Abstract
Objective
Study tested whether cocaine dependent patients using cocaine or alcohol at intake or in the first few weeks of intensive outpatient treatment would benefit more from extended continuing care than patients abstinent during this period. The effect of incentives for continuing care attendance was also examined.
Methods
Participants (N=321) were randomized to: treatment as usual (TAU), TAU and Telephone Monitoring and Counseling (TMC), or TAU and TMC plus incentives (TMC+). The primary outcomes were: (1) abstinence from all drugs and heavy alcohol use, and (2) cocaine urine toxicology. Follow-ups were at 3, 6, 9, 12, 18, and 24 months.
Results
Cocaine and alcohol use at intake or early in treatment predicted worse outcomes on both measures (ps≤ .0002). Significant effects favoring TMC over TAU on the abstinence composite were obtained in participants who used cocaine (OR=1.95 [1.02, 3.73]) or alcohol (OR=2.47 [1.28, 4.78]) at intake or early in treatment. A significant effect favoring TMC+ over TAU on cocaine urine toxicology was obtained in those using cocaine during that period (OR= 0.55 [0.31, 0.95]). Conversely, there were no treatment effects in participants abstinent at baseline, and no overall treatment main effects. Incentives almost doubled the number of continuing care sessions received, but did not further improve outcomes.
Conclusion
An adaptive approach for cocaine dependence in which extended continuing care is provided only to patients who are using cocaine or alcohol at intake or early in treatment improves outcomes in this group while reducing burden and costs in lower risk patients.
Keywords: cocaine dependence, continuing care, adaptive treatment, incentives, moderators
Substance use disorders often have a chronic course, with afflicted individuals cycling through periods of abstinence, sporadic use, and heavy use (Hser, Longshore, & Anglin, 2007; McKay, 2009a; McLellan, Lewis, O’Brien, & Kleber, 2000). Wider use of effective continuing care has been recommended to increase rates of sustained recoveries and limit the severity and duration of relapse episodes that do occur (Dennis & Scott, 2007; Humphreys & Tucker, 2002; McKay, 2009a; Miller & Weisner, 2002). Continuing care interventions with longer durations and active efforts to deliver the intervention tend to show larger effects (McKay, 2009b; McKay et al., 2010; Scott & Dennis, 2009).
Although effective, extended continuing care models for substance use disorders are labor intensive and add to the cost of treatment. It is therefore important to determine which patients are most likely to benefit from these interventions. One such group may be patients who are using drugs or alcohol immediately prior to intake, or who continue to use early in treatment. For example, prior studies shown that cocaine dependent patients who are using cocaine immediately prior to treatment have worse retention and drug use outcomes than those who have stopped using (Ahmadi et al., 2009; Alterman et al., 1997; Kampman et al., 2001).
Similarly, patients who continue to use drugs or alcohol in the first few weeks of treatment are at higher risk for early dropout and poor outcomes (Higgins, Badger, & Budney, 2000; McKay et al., 1999, McKay et al., 2005; Plebani, Kampman, & Lynch, 2009; Preston et al., 1998). In a study by McKay et al. (1999), patients who continued to use cocaine or alcohol during a 4-week intensive outpatient treatment program had worse outcomes than those who remitted substance dependence during that period. However, providing coping-skills based relapse prevention continuing care to these patients produced better cocaine and alcohol use outcomes than standard care. Conversely, there were no continuing care effects in remitted patients. Alcohol use has also been reported to precipitate cocaine relapse in cocaine dependent individuals (McKay, Alterman, Rutherford, Cacciola, & McLellan, 1999).
The goal of the present study was to determine whether substance use status immediately prior to intake and during the first few weeks of treatment could be used to identify patients who would most benefit from extended continuing care. Therefore, the study was designed to develop an adaptive model of treatment (McKay, 2009a; Murphy et al., 2007), in which patient progress is used to determine whether standard care needs to be augmented to achieve optimal outcomes. Participants were patients enrolled in publicly-funded intensive outpatient programs (IOPs); all were cocaine dependent and the majority were also alcohol dependent. Therefore, it was hypothesized that participants who were actively using cocaine or alcohol at intake or in the first few weeks of treatment would have worse substance use outcomes than those who had successfully achieved initial abstinence, but would benefit to a greater degree from extended continuing care.
However, because patients with active use prior to or early in treatment are at greater risk to dropout, we also evaluated the impact of providing low-level incentives for continuing care session attendance. Incentivizing attendance has increased attendance rates in treatment for substance use disorders, although the magnitude of effects has been somewhat smaller than when abstinence is incentivized (Bride & Humble, 2008; Businelle et al., 2009; Lussier et al., 2006; Petry et al., 2006). A preliminary analysis of continuing care participation in the present study indicated that incentives dramatically increased the number of sessions attended in the first year of the follow-up (Van Horn, et al., 2011).
The extended continuing care intervention in the study, Telephone Monitoring and Counseling, included a combination of telephone and in-person sessions. The intervention includes cognitive-behavioral therapy (CBT)-like elements, such as regular monitoring of current substance use and other risk and protective factors, identification of upcoming high-risk situations, and selection and rehearsal of coping strategies; and linkage to community supports (McKay et al., 2010). The telephone is well suited for the delivery of extended continuing care, because of added convenience for patients, reductions in barriers to attending clinic-based care, and greater flexibility in scheduling sessions (McKay, 2009b). Two prior studies have shown that this intervention produces better drug and alcohol use outcomes than standard care (McKay et al., 2005; McKay et al., 2010).
In the present study, participants were cocaine dependent IOP patients (N=321) who were randomly assigned to standard care only (i.e., treatment as usual, or TAU), TAU and Telephone Monitoring and Counseling (TMC), or TAU and TMC plus incentives (TMC+), and followed for 24 months. Because many study participants were also dependent on alcohol and had a history of other drug use, the first outcome measure was abstinence from all drugs in a given follow-up period, as indicated by both urine toxicology tests and self-report, and no reported days of heavy alcohol use during the period. Cocaine urine toxicology was included as a second outcome, to provide a measure specific for cocaine use only. The following hypotheses were tested:
TMC and TMC+ will produce better outcomes than TAU.
Cocaine and alcohol use at intake or early in treatment will predict worse outcomes.
Treatment effects favoring TMC and TMC+ over TAU will be larger in participants with cocaine or alcohol use at intake or early in treatment.
Adding incentives for attendance to TMC will produce larger treatment effects.
Method
Participants
The participants were 321 adults enrolled in two publicly funded IOPs in Philadelphia who met criteria for lifetime DSM-IV cocaine dependence and had used cocaine in the 6 months prior to entering treatment. The other criteria for eligibility were a willingness to participate in research and be randomly assigned to a treatment condition; completion of two weeks of IOP; no psychiatric or medical condition that precluded outpatient treatment (i.e., severe dementia, current hallucinations); between the ages of 18 and 65; no regular IV heroin use (i.e., 3 or more times per week) within the past 12 months; ability to read at approximately the 4th grade level; and at least a minimum degree of stability in living situation (e.g., not living on the street). To facilitate follow-up, participants had to be able to provide the names, addresses, and telephone numbers of at least three contacts.
The participants were on average 43.2 (sd= 7.4) years old and had 11.6 (sd= 1.8) years of education. The majority of participants were male (76%) and African American (89%). Most met criteria for current cocaine dependence (83.2%), and a little over one-third had current alcohol dependence (38.9%). The participants used cocaine on an average of 42.2% (sd=30.7) of the days in the six months prior to baseline, and drank alcohol on 32.0% (sd= 32.8) of the days. Rates of current/lifetime dependence on other drugs were lower (cannabis—12.1%/23.7%, opiates—1.9%/8.8%, and sedatives—1.0%/3.7%). Participants averaged 4.5 (sd= 5.6) prior treatments for drug problems.
Intensive Outpatient Treatment
The IOP programs provided approximately 9 hours of group-based treatment per week, and patients could typically attend for up to 3–4 months (McKay et al., 2010). Patients who completed the IOP at these programs were typically offered 2–3 months standard outpatient treatment (i.e., one group counseling session per week) for a total of up to 6 months of treatment.
Continuing Care Treatment Conditions
Telephone monitoring and counseling (TMC)
Participants in this condition had 1–2 initial face-to-face sessions in the first week (i.e., week 3 of IOP) to orient them to the protocol. The participant and counselor decided who would initiate the calls; this decision was made on the basis of what would yield the highest contact rate, and was subject to review and change at later points. A toll free number was provided to reduce financial barriers to call completion.
Following this session, participants received brief telephone calls for up to 24 months. These 20 minute calls were offered weekly for the first 8 weeks, every other week for the next 44 weeks, once per month for 6 months, and every other month for the final 6 months. Therefore, the total number of possible scheduled calls in the protocol was 39. Each call began with a structured 13-item assessment of current substance use, HIV risk behaviors, and IOP attendance; other risk factors (e.g., craving, low self-efficacy, being in risky situations, etc.); and protective factors (e.g., attendance at self-help meetings, participation in other pro-recovery social activities, etc.), which was referred to as the progress assessment.
The CBT-based counseling was linked to the results of the progress assessment and also addressed any anticipated risky situations. Participants identified potential coping strategies and behaviors, with help from the counselor as needed, and these were briefly rehearsed during the remainder of the session. While participants were still attending IOP, and barriers to successful IOP completion were addressed. Participants were given the option of completing some of their sessions in person, rather than over the telephone, if they had difficulty in getting private access to a telephone or preferred to attend the session at the clinic. The intervention condition also included a stepped-care component, which was triggered when changes to protective and risk factors results in a negative shift of 5 points or more on the progress assessment summary score, and included additional telephone or clinic sessions (see McKay et al., 2010).
Telephone monitoring and counseling plus incentives (TMC+)
This intervention was the same as TMC, with the addition of incentives for attending sessions. Participants received a $10 gift coupon for each regularly scheduled or step care session attended in the first year, and bonus $10 gift coupons every time 3 consecutively scheduled sessions were completed. The coupons were for department stores (Walmart and Target), and a local grocery store chain.
Therapists
Seven therapists (five women and two men) delivered both TMC and TMC+. All therapists had prior experience with providing outpatient treatment for substance use disorders, ranging from 1 to 20 years. Five of the therapists had MA-level degrees in psychology or social work, one had a BA, and one had a Ph.D. in clinical psychology. Four of the therapists had provided telephone-based continuing care in a prior study (McKay et al., 2010).
Adherence to treatment protocols
The TMC and TMC+ sessions were audiotaped to facilitate supervision and monitor adherence to the protocol as described in the manuals. Individual supervision was provided weekly by the study clinical coordinator, and one group supervision session was also held per week. Any deviations from the treatment protocol identified by the clinical coordinator were immediately addressed in the weekly supervision meetings.
Procedures
Recruitment
Potential participants were screened during their first two weeks in the two IOPs by the study research technicians. Those who appeared eligible were informed that they would be given a full screening if they completed two weeks of the IOP and wanted to participate in the research study. Informed consent procedures were completed for those who appeared eligible after completing 2 weeks of IOP. A final determination of eligibility for the study was made after the baseline assessments were completed. The study was conducted in compliance with the policies of the Institutional Review Boards of the University of Pennsylvania and the City of Philadelphia. Participants were recruited between July 2007 and November 2009.
Representativeness of the study sample
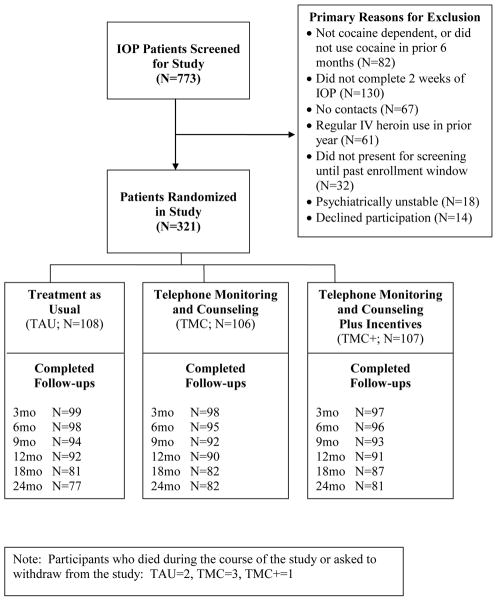
A total of 773 patients were screened at the two IOPs, and of these, 321 were eligible and willing to participate and were enrolled in the study (see Figure 1). The primary reasons for failure to enter the study were as follows: did not have lifetime cocaine dependence or had no cocaine use in the prior 6 months (82 of 452 not eligible, or 18%), stopped coming to IOP during the first two weeks of treatment (130, or 29%), had no contacts (67, or 15%), had regular IV opiate use in the prior 12 months (61, or 13%), did not present for the screening until past the window for study enrollment (32, or 7%), was psychiatrically unstable (18, or 4%), and declined participation (14, or 3%).
Figure 1.
Consort Diagram
Randomization procedures
Separate randomized allocation schemes were used at each site. Blocked randomization schemes, using blocks of size 30, were used to yield a balanced allocation of participants to the three treatment conditions at each site. The study statistician generated the sequences. The assignments were placed in envelopes by the study coordinator, and the sequence was concealed until the point of randomization.
Assessments
Baseline assessments were completed in week 3 of IOP. Follow-up assessments were conducted at 3, 6, 9, 12, 18, and 24 months post baseline. Most follow-ups were done at the research offices, with a small number conducted at other sites (i.e., prison), or over the telephone. Participants received $50 for the baseline assessment, and $50 each for the six follow-up sessions. All study interviews were conducted by experienced research personnel who were blind to the study hypotheses, but not to treatment condition. The nature of material gathered at follow-ups, informal comments made by participants, and the length of the follow-up precluded maintaining a cadre of interviewers unaware of treatment condition assignment.
Measures
Psychiatric diagnoses
The Structured Clinical Interview for DSM-IV (SCID) (First et al., 1996) was administered at baseline by MA-level clinicians to assess DSM-IV Axis I disorders. It was used to determine substance use disorder diagnoses and rule out any psychiatric disorders that would preclude study participation.
Self-reported cocaine and alcohol use
Time-line follow-back (TLFB) (Sobell, Maisto, Sobell, & Cooper, 1979) calendar assessment techniques were used to gather self-reports of cocaine and alcohol use during the 6 months preceding the baseline assessment and the 24 month follow-up period. In validity studies with drug abusers, TLFB reports of days of cocaine use were highly correlated with urine toxicology results (Ehrman & Robbins, 1994; Fals-Stewart et al., 2000). In alcoholic samples, TLFB reports of percent days abstinent have generally correlated .80 or better with collateral reports (Maisto, Sobell, & Sobell, 1979; Stout, Beattie, Longabaugh, & Noel, 1989). In cases where participants missed one or more follow-ups but then completed a subsequent follow-up, data from the missing follow-ups were obtained at the next follow-up via the TLFB calendar method.
Problem severity and other drug use
The Addiction Severity Index (ASI; McLellan, Luborsky, Woody, & O’Brien, 1980) was used to gather information on lifetime substance use and prior addiction treatment, problem severity levels at baseline in seven areas of functioning (i.e., medical, employment, drug use, alcohol use, legal, family/social, and psychiatric), and other drug use at each follow-up. The ASI has demonstrated adequate to good internal consistency, test-retest, and inter-rater reliabilities (McLellan et al., 1985).
Urine toxicology
Urine samples were obtained at baseline and at each follow-up point to provide a more objective measure of cocaine and other drug use (e.g., amphetamines, opiates, barbiturates, benzodiazepines, and THC). The samples were tested at the Philadelphia Veterans Affairs Medical Center laboratory with a homogenous enzyme immunoassay method, using established cutoffs for drug positive results.
Outcome measures
Because many of the participants were abusing or dependent on other drugs or alcohol in addition to cocaine, the primary substance use outcome was a dichotomous measure of good overall substance use outcomes (i.e., “abstinence composite”). To be considered abstinent on this measure in a given segment of the follow-up (3 month periods in months 1–12, 6 month periods in months 13–24), the participant had to have (1) no cocaine use, (2) no use of other drugs of abuse, and (3) no heavy alcohol use (i.e., 5 or more drinks/day for men, 4 or more drinks/day for women).
The measure was operationalized in the following manner. Information from the TLFB was considered first. Any cocaine use or heavy alcohol use reported on the TLFB generated a non-abstinent score for that follow-up period. Next, urine toxicology data and ASI drug use data were considered in participants who had provided that data at the follow-up point and reported no cocaine use or heavy drinking on the TLFB. A positive urine toxicology result on any of the 5 substances or reports of any days of drug use on the ASI placed the participant in the non-abstinent category for that period. Sensitivity analyses were done in which missing urine toxicology or ASI data in participants who reported no cocaine use or heavy alcohol use on the TLFB for that period also resulted in a non-abstinent score on the composite. Since this did not produce any differences in results, the original operationalization was retained. Cocaine urine toxicology alone was included to provide an outcome measure specific for cocaine use.
Moderator measures
The two moderators were dichotomous indicators of whether participants had used any cocaine or any alcohol over the 30 days prior to baseline, derived from the TLFB and ASI. These measures were dichotomous, rather than continuous, due to the skewed nature of their distributions. A little less than half the participants reported any cocaine use during this period, and about one-third reported any alcohol use.
Participation in standard care
The TLFB was also used to gather data on days of out-patient substance abuse treatment received by participants in the study.
Follow-Up Rates
The follow-up rates at each follow-up point were as follows: 3 months, 79.4%; 6 months, 76.9%; 9 months, 71.7%; 12 months, 72.9%; 18 months, 71.0%; and 24 months, 74.8%. When TLFB data from subsequent follow-up points were used to backfill prior missing follow-ups, the TLFB follow-up rates were: 3 months, 91.6%; 6 months, 90.0%; 9 months, 86.9%; 12 months, 85.0%; 18 months, 77.9%; and 24 months, 74.8%. The three treatment conditions did not differ significantly on follow-up rates at any point.
Data Analyses
Differences between the three conditions at baseline were evaluated with one-way ANO-VAs (continuous measures) and chi-square tests (categorical measures). Treatment differences in number of days on which intensive outpatient treatment sessions were received were also evaluated with one-way ANOVAs.
Generalized estimating equations (GEE; SAS PROC GENMOD) were used to compare the continuing care conditions on the binary abstinence composite and urine toxicology outcome measures at 3, 6, 9, 12, 18, and 24 months in intent-to-treat analyses. Time was modeled as a categorical factor with six levels. Preliminary analyses indicated site did not interact with treatment condition or the moderator variables, but it did predict both outcomes and so was included as a covariate in all analyses. In the treatment condition main effect analyses, the independent variables were treatment condition, time, and treatment x time interactions. The moderator analyses also included the moderator variable, moderator x treatment interactions, moderator x time interactions, and moderator x treatment x time interactions. However, the moderator x time and 3-way interactions did not approach significance in any of these analyses, and were therefore removed. Focused contrasts were used to compare the three treatment conditions at each level of the moderators. Finally, pattern mixture analyses (Hedeker & Gibbons, 1997) were conducted to evaluate the potential effects of non-ignorably missing data on the two outcomes.
Results
Comparison of Treatment Conditions at Baseline
Participants in the three treatment conditions were compared on 22 demographic, diagnostic, treatment, and problem severity level variables assessed at baseline. These data are presented in Table 1. The conditions did not differ significantly on any of these variables. Analyses were also done within the subgroups of patients who used cocaine or alcohol immediately prior to or early in IOP to compare the treatment conditions on substance use measures at baseline (e.g., number of prior treatments for drug and alcohol use disorders, frequency of cocaine and alcohol use in the prior 6 months, drug and alcohol problem severity in the prior 30 days, and urine toxicology) and gender. None of these comparisons approached significance.
Table 1.
Characteristics of Sample at Baseline
| TAU N=108 | TMC N=106 | TMC+ N=107 | F or Chi-sq | P Value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Race - % (N) | 5.02 | .29 | |||
| African American | 90.7 (97) | 84.0 (89) | 91.6 (98) | ||
| White | 7.5 (8) | 9.4 (10) | 5.6 (6) | ||
| Other | 1.9 (2) | 6.6 (7) | 2.8 (3) | ||
| Gender - % male (N) | 75.9 (82) | 75.5 (80) | 77.6 (83) | 0.14 | .93 |
| Age – m (sd) | 42.9 (8.0) | 43.3 (7.8) | 43.4 (6.48) | 0.13 | .87 |
| Education – m (sd) | 11.4 (1.9) | 11.8 (1.6) | 11.5 (1.8) | 1.66 | .19 |
| Ever Married-- % (N) | 38.9 (42) | 41.5 (44) | 38.3 (41) | 0.26 | .88 |
| Substance Use | |||||
| Prior treatments for drug - m (sd) | 4.4 (5.2) | 4.4 (5.7) | 4.6 (5.9) | 0.05 | .95 |
| Years of regular cocaine use – m (sd) | 14.9 (7.6) | 14.3 (7.7) | 15.9 (7.4) | 1.16 | .32 |
| Years of regular alcohol use – m (sd) | 13.7 (11.1) | 14.0 (11.0) | 16.6 (11.5) | 2.16 | .12 |
| Substance use in prior 6 months | |||||
| % days cocaine – m (sd) | 43.4 (31.3) | 41.7 (31.2) | 41.4 (29.7) | 0.14 | .87 |
| % days alcohol – m (sd) | 29.6 (33.4) | 34.1 (33.2) | 32.3 (31.9) | 0.51 | .60 |
| Current Diagnosis Prior to Treatment | |||||
| Cocaine dependence - % (N) | 81.5 (88) | 84.0 (89) | 84.1 (90) | 0.34 | .85 |
| Alcohol dependence - % (N) | 32.4 (35) | 38.7 (41) | 45.8 (49) | 4.06 | .13 |
| Current Substance Use | |||||
| Any cocaine in prior 30 days - % (N) | 47.2 (51) | 40.6 (43) | 40.2 (43) | 1.38 | .50 |
| Any alcohol in prior 30 days - % (N) | 35.2 (38) | 33.0 (35) | 34.6 (37) | 0.12 | .94 |
| ASI drug composite – m (sd) | 0.15 (.07) | 0.15 (.07) | 0.15 (.08) | 0.30 | .74 |
| ASI alcohol composite – m (sd) | 0.16 (.20) | 0.14 (.18) | 0.18 (.19) | 1.12 | .33 |
| Other Problem Severities | |||||
| Living with person who encourages substance use % (N) | 17.6 (19) | 17.0 (18) | 19.6 (21) | 0.28 | .88 |
| ASI Composites – m (SD) | |||||
| Medical | 0.40 (.35) | 0.41 (.37) | 0.43 (.36) | 0.13 | .88 |
| Employment | 0.92 (.14) | 0.89 (.17) | 0.91 (.14) | 1.25 | .29 |
| Legal | 0.10 (.15) | 0.11 (.18) | 0.07 (.14) | 1.77 | .17 |
| Family/Social | 0.20 (.22) | 0.24 (.22) | 0.20 (.23) | 1.31 | .27 |
| Psychiatric | 0.25 (.21) | 0.21 (.21) | 0.28 (.23) | 2.63 | .08 |
Participation in Outpatient Treatment
Over the first six months of the follow-up, participants averaged 30 days on which they received IOP or OP sessions (range 0 to 76, sd=15.7), with no difference between the treatment conditions [mean days TAU = 30.8, TMC = 29.0, TMC+ = 30.5; F(2,281)= .38, p= .69].
Participation in TMC and TMC+
In TMC, 77 of 106 participants (72.6%) completed the orientation session and were eligible to receive continuing care sessions. In the TMC+ condition, 89 of the 107 participants (83.2%) completed orientation. The mean number of continuing care sessions received by participants who completed their orientations was 15.5 (SD= 14.1) in TMC and 26.0 (SD= 12.8) in TMC+ [F(1,164)= 26.30, p< .0001]. The mean duration of sessions was 21.1 minutes (SD= 13.6) in TMC and 20.1 minutes (SD= 11.8) in TMC+. The percentage of sessions completed in person, as opposed to over the telephone, was 46.4% in TMC and 42.4% in TMC+. In person sessions were longer than telephone sessions (25.9 min vs. 16.4 min, respectively). Only a small proportion of in person sessions (8.2%) immediately followed a step-up recommendation. Therefore, most in person sessions indicated patient preference, rather than a therapist recommendation for stepped care. Participants in TMC+ who had completed an orientation earned an average of 24.7 vouchers (sd=13.7)
Adherence to Treatment Manuals
All sessions were recorded and 5% were randomly selected and scored for adherence to the manuals (191 of 3428 sessions), using a 12-item checklist developed in a prior study (McKay et al., 2010). Ratings were performed by the clinical supervisor and therapists trained in the protocol who had not provided clinical services in the study. Overall, the treatments were provided in a manner highly consistent with the protocol, with little difference between the conditions. The only significant differences were that therapists were more likely to ask the patient to anticipate upcoming high-risk situations in TMC+ than in TMC [93% vs. 77% of sessions coded; chi-square (1)= 10.6, p< .01], and were more likely to refer the patient to their IOP counselor for a particular issue in TMC than in TMC+ [14% vs. 4%; chi-square (1)=5.6, p< .05].
Treatment Condition Main Effects
Data from each of the two outcome measures are presented in Table 2. Rates of good outcomes on the abstinence composite were about 50% at the 3-month follow-up and declined by about 10 percentage points by the 24-month follow-up (time effect p= .01). Rates of cocaine positive urines were around 25% at 3 months and rose to about 30% by month 24 (time effect ns). None of the treatment group comparisons on either outcome was significant (see Table 3).
Table 2.
Main Effect Outcomes
| Month 3 | Month 6 | Month 9 | Month 12 | Month 18 | Month 24 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abstinence Composite | ||||||||||||||||||
| Abstinent | Abstinent | Abstinent | Abstinent | Abstinent | Abstinent | |||||||||||||
| N | Prop | (N) | N | Prop | (N) | N | Prop | (N) | N | Prop | (N) | N | Prop | (N) | N | Prop | (N) | |
|
|
||||||||||||||||||
| TAU (N=108) | 99 | .44 | (44) | 98 | .44 | (43) | 93 | .46 | (43) | 91 | .37 | (34) | 81 | .36 | (29) | 77 | .32 | (25) |
| TMC (N=106) | 97 | .58 | (56) | 91 | .43 | (42) | 87 | .41 | (36) | 88 | .41 | (36) | 83 | .35 | (29) | 82 | .41 | (34) |
| TMC+ (N=107) | 97 | .47 | (46) | 94 | .43 | (40) | 92 | .42 | (39) | 91 | .44 | (40) | 85 | .38 | (32) | 80 | .36 | (29) |
| Cocaine Urine Toxicology | ||||||||||||||||||
| Positive | Positive | Positive | Positive | Positive | Positive | |||||||||||||
| N | Prop | (N) | N | Prop | N | N | Prop | (N) | N | Prop | (N) | N | Prop | (N) | N | Prop | (N) | |
|
|
||||||||||||||||||
| TAU (N=108) | 89 | .31 | (28) | 82 | .26 | (21) | 74 | .30 | (22) | 76 | .37 | (28) | 67 | .33 | (22) | 69 | .38 | (26) |
| TMC (N=106) | 76 | .22 | (17) | 76 | .24 | (18) | 69 | .25 | (17) | 73 | .27 | (20) | 72 | .29 | (21) | 80 | .26 | (21) |
| TMC+ (N=107) | 83 | .20 | (17) | 83 | .28 | (23) | 78 | .29 | (23) | 77 | .27 | (21) | 80 | .24 | (19) | 75 | .35 | (26) |
N= number followed up; Prop = proportion abstinent (abstinence composite) or proportion with a cocaine positive urine; (N)= number abstinent (abstinence composite) or number with a cocaine positive urine.
Table 3.
Treatment Condition Main Effects
| Outcome | TX Group (df=2) | Time (df=5) | Group X Time (df=10) | TMC vs. TAU | TMC+ vs. TAU | TMC+ vs. TMC |
|---|---|---|---|---|---|---|
| Abstinence Composite | X2= 0.19 p= .91 |
X2= 14.97 p= .01 |
X2= 8.71 p= .56 |
z= 0.44 p= .66 |
z= 0.22 p= .83 |
z= −0.21 p= .83 |
| Cocaine Urine Toxicology | X2= 1.82 p= .40 |
X2= 7.88 p= .16 |
X2= 6.68 p= .76 |
z= −1.31 p= .19 |
z= −0.95 p= .34 |
z= 0.39 p= .69 |
Effects of Cocaine and Alcohol Use at Intake and Early in Treatment
Cocaine use
Of the 137 participants who used cocaine in the 30 days prior to baseline, 46.3% used during IOP, 22.1% used both during and prior to IOP, and 31.6% used prior to IOP only. Participants in this group had much worse outcomes on both the abstinence composite (p< .0001) and cocaine urine toxicology (p< .0001) than the cocaine abstinent participants (see Table 4). The interaction between treatment condition and cocaine use in the 30 days prior to baseline was significant at the level of a trend (p= .07) with the abstinence composite but not with cocaine urine toxicology (p= .13).
Table 4.
Subgroup Analyses
| Outcome | Moderator | Moderator Effect | Moderator x Treatment | Current Use | TMC vs. TAU | TMC+ vs. TAU | TMC+ vs. TMC |
|---|---|---|---|---|---|---|---|
| Abstinence Composite | Cocaine Use | x2=28.78 p< .0001 |
x2=5.28 p= .071 |
Yes | z= 2.03 p= .042 |
z= 1.48 p= .139 |
z= −0.63 p= .531 |
| No | z= −0.87 p= .385 |
z= −1.04 p= .297 |
z= −0.25 p= .803 |
||||
| Alcohol Use | x2=15.91 p< .0001 |
x2=6.38 p= .041 |
Yes | z= 2.69 p= .007 |
z= 1.69 p= .091 |
z= −1.08 p= .282 |
|
| No | z= −0.68 p= .500 |
z= −0.47 p= .641 |
z= 0.17 p= .866 |
||||
| Cocaine Urine Toxicology | Cocaine Use | x2=14.24 p= .0002 |
x2=4.05 p= .132 |
Yes | z= −1.23 p= .218 |
z= −2.13 p= .033 |
z= −0.70 p= .483 |
| No | z= −0.58 p= .562 |
z= 0.76 p= .448 |
z= 1.36 p= .175 |
||||
| Alcohol Use | x2=12.06 p= .0005 |
x2=0.08 p= .962 |
Yes | z= −0.84 p= .401 |
z= −0.88 p= .376 |
z= 0.00 p= .999 |
|
| No | z= −1.10 p= .271 |
z= −0.73 p= .468 |
z= 0.41 p= .684 |
Current use= use (yes/no) in 30 days prior to baseline (a period covering the week prior to IOP through the first 3 weeks of IOP). Moderator Effect refers to effect of moderator variable on the outcome variables. Moderator x Treatment refers to the effect of this interaction on the outcome variables.
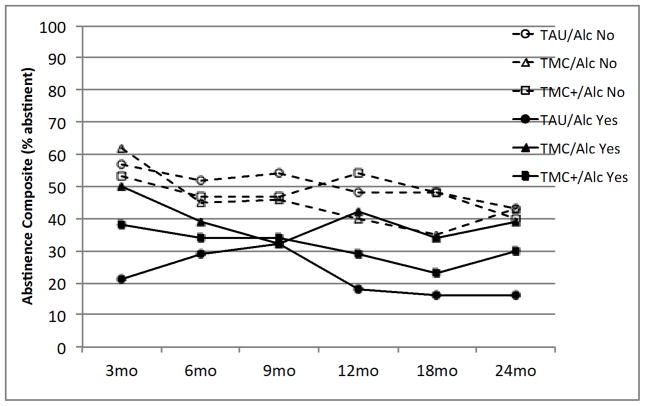
Focused contrasts indicated that among participants with some cocaine use at baseline, outcomes on the abstinence composite were better in TMC than in TAU (OR= 1.95 [1.02, 3.37], p= .04), whereas TMC+ and TAU did not differ (OR= 1.58 [0.86, 2.91], p= .14). Rates of cocaine positive urine test were lower in TMC+ than in TAU (OR= 0.55 [0.31, 0.95], p= .03), whereas TMC and TAU did not differ on this outcome (OR= 0.68 [0.37, 1.25], p= .22). There were no differences between TMC+ and TMC on either outcome. Among participants with no cocaine use in the 30 days prior to baseline, none of the treatment group contrasts with either outcome measure was significant (see Table 4). These effects are illustrated in Figures 2 and 3.
Figure 2.
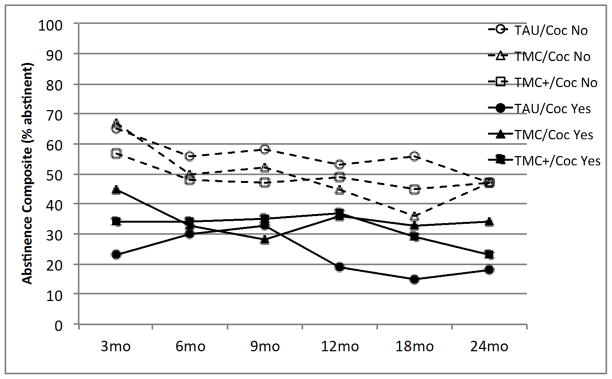
Moderating effect of baseline cocaine use on abstinence composite outcomes. Solid lines indicated cocaine use in 30 days prior to baseline, dashed lines indicate no cocaine use in that period. In patients with recent cocaine use, TMC produced higher rates of abstinence than TAU (p< .05), whereas the comparisons of TMC+ vs. TAU (p= .14) and TMC+ vs. TMC (p= .53) were not significant. There were no significant treatment group differences in patients cocaine abstinent in the 30 days prior to baseline.
Figure 3.
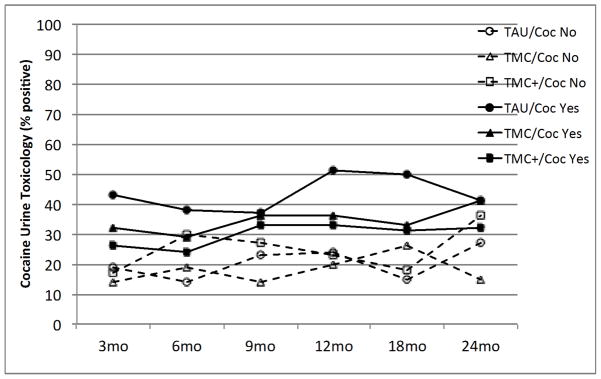
Moderating effect of baseline cocaine use on cocaine urine toxicology outcomes. Solid lines indicated cocaine use in 30 days prior to baseline, dashed lines indicate no cocaine use in that period. In patients with recent cocaine use, TMC+ produced higher rates of abstinence than TAU (p< .05), whereas the comparisons of TMC vs. TAU (p= .22) and TMC+ vs. TMC (p= .48) were not significant. There were no significant treatment group differences in patients cocaine abstinent in the 30 days prior to baseline.
Alcohol use
Of the 110 participants who used alcohol in the 30 days prior to baseline, 45.9% drank during IOP, 27.0% drank both during and prior to IOP, and 27.0% drank prior to IOP only. Participants in this group also had worse outcomes on the abstinence composite (p< .0001) and cocaine urine toxicology (p= .0005) than the alcohol abstinent participants. The interaction between treatment condition and alcohol use in the 30 days prior to baseline was significant with the abstinence composite (p= .04), but not with cocaine urine toxicology (p= .96).
Focused contrasts indicated that in participants with alcohol use in the prior 30 days, scores on the abstinence composite were higher in TMC than in TAU (OR= 2.47 [1.28, 4.78], p= .007). Abstinence rates were higher in TMC+ than TAU at the level of a trend (OR= 1.71 [0.92, 3.17], p= .09). However, neither TMC nor TMC+ was superior to TAU on cocaine urine toxicology. Moreover, there was no difference between TMC+ and TMC on either outcome. In participants with no alcohol use in the prior 30 days, there were no significant differences between the treatment conditions on either outcome (see Table 4). These effects on the abstinence composite are illustrated in Figure 4.
Figure 4.
Moderating effect of baseline alcohol use on abstinence composite outcomes. Solid lines indicated alcohol use in 30 days prior to baseline, dashed lines indicate no alcohol use in that period. In patients with recent alcohol use, TMC produced higher rates of abstinence than TAU (p< .01), whereas the comparisons of TMC+ vs. TAU (p= .09) and TMC+ vs. TMC (p= .28) were not significant. There were no significant treatment group differences in patients alcohol abstinent in the 30 days prior to baseline.
Cocaine or alcohol use
Of the participants with cocaine use at baseline, 73.4% also had alcohol use. Of those with alcohol use at baseline, 91.8% also had cocaine use. Because these measures were clearly not independent, the moderating effect of any use of cocaine or alcohol was also examined. With the abstinence composite outcome, these analyses yielded the same results as the separate analyses of baseline cocaine and alcohol use (i.e., significant effects favoring TMC over TAU in the group with any use). However, with the cocaine urine toxicology outcome the results favoring TMC+ over TAU in the any use group were significant only at the level of a trend (p< .10).
Effects of Missing Data
The potential impact of missing follow-up data was examined in pattern mixture analyses. All participants were categorized as either research completers or dropouts. This term did not predict either of the two outcomes (p> .90) and did not interact with treatment condition to predict outcomes (p> .50). In two of the moderator analyses, the 3-way interaction of treatment condition by moderator by dropout status approached significance (p< .10). In each case, the interaction was accounted for by the TAU condition. In TAU participants abstinent at baseline, outcomes were better in research dropouts than in completers. Conversely, in those with active substance use at baseline, outcomes in TAU were better in completers than in dropouts. No effects were apparent in either TMC or TMC+. The same ordering of treatment conditions in Figures 2–4 was obtained in both the research completers and dropouts. Therefore, missing data did not appear to influence the outcomes.
Discussion
This study evaluated an adaptive treatment model for cocaine dependence, in which substance use status at intake and in the first few weeks of treatment was used to identify patients who most benefited from extended continuing care. The impact of providing low level incentives for continuing care attendance was also evaluated. The participants all met criteria for cocaine dependence (lifetime) and were typical of patients in publicly-funded addiction treatment programs, in that many also had alcohol dependence, were using other drugs, and had multiple prior treatments for drug dependence (McKay et al., 2005; Scott & Dennis, 2009). Many of the participants also had significant employment, social, and psychiatric problems.
Cocaine and alcohol use immediately prior to or during the first few weeks of IOP was reported by 43% and 34%, respectively, of the participants, with about one-third reporting use prior to IOP, and two-thirds reporting use during IOP or both prior to and during IOP. Participants with cocaine or alcohol use during this period had much worse outcomes over 24 months on a composite abstinence measure that included cocaine use, other drug use, and heavy alcohol use; and on a separate cocaine urine toxicology measure. These findings replicate several prior studies (Alterman et al., 1997; Higgins et al., 2000; Kampman et al., 2001; McKay et al., 1999; McKay et al., 2005; Plebani et al., 2009), which have demonstrated that substance use status at intake and in the first few weeks of treatment predicts poorer longer-term outcomes.
However, these high-risk patients clearly benefited from extended continuing care. Specifically, TMC produced significantly better outcomes than standard care on the abstinence composite for those with any cocaine or alcohol use at baseline, and TMC+ produced significantly better cocaine urine toxicology outcomes than standard care for those with cocaine use at baseline. Therefore, both cocaine and alcohol use immediately prior to or early in treatment moderated the continuing care effect on the outcome that included cocaine, other drug, and heavy alcohol use, whereas only cocaine use in this period moderated treatment response on the outcome specific to cocaine use. As is shown in Figures 2–4, these effects were sustained to the end of the 24 month follow-up. Conversely, there were no treatment group effects in patients who were abstinent from cocaine and alcohol in the 30 days prior to baseline.
These findings suggest that providing extended continuing care to cocaine dependent patients in intensive outpatient programs who are using cocaine or alcohol at the time of intake or in the first few weeks of treatment, rather than to all patients, may be a cost-effective strategy for improving long-term outcomes. In such an adaptive model (McKay, 2009a; Murphy et al., 2007), patients who have drug positive urine samples at intake to treatment or who report active drug or alcohol use in the prior week would be referred to extended continuing care, which would augment and extend standard care. Patients who are abstinent at intake but provide drug positive urines or report use during the first 2–3 weeks of treatment would also be referred to extended continuing care. Conversely, patients who were abstinent over this period would receive standard, shorter-term treatment.
The treatment effect favoring TMC over TAU on the abstinence composite was largest in patients using alcohol in the 30 days prior to baseline (OR=2.47). Almost all of these patients (92%) were also using cocaine during this period, which meant that this group was largely comprised of patients who used both cocaine and alcohol at intake or early in treatment. Prior studies found that patients with co-occurring cocaine and alcohol dependence have worse outcomes than those dependent on only one substance (Carroll, Rounsaville, & Bryant 1993; McKay et al., 2005). This may explain why extended continuing care was particularly helpful for this group.
These findings are consistent with the results of an earlier continuing care study (McKay et al., 1999), which found that patients in a 4 week IOP who continued to use cocaine or alcohol during IOP benefited from a coping skills-based relapse prevention intervention, whereas those who achieved remission during that period did equally well in that intervention or standard care. Another recent study with cocaine dependent patients also found that abstinence status at or within a few days of intake could be used in an adaptive protocol to identify which patients would benefit from augmented treatment (Petry, Barry, Alessi, Rounsaville, & Caroll, 2012). In this study, high magnitude incentives ($560) for abstinence improved outcomes for patients who had a cocaine positive urine at or within a few days of intake. Conversely, patients abstinent at the start of treatment benefited equally from lower magnitude incentives ($250) for either attendance or abstinence. However, these group differences were no longer present at a 9 month follow-up, which suggests the effects in this study were of relatively short duration.
The present study also examined whether providing low-level incentives for continuing care attendance would increase sustained participation in the intervention and lead to better outcomes. Results indicated the version of the continuing care intervention that included incentives (i.e., TMC+) produced significantly lower rates of cocaine positive urines than standard care in patients who were using cocaine at baseline, whereas TMC did not. However, there was clearly no advantage for TMC+ over TMC on the abstinence composite measure, which is probably the more clinically informative outcome for this population, as it combined urine toxicology and self-report data for cocaine, other drugs, and alcohol. Moreover, TMC+ did not produce significantly better outcomes than TMC in any of the analyses, and there were no main effects favoring TMC+ over standard care in the full sample.
The failure of incentive to further improve outcomes likely reflects the fact that continuing care participation was incentivized rather than abstinence. Because the majority of the continuing care contacts were completed over the telephone, it was not possible to collect urine samples on a frequent basis and incentivize toxicology results. A ceiling effect may also have been present, in which attendance at more than 15–20 continuing care sessions over a 24 month period does not further improve outcomes. However, it may also be that providing incentives for attendance diminished the impact of the sessions, perhaps because some participants in that condition were completing telephone contacts primarily to earn the incentives. In a recent study by Litt et al. (2009), adding incentives for completing between session tasks to a treatment designed to increase social support produced worse drinking outcomes than the same treatment without incentives, as well as lower self-efficacy.
Contrary to the first hypothesis of the study, there were no significant main effects favoring TMC and TMC+ over TAU. This was largely because outcomes in patients who were not using cocaine or alcohol in the 30 days prior to baseline actually favored standard care over the two extended continuing care interventions, though not significantly. We had expected smaller treatment effects in this group of treatment responders, but not effects in the opposite direction. These findings suggest that extended continuing care may actually be contraindicated in patients who have managed to stop using alcohol and drugs immediately prior to and in the first weeks of treatment. It is possible that for these patients, the addition of the continuing care sessions on top of the IOP treatment they were receiving—and responding to—may have in some way diluted the positive effects of the IOP.
There has been little prior research on the potential negative implications of over treatment. One study found that among substance abuse patients “overmatched” to treatment (i.e., received residential when appropriate for IOP), rates of no-shows were higher in women, in those with supportive family environments, and in those with anxiety disorders (Angarita et al., 2007). A recent meta-analysis of research on self-determination theory found that promoting patients’ autonomy was correlated with greater intrinsic motivation and autonomous self-regulation, and also promoted better mental and physical health outcomes (Ng et al., 2012). These studies raise the possibility that providing extended interventions to treatment responders could reduce feelings of autonomy and self-efficacy, and perhaps shift the degree to which success is attributed to the program rather than to the individual. Potential mediation effects will be examined in a separate report.
Finally, the lack of main effects favoring TMC and TMC+ over TAU in the full sample at first glance appears inconsistent with the results of a recent study of TMC for alcohol dependence (McKay et al., 2010). However, in that study participants all had current dependence at intake, and baseline frequency of use was consequently higher than in the present study (63% days alcohol use vs. 42% days cocaine use and 32% days alcohol use in the current study). Therefore, the results in the present study in the subgroup that was actively using at intake or early in treatment are consistent with results obtained in the prior study, which required current dependence at intake to treatment (McKay et al., 2010).
Study Strengths and Limitations
The study had a number of strengths, including a randomized design, the inclusion of patients from “real world” publicly funded addiction treatment programs, a relatively large sample size, documented adherence to the treatment manuals (Carroll et al., 2000), availability of both self-report and biological outcome data, six outcome assessments over a 24 month period, and a good follow-up rate. At the same time, the study had several limitations. The sample consisted largely of middle-aged, African American men with cocaine dependence and high rates of co-occurring alcohol and marijuana use disorders. The results may not generalize to other populations, such as younger patients, or those with primary methamphetamine or prescription drug abuse or dependence. Participants were given the option of attending some continuing care sessions in person, rather than over the telephone. Despite the convenience of telephone sessions, over 40% of the sessions were completed in person, which speaks to the appeal of face-to-face contact with a counselor. We therefore tested hybrid models of continuing care, which included both telephone and face-to-face sessions. The same results might not have been obtained in a pure call center model, in which all continuing care sessions are provided over the telephone.
The continuing care interventions were delivered by counselors who did not provide the IOP intervention to study participants, and who did not work in the IOPs. It is conceivable that using IOP counselors to provide continuing care may increase the patients’ experience of continuity of care, and thereby further increase the effectiveness of the intervention. Finally, the results in the present study were obtained in participants who also managed to complete at least two weeks of IOP. It is not clear that telephone-based continuing care would be effective with patients who drop out of IOP in the first two weeks.
Final Conclusions
The results of this study indicate that adding extended continuing care that combines brief telephone and in-person sessions to intensive outpatient treatment can improve longer-term substance use outcomes for cocaine dependent patients who are actively using cocaine or alcohol immediately prior to or in the first weeks of treatment. Conversely, patients who are able to refrain from cocaine or alcohol use in this period do at least as well with IOP alone. The provision of low-level incentives for attendance dramatically increases the number of continuing care sessions received, but it clearly does not produce better substance use outcomes than the same intervention without incentives and, moreover, adds to the cost. It may therefore be possible to maximize the effectiveness of extended continuing care for cocaine dependence and limit costs by implementing an adaptive treatment model in which extended continuing care without incentives for attendance is provided only to those patients who are actively using cocaine or alcohol immediately prior to or in the first few weeks of outpatient treatment.
Acknowledgments
This research was supported by grants R01 DA020623, K02 DA000361, and K24 DA029062 from the National Institute on Drug Abuse. Additional support was provided by the Center of Excellence in Substance Abuse Treatment and Education of the Department of Veterans Affairs. We thank the management and clinical staffs at NorthEast Treatment Centers and Presbyterian Hospital for collaborating on this research project and providing access to patients in their programs.
Contributor Information
James R. McKay, University of Pennsylvania and the Philadelphia Veterans Affairs Medical Center
Deborah Van Horn, University of Pennsylvania and the Philadelphia Veterans Affairs Medical Center.
Kevin G. Lynch, University of Pennsylvania
Megan Ivey, University of Pennsylvania.
Mark S. Cary, University of Pennsylvania
Michelle Drapkin, University of Pennsylvania and the Philadelphia Veterans Affairs Medical Center.
Donna M. Coviello, University of Pennsylvania
Jennifer G. Plebani, University of Pennsylvania
References
- Ahmadi J, Kampman KM, Oslin DM, Pettinati HM, Dackis C, Sparkman T. Predictors of treatment outcome in outpatient cocaine and alcohol dependence treatment. American Journal of Addictions. 2009;18:81–86. doi: 10.1080/10550490802545174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alterman AI, Kampman K, Boardman CR, Cacciola JS, Rutherford MJ, McKay JR, Maany IA. Cocaine-positive baseline urine predicts outpatient treatment attrition and failure to attain initial abstinence. Drug and Alcohol Dependence. 1997;46:79–85. doi: 10.1016/s0376-8716(97)00049-5. [DOI] [PubMed] [Google Scholar]
- Angarita GA, Reif S, Pirad S, Lee S, Sharon E, Gastfriend DR. No-show for treatment in substance abuse patients with comorbid symptomatology: Validity results from a controlled trial of the ASAM Patient Placement Criteria. Journal of Addiction Medicine. 2007;1:79–87. doi: 10.1097/ADM.0b013e3180634c1d. [DOI] [PubMed] [Google Scholar]
- Bride BE, Humble MN. Increasing retention of African-American women on welfare in outpatient substance user treatment using low-magnitude incentives. Substance Use and Misuse. 2008;43:1016–1026. doi: 10.1080/10826080801914154. [DOI] [PubMed] [Google Scholar]
- Businelle MS, Rash CJ, Burke RS, Parker JD. Using vouchers to increase continuing care participation in veterans: Does magnitude matter? American Journal of Addiction. 2009;18:122–129. doi: 10.1080/10550490802545125. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter TL, Ball SA, Fenton L, Rounsaville BJ. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug and Alcohol Dependence. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Bryant KJ. Alcoholism in treatment-seeking cocaine abusers: Clinical and prognostic significance. Journal of Studies on Alcohol. 1993;54:199–208. doi: 10.15288/jsa.1993.54.199. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK. Managing addiction as a chronic condition. Addiction Science and Clinical Practice. 2007 Dec;:45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrman RN, Robbins SJ. Reliability and validity of six-month timeline reports of cocaine and heroin use in a methadone population. Journal of Consulting and Clinical Psychology. 1994;62:843–850. doi: 10.1037//0022-006x.62.4.843. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders—patient edition. Biometrics Research Department, New York State Psychiatric Institute; NY: 1996. (SCID-I/P, version 2.0) [Google Scholar]
- Hedeker D, Gibbons R. Applications of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods. 1997;2:64–78. [Google Scholar]
- Higgins ST, Badger GJ, Budney AJ. Initial abstinence and success in achieving longer term cocaine abstinence. Experimental and Clinical Psychopharmacology. 2000;8:377–386. doi: 10.1037//1064-1297.8.3.377. [DOI] [PubMed] [Google Scholar]
- Hser YI, Longshore D, Anglin MD. The life course perspective on drug use: a conceptual framework for understanding drug use trajectories. Evaluation Review: A journal of Applied Social Research. 2007;31:515–547. doi: 10.1177/0193841X07307316. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Tucker JA. Toward more responsive and effective intervention systems for alcohol-related problems. Addiction. 2002;97:126–132. doi: 10.1046/j.1360-0443.2002.00004.x. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Changing network support for drinking: Network support project 2-year follow-up. Journal of Consulting and Clinical Psychology. 2009;77:229–242. doi: 10.1037/a0015252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Sobell LC, Sobell MB. Comparison of alcoholics’ self-reports of drinking behavior with reports of collateral informants. Journal of Consulting and Clinical Psychology. 1979;47:106–122. [PubMed] [Google Scholar]
- McKay JR. Treating substance use disorders with adaptive continuing care. Washington DC: American Psychological Association; 2009a. [Google Scholar]
- McKay JR. Continuing care research: What we’ve learned and where we’re going. Journal of Substance Abuse Treatment. 2009b;36:131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Alterman AI, Cacciola JS, O’Brien CP, Koppenhaver JM, Shepard Continuing care for cocaine dependence: Comprehensive 2-year outcomes. Journal of Consulting and Clinical Psychology. 1999;67:420–427. doi: 10.1037//0022-006x.67.3.420. [DOI] [PubMed] [Google Scholar]
- McKay JR, Alterman AI, Rutherford MJ, Cacciola JS, McLellan AT. The relationship of alcohol use to cocaine relapse in cocaine dependent patients in an aftercare study. Journal of Studies on Alcohol. 1999;60:176–180. doi: 10.15288/jsa.1999.60.176. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Pettinati HM. The effectiveness of telephone based continuing care for alcohol and cocaine dependence: 24 month outcomes. Archives of General Psychiatry. 2005;62:199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Ratichek S, Morrison R, Koppenhaver J, Pettinati HM. The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12 month outcomes. Journal of Consulting and Clinical Psychology. 2004;72:967–979. doi: 10.1037/0022-006X.72.6.967. [DOI] [PubMed] [Google Scholar]
- McKay JR, Van Horn D, Oslin D, Lynch KG, Ivey M, Ward K, Drapkin M, Becher J, Coviello D. A randomized trial of extended telephone-based continuing care for alcohol dependence: Within treatment substance use outcomes. Journal of Consulting and Clinical Psychology. 2010;78:912–923. doi: 10.1037/a0020700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Van Horn D, Morrison R. Telephone continuing care for adults. Center City MN: Hazelden Foundation Press; 2010. [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr H, O’Brien CP. New data from the Addiction Severity Index: Reliability and validity in three centers. Journal of Nervous and Mental Disease. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients: The Addiction Severity Index. Journal of Nervous and Mental Disease. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Miller WR, Weisner C. Integrated care. In: Miller WR, Weisner CM, editors. Changing substance abuse through health and social systems. New York: Kluwer Academic/Plenum; 2002. pp. 243–253. [Google Scholar]
- Murphy SA, Lynch KG, McKay JR, Oslin DW, Ten Have TR. Developing adaptive treatment strategies in substance abuse research. Drug and Alcohol Dependence. 2007;88:S24–S30. doi: 10.1016/j.drugalcdep.2006.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng JYY, Ntoumanis N, Thogersen-Ntoumani C, Deci EL, Ryan RM, Duda JL, Williams GC. Self-determination theory applied to health contexts: A meta-analysis. Perspectives on Psychological Sciences. 2012;7:325–340. doi: 10.1177/1745691612447309. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Carroll KM, Hanson T, MacKinnon S, Rounsaville B, Sierrra S. Contingency management treatments: Reinforcing abstinence versus adherence with goal-related activities. Journal of Consulting and Clinical Psychology. 2006;74:592–601. doi: 10.1037/0022-006X.74.3.592. [DOI] [PubMed] [Google Scholar]
- Petry NM, Barry D, Alessi SM, Rounsaville BJ, Carroll KM. A randomized trial adapting contingency management targets based on initial abstinence status of cocaine dependent patients. Journal of Consulting and Clinical Psychology. 2012 Jan 16; doi: 10.1037/a0026826. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plebani JG, Kampman KM, Lynch KG. Early abstinence in cocaine pharmacotherapy trials predicts successful treatment outcomes. Journal of Substance Abuse Treatment. 2009;37:313–317. doi: 10.1016/j.jsat.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston KL, Silverman K, Higgins ST, Brooner RK, Montoya I, Schuster CR, Cone EJ. Cocaine use early in treatment predicts outcome in a behavioral treatment program. Journal of Consulting and Clinical Psychology. 1998;66:691–696. doi: 10.1037//0022-006x.66.4.691. [DOI] [PubMed] [Google Scholar]
- Scott CK, Dennis ML. Results from two randomized clinical trials evaluating the impact of quarterly recovery management checkups with adult chronic substance users. Addiction. 2009;104:959–971. doi: 10.1111/j.1360-0443.2009.02525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behavior Research and Therapy. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Stout RL, Beattie MC, Longabaugh R, Noel N. Factors affecting correspondence between patient and significant other reports of drinking [abstract] Alcoholism: Clinical and Experimental Research. 1989;12:336. [Google Scholar]
- Van Horn DHA, Drapkin M, Ivey M, Thomas T, Domis SW, Abdalla O, Herd D, McKay JR. Voucher incentives increase treatment participation in telephone-based continuing care for cocaine dependence. Drug and Alcohol Dependence. 2011;114:225–228. doi: 10.1016/j.drugalcdep.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JB, First MB, Spitzer RL, Davis M, Borus J, Howes MJ, Kane J, Pope HG, Rounsaville B, Wittchen HU. The Structured Clinical Interview for DSM-III-R (SCID): II. Multisite test-retest reliability. Archives of General Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]