 30.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 31.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 32.Broadbent DE, Cooper PF, FitzGerald P, et al. The Cognitive Failures Questionnaire (CFQ) and its correlates. Br J Clin Psychol. 1982;21:1–16. doi: 10.1111/j.2044-8260.1982.tb01421.x. [DOI] [PubMed] [Google Scholar]
- 33.Drachman DA, Swearer JM. Screening for dementia: Cognitive Assessment Screening Test (CAST) Am Fam Physician. 1996;54:1957–1962. [PubMed] [Google Scholar]
- 34.Derogatis LR, Spencer MS. The Brief Symptom Inventory (BSI) Administration, Scoring, and Procedures Manual. Baltimore MD: Johns Hopkins University School of Medicine; 1982. [Google Scholar]
- 35.Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples) Biometrika. 1965;52:591–611. [Google Scholar]
- 36.Schafer JL. Analysis of Incomplete Multivariate Data. New York: Chapman & Hall; 1996. [Google Scholar]
- 37.Maercker A, Forstmeier S, Enzler A, et al. Adjustment disorders, posttraumatic stress disorder, and depressive disorders in old age: findings from a community survey. Compr Psychiatry. 2008;49:113–120. doi: 10.1016/j.comppsych.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 38.Heun R, Papassotiropoulos A, Ptok U. Subthreshold depressive and anxiety disorders in the elderly. Eur Psychiatry. 2000;15:173–182. doi: 10.1016/s0924-9338(00)00228-5. [DOI] [PubMed] [Google Scholar]
- 39.Phelan EA, Larson EB. "Successful aging"--where next? J Am Geriatr Soc. 2002;50:1306–1308. doi: 10.1046/j.1532-5415.2002.t01-1-50324.x. [DOI] [PubMed] [Google Scholar]
- 40.Giltay EJ, Kamphuis MH, Kalmijn S, et al. Dispositional optimism and the risk of cardiovascular death: the Zutphen Elderly Study. Arch Intern Med. 2006;166:431–436. doi: 10.1001/archinte.166.4.431. [DOI] [PubMed] [Google Scholar]
- 41.Levy B, Ashman O, Dror I. To be or not to be: the effects of aging stereotypes on the will to live. Omega (Westport) 2000;40:409–420. doi: 10.2190/y2ge-bvyq-nf0e-83vr. [DOI] [PubMed] [Google Scholar]
- 42.Levy BR, Slade MD, Kasl SV. Longitudinal benefit of positive self-perceptions of aging on functional health. J Gerontol. 2002;57B:P409–P417. doi: 10.1093/geronb/57.5.p409. [DOI] [PubMed] [Google Scholar]
- 43.Reynolds CF. Recognition and differentiation of elderly depression in the clinical setting. Geriatrics. 1995;50:S6–S15. [PubMed] [Google Scholar]
- 44.Zisook S, Montross L, Kasckow J, et al. Subsyndromal depressive symptoms in middle-age and older persons with schizophrenia. Am J Geriatr Psychiatry. 2007;15:1005–1014. doi: 10.1097/JGP.0b013e3180a725ec. [DOI] [PubMed] [Google Scholar]
- 45.Ahern NR, Kiehl EM, Lou Sole M, et al. A review of instruments measuring resilience. Issues in Comprehensive Pediatric Nursing. 2006;29:103–125. doi: 10.1080/01460860600677643. [DOI] [PubMed] [Google Scholar]
- 46.Avila-Funes JA, Gray-Donald K, Payette H. Association of nutritional risk and depressive symptoms with physical performance in the elderly: the Quebec longitudinal study of nutrition as a determinant of successful aging (NuAge) J Am Coll Nutr. 2008;27:492–498. doi: 10.1080/07315724.2008.10719730. [DOI] [PubMed] [Google Scholar]
- 47.Luppa M, Heinrich S, Angermeyer MC, et al. Healthcare costs associated with recognized and unrecognized depression in old age. Int Psychogeriatr. 2008;20:1219–1229. doi: 10.1017/S1041610208007680. [DOI] [PubMed] [Google Scholar]