Abstract
Previous research using confirmatory factor analysis to model psychopathology comorbidity supported the hypothesis of a broad general factor (i.e., a “bifactor”; Holzinger & Swineford, 1937) of psychopathology in children, adolescents, and adults, with more specific higher-order internalizing and externalizing factors reflecting additional shared variance in symptoms (Lahey et al., 2012; Lahey, Van Hulle, Singh, Waldman, & Rathouz, 2011). The psychological nature of this general factor has not been explored, however. The current study tests a prediction derived from the spectrum hypothesis of personality and psychopathology, that variance in a general psychopathology bifactor overlaps substantially—at both phenotypic and genetic levels—with the dispositional trait of negative emotionality. Data on psychopathology symptoms and dispositional traits were collected from both parents and youth in a representative sample of 1,569 twin pairs (ages 9–17) from Tennessee. Predictions based on the spectrum hypothesis were supported, with variance in negative emotionality and the general factor overlapping substantially at both phenotypic and etiologic levels. Furthermore, stronger correlations were found between negative emotionality and the general psychopathology factor than among other dispositions and other psychopathology factors.
Keywords: comorbidity, negative emotionality, spectrum model, internalizing, externalizing
Common Genetic Influences on Negative Emotionality and a General Psychopathology Factor in Childhood and Adolescence
A full understanding of psychopathology will require an explanation of both its diversity and its substantially correlated nature. The finding that some maladaptive emotions and behaviors (i.e., symptoms) are more correlated than others has been used to define relatively distinct dimensions of psychopathology symptoms empirically (Quay, 1986). Nonetheless, these dimensions are positively correlated with one another to varying degrees, often substantially (Achenbach, Conners, Quay, Verhulst, & Howell, 1989). Similarly, when psychopathology is viewed categorically, the co-occurrence (comorbidity) of mental disorders substantially exceeds chance levels (Krueger & Markon, 2006).
The correlations among dimensions of psychopathology and the corresponding comorbidity among categorical diagnoses are systematic, prevalent in all age groups, and in need of understanding (Krueger & Markon, 2006). When structural models of psychopathology have been used to address these correlations and comorbidity, second-order factors of internalizing (INT) psychopathology (e.g., depression and anxiety) and externalizing (EXT) psychopathology (e.g., conduct problems and substance use) have typically been defined based on the correlations among the specific dimensions of psychopathology or categorical diagnoses (Achenbach & Edelbrock, 1984; Lahey et al., 2004; Krueger, 1999). These structural models replicate across child, adolescent, and adult samples, at least at broad levels of abstraction.
It is very important to note, however, that the broad domains of INT and EXT are themselves substantially correlated across the life span (e.g., a meta-analysis estimated the correlation of INT and EXT in adults to be at r = .50, Krueger & Markon, 2006). The meaning and origin of this correlation between INT and EXT has yet to be explained. One possibility is that INT and EXT both reflect a very broad higher-order factor of psychopathology. In previous studies, such broad dimensions of “general distress” or “demoralization” among psychopathology items have been extracted from adult samples (Meijer et al., 2011; Tellegen et al., 2006).
Furthermore, using confirmatory factor analysis of categorical diagnoses from a large representative sample of adults, Lahey et al. (2012) found that a model specifying an externalizing factor, a distress factor, and a fears factor, along with a general “bifactor” on which every diagnosis loaded, fit the data better than models without the general bifactor. In addition, the general bifactor predicted concurrent and future functioning and psychopathology over and above predictions based on the externalizing, distress, and fears factors. These findings are important because they support the criterion validity of the general bifactor (Lahey et al., 2012). The bifactor model has a long history in psychometrics (Holzinger & Swineford, 1937), and refers to a model in which all items load on a general factor in addition to subsets of items loading on two or more specific factors that are uncorrelated with the general factor. Perhaps most well known in the intelligence literature, which differentiates a “g factor” (Spearman, 1904) from specific factors of intelligence (e.g., Gignac, 2005), the bifactor model has only recently been applied to psychopathology. It has proven useful in personality research (Chen, Hayes, Carver, Laurenceau, & Zhang, 2012) and in decomposing broad, general variance accounting for the comorbidity among disorder from more specific factors (e.g., Martel, Gremillion, Roberts, von Eye, & Nigg, 2010; Patrick, Hicks, Nichol, & Krueger, 2007; Tackett, Daoud, De Bolle, & Burt, 2013). Thus, it is well-suited for testing the hypotheses in the current investigation.
Directly relevant to the present study, a recent study of a large representative sample of twin pairs found that a general bifactor of genetic influences, on which the genetic component of every dimension of psychopathology loaded, accounted for the majority of the genetic influences on a broad range of internalizing and externalizing symptoms in childhood and adolescence (Lahey, van Hulle, Singh, Waldman, & Rathouz, 2011). In contrast, the same study found that environmental influences accounted for only a small portion of the covariation among psychopathology dimensions. Taken together, these findings suggest the hypothesis that a general factor of psychopathology can be described that is robust across age, reflects shared (i.e., pleiotropic) genetic influences on many forms of psychopathology, and improves predictions of future individual functioning. But, what does this general factor of psychopathology represent in psychological terms? The present study aims to address this issue by testing a hypothesis derived from a specific theoretical framework for conceptualizing the role of broad dispositional traits in psychopathology.
Alternative Explanations of the General Bifactor
We are interested in the general bifactor because the broad correlations among dimensions of psychopathology may reflect etiologic processes and biopsychological mechanisms that are nonspecifically involved in risk for many common forms of psychopathology (Lahey, et al., 2012; Lahey, et al., 2011). Because research on the etiology and mechanisms of psychopathology largely progresses as if each form of psychopathology has mostly or entirely unique causes and mechanisms, it would be very important to know if such nonspecific factors are important in psychopathology. In evaluating this hypothesis, however, it is important also to evaluate other viable explanations for the broad correlations among dimensions of psychopathology that are the basis of the general bifactor. For example, a bifactor could arise solely from a general ‘evaluation bias’ which leads informants to rate negatively (or positively) worded items in personality inventories (Anusic, Schimmack, Pinkus, & Lockwood, 2009; Pettersson & Turkheimer, 2010) or in measures of psychopathology symptoms (Pettersson & Turkheimer, 2012) more similarly than is ‘actually’ the case. We will address this alternative interpretation in the present study in part by examining phenotypic and genetic correlations between the general bifactor based on negatively worded psychopathology symptoms and three dispositional dimensions defined by either positively or negatively worded items. If the bifactor is solely an ‘evaluation factor,’ correlations of the psychopathology bifactor with these dispositional dimensions should be equal in absolute magnitudes and the correlations should be positive with dispositional dimensions defined by negatively worded items and inverse with the disposition defined by positively worded items.
Dispositions and Psychopathology
Multiple hypotheses have been put forth to explain the ways in which personality and psychopathology are interconnected (Widiger & Smith, 2008). In attempting to understand the role that personality dimensions play in the general factor of psychopathology, we focus here on the spectrum model of relations between personality and psychopathology. The spectrum model posits etiologic connections between personality and psychopathology, and has proven to be a useful framework for examining this issue in both adults (Widiger & Smith, 2008) and youth (Nigg, 2006; Tackett, 2006).
Relatively stable tendencies to experience negative affect and distress constitute one of the most robust of all identified dispositional dimensions (Watson & Clark, 1984). In models of temperament and personality, this factor is labeled as neuroticism or negative emotionality (NE). Many studies have found NE to be one of the first factors extracted from individual difference items across development, across cultures, across species and across samples from normal and abnormal populations (Gosling & John, 1999; John, Naumann, & Soto, 2008; Lahey, 2009; Markon, Watson, & Krueger, 2005; Rothbart & Bates, 2006; Tackett et al., 2012).
In the present study, we focus on NE because it is robustly correlated with a wide range of mental and physical health problems (Lahey, 2009; Meijer, de Vries, & van Bruggen, 2011; Tellegen et al., 2006; Watson, Clark, & Harkness, 1994). More specifically, a review of the literature found that NE was substantially correlated with both INT and EXT dimensions of psychopathology in adults, whereas disinhibitory traits were associated with only EXT (Krueger & Markon, 2006). Furthermore, NE has been found to account for substantial variance in the phenotypic correlation between INT and EXT in adults (Khan, Jacobson, Gardner, Prescott, & Kendler, 2005) with similar findings in youth (De Bolle, Beyers, De Clercq, & De Fruyt, 2012; Oldehinkel, Hartman, De Winter, Veenstra, & Ormel, 2004). Because the addition of a general psychopathology factor largely explains the correlation between EXT and INT in models without such a factor (Lahey et al., 2011, 2012), these several findings suggest the hypothesis that NE would be associated with the general bifactor of psychopathology.
Emerging data from family studies suggest that NE shares a substantial proportion of its genetic influences with broad forms of psychopathology. Ormel and colleagues (2005) found that temperament partially mediated the effects of familial loading (measured by summing parental lifetime diagnoses) on psychopathology in youth, which provides additional support for a spectrum conceptualization. Another recent investigation (Mikolajewski, Allan, Hart, Lonigan, & Taylor, 2013) found evidence that genetic influences shared with NE accounted for approximately 12% of the variance in INT and 9% of the variance in EXT as rated on parent questionnaires. Furthermore, we recently examined the role of dispositions in the specific cross-domain comorbidity of conduct disorder (CD) and major depressive disorder (MDD) in youth (Tackett, Waldman, van Hulle, & Lahey, 2011). This revealed that genetic influences on the comorbidity of CD and MDD were partially accounted for by genetic influences on NE.
The present study tests the hypothesis that NE is associated with a general bifactor of psychopathology in a large representative sample of child and adolescent twins rather than with more specific factors of psychopathology. We first test key predictions derived from the spectrum hypothesis regarding the extent to which phenotypic variance in a general bifactor of psychopathology is shared with phenotypic variance in NE. Then, we expand our test of the spectrum hypothesis by testing the prediction that NE and the general bifactor of psychopathology share genetic influences.
Following the structured multivariate biometric framework of Lahey et al. (2011), we used a bifactor model approach to capture the higher-order genetic structure of youth psychopathology in the same sample of twins used by Lahey et al. (2011) and Tackett et al. (2012). We also estimated the remaining unique variance characterizing INT and EXT problems, after accounting for shared variance with the general factor, which is expected to show distinct associations with youth dispositions. Although the focus of the current study is on the broad disposition of trait NE, we further explore associations with two dispositions—prosociality and daring—as additional tests of the study hypotheses.
The Present Study
The specific goals of the present study are twofold:
- To examine the extent to which the general factor of psychopathology shares phenotypic variance with the dispositional trait of NE. We will also quantify phenotypic correlations of the two specific factors of INT and EXT and the two dispositions of prosociality and daring, drawing hypotheses from the broader literature (Nigg, 2006; Tackett, 2006).
-
We hypothesize that a general factor of psychopathology is on the same spectrum as NE, such that (1) NE is positively associated at the phenotypic level with the general bifactor of psychopathology, (2) NE is more strongly associated with the bifactor than it is with the specific second-order EXT or INT factors (i.e., specific in the sense that the general bifactor is also accounted for in the model), and (3) that NE is more strongly associated with the bifactor than are two other dispositions of prosociality and daring.Consistent with previous findings (Krueger & Markon, 2006), we hypothesize that specific EXT factor in the bifactor model will show associations with high NE, low prosociality, and high daring.We hypothesize that specific INT factor will show associations with high prosociality, low daring, and perhaps NE.
-
To test the hypothesis that the general bifactor of genetic influences on psychopathology will be substantially correlated with additive genetic influences on NE. This hypothesis is a key component of a comprehensive spectrum model integrating NE, INT, EXT, and the general bifactor at etiologic levels.
Method
Participants
Caregivers (90.8% biological mothers) of 1,569 twin pairs participated in the Tennessee Twin Study (TTS), a representative sample of 6–17-year-old twins living in one of Tennessee’s five metropolitan statistical areas in the years 2000–2001. These areas included Nashville, Memphis, Knoxville, Chattanooga, and Bristol. A random sample was selected, stratified by age and geographic region, with an overall response rate of 70% of eligible families participating. Ethnic composition of the TTS was rated by caregivers as primarily non-Hispanic white (71%), followed by African American (24%), Hispanic (2%) and Other (3%). Caregivers completed a questionnaire on the twins’ physical similarities to assign zygosity (Peeters, Van Gestel, Vlietinck, Derom, & Derom, 1998), with ambiguous cases resolved using 12 polymorphic DNA markers obtained from cheek swabs. Of the 2,063 participating families in the TTS, the current study utilized those with complete interview data for both dispositions and psychopathology (missing data at the item level was minimal), limited to those families with both caregiver and self-report ratings. Self-report was only collected from those twins ages 9 and higher, resulting in the subsample of families (N = 1,569) used for the present study. Information from monozygotic twin pairs (n = 316 female pairs; n = 283 male pairs), same-sex dizygotic twin pairs (n = 256 female pairs; n = 258 male pairs), and opposite-sex dizygotic twin pairs (n = 456 pairs) were used in the present analyses. Detailed information regarding the TTS is published (Lahey, Rathouz, et al., 2008).
Measures
Dispositional traits and psychopathology symptoms were assessed using two independent measures with parallel formats, described below. Both measures were administered in computer-assisted structured interviews by trained lay interviewers (Lahey, Rathouz, et al., 2008).
The Child and Adolescent Psychopathology Scale (CAPS)
The CAPS (Lahey et al., 2004) is a structured clinical interview designed to assess symptoms of child and adolescent disorders (ADHD, ODD, CD, MDD, GAD, SAD, agoraphobia, social phobia, specific phobia, and obsessive-compulsive disorder (OCD)). One symptom was omitted (the GAD symptom regarding difficulty controlling worrying) because it was judged as too difficult for participants to report on. The CAPS assesses major diagnostic symptoms from DSM-IV using a modified response scale offering increased dimensionality from 1 (Not at all) to 4 (Very Much). CAPS items were randomized with two item orders counterbalanced across participants to control for order effects. More information about CAPS properties, including test-retest information, can be found in previous publications (Lahey et al., 2004). We combined information from multiple informants using the same approach in Lahey et al. (2011), such that a best informant method emphasizing the highest endorsement for a given symptom was used for anxiety disorders, depression, and CD. Given evidence the children and adolescents are not reliable and valid informants on symptoms of ODD and ADHD (Bird, Gould, & Staghezza, 1992; Hart, Lahey, Loeber, & Hanson, 1994; Jensen et al., 1999), only caregiver reports were used in these domains.
The Child and Adolescent Dispositions Scale (CADS)
The CADS utilizes the same structured interview format and the same response scale of 1 (Not at all) to 4 (Very much) to assess information on the twins’ dispositional characteristics (Lahey et al., 2008). The CADS was developed to assess a theoretical model for the development of CD, but the dispositional scales are correlated with other specific dimensions of psychopathology (Lahey, Applegate, et al., 2008; Lahey, Rathouz, Applegate, Tackett, & Waldman, 2010). The CADS measures three broad socioemotional dispositions: NE, prosociality (empathy and remorse), and daring (sensation seeking and risk taking). The scales consist of the following number of items: NE-9 items for parents and 7 items for youth; prosociality-12 items for parents and 13 items for youth; and daring-5 items for both informants. Other dimensions of personality that could be relevant to INT or EXT (e.g., positive affect/emotionality) were not measured. Nonetheless, NE, prosociality, and daring are measured reliably and validly in the CADS and these dimensions show theoretically expected connections with dispositions in other personality trait models (Lahey, Applegate, et al., 2008; Lahey, et al., 2010; Mikolajewski, et al., 2013). It is important to note that the CADS was intentionally developed to avoid item overlap with DSM-IV diagnostic symptoms. Specifically, the authors of the CADS used a consensus approach that sought to exclude direct synonyms or antonyms of DSM-IV symptoms in the CADS item pool to minimize item contamination in future tests of disposition-psychopathology relations. Because little is known about the best way to integrate information from different informants on child and adolescent personality dimensions (Tackett et al., 2012), analyses of CADS dimensions were run separately for caregiver and child reports.
Statistical Analyses
Mean ratings of 11 psychopathology dimensions were residualized on age, sex, age-squared, and age × sex. For phenotypic analyses, classical confirmatory factor analysis was used to construct models with a latent bifactor as well as latent factors for INT and EXT. Manifest measures of NE, daring and prosociality were incorporated into joint models to test the associations between these personality dispositions and latent psychopathology constructs.
Exploiting the twin data, univariate biometric models were used to decompose observed phenotypic variance into variance attributable to additive genetic factors (A), environmental factors shared by the twins (C), and environmental factors not shared by the twins, plus measurement error (E; Neale & Cardon, 1992). These models were applied to each dimension of psychopathology, one at a time, as well as to each of the three personality dispositions. Additionally, models were fitted separately to parent and youth reports to examine potential evidence for substantive differences between informants. High convergence was found for parent and youth report, with most dimensions and dispositions yielding strongest support for an AE model. The dimensions with a small and non-significant C component in univariate analyses were specified to have a zero C component in the subsequent multivariate models.
The present multivariate behavior genetic analyses builds on the analyses reported in Lahey et al. (2011); the approach is briefly described here. Model specification began with a standard correlated factors multivariate biometric ACE model (Neale & Cardon, 1992) for twelve dimensions (11 dimensions of psychopathology and 1 dispositional dimension in each model). This captures the entire variance-covariance structures of the genetic, shared environmental, and unshared environmental influences across the ensemble of psychopathology phenotypes and psychological dispositions (Loehlin, 1996). As such, the model includes not only a genetic variance component for each phenotypic dimension, but also the covariance in genetic influences between each pair of dimensions.
Then, rather than estimating this general multivariate ACE model, we constrained the specification by imposing a confirmatory factor analysis (CFA) model for the underlying structure of the genetic covariances of the 11 psychopathology dimensions and the dispositional dimension, allowing the environmental components of variance to freely correlate. These models are direct extensions of those fitted and presented in Lahey et al. (2011) in that they include genetic and environmental components of variance for each dispositional dimension, allowing us to estimate and test genetic overlap between the latent genetic psychopathology dimensions and the three dispositions. The entire variance-covariance structure—both the multivariate ACE decomposition and the CFA structure on the genetic components of variance—was then estimated in a single instance of this unified model in Mplus (Muthén & Muthén, 1998–2006). Mplus scripts are available from the first author on request.
For the phenotypic analyses, we used standard covariance structure model estimation procedures in Mplus, allowing for non-normal and correlated data. In these analyses, co-twins were used as independent observations in model estimation and estimation was based on the assumption of normality. But, for constructing tests and confidence intervals, the Mplus CLUSTER feature together with robust maximum likelihood (MLR), which employ a “sandwich” estimator of variance, were used both to allow for the skewed nature of some of the manifest variables and to account for correlation between co-twins. Direct comparison of the magnitudes of the correlation coefficients was handled through tests of nested models, using the scaled Satorra-Bentler chi-square statistic appropriate for MLR (Satorra, 2000) and the Wald test. The hierarchical biometric analyses also used MLR, but because each twin pair was considered a single observation, the CLUSTER option was not necessary. Aside from that, the biometric analyses were also set up as covariance structure models.
Results
Phenotypic associations between general and specific factors of psychopathology and dispositional dimensions
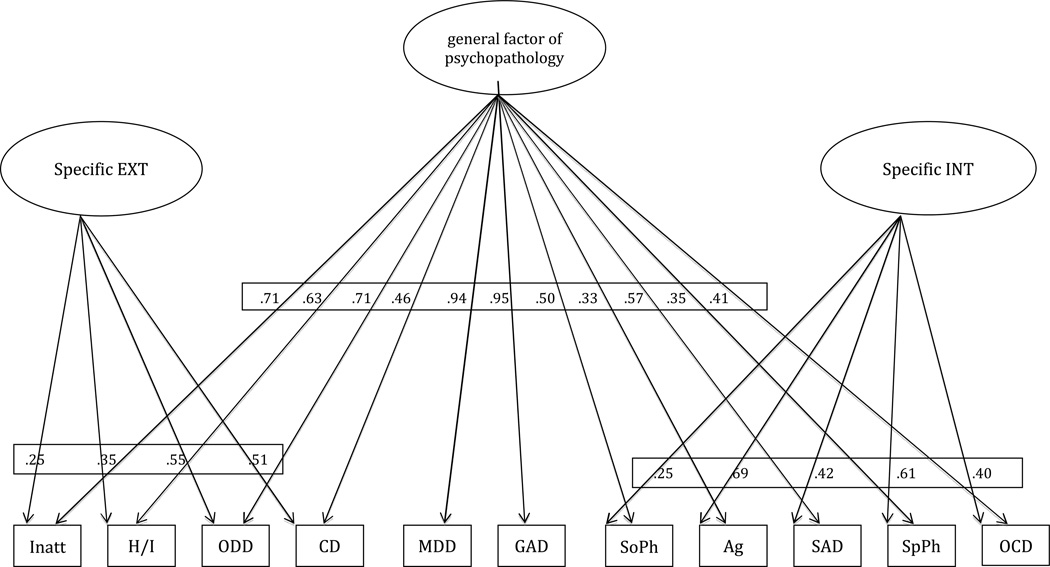
To test the prediction that a general factor would show a strong phenotypic association with NE, a bifactor model based on phenotypic correlations was fitted to the symptom dimensions according to the best-fitting model as presented previously in Lahey et al. (2011). All symptom dimensions were allowed to load on the general bifactor of psychopathology in this model (see Figure 1 and Table 1). In addition a specific EXT factor was defined by conduct, oppositional defiant, inattentive, and hyperactive/impulsive symptom dimensions. A specific INT factor was defined by social phobia, agoraphobia, separation anxiety, specific phobia, and obsessive compulsive symptom dimensions. Unlike the final model selected in Lahey et al. (2011), and in order to provide a stronger test of the hypothesis that the general bifactor accounts for the correlations between INT and EXT, specific EXT and specific INT were not allowed to correlate with one another. This approach is consistent with the definition of the bifactor model, which requires that covariation between specific factors is captured entirely by the general factor (Brown, 2006). This model fit the data well (CFI = 0.96, RMSEA = 0.06, SRMR = 0.03). For comparative purposes, however, a phenotypic bifactor model in which INT and EXT were allowed to correlate also fit well (CFI = 0.97, RMSEA = 0.06, SRMR = 0.03), with a small negative correlation between specific INT and specific EXT (r = −.18; 95% C.I. = −.25, −.11).
Figure 1.
Phenotypic bifactor model of the general factor of psychopathology, specific EXT and specific INT factors.
Table 1.
Figure 1 Standardized Parameter Estimates, Standard Errors, and 95% Confidence Intervals
| Standardized parameter estimate |
Standard Error | 95% Confidence Interval | ||
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Symptom loadings on the general factor | ||||
| Inatt | .71 | .01 | .69 | .73 |
| H/I | .63 | .02 | .60 | .66 |
| ODD | .71 | .01 | .69 | .74 |
| CD | .46 | .02 | .42 | .50 |
| MDD | .94 | .00 | .94 | .95 |
| GAD | .95 | .01 | .94 | .96 |
| SoPh | .50 | .02 | .46 | .53 |
| Ag | .33 | .02 | .29 | .37 |
| SAD | .57 | .02 | .54 | .60 |
| SpPh | .35 | .02 | .31 | .39 |
| OCD | .41 | .02 | .37 | .46 |
| Symptom loadings on specific EXT | ||||
| Inatt | .25 | .02 | .19 | .29 |
| H/I | .35 | .03 | .30 | .41 |
| ODD | .55 | .02 | .51 | .60 |
| CD | .51 | .02 | .47 | .55 |
| Symptom loadings on specific INT | ||||
| SoPh | .25 | .02 | .20 | .29 |
| Ag | .69 | .03 | .64 | .75 |
| SAD | .42 | .03 | .37 | .47 |
| SpPh | .61 | .03 | .55 | .65 |
| OCD | .40 | .03 | .34 | .46 |
Note. EXT = externalizing; INT = internalizing; Inatt = inattentive symptoms; H/I = hyperactive/impulsive symptoms; ODD = oppositional defiant disorder symptoms; CD = conduct disorder symptoms; MDD = major depressive disorder symptoms; GAD = generalized anxiety disorder symptoms; SoPh = social phobia symptoms; Ag = agoraphobia symptoms; SAD = separation anxiety disorder symptoms; SpPh = specific phobia; OCD = obsessive compulsive disorder symptoms.
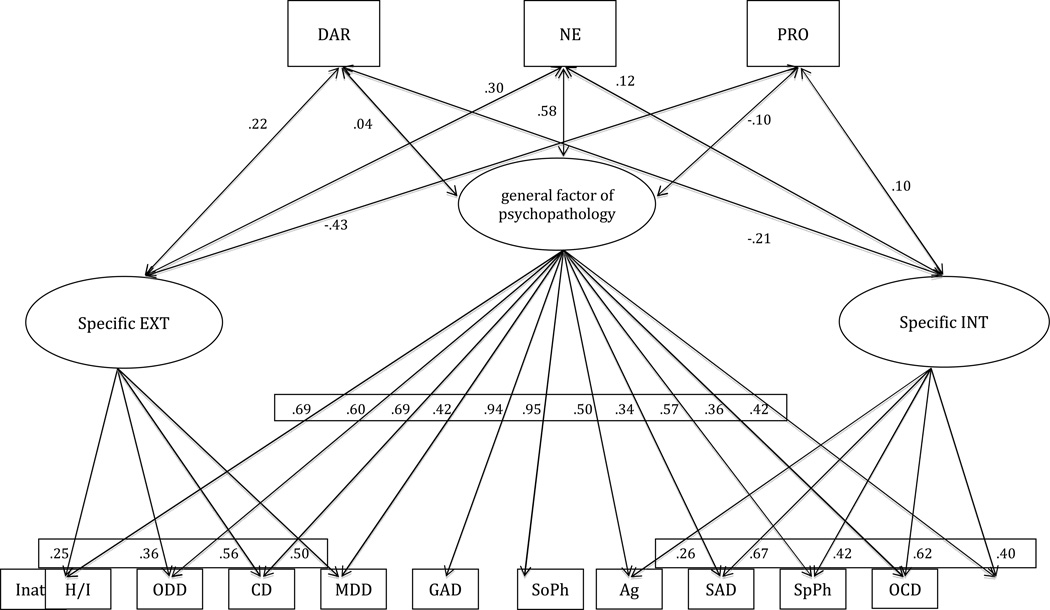
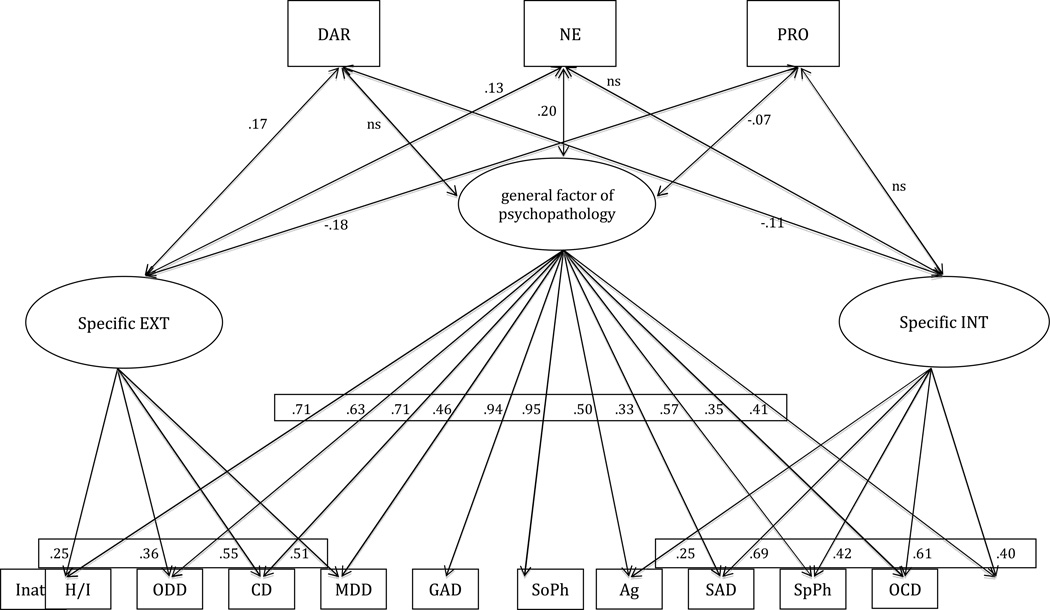
Next, all three CADS dispositions were simultaneously entered into the phenotypic psychopathology bifactor model to estimate correlations between the three dispositions and the general factor of psychopathology, the specific EXT factor, and the specific INT factor. Models were fitted separately for parent and youth reports of CADS dimensions. Results for the phenotypic bifactor model incorporating parent-rated CADS are presented in Figure 2 and Table 2; results for the phenotypic bifactor model incorporating youth-rated CADS are presented in Figure 3 and Table 3. Because the results did not change when the CADS dispositions were allowed to correlate with one another, the model presented did not allow correlations among the dispositions, consistent with previous findings that the CADS disposition typically show only modest cross-trait correlations (Lahey et al., 2010).
Figure 2.
Phenotypic bifactor model of the general factor of psychopathology, specific EXT and specific INT factors and their associations with parent-report of three socioemotional dispositions.
Table 2.
Figure 2 Standardized Parameter Estimates, Standard Errors, and 95% Confidence Intervals
| Standardized parameter estimate |
Standard Error | 95% Confidence Interval | ||
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Symptom loadings on the general factor | ||||
| Inatt | .69 | .01 | .67 | .72 |
| H/I | .60 | .02 | .57 | .64 |
| ODD | .69 | .01 | .66 | .71 |
| CD | .42 | .02 | .38 | .46 |
| MDD | .94 | .01 | .93 | .95 |
| GAD | .95 | .01 | .94 | .96 |
| SoPh | .50 | .02 | .46 | .53 |
| Ag | .34 | .02 | .30 | .38 |
| SAD | .57 | .02 | .54 | .60 |
| SpPh | .36 | .02 | .32 | .40 |
| OCD | .42 | .02 | .38 | .46 |
| Symptom loadings on specific EXT | ||||
| Inatt | .25 | .02 | .21 | .29 |
| H/I | .36 | .02 | .31 | .40 |
| ODD | .56 | .02 | .52 | .60 |
| CD | .50 | .02 | .46 | .54 |
| Symptom loadings on specific INT | ||||
| SoPh | .26 | .03 | .21 | .31 |
| Ag | .67 | .03 | .62 | .73 |
| SAD | .42 | .03 | .37 | .47 |
| SpPh | .62 | .03 | .57 | .67 |
| OCD | .40 | .03 | .33 | .46 |
| NE correlations | ||||
| Parent report | ||||
| Specific EXT | .30 | .02 | .26 | .34 |
| General factor | .58 | .02 | .55 | .61 |
| Specific INT | .12 | .02 | .07 | .16 |
| DAR correlations | ||||
| Parent report | ||||
| Specific EXT | .22 | .03 | .17 | .27 |
| General factor | .04 | .02 | .00 | .07 |
| Specific INT | −.21 | .03 | −.26 | −.16 |
| PRO correlations | ||||
| Parent report | ||||
| Specific EXT | −.43 | .03 | −.48 | −.37 |
| General factor | −.10 | .02 | −.14 | −.06 |
| Specific INT | .10 | .03 | .05 | .16 |
Note. EXT = externalizing; INT = internalizing; Inatt = inattentive symptoms; H/I = hyperactive/impulsive symptoms; ODD = oppositional defiant disorder symptoms; CD = conduct disorder symptoms; MDD = major depressive disorder symptoms; GAD = generalized anxiety disorder symptoms; SoPh = social phobia symptoms; Ag = agoraphobia symptoms; SAD = separation anxiety disorder symptoms; SpPh = specific phobia; OCD = obsessive compulsive disorder symptoms; DAR = daring items; NE = negative emotionality items; PRO = prosociality items.
Figure 3.
Phenotypic bifactor model of the general factor of psychopathology, specific EXT and specific INT factors and their associations with youth-report of three socioemotional dispositions.
Table 3.
Figure 3 Standardized Parameter Estimates, Standard Errors, and 95% Confidence Intervals
| Standardized parameter estimate |
Standard Error | 95% Confidence Interval | ||
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Symptom loadings on the general factor | ||||
| Inatt | .71 | .01 | .69 | .73 |
| H/I | .63 | .02 | .60 | .66 |
| ODD | .71 | .01 | .69 | .74 |
| CD | .46 | .02 | .42 | .50 |
| MDD | .94 | .01 | .94 | .95 |
| GAD | .95 | .01 | .94 | .96 |
| SoPh | .50 | .02 | .46 | .53 |
| Ag | .33 | .02 | .29 | .37 |
| SAD | .57 | .02 | .54 | .60 |
| SpPh | .35 | .02 | .31 | .39 |
| OCD | .41 | .02 | .37 | .46 |
| Symptom loadings on specific EXT | ||||
| Inatt | .25 | .02 | .20 | .29 |
| H/I | .36 | .03 | .31 | .41 |
| ODD | .55 | .02 | .51 | .59 |
| CD | .51 | .02 | .47 | .54 |
| Symptom loadings on specific INT | ||||
| SoPh | .25 | .02 | .20 | .29 |
| Ag | .69 | .03 | .63 | .74 |
| SAD | .42 | .03 | .37 | .47 |
| SpPh | .61 | .03 | .56 | .66 |
| OCD | .40 | .03 | .34 | .46 |
| NE correlations | ||||
| Youth report | ||||
| Specific EXT | .13 | .02 | .08 | .17 |
| General factor | .20 | .02 | .16 | .24 |
| Specific INT | .02 | .02 | −.02 | .06 |
| DAR correlations | ||||
| Youth report | ||||
| Specific EXT | .17 | .03 | .12 | .21 |
| General factor | .05 | .02 | .01 | .09 |
| Specific INT | −.11 | .03 | −.16 | −.06 |
| PRO correlations | ||||
| Youth report | ||||
| Specific EXT | −.18 | .03 | −.23 | −.13 |
| General factor | −.07 | .02 | −.11 | −.03 |
| Specific INT | .02 | .02 | −.02 | .07 |
Note. EXT = externalizing; INT = internalizing; Inatt = inattentive symptoms; H/I = hyperactive/impulsive symptoms; ODD = oppositional defiant disorder symptoms; CD = conduct disorder symptoms; MDD = major depressive disorder symptoms; GAD = generalized anxiety disorder symptoms; SoPh = social phobia symptoms; Ag = agoraphobia symptoms; SAD = separation anxiety disorder symptoms; SpPh = specific phobia; OCD = obsessive compulsive disorder symptoms; DAR = daring items; NE = negative emotionality items; PRO = prosociality items.
Consistent with our hypotheses, the general factor of psychopathology correlated more strongly at the phenotypic level with NE than with daring or prosociality in both parent and youth reports. Specifically, the correlation between parent-reported NE and the general bifactor of psychopathology could not be constrained to equal the correlation between parent-reported daring and the general bifactor of psychopathology (chi-square = 159.43, df = 1, p<.001). Given that the prosociality dimension was keyed in the opposite direction, the parameter sign was first reversed and then constrained to equal that of parent-reported NE and the general bifactor of psychopathology. This test indicated that the correlation between parent-reported NE and the general bifactor of psychopathology could not be constrained to equal the correlation between parent-reported prosociality and the general bifactor of psychopathology (Wald test = 202.34, df = 1, p<.000). Similarly, the correlation between youth-reported NE and the general factor of psychopathology could not be constrained to equal the correlation between youth-reported daring and the general bifactor of psychopathology (chi-square = 16.27, df = 1, p<.001) and the correlation between youth-reported NE and the general bifactor of psychopathology could not be constrained to equal the correlation between youth-reported prosociality and the general bifactor of psychopathology (Wald test = 30.97, df = 1, p<.000).
As hypothesized, NE showed significantly stronger phenotypic associations with the general bifactor of psychopathology than it did with the specific EXT or specific INT factors. That is, the correlation between parent-reported NE and the general bifactor of psychopathology could not be constrained to equal the correlation of parent-reported NE with either INT (chi-square = 253.96, df = 1, p<.001) or EXT (chi-square = 166.07, df = 1, p<.001). Similarly, the correlation between youth-reported NE and the general bifactor of psychopathology could not be constrained to equal the correlation between youth-reported NE and INT (chi-square = 43.77, df = 1, p<.001) or youth-reported EXT (chi-square = 29.75, df = 1, p<.001).
Furthermore, as predicted by Lahey and Waldman (2003), the specific EXT and specific INT factors both showed significant associations with parent-reported NE, but this was found for youth-reported NE only with the specific EXT factor (see Tables 2 and 3). For both parent- and youth-reported CADS dimensions, the specific EXT factor also showed significant and important associations with both low prosociality and high daring. For both parent and youth reports of dispositions, specific INT showed additional associations with low daring. Only in parent-reports was specific INT also significantly correlated with high prosociality.
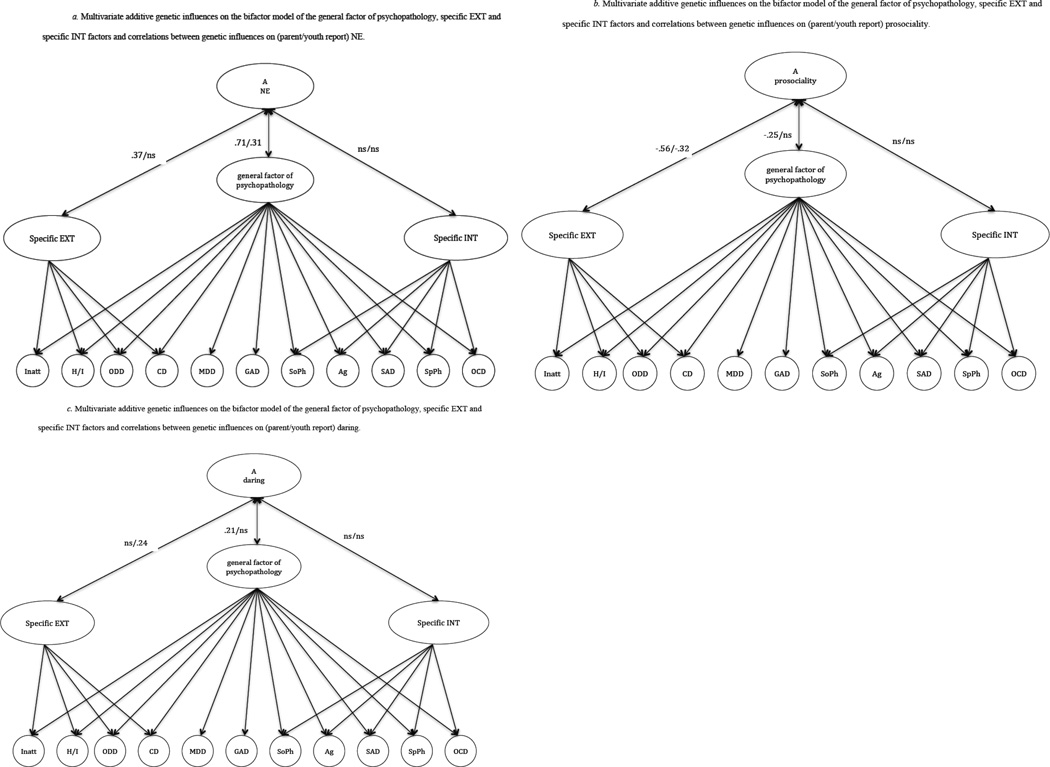
Shared etiologic influences on psychopathology and dispositional dimensions
Because we used a sample of twins, we were able to take the important next step of examining the spectrum hypothesis regarding genetic influences common to both the general bifactor and NE. Specifically, additive genetic and nonshared environmental influences on NE were incorporated into the overall bifactor model for the genetic covariance structure as presented in Lahey et al. (2011). This allowed us to examine the correlations between additive genetic influences on NE with the bifactor, specific INT, and specific EXT components of the genetic influences on psychopathology. Models incorporating genetic influences common to NE and higher-order psychopathology factors fit well for both parent-reported NE (CFI = .98, RMSEA = .03, SRMR = .07) and youth-reported NE (CFI = .98, RMSEA = .03, SRMR = .07). For parsimonious presentation of results, combined findings from these two models are presented in Figure 4 and Table 4.
Figure 4.
Multivariate additive genetic influences on the bifactor model of the general factor of psychopathology, specific EXT and specific INT factors, and correlations between genetic influences on (parent/youth report) of three dispositions (4a – NE, 4b – prosociality, 4c – daring).
Table 4.
Figure 4a–c Standardized Parameter Estimates, Standard Errors, and 95% Confidence Intervals
| Standardized parameter estimate |
Standard Error | 95% Confidence Interval | ||
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| NE correlations (4a) | ||||
| Parent report | ||||
| Specific EXT | .37 | .08 | .21 | .52 |
| General factor | .71 | .04 | .64 | .78 |
| Specific INT | .07 | .04 | −.01 | .15 |
| Youth report | ||||
| Specific EXT | .07 | .07 | −.07 | .20 |
| General factor | .31 | .04 | .24 | .39 |
| Specific INT | −.07 | .05 | −.17 | .03 |
| PRO correlations (4b) | ||||
| Parent report | ||||
| Specific EXT | −.56 | .07 | −.69 | −.43 |
| General factor | −.25 | .05 | −.35 | −.16 |
| Specific INT | −.05 | .05 | −.15 | .04 |
| Youth report | ||||
| Specific EXT | −.32 | .08 | −.47 | −.17 |
| General factor | −.07 | .04 | −.15 | .00 |
| Specific INT | −.05 | .05 | −.15 | .05 |
| DAR correlations (4c) | ||||
| Parent report | ||||
| Specific EXT | .11 | .11 | −.10 | .33 |
| General factor | .21 | .06 | .10 | .32 |
| Specific INT | .06 | .09 | −.13 | .24 |
| Youth report | ||||
| Specific EXT | .24 | .07 | .10 | .37 |
| General factor | .08 | .05 | −.01 | .18 |
| Specific INT | −.08 | .08 | −.24 | .08 |
Note. EXT = externalizing; INT = internalizing; DAR = daring items; NE = negative emotionality items; PRO = prosociality items.
Consistent with our predictions, the general bifactor based on genetic correlations among the dimensions of psychopathology was correlated with additive genetic influences on NE for both parent (r = .71, 95% CI = .64–.78) and youth (r = .31, 95% CI =.23–.39) reports of NE. The specific EXT factor based on genetic covariances also was correlated with additive genetic influences on NE for parent (r = .37, 95% CI = .22–.53), but not for youth (r = .07, 95% CI = −.07– .20) reports of NE. The specific INT factor based on genetic covariances did not correlate with additive genetic influences on NE for either parent (r = .07, 95% CI = −.01–.14) or youth report (r = −.07, 95% CI = −.17–.03).
In these models based on genetic covariances, we further examined the extent to which the general psychopathology bifactor, and the specific EXT and INT factors were correlated with genetic influences on prosociality and daring. The general bifactor was correlated with additive genetic influences on prosociality for only the parent report (r = −.25, 95% CI = −.35, –.15) of prosociality. The specific EXT factor of genetic influences was correlated with additive genetic influences on prosociality for both youth (r = −.32, 95% CI = −.47, –.17) and parent (r = −.56, 95% CI = −.69, –.43) report of prosociality. The specific INT factor was not significantly correlated with additive genetic influences on prosociality. The general bifactor was correlated with additive genetic influences on daring for only the parent report (r = .21, 95% CI = .10, .32) of daring. The specific EXT factor was correlated with additive genetic influences on daring for only the youth (r = .24, 95% CI = .10, .38) report of daring. The specific INT factor was not significantly correlated with additive genetic influences on daring.
Discussion
Previous research has identified a general bifactor of psychopathology that accounts for the robust correlation among INT and EXT factors of psychopathology in youth and adults (Lahey et al., 2012). The current study tested predictions derived from a spectrum hypothesis that the dispositional trait of NE overlaps both phenotypically and etiologically with the general bifactor of psychopathology in childhood and adolescence. These predictions were supported in that NE evidenced higher phenotypic correlations with the general bifactor than with either specific EXT or specific INT factors. In addition, the general psychopathology factor evidenced higher phenotypic correlations with NE than with two other dispositional traits of daring and prosociality. Moreover, common genetic influences on NE and the general psychopathology bifactor were found, with genetic influences showing greater correlations between NE and the general psychopathology bifactor than with the specific psychopathology factors. Similarly, the other CADS dispositions shared less genetic variance with the general bifactor than did NE.
Secondary aims of the present study included examination of associations between the CADS dispositions and specific variance in EXT and INT (i.e., when the general bifactor was accounted for in the model). The predictions that specific EXT would also show significant phenotypic associations with low prosociality and high daring (Lahey & Waldman, 2003) were supported in both parent and youth informants of these dispositions. In addition, parent- and youth-reported NE were both found to be significantly associated phenotypically with the specific EXT factor in addition to their associations with the general psychopathology bifactor. Also as predicted (Lahey & Waldman, 2003), the specific INT factor was significantly associated with both parent and youth reports of low daring at the phenotypic level. Further secondary analyses revealed some overlapping genetic influences common to the psychopathology factors and the other dispositions (daring and prosociality), but these connections were mostly modest. Nonetheless, these analyses revealed a potentially important correlation (r = −.56) between genetic influences on specific EXT and genetic influences on parent-reported prosociality that is consistent with our earlier hypotheses (Lahey & Waldman, 2003).
Insofar as these data demonstrate that the general bifactor is correlated substantially with dispositional NE, both phenotypically and genetically, the current study provides a comprehensive and stringent test of a spectrum model explanation for a hypothesized general factor of psychopathology. These results have important implications for conceptualizing comorbidity in youth, such that dispositional NE may represent a nonspecific vulnerability factor that underlies multiple dimensions of psychopathology (Lahey, 2009; Ormel et al., 2005). The present findings for specific variance in EXT and INT are largely consistent with previous empirical findings (De Bolle et al., 2012; Mikolajewski et al., 2012; Oldehinkel et al., 2004; Ormel et al., 2005) and theoretical conceptualizations of personality-psychopathology associations in youth (Lahey & Waldman, 2003; Nigg, 2006; Tackett, 2006), but extend previous studies by examining specific variance in each domain after accounting for the general psychopathology bifactor. Our predictions for EXT based on the spectrum model were largely supported, such that specific variance in EXT was further associated with characteristics such as risk-taking, lack of empathy, and NE/low frustration tolerance (Khan et al., 2005; Lahey & Waldman, 2005). The CADS may not characterize all dispositions associated with INT, but the findings that NE is nonspecifically associated with internalizing dimensions through the general bifactor and that lower daring is directly associated with INT are consistent with our hypotheses (Lahey & Waldman, 2003).
Alternative Interpretations of the General Bifactor
Our analyses are based on the assumption that the general bifactor has meaning because it reflects shared etiologic factors and biopsychological mechanisms, but as noted above it is possible that the bifactor is merely an artifact of a general tendency of informants to non-veridically rate all negatively and positively worded items similarly (Pettersson & Turkheimer, 2010, 2012). The directions of both the genetic and phenotypic associations between the general psychopathology bifactor and the three dispositional dimensions are consistent with the hypothesis that the bifactor is an artifact of a negative evaluation bias. This is because the bifactor, which is derived from correlations among dimensions of negatively worded symptoms, was found to be positively correlated with the two dispositions based on negatively worded items (negative emotionality and daring) and inversely correlated with the disposition based on positively worded items (prosociality). Nonetheless, there were marked and statistically significant differences in the magnitudes of those correlations. Consistent with our hypothesis, negative emotionality showed significantly stronger correlations with the psychopathology bifactor than did either daring or prosociality. Such differences in magnitude are not consistent with the hypothesis that evaluation bias is the sole explanation for the general bifactor.
Another argument against the evaluation bias hypothesis comes from our earlier analyses of data from the same study of twins (Lahey, et al., 2011). When a general psychopathology bifactor was specified based on CFA of genetic covariances, the loadings of each dimension of psychopathology on the bifactor were substantial and the unique genetic influences on specific dimensions ranged from small to moderate. In contrast, when the general psychopathology bifactor was specified based on nonshared environmental covariances among the same dimensions of psychopathology in the same sample, loadings on the bifactor were small and unique nonshared environmental influences on each dimension were large. This distinctly different pattern of findings for genetic and environmental covariances in the bifactor model is not consistent with the hypothesis that the bifactor is an artifact of a negative evaluation bias in reporting symptoms. This is because there is no reason to suspect that the magnitude of the putative negative evaluation bias—which presumably makes ratings of negatively worded symptoms more similar within each rated individual—would be greater when reporting on negatively worded symptoms of a given individual when that individual has a monozygotic than a dizygotic twin. Instead, the results of our previous analyses are more consistent with the hypothesis that the broad correlations among dimensions of psychopathology that give rise to the bifactor reflect shared genetic influences considerably more so than environmental factors, which commonly influence all dimensions of psychopathology (Lahey, et al., 2011). Although these two sets of findings are inconsistent with the hypothesis that the widespread correlations among dimensions of psychopathology reflect only an evaluation bias based on the valence of the items, it is very important to continue to examine the negative evaluation bias hypothesis and other explanations of the general bifactor in terms other than substantive causes of covariation.
Limitations and Future Directions
The present findings are supported by previous work using the PANAS Negative Affect scale (Watson, Clark, & Tellegen, 1998), which found correlations with internalizing psychopathology (Mikolajewski et al., 2012) that were similar in magnitude with the present correlations of internalizing with the CADS measure of NE. Nonetheless, the CADS dispositional scales used here may not capture all aspects of personality that are relevant to psychopathology, particularly the specific INT factor. Low surgency or positive affect may also be relevant (e.g., De Bolle et al., 2012; Durbin, Klein, Hayden, Buckley, & Moerk, 2005; Oldehinkel et al., 2004), although evidence for the explanatory power of positive emotionality/extraversion for broadband comorbidity has not been consistent (see Khan et al., 2005). It will be useful for future studies using different temperament/personality frameworks to examine associations with the general psychopathology factor, specific EXT and specific INT across different traits and facets.
Although use of both parent and youth reports on psychopathology and dispositions is a strength of the present study, the use of such multi-informant data raises the longstanding question in child clinical research: “Who reports best on what?” (Achenbach, 2006). Informant discrepancies for child psychopathology have been extensively documented and discussed (De Los Reyes & Kazdin, 2005), offering some guidance in how to combine these reports for various symptom domains (e.g., Lahey et al., 2011). Much less is known about incorporating informants for measurement of child personality, however (Tackett, 2012), leading to a more comprehensive approach for measurement of dispositional traits in the current study. Specifically, given the nascent state of empirical research on multi-informant assessment of child personality, we thought it prudent to present results separately from parent and youth informants. It is important to note that the overall pattern of results was virtually identical using parent- and youth-reported dispositions, even though there was a systematic difference in magnitude supporting stronger findings for parent-reported dispositions. The sole use of parent reports for ADHD and ODD may have contributed to the higher magnitudes of parameter estimates associated with parent-reported dispositions. As researchers continue to make advances in answering this longstanding question—for both personality and psychopathology in childhood—researchers should take increasingly refined approaches to integrating such information whenever possible.
Conclusion
In a large, representative sample of same- and opposite-sex twin pairs from Tennessee, the present study tested interrelated hypotheses regarding connections between the dispositional trait of NE and a general factor of psychopathology in childhood and adolescence. Hypotheses were confirmed at the phenotypic level, such that the dispositional trait of NE showed stronger connections with the general factor of psychopathology than it did with either specific variance in INT or specific variance in EXT. Furthermore, associations between NE and the general factor of psychopathology were stronger than were associations with the two other dispositions (prosociality and daring) and the general factor of psychopathology. These results replicated at the genetic level, suggesting that NE shares greater genetic overlap with the general factor of psychopathology than it does with either specific variance in INT or EXT, and the strength of this relationship is greater for NE than it is for the dispositions of prosociality or daring. These findings support a spectrum hypothesis explanation of relations between NE and multiple forms of psychopathology, providing further clarity regarding the psychological nature of psychopathology comorbidity in youth. Future research should examine the robustness of these findings in other samples, expand tests of specificity to other dispositions, better disentangle the general factor of psychopathology from social desirability and response bias, and provide tests of criterion validity for the general factor of psychopathology.
Acknowledgment
This study was supported in part by NIMH grant R01 MH59111.
Contributor Information
Jennifer L. Tackett, Department of Psychology, University of Houston
Benjamin B. Lahey, Department of Health Studies, University of Chicago
Carol Van Hulle, Department of Psychiatry, University of Chicago.
Irwin Waldman, Department of Psychology, Emory University.
Robert F. Krueger, Department of Psychology, University of Minnesota
Paul J. Rathouz, Department of Biostatistics & Medical Informatics, University of Wisconsin School of Medicine and Public Health
References
- Achenbach TM. As others see us: Clinical and research implications of cross-informant correlations for psychopathololgy. Current Directions in Psychological Science. 2006;15:94–98. [Google Scholar]
- Achenbach TM, Conners CK, Quay HC, Verhulst FC, Howell CT. Replication of empirically derived syndromes as a basis for taxonomy of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 1989;17:299–323. doi: 10.1007/BF00917401. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Edelbrock CS. Classification of child psychopathology: Review and analysis of empirical efforts. Psychological Bulletin. 1978;85:1275–1301. [PubMed] [Google Scholar]
- Achenbach TM, Edelbrock CS. Psychopathology of childhood. Annual Review of Psychology. 1984;35:227–256. doi: 10.1146/annurev.ps.35.020184.001303. [DOI] [PubMed] [Google Scholar]
- Anusic I, Schimmack U, Pinkus RT, Lockwood P. The nature and structure of correlations among big five ratings: The halo-alpha-beta model. Journal of Personality and Social Psychology. 2009;97:1142–1156. doi: 10.1037/a0017159. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, Gatzke-Kopp L. Multifinality in the development of personality disorders: A biology × sex × environment interaction model of antisocial and borderline traits. Development and Psychopathology. 2009;21:735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. New York: Guilford; 2006. [Google Scholar]
- Chen FF, Hayes A, Carver CS, Laurenceau J, Zhang Z. Modeling general and specific variance in multifaceted constructs: A comparison of the bifactor model to other approaches. Journal of Personality. 2012;80:219–251. doi: 10.1111/j.1467-6494.2011.00739.x. [DOI] [PubMed] [Google Scholar]
- De Bolle M, Beyers W, De Clercq B, De Fruyt F. General personality and psychopathology in referred and nonreferred children and adolescents: An investigation of continuity, pathoplasty, and complication models. Journal of Abnormal Psychology. 2012 doi: 10.1037/a0027742. Advance online publication. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Durbin CE, Klein DN, Hayden EP, Buckley ME, Moerk KC. Temperamental emotionality in preschoolers and parental mood disorders. Journal of Abnormal Psychology. 2005;114:28–37. doi: 10.1037/0021-843X.114.1.28. [DOI] [PubMed] [Google Scholar]
- Gignac GE. Revisiting the factor structure of the WAIS-R: Insights through nested factor modeling. Assessment. 2005;12:320–329. doi: 10.1177/1073191105278118. [DOI] [PubMed] [Google Scholar]
- Gosling SD, John OP. Personality dimensions in nonhuman animals: A cross-species review. Current Directions in Psychological Science. 1999;8:69–75. [Google Scholar]
- Hart EL, Lahey BB, Loeber R, Hanson KS. Criterion validity of informants in the diagnosis of disruptive behavior disorders in children: A preliminary study. Journal of Consulting and Clinical Psychology. 1994;62:410–414. doi: 10.1037/0022-006X.62.2.410. [DOI] [PubMed] [Google Scholar]
- Holzinger KJ, Swineford F. The bi-factor method. Psychometrika. 1937;2:41–54. [Google Scholar]
- Jensen PS, Rubio-Stipec M, Canino G, Bird HR, Dulcan MK, Schwab-Stone ME, et al. Parent and child contributions to diagnosis of mental disorder: Are both informants always necessary? Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- John OP, Naumann LP, Soto CJ. Paradigm shift to the integrative big five trait taxonomy: History, measurement, and conceptual issues. In: John OP, Robins RW, Pervin LA, editors. Handbook of Personality: Theory and Research. 3rd ed. New York: Guilford; 2008. pp. 114–158. [Google Scholar]
- Joreskog KG, Sorbom D. LISREL8: Structural equation modeling with the SIMPLIS command language. Hillsdale, NJ: Erlbaum; 1993. [Google Scholar]
- Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. British Journal of Psychiatry. 2005;186:190–196. doi: 10.1192/bjp.186.3.190. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner S, Tackett JL, Bagby RM. The structure of internalizing disorders in middle childhood and evidence for personality correlates. Journal of Psychopathology and Behavioral Assessment. 2012;34:22–34. [Google Scholar]
- Lahey BB. Public health significance of neuroticism. American Psychologist. 2009;64:241–256. doi: 10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Chronis AM, Jones HA, Hall Williams S, Loney J, Waldman ID. Psychometric characteristics of a measure of emotional dispositions developed to test a developmental propensity model of conduct disorder. Journal of Clinical Child and Adolescent Psychology. 2008;37:794–807. doi: 10.1080/15374410802359635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, Rathouz PJ. Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology. 2012;121:971–977. doi: 10.1037/a0028355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: Generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Applegate B, Hulle CV, Garriock HA, Urbano RC, et al. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Applegate B, Tackett JL, Waldman ID. Psychometrics of a self-report version of the child and adolescent dispositions scale. Journal of Clinical Child and Adolescent Psychology. 2010;39:351–361. doi: 10.1080/15374411003691784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. 2011;68:181–189. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Waldman ID. A developmental propensity model of the origins of conduct problems during childhood and adolescence. In: Lahey BB, Moffitt TE, Caspi A, editors. Causes of conduct disorder and juvenile delinquency. New York: Guilford; 2003. pp. 76–117. [Google Scholar]
- Lahey BB, Waldman ID. A developmental model of the propensity to offend during childhood and adolescence. In: Farrington DP, editor. Advances in criminological theory. Volume 13. Piscataway, NJ; Transaction Publishers: 2005. pp. 15–50. [Google Scholar]
- Loehlin JC. The cholesky approach: A cautionary note. Behavior Genetics. 1996;26:65–69. [Google Scholar]
- Markon KE, Krueger RF, Watson D. Delineating the structure of normal and abnormal personality: An integrative hierarchical approach. Journal of Personality and Social Psychology. 2005;88:139–157. doi: 10.1037/0022-3514.88.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Gremillion M, Roberts B, von Eye A, Nigg JT. The structure of childhood disruptive behaviors. Psychological Assessment. 2010;22:816–826. doi: 10.1037/a0020975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijer RR, de Vries RM, van Bruggen V. An evaluation of the brief symptom inventory-18 using item response theory: Which items are most strongly related to psychological distress? Psychological Assessment. 2011;23:193–202. doi: 10.1037/a0021292. [DOI] [PubMed] [Google Scholar]
- Mikolajewski AJ, Allan NP, Hart SA, Lonigan CJ, Taylor J. Negative affect shares genetic and environmental influences with symptoms of childhood internalizing and externalizing disorders. Journal of Abnormal Child Psychology. 2013;41:411–423. doi: 10.1007/s10802-012-9681-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Fourth edition. Los Angeles, CA: Muthén & Muthén; 1998–2006. [Google Scholar]
- Neale MC, Cardon LR. Methodology for genetic studies of twins and families. Boston: Kluwer Academic; 1992. [Google Scholar]
- Nigg JT. Temperament and developmental psychopathology. Journal of Child Psychology and Psychiatry. 2006;47:395–422. doi: 10.1111/j.1469-7610.2006.01612.x. [DOI] [PubMed] [Google Scholar]
- Oldehinkel AJ, Hartman CA, De Winter AF, Veenstra R, Ormel J. Temperament profiles associated with internalizing and externalizing problems in preadolescence. Development and Psychopathology. 2004;16:421–440. doi: 10.1017/s0954579404044591. [DOI] [PubMed] [Google Scholar]
- Ormel J, Oldehinkel AJ, Ferdinand RF, Hartman CA, De Winter AF, Veenstra R, et al. Internalizing and externalizing problems in adolescence: General and dimension-specific effects of familial loadings and preadolescent temperament traits. Psychological Medicine. 2005;35:1825–1835. doi: 10.1017/S0033291705005829. [DOI] [PubMed] [Google Scholar]
- Oshri A, Rogosch FA, Burnette ML, Cicchetti D. Developmental pathways to adolescent cannabis abuse and dependence: Child maltreatment, emerging personality, and internalizing versus externalizing psychopathology. Psychology of Addictive Behaviors. 2011;25:634–644. doi: 10.1037/a0023151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick CJ, Hicks BM, Nichol PE, Krueger RF. A bifactor approach to modeling the structure of the Psychopathy Checklist-Revised. Journal of Personality Disorders. 2007;21:118–141. doi: 10.1521/pedi.2007.21.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters H, Van Gestel S, Vlietinck R, Derom C, Derom R. Validation of a telephone zygosity questionnaire in twins of known zygosity. Behavior Genetics. 1998;28:159–161. doi: 10.1023/a:1021416112215. [DOI] [PubMed] [Google Scholar]
- Pettersson E, Turkheimer E. Item selection, evaluation, and simple structure in personality data. Journal of Research in Personality. 2010;44:407–420. doi: 10.1016/j.jrp.2010.03.002. [Article]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettersson E, Turkheimer E. The role of evaluation in the genetic structure of externalizing and internalizing spectra. Behavior Genetics. 2012;42:960–960. [Google Scholar]
- Quay HC. Classification. In: Quay HC, Werry JS, editors. Psychopathological disorders of childhood. 3rd ed. New York: Wiley; 1986. pp. 1–42. [Google Scholar]
- Rothbart MK, Bates JE. Temperament. In: Eisenberg N, Damon W, Lerner RM, editors. Handbook of Child Psychology, 6th ed., Vol 3: Social, emotional, and personality development. Hoboken, NJ: Wiley; 2006. pp. 99–166. [Google Scholar]
- Spearman C. "General intelligence" objectively determined and measured. American Journal of Psychology. 1904;15:201–292. [Google Scholar]
- Tackett JL. Evaluating models of the personality-psychopathology relationship in children and adolescents. Clinical Psychology Review. 2006;26:584–599. doi: 10.1016/j.cpr.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Tackett JL. Parent informants for child personality: Agreement, discrepancies, and clinical utility. Journal of Personality Assessment. 2011;93:539–544. doi: 10.1080/00223891.2011.608763. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Daoud SLSB, De Bolle M, Burt SA. Is relational aggression part of the externalizing spectrum? A bifactor model of youth antisocial behavior. Aggressive Behavior. 2013;39:149–159. doi: 10.1002/ab.21466. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Slobodskaya H, Mar RA, Deal J, Halverson CF, Jr, Baker SR, Pavlopoulos V, Besevegis E. The hierarchical structure of childhood personality in five countries: Continuity from early childhood to early adolescence. Journal of Personality. 2012;80:1–33. doi: 10.1111/j.1467-6494.2011.00748.x. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Waldman ID, Van Hulle CA, Lahey BB. Shared genetic influences on negative emotionality and major depression/conduct disorder comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:818–827. doi: 10.1016/j.jaac.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellegen A, Ben-Porath YS, Sellbom M, Arbisi PA, McNulty JL, Graham JR. Further evidence on the validity of the MMPI-2 restructured clinical (RC) scales: Addressing questions raised by Rogers, Sewell, Harrison and Jordan and Nichols. Journal of Personality Assessment. 2006;87:148–171. doi: 10.1207/s15327752jpa8702_04. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Harkness AR. Structures of personality and their relevance to psychopathology. Journal of Abnormal Psychology. 1994;103:18–31. [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Smith GT. Personality and psychopathology. In: John OP, Robins RW, Pervin LA, editors. Handbook of Personality: Theory and Research. 3rd ed. New York: Guilford; 2008. pp. 743–769. [Google Scholar]