Abstract
Objective
Most adolescents relapse within 90 days of discharge from residential substance use treatment. We hypothesized that Contingency Management (CM), Assertive Continuing Care (ACC), and their combination (CM+ACC) would each be more effective than Usual Continuing Care (UCC).
Method
337 adolescents were randomized to 4 continuing care conditions following residential treatment: UCC alone, CM, ACC, or CM+ACC. UCC was available across all conditions. Outcome measures over 12 months included percentage of days abstinent from alcohol, heavy alcohol, marijuana, and any alcohol or other drugs (AOD) using self-reports and toxicology testing and remission status at 12 months.
Results
CM had significantly higher rates of abstinence than UCC for heavy alcohol use (t(297)= 2.50, p<.01, d = 0.34), any alcohol use (t(297)= 2.58, p<.01, d = 0.36), any AOD use (t(297)= 2.12, p=.01, d = 0.41), and had a higher rate in remission (Odds Ratio [OR]=2.45 [90% CI: 1.18 to 5.08], p=.02). ACC had significantly higher rates of abstinence than UCC from heavy alcohol use (t(297)= 2.66, p<.01, d = 0.31), any alcohol use (t(297)= 2.63, p<.01, d = 0.30), any marijuana use (t(297)= 1.95, p=.02, d = 0.28), any AOD use (t(297)= 1.88, p=.02, d = 0.30), and had higher rates in remission (OR=2.31 [90% CI: 1.10 to 4.85], p=.03). The ACC+CM condition was not significantly different from UCC on any outcomes.
Conclusions
CM and ACC are promising continuing care approaches after residential treatment. Future research should seek to further improve their effectiveness.
Keywords: adolescent, continuing care, substance use disorder, treatment
Adolescents with the most severe alcohol and other drug (AOD) use disorders are typically admitted to residential treatment. Of the more than 21,000 U.S. adolescents admitted to residential treatment supported by public funds in 2009, 53% received an unfavorable discharge and 76% failed to complete 90 days of treatment (United States Department of Health and Human Services, 2009), the length of stay threshold associated with better outcomes (Hser et al., 2001). Additional research has shown that 60–70% of adolescents relapse within 90 days after residential treatment (Brown, Vik, & Creamer, 1989; Godley, Godley, Dennis, Funk, & Passetti, 2002). Providing continuing care following addiction treatment can improve clinical outcomes (Dennis & Scott, 2007; Godley, Godley, Dennis, Funk, & Passetti, 2007; Kaminer, Burleson, & Burke, 2008; Kim et al., 2011; McKay, 2009; Saitz, Larson, LaBelle, Richardson, & Samet, 2008; Winters, Stinchfield, Latimer, & Lee, 2007), but relatively few adult and adolescent patients attend even one continuing care session following discharge from residential treatment (Donovan, 1998; Godley & Godley, 2011).
Although some adolescent patients lack motivation to follow through with continuing care referrals, structural barriers exist as well. Residential treatment programs receiving state and/or Medicaid reimbursement typically serve large geographical areas, requiring referral to treatment organizations closer to the patient’s home after residential treatment. A recent study showed that continuing care was initiated about half the time for those with planned residential discharges and less than 10% of the time for those with unplanned discharges (Godley & Godley, 2012).
Only one randomized trial of continuing care for youth discharged from residential treatment has been published, and that study examined the effects of Assertive Continuing Care (ACC; Godley et al., 2007). This intervention was developed to overcome barriers to continuing care participation by sending clinicians trained in the Adolescent Community Reinforcement Approach (A-CRA) and case management (Godley, Godley, & Dennis, 2001) to meet with youth in their school, home, or other community location within two weeks of discharge. In this experiment, adolescents assigned to ACC after residential treatment were significantly more likely than those receiving Usual Continuing Care (UCC) to receive continuing care (94% vs. 54%) and attend more sessions. Main effects of ACC were found for abstinence from their primary drug, marijuana, over a 9-month follow-up (d=.32). Decreases for alcohol and other drugs were all in the predicted direction but not significant (Godley et al., 2007). The effects of ACC may be due to the combination of (a) case management services designed to increase adherence to the requirements of school and/or juvenile justice – two common social systems in which youth are involved; (b) A-CRA for the adolescent, which uses both operant learning and cognitive behavior therapy procedures to identify and increase reinforcing pro-social activities and facilitates the development of improved communication, relapse prevention, and other skills; (c) A-CRA sessions for both the adolescent and caregiver; and (d) homework assigned after each session to practice a new skill and engage in a new or recurring pro-social activity. Despite the durable success of ACC in the initial trial relative to UCC, effect sizes for both marijuana and alcohol were small, suggesting that additional improvements to the model should be considered.
Contingency Management (CM) interventions have been successfully added to the Community Reinforcement Approach and Cognitive Behavior Therapy in trials with adults to further improve substance use outcomes (Higgins, Silverman, & Heil, 2007). The effectiveness of CM in addiction treatment is rapid and reliable through the active phase by providing contingent reinforcement for drug abstinence and, in some studies, treatment attendance or verifiable activities. Only a few controlled studies combining CM with other treatments have been conducted for adolescents with AOD use disorders, and none were continuing care studies. Compared to a family court condition, a juvenile drug court intervention enhanced with Multi-Systemic Therapy plus CM evidenced large effects in decreasing substance use (ESs = 0.0.38 to 2.48) and criminal behavior (ESs = −0.04 to 1.88; Henggeler et al., 2006), and CM combined with parent training and Motivational Enhancement/Cognitive Behavior Therapy (MET/CBT) was more effective for adolescents than MET/CBT alone in increasing continuous abstinence from marijuana during the 3-month treatment phase (d=0.48) but less so over extended follow-up (Stanger, Budney, Kamon, & Thostensen, 2009). In studies by Azrin and colleagues (Azrin et al., 1994, 2001), a multi-component Family Behavior Therapy intervention including parent-mediated CM for abstinence and pro-social activities significantly reduced drug use compared to supportive counseling (Azrin et al., 1994) but in a second study, did not reduce drug use more than a cognitive behavioral problem-solving condition (Azrin et al., 2001). The available evidence suggests that adding CM to cognitive behavioral therapies is a promising strategy to improve adolescents’ drug use outcomes. Although several studies with adults found CM combined with CBT interventions to be more effective than either CM or CBT alone (Higgins et al., 2007; Kadden, Litt, Kabela-Cormier, & Petry, 2007), other studies found that CM alone was as effective (Rawson et al., 2002) or more effective than CM and CBT combined (Carroll et al., 2012). Because CM alone has demonstrated effectiveness with adults and is relatively straightforward to implement, it merits testing with adolescents as a post-treatment continuing care intervention.
In summary, CM has demonstrated efficacy in producing abstinence for adults and, in combination with other interventions, for adolescents. In addition, ACC has shown promise in a single trial sustaining abstinence for significantly more youth than UCC, but the effects were relatively small. For the present study, it was expected that the immediate contingent reinforcement offered through CM would improve engagement in pro-social activities and lead to greater improvement in abstinence outcomes, but because the ACC intervention is designed to increase abstinence (through increasing pro-social activities, social skills, relationship with parents, and better adherence to education and juvenile justice requirements), it was unclear whether this would exceed ACC alone. The combination of CM and ACC might provide additional sustained benefit by rapid contingent reinforcement of abstinence and pro-social activities via CM with skills training and case management provided through ACC; however, this has never been tested. The present study reports the results of a randomized trial to assess the degree to which three experimental approaches were more successful at engaging youth in post-residential continuing care and maintaining AOD abstinence during the 12 months following residential discharge relative to a UCC alone condition: (a) CM, a well-established, replicable evidence-based intervention; (b) ACC, a multi-component intervention with behavioral, CBT, and case management elements; and (c) CM +ACC, a combination of both approaches.
Methods
Design
Patients recruited for the study had been admitted to one of two residential treatment programs and, after agreeing to participate, were randomly assigned in blocks of 4 within site to ensure balance over time and by site. The study manager listed all possible sequences of the four conditions, and a random number generator determined which sequence would occur next for each site. Research assistants, who did not deliver interventions or have knowledge of assignments, collected data during study intake and 3, 6, 9, and 12 months after discharge. Patient enrollment began in 2004, and all follow-ups were concluded in 2008.
Participants
Participants were 337 adolescents admitted to residential treatment who met Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) criteria for AOD use disorders in the past year, were 12–18 years old, and resided in one of ten Illinois Counties. Exclusion criteria were leaving residential treatment prior to day seven; not returning to one of the ten target counties at discharge; significant cognitive impairment; being a ward of child protective services or a danger to self or others; meeting DSM- IV criteria for pathological gambling; being discharged to the state department of corrections; or already participating in a treatment study. Eligible adolescents and their guardians were approached about the study during the first week of adolescents’ admissions. Study participation was voluntary and under the supervision of the research organization’s Institutional Review Board. A Federal Certificate of Confidentiality was also obtained.
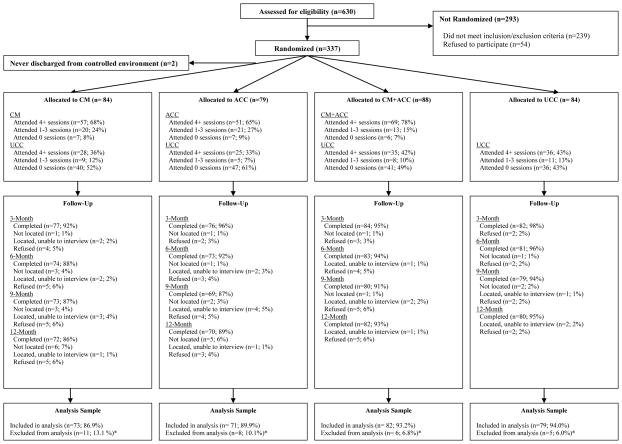
Of 630 adolescents who met inclusion criteria, 293 were not eligible based on inclusion and exclusion criteria (Figure 1). Among 391 eligible adolescents, 337 (86%) agreed to participate. When compared with those who agreed to participate, refusers (n=54) were less likely to report being of mixed race (2%) than study participants (18 %) χ2 (3) = 10.91, p < .05. Two adolescents were dropped from the study after randomization because they were discharged to juvenile correction facilities. Of the 335 remaining adolescents, follow-up interviews were completed with 95% at 3 months, 93% at 6 months, 90% at 9 months, and 91% at 12 months. Urine tests were completed at 3- and 12-month follow-ups.
Figure 1.
Participant flow diagram from eligibility determination through analysis.
UCC was provided by community-based clinicians employed, trained, and supervised at numerous outpatient clinics scattered throughout the multi-county study area. Nine study clinicians provided ACC, CM, and ACC+CM interventions, completed training workshops, and audio-recorded all treatment sessions. Over the course of the study, five study clinicians were located at one site, and 4 were located at a second site. Sessions were reviewed weekly by a single clinical supervisor and evaluated using rating checklists to assess fidelity to specific procedures. Feedback on performance was provided to clinicians by the supervisor. These reviews continued both before and after clinicians achieved proficiency in delivery of ACC and CM. Any problems arising from low fidelity ratings (e.g., omission of a component of a procedure; failure to practice a new skill with a participant; failure to constructively shape participants’ skill acquisition; failure to set new activity goals or assign homework; and deviation from the model by lecturing or using confrontation) were addressed by the supervisor with the clinician through instruction, practice, and feedback during weekly supervision. Clinicians also entered electronic service data to document the implementation of CM and ACC.
Interventions
Usual Continuing Care (UCC
At discharge from residential treatment, adolescents in all conditions were referred to UCC clinics based on proximity to their homes by their residential counselors. Adolescents who were discharged “against staff advice” or “at staff request” received a letter informing them where to obtain additional treatment, while those discharged “as planned” received a continuing care appointment date and time, typically within 2 weeks. Due to the large number of UCC clinicians across the ten counties, no attempt was made to standardize UCC. A survey of 12 such clinics (Godley et al., 2007) revealed considerable diversity in services offered, including intensive outpatient programs (3–5 days per week) and lower intensity aftercare programs (1–2 groups per week). Program elements included urine testing, social skills training, optional parental counseling, referral to 12-step groups, and case coordination with schools and probation officers. None of these programs provided home visits or required parent sessions. UCC was delivered exactly as it would be outside the context of an experiment.
Contingency Management (CM)
Adolescents in this condition were referred to UCC by the residential program and were assigned to 12 scheduled weekly home visits from a study clinician who administered CM procedures for negative alcohol and drug tests and for participating in pro-social activities (Petry, 2000). Meetings may also have occurred in another agreed upon community location. Participants were asked to provide a breath alcohol and urine sample for testing of amphetamine/methamphetamine, marijuana, cocaine, and opiates. Adolescents also chose activities for the upcoming week and provided verifications for activities completed in the prior week. Adolescents earned prize drawings for verified completed activities and negative breath and/or urine samples. They drew slips of paper from a bowl that contained 510 slips: 150 (29%) showed a smiling face; 324 (64%) read “small”; 35 (6.8%) read “large”; and 1 (0.2%) read “jumbo.” The smiling face indicated that no prize was won; “small” indicated a prize worth U.S. $1 (e.g., candy, soda, toiletries); “large” indicated a prize worth U.S. $25 (e.g., prepaid cell phone minutes, CD player, gift certificates); and “jumbo” indicated a prize worth U.S. $100 (e.g., DVD player, video game console). Replacement was used so that the odds of picking each prize category were the same each draw.
Adolescents earned at least one draw for each activity completed, with a maximum of two reinforced activities each week. Bonus draws were awarded when two activities were completed within a week. Bonus draws started at one for the first week in which two activities were completed, and increased by one for each successive week in which two activities were completed. If an adolescent failed to complete (or verify) two activities in a week, no bonus draws were earned, and bonus draws reset to one. Adolescents could earn up to 117 draws for completing 24 activities over 12 weeks.
Adolescents could also earn up to 117 draws for providing negative urine and breath samples. At each meeting, adolescents earned one draw for a negative breathalyzer test and one for a negative urine test. As with activity draws, bonus draws started at one for the first week in which both tests were negative, and then increased one per week in which both tests were negative. Bonus draws were reset to one if the adolescent was not available to provide a sample, refused a sample, or tested positive (Godley, Godley, Wright, Funk, & Petry, 2008; Petry & Stitzer, 2002).
Assertive Continuing Care (ACC)
Adolescents in this condition were referred to UCC by the residential program and assigned to an ACC clinician, who planned to conduct 10 adolescent sessions over 12 weeks after discharge from residential care. During that time, clinicians also met with caregivers twice and with the adolescent and caregiver together twice. Meetings took place in the home or other agreed upon location. The goals were to increase engagement in continuing care and other needed services, improve engagement in substance-free activities, and reduce substance use. Clinicians providing the ACC intervention followed two manuals (Godley et al., 2007; Godley, Meyers, et al., 2001). One provided details related to case management services, including linkage to or assistance accessing needed services such as GED, alternative high school, attendance at required probation officer meetings, or prenatal or other medical appointments. On rare occasions, assistance was provided to access pro-social activities. The second manual described the clinical procedures of the Adolescent Community Reinforcement Approach (A-CRA; Dennis, Godley, et al., 2004; Godley et al., 2007; Godley, Meyers, et al., 2001; Meyers & Smith, 1995). A-CRA is an adaptation of the Community Reinforcement Approach (CRA) that was initially developed and tested with adults (Azrin, Sisson, Meyers, & Godley, 1982; Hunt & Azrin, 1973). When administering A-CRA, clinicians aim to increase adolescents’ access to social reinforcers through successive approximation and skills-training activities to encourage engaging in pro-social activities. As pro-social activities become reinforcing, they compete with substance use behavior. Abstinence, healthy social activities, positive peer relationships, and improved family relationships are promoted through a positive, non-confrontational approach. A-CRA included procedures for conducting a functional analysis of substance using behaviors and social activities. Adolescent self-rating of 16 life health areas (e.g., relationships, money management, school) was used to develop individualized goals for treatment, monitor success in meeting goals, and modify or develop new goals. With the adolescent, clinicians focused skill-building on pro-social recreation, relapse prevention, anger management, communication, and problem-solving, including discussions about ways to have fun without using substances and making non-substance using friends. In the caregiver and adolescent sessions, clinicians focused on improving positive interactions and helpful behavior through communication and problem-solving skills training.
CM+ACC
Adolescents in this condition were referred to UCC by the residential program and assigned to the CM and ACC interventions described above over 12 weeks after residential discharge. CM and ACC procedures were provided at the 12 planned weekly sessions with the individual adolescent. Meetings occurred in the home or other agreed upon community location. Each session began with the breathalyzer and urine tests and a CM review of activity verifications and prize drawings, followed by ACC counseling and case management activities, and concluded with the participant choosing activities for the next week. During that time, clinicians also attempted to meet with caregivers twice and with the adolescent and caregiver together twice as part of ACC.
Assessment Procedures
All ACC and CM sessions were audio-recorded except in the rare event of equipment problems or if an adolescent refused recording. At least one recording per therapist was reviewed weekly for fidelity to the manuals. As a further check on adherence and treatment service documentation, the clinical supervisor compared randomly selected recordings to clinician-entered treatment services data, which documented each ACC clinical procedure used in each session.
The primary outcome was self-reported percent of days abstinent from alcohol and other drugs over the 12 months after discharge from residential treatment as assessed with the Global Appraisal of Individual Needs (GAIN; Dennis, Titus, White, Unsicker, & Hodgkins, 2003). The GAIN has established norms based on >15,000 youth and has been validated with subjective and objective indicators (Dennis, Funk, Godley, Godley, & Waldron, 2004; Dennis, Godley, et al., 2004; Dennis, White, & Ives, 2009; Godley et al., 2002). To increase the validity of self-report, prior to administering the GAIN, participants were asked if they had any AOD use in the past week. If participants denied any past week AOD use, they were tested using an immunochromatographic assay with a one-step drug cup (www.cliawaived.com) for amphetamine/methamphetamine, marijuana, cocaine/benzoylecgonine, and opiates/morphine. If they tested positive for a drug, but did not self-report using it in the past week, they were reminded to include all drugs, even if they used it in combination with something else, and were asked again about recent substance use. The GAIN includes questions regarding how many days (in the past 90) the participant was abstinent from “any alcohol or other drug use,” days using each of 16 substances (alcohol, heavy alcohol use [5+ drinks or being drunk], marijuana, crack, other cocaine, heroin, street methadone, other opioids, methamphetamines, other stimulants, tranquilizers, PCP, other hallucinogens, sedatives, inhalants, and other drugs), and the days in a controlled environment. Percent of days abstinent over 12 months (adjusted for days in a controlled environment) was based on the total over the 4 quarters. The on-site testing procedure resulted in a relatively low false negative rate (positive urine test but no self-reported use) of 7.8% (25 of 320 tests). Chi-square tests revealed no significant differences in false negative rates across conditions, ps > .22. Days in a controlled environment was computed across items for the number of days out of the past 90 the participant was in residential treatment, juvenile detention, or in the hospital for physical or mental health reasons.
The secondary outcome measure used a dichotomous classification of whether participants were in remission in month 12. Remission was coded if the patient was living in the community and reported no use, abuse, or dependence symptoms for the past 30 days at month 12. Any indication of AOD use from self-report or urine tests and any indication of being in a controlled environment coded the participant as not in remission.
Adverse Events
There were no deaths or study-related serious adverse events during the trial. One CM participant was withdrawn from the intervention at the parents’ request after 5 weeks because they disagreed with activity incentives being earned while urine tests were positive.
Statistical Analysis
All analyses were conducted with SPSS Version 17 (SPSS, 2007). The primary outcome variable was analyzed using a multivariate general linear model (GLM) using 3 planned orthogonal contrast (CM vs. UCC, ACC vs. UCC, CM+ACC vs. UCC) after controlling for site, intake clinical risk characteristics, and pre-randomization residential treatment variables. To derive covariate values, control variables (Table 1) were first used to predict the primary outcome variable and different substance use outcomes in separate equations. The expected or predicted outcome from these preliminary GLMs were then used as covariates in the analyses of primary outcomes to partial out explainable variance from the error term from subsequent analyses and improve power. Each contrast was evaluated with the directional t-test for each parameter, testing the hypothesis that the experimental condition result was greater than the UCC. The overall F statistic from the GLM output is based on the average of three squared t-scores.
Table 1.
Participant intake characteristics and residential treatment received
| Measure | CM (n = 73) | ACC (n = 71) | ACC+CM (n = 82) | UCC (n = 79) | F or χ2 | p-value |
|---|---|---|---|---|---|---|
| Demographics [No. (%)] | ||||||
| Female | 21 (29) | 31 (44) | 30 (37) | 28 (35) | 4.18 | 0.25 |
| Age Mean (SD), | 15.7 (1.2) | 15.5 (1.2) | 15.9 (1.2) | 15.9 (1.0) | 1.86 | 0.14 |
| Race: | ||||||
| African American | 14 (19) | 4 (6) | 13 (16) | 6 (8) | 14.44 | 0.11 |
| Caucasian | 46 (63) | 55 (78) | 51 (62) | 60 (76) | ||
| Hispanic | 4 (6) | 5 (7) | 6 (7) | 1 (1) | ||
| Mixed/Other | 13 (18) | 11 (16) | 18 (22) | 13 (17) | ||
| Single Parent Family | 49 (69) | 42 (61) | 52 (69) | 47 (62) | 1.97 | 0.58 |
| Ever Homeless or Runaway | 36 (49) | 28 (39) | 33 (40) | 36 (46) | 1.97 | 0.59 |
| High severity victimization | 39 (53) | 36 (51) | 41 (50) | 33 (42) | 2.34 | 0.52 |
| Substance Severity: | ||||||
| Dependence | 62 (86) | 54 (76) | 65 (81) | 62 (81) | 5.60 | 0.48 |
| Abuse Only | 8 (11) | 16 (23) | 13 (16) | 15 (20) | ||
| Weekly Use Only | 2 (3) | 1 (1) | 2 (3) | 0 (0) | ||
| Any Co-occurring Psychiatric Disorder: | 56 (77) | 55 (78) | 69 (84) | 63 (80) | 1.62 | 0.66 |
| Mood Disorder | 32 (44) | 32 (45) | 41 (50) | 36 (46) | 0.69 | 0.88 |
| Generalized Anxiety | 10 (14) | 7 (10) | 13 (16) | 10 (13) | 1.24 | 0.75 |
| Traumatic Stress | 18 (25) | 23 (33) | 34 (42) | 25 (32) | 5.03 | .17 |
| ADHD | 38 (52) | 32 (45) | 45 (55) | 34 (43) | 2.97 | .40 |
| Conduct Disorder | 47 (64) | 42 (60) | 58 (71) | 52 (66) | 1.97 | .58 |
| Any Violent Crime | 36 (49) | 39 (55) | 49 (60) | 49 (62) | 2.94 | 0.40 |
| Current criminal justice involvement | 67 (92) | 56 (79) | 71 (87) | 69 (87) | 5.22 | 0.16 |
| Prior substance abuse treatment: | ||||||
| Once | 28 (38) | 31 (44) | 33 (40) | 30 (38) | 4.43 | 0.63 |
| 2+ episodes | 22 (30) | 15 (21) | 17 (21) | 25 (32) | ||
| Ever attended self-help group | 27 (37) | 21 (30) | 25 (31) | 19 (24) | 3.03 | 0.40 |
| Intake Scores on Main GAIN Scales [Mean (SD)] | ||||||
| Substance Problem Scale | 10.1 (3.4) | 9.5 (3.6) | 10.0 (3.9) | 9.3 (3.8) | 0.71 | 0.55 |
| Internal Mental Distress Scale | 10.0 (10.0) | 10.8 (9.7) | 12.3 (10.2) | 10.4 (8.8) | 0.88 | 0.45 |
| Behavior Complexity Scale | 12.9 (9.1) | 11.5 (8.6) | 13.8 (7.7) | 13.1 (7.9) | 1.02 | 0.39 |
| Crime and Violence Scale | 9.4 (6.4) | 9.1 (6.3) | 8.9 (5.2) | 9.6 (5.9) | 0.21 | 0.89 |
| Social Risk Index | 14.4 (4.4) | 15.8 (4.9) | 14.6 (4.4) | 15.2 (5.3) | 1.39 | 0.25 |
| Recovery Environment Risk Index | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) | 0.15 | 0.93 |
| Treatment Resistance Index | 1.3 (0.9) | 1.2 (1.0) | 1.5 (1.0) | 1.3 (1.0) | 1.10 | 0.35 |
| Treatment Motivation Index | 2.8 (1.1) | 2.7 (1.1) | 2.6 (1.0) | 2.6 (1.2) | 0.66 | 0.58 |
| Self-Efficacy Scale | 4.1 (1.5) | 4.0 (1.2) | 3.9 (1.4) | 3.8 (1.4) | 0.47 | 0.71 |
| Problem Orientation Scale | 2.0 (2.0) | 1.9 (2.0) | 2.1 (2.0) | 2.1 (2.1) | 0.21 | 0.89 |
| Personal Source of Stress Index | 1.8 (1.5) | 1.5 (1.4) | 1.7 (1.5) | 1.8 (1.6) | 0.83 | 0.48 |
| Other Source of Stress Index | 1.5 (1.9) | 1.4 (1.8) | 1.5 (1.6) | 1.4 (1.5) | 0.07 | 0.97 |
| Emotional Problems Scale | 0.3 (0.2) | 0.3 (0.2) | 0.4 (0.2) | 0.3 (0.2) | 0.98 | 0.41 |
| Illegal Activity Scale | 0.1 (.1) | 0.1 (.1) | 0.2 (0.2) | 0.2 (0.2) | 2.86 | 0.04 |
| Intake Values for Outcome Measures [Mean (SD)] | ||||||
| % of Days in a controlled environment | 11.7 (17.6) | 16.6 (22.5) | 15.0 (20.7) | 11.2 (17.6) | 1.21 | 0.31 |
| % of Days abstinent from AOD | 32.4 (32.5) | 34.5 (28.9) | 25.7 (29.0) | 28.1 (30.8) | 1.34 | 0.26 |
| % of Days abstinent from heavy alcohol | 79.07 (26.7) | 74.7 (27.8) | 75.0 (25.3) | 77.3 (24.1) | 0.47 | 0.71 |
| % of Days abstinent from alcohol | 76.33 (28.6) | 71.4 (28.4) | 73.8 (25.8) | 74.6 (25.5) | 0.42 | 0.74 |
| % of Days abstinent from Marijuana use | 42.4 (35.0) | 42.0 (35.0) | 30.9 (30.2) | 33.1 (32.7) | 2.59 | 0.06 |
| In remission No. (%) | 6 (8) | 7 (10) | 5 (6) | 9 (11) | 2.86 | 0.43 |
| Residential treatment prior to continuing care [No. (%)] | ||||||
| Any Alcohol or drug use in treatment | 9 (12) | 8 (10) | 6 (7) | 8 (10) | 1.12 | 0.78 |
| Planned discharge | 40 (55) | 34 (48) | 47 (57) | 52 (66) | 5.05 | 0.17 |
| Length of residential stay (days) Mean (SD) | 77 (42.9) | 66 (46.2) | 72 (48.7) | 79 (48.6) | 1.06 | 0.37 |
Remission was analyzed with logistic regression using the same omnibus test based on the 3 planned orthogonal contrasts described above after controlling for baseline risk and residential treatment variables. Each contrast was evaluated with a chi-square testing the hypothesis that the odds ratio of the experimental over UCC condition was > 1.0.
Missing data (<1% of data) on any intake variable or pre-random assignment residential treatment variables were replaced with the SPSS Replace Missing Value procedure in which we sorted records by site, condition, and total symptom count, then used the median of the four nearest valid answers (see McDermeit, Funk, & Dennis 1999). Less than 10% of participants missed any given interview wave, and less than 10% missed more than one interview across all waves. Up to one follow-up wave of data on the outcome measures was replaced using the average of the other waves. Cases with 2 or more missing waves of follow-up data were deleted from the final analysis. This process resulted in a sample of n = 305 for the outcome analysis, with any missing data replaced for < 5% of the cases. The pattern of findings did not change, using HLM with all cases included, but deletion prevented generalizing from one or two observations to all follow-up waves.
Results
Demographic and Clinical Characteristics
Of the 305 adolescents included in the outcome analysis, 63% were male, 70% described themselves as White/Caucasian, 12% as Black/African American, and 18% as other/mixed. Five percent described themselves as Hispanic, including those who reported themselves as mixed race. Average age was 15.7 years (SD = 1.2), 79% were in school, and 86% were involved in the criminal justice system. Ninety-one percent met criteria for marijuana use disorder, 58% for alcohol use disorder, and 54% for both marijuana and alcohol disorders. Over half (81%) reported symptoms for co-occurring psychological problems (percentages by specific mental health problem can be found in Table 1). Referrals to residential treatment were made by the juvenile justice system (47%), family members (13%), another agency (12%), and other sources (28%). Based on self-report, 23% of adolescents had private insurance, 41% public insurance, and 36% mixed source, unknown, or no insurance. Average length of stay in residential treatment was 71 days, and 56% were classified as successful discharges by clinical staff. Analyses of intake variables revealed one significant group difference, illegal activity scale.
Treatment Adherence, Engagement, and Exposure
Agreement rates between supervisor reviews of audio-recorded sessions and clinician coding of specific treatment procedure implementation ranged from 82% – 94% by clinician and averaged 87% agreement across all comparisons. Using the Washington Circle performance standard for outpatient engagement (attending 4+ sessions within first 45 days; Garnick et al., 2002), Table 2 shows that the three experimental conditions did not differ significantly in engagement, but all were significantly more likely to engage adolescents than UCC, with engagement rates ranging from 75% (ACC) to 84% (CM+ACC) compared to 49% for the UCC condition. CM, ACC, and CM+ACC participants attended 69%, 54%, and 66%, respectively, of planned sessions and there was no significant difference between them; however, within the ACC and CM+ACC conditions, only 28% and 33% of participants received caregiver/adolescent sessions. As no attempt was made to standardize UCC, this condition did not have a planned number of sessions.
Table 2.
Treatment process measures by condition
| Measure No. (%) | CM (n = 73) | ACC (n = 71) | CM+ACC (n = 82) | UCC (n = 79) | χ2 | p-value |
|---|---|---|---|---|---|---|
| ACC and CM Sessions\a | ||||||
| None | 6 (8) | 6 (9) | 4 (5) | 79 (100) | 239.15 | <.01 |
| 1–3 Sessions | 16 (22) | 16 (23) | 12 (15) | 0 (0) | ||
| 4+ Sessions | 51 (70) | 49 (69) | 66 (81) | 0 (0) | ||
| Usual Continuing Care sessions | ||||||
| None | 36 (50) | 42 (59) | 38 (48) | 29 (37) | 7.52 | 0.28 |
| 1–3 Sessions | 8 (11) | 6 (9) | 8 (10) | 11 (14) | ||
| 4+ Sessions | 28 (39) | 23 (32) | 34 (43) | 38 (49) | ||
| Total CM/ACC/UCC Sessions\b | ||||||
| None | 4 (6) | 6 (9) | 2 (2) | 29 (37) | 53.28 | < .01 |
| 1–3 Sessions | 13 (18) | 12 (17) | 11 (13) | 11 (14) | ||
| 4+ Sessions | 56 (77) | 53 (75) | 69 (84) | 38 (49) | ||
When compared across the three experimental conditions only, there was no significant difference, χ2(1) = 3.31, p = .52.
When compared across the three experimental conditions only, there was no significant difference, χ2 (1) = 3.62, p = .47.
Out of 3,082 activities assigned in both CM conditions, 1,935 (63%) were completed. These participants averaged nearly 7 (out of 12 possible) urine screens, with the CM participants averaging 82.9% negative results for all tested illegal drugs compared to 72.1% negative results for CM+ACC (p = .05). The longest average continuous weeks of abstinence (out of 12) was 5.7 for the CM group compared to 5.3 for the CM+ACC group (p = .56). Breathalyzer tests for recent alcohol use were conducted at the same time as urine tests, and 100% of these tests were negative for alcohol in both CM conditions.
Primary Outcomes
Although there were no between-condition baseline differences found for percent of time spent in a controlled environment (Table 1), outcome analysis revealed a significant difference for this variable over the follow-up period, F(3,297) = 4.30, p < .05. The a priori contrasts showed significantly fewer days in a controlled environment for CM than UCC (13% to 21%, t(297)= −2.81, p=.03, d = −0.35) and ACC compared to UCC (d=−.25). Because of this finding, AOD abstinence outcomes variables over the 12-month period were adjusted to remove bias in the calculation of percent days abstinent.
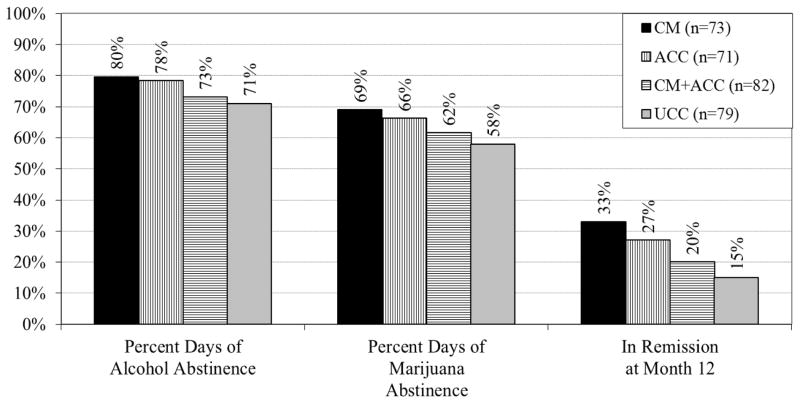
The results for the sample’s percent of days abstinent from primary drugs of abuse, alcohol and marijuana, as well as remission status at the last follow-up wave are shown in Figure 2. Results for overall comparison of the experimental conditions to the control group were all significant using a directional test (experimental > UCC): abstinent from any AOD use, F(3,297) = 2.79, p < .05; abstinent from Heavy Alcohol, F(3,297) = 4.56, p < .01; abstinent from Alcohol, F(3,297) = 4.68, p < .01; and abstinent from marijuana, F(3,297) = 2.79, p < .05.
Figure 2.
Primary and Secondary Outcomes over 12 Months.
Subsequent analyses were conducted on the planned orthogonal contrasts of the individual experimental conditions versus the UCC control group. In the 12 months after discharge from residential treatment, CM resulted in significantly higher rates of AOD abstinence days than UCC (65.1% to 52.6%, t(297)= 2.12, p=.01, d = 0.41). This pattern also was true for heavy alcohol use (81.2% to 73.1%, t(297)= 2.50, p<.01, d = 0.34), any alcohol use (79.6% to 71.1%, t(297)= 2.58, p<.01, d = 0.36), and marijuana use (69% to 58%, t(297)= 2.01, p=.01, d = 0.38). Likewise, in the 12 months after discharge from residential treatment, ACC had significantly higher rates than UCC for days of abstinence from any AOD use (61.6% to 52.6%, t(297)= 1.88, p=.02, d = 0.30), heavy alcohol use (80.3% to 73.1%, t(297)= 2.66, p<.01, d = 0.31), any alcohol use (78.3% to 71.1%, t(297)= 2.63, p<.01, d = 0.30), and marijuana use (66.2% to 58.0%, t(297)= 1.95, p=.02, d = 0.28). In the 12 months after residential treatment, CM+ACC was not associated with significantly higher abstinence rates than UCC in any AOD use outcome measures. Table 3 provides the sample size, means, standard deviations, directional t-tests, probability of the null hypotheses, and effect sizes across the 3 contrasts for percent of days in a controlled environment, percent of days abstinent from alcohol use, and percent of days abstinent from marijuana use.
Table 3.
Primary and secondary outcomes by planned contrasts\a
| Measure | CM (n=73) | ACC (n=71) | CM+ACC (n=82) | UCC (n=79) | Total (n=305) |
|---|---|---|---|---|---|
| Percent of Days [Mean (SD)]: | |||||
| In a Controlled Environment | 13.3 (17.1) | 15.7 (20.1) | 20.2 (25.1) | 21.3 (25.2) | 17.8 (22.6) |
| Contrast t (297) | −2.81 | −2.22 | −0.27 | ||
| p | 0.03 | 0.03 | 0.79 | ||
| Pairwise Cohen’s Effect Size d | −0.35 | −0.25 | −0.05 | ||
| 95% CI for d | (−0.78, −0.13) | (−0.68, −0.04) | (−0.35, 0.28) | ||
| Abstinent from Alcohol | 79.6 (21.3) | 78.3 (22.1) | 73.1 (25.4) | 71.1 (25.6) | 75.3 (23.9) |
| Contrast t (297) | 2.58 | 2.63 | 0.68 | ||
| p | <.01 | <.01 | 0.25 | ||
| Pairwise Cohen’s Effect Size d | 0.36 | 0.30 | 0.09 | ||
| 95% CI for d | (0.10, 0.74) | (0.11, 0.75) | (−0.20, 0.42) | ||
| Abstinent from Marijuana | 69.0 (27.2) | 66.2 (30.4) | 61.6 (29.4) | 58.0 (28.2) | 63.5 (29.0) |
| Contrast t (297) | 2.01 | 1.95 | 0.70 | ||
| p | 0.01 | 0.02 | 0.24 | ||
| Pairwise Cohen’s Effect Size d | 0.38 | 0.28 | 0.12 | ||
| 95% CI for d | (0.0.1, 0.65) | (0.00, 0.63) | (−0.20, 0.42) | ||
|
| |||||
| In Remission\b at Month 12 [No. (%)] | 24 (33) | 19 (27) | 16 (20) | 12 (15) | 71 (23) |
| Odds Ratio | 2.45 | 2.31 | 1.12 | ||
| 95% OR | (1.18, 5.08) | (1.10, 4.85) | (0.53, 2.38) | ||
| Contrast Chi-square (1) | 4.17 | 3.53 | 0.60 | ||
| p | 0.02 | 0.03 | 0.40 | ||
| Pairwise Cox’s d | 0.54 | 0.51 | 0.07 | ||
Site and all variables in Table 1 were used to generate a propensity score for each outcome; these scores were then used as covariates.
Note: with the 2013 publication of the DSM V, early remission is defined as the absence of symptoms over the past 90 days, not past 30 days as in the DSM IV and reported here.
Other outcome measures from the GAIN were tested; however, no significant differences were found between the experimental conditions and UCC for percent of days patients experienced emotional or family problems, engaged in illegal activities, and attended school or their job. We also tested the extent to which engagement (4+ sessions attended in first six weeks) and a formative index of pro-social activities was related to AOD abstinence outcomes. A priori contrasts showed that the experimental conditions were significantly higher than UCC for engagement and pro-social activities and each had small significant correlations (~.20) with AOD outcomes; however, neither the Baron and Kenney (1986) method nor bias-correct bootstrapping procedure (MacKinnon, Lockwood, & Williams, 2004) found that engagement or pro-social activities mediated condition assignment and AOD outcomes.
Secondary Outcome
The proportion of adolescents in remission at the end of the follow-up period for each condition is also shown in Figure 2 and was significantly different overall, χ2(3) = 10.07, p < .01. When CM was compared to UCC, it resulted in higher remission at month 12 (33% vs. 15%; d=0.54). ACC also produced higher remission at month 12 when compared to UCC (27% vs. 15%; d=0.51). The combination of CM and ACC when compared to UCC did not result in significantly higher remission at month 12. Table 3 contains the odds ratio of each condition (relative to UCC), its 95% confidence interval, chi-square, and p value for each contrast.
Discussion
Results of the present study demonstrated that both the CM and ACC conditions resulted in significantly more days of abstinence from alcohol and illicit drug use than UCC over a 12-month period, and both conditions were more likely to be in remission at the 12-month follow-up. In addition, CM and ACC resulted in significantly fewer days spent in residential treatment, juvenile detention, and hospitals over the 12-month period. Since UCC was available to all conditions, we checked for differential rates of UCC services received both during the 3-month active continuing care phase and over the last 9 months of the study, and no differences were found between conditions. Multiple treatment effects tested between the ACC and the CM conditions were all d=.12 or less, making it difficult to recommend one treatment over the other. Compared to the UCC alone condition, effect sizes of clinical outcomes, while improved over the prior ACC study (Godley et al., 2007), were in the small to medium range.
Outcomes for the experimental conditions in this study both contradict and are consistent with previous research. Contrary to some CM trials for cocaine and marijuana (Epstein, Hawkins, Covi, Umbricht, & Preston, 2003; Stanger et al., 2009), the present study found home-based CM maintained results 9 months after the active phase of continuing care; however, unlike prior CM trials, the CM condition in this study followed a course of residential treatment, and this sequence of treatment may have been helpful in maintaining efficacy through 12 months. It is also noteworthy that few trials with adults (e.g., Carroll et al., 2012; McKay et al., 2010) and no trials with adolescents that we are aware of have studied the effects of CM without the addition of CBT, family, or another therapy. While the CM-only condition performed comparatively well, effectiveness of detecting some drugs may have been hindered by the inability to conduct urine tests more than once per week and the fact that a single nonrandom breath test once per week will not deter or detect much alcohol use. Given the long half life of marijuana, patients often waited two weeks after a positive urine test before the next specimen tested negative; however, since patients were also able to earn prize drawings for negative breath alcohol samples and completed pro-social activities, they were presented with other opportunities to earn prizes while waiting for a negative marijuana urine test.
The findings for both CM and ACC compare favorably to the previous ACC study (Godley et al., 2007) in that both conditions resulted in a greater percentage of adolescents in full remission over 12 months compared to a 9-month follow-up. By comparison, a study of 600 youth with marijuana use disorders treated in outpatient settings conducted by Dennis, Godley, et al. (2004) found 24% of youth in remission at 12-month follow-up. Although there are marginal improvements over this rate for the CM and ACC conditions, it is worth noting that participants in the present study were likely more impaired than the outpatient sample studied (Dennis et al., 2004; Godley, Godley, & Dennis, 2001). In addition, the finding in this study that CM and ACC resulted in significant improvements relative to UCC in reducing days in juvenile detention, residential, and hospital treatment over the 12-month follow up suggest the costs of these interventions may be at least partially offset by reductions in utilization of these costly services.
For the CM+ACC condition, it was hoped that the procedures for increasing engagement in pro-social activities in both ACC and CM would be complementary and compensate for any deficits the single conditions might have in either producing better pro-social or sustained abstinence outcomes. It might also be expected that providing more treatment services to patients would generally result in better clinical outcomes. Our results did not support these assumptions but are consistent with other study findings. For example, Henggeler et al. (2006) conducted a randomized trial of a complex intervention involving Drug Court+Multisystemic Therapy (MST)+CM that resulted in better outcomes than Family Court or Drug Court only, but were not significantly different than the Drug Court+MST condition. Of note in the Henggeler et al. (2006) study is the significant improvement compared to drug court only for the Drug Court+MST condition. The MST intervention targets caregiver empowerment using CBT and behavior management skills training to improve parenting and parent-child interactions. While the present study found it difficult to hold the caregiver-adolescent sessions, it is possible that greater adherence to these sessions would have further improved outcomes in the ACC conditions. Similarly, it may have served to better integrate the CM+ACC conditions had parents been taught to administer CM and negotiate contingent reinforcement for negative drug screens and verifiable activities of high importance to both the parent and adolescent. Within the context of broader interventions, positive results have been reported teaching caregivers contingency contracting (Azrin et al., 2001) and CM (Henggeler et al., 2006).
Also consistent with our findings, Carroll et al. (2012) found that young adults court-mandated to treatment had better marijuana use outcomes in a CM for abstinence only condition and a CBT-only condition than for two combination conditions (CM for abstinence + CBT; CBT+CM adherence to session attendance/homework). These investigators suggested that less demanding approaches may be comparatively more appealing and effective for samples containing high numbers of individuals not seeking treatment on their own. Similarly, our sample had high rates of youth on juvenile probation required to seek treatment. Adolescents in the combined condition received an initial course of residential treatment followed by the simultaneous referral to UCC and the combination of CM+ACC, and while compliance with attendance was as good as or better than other conditions, participants may have been overwhelmed by the combined demands of these interventions.
Across experimental conditions, putative change mechanisms included: (a) increasing the engagement rate of patients in the experimental continuing care conditions relative to UCC (both CM and ACC); (b) increasing participation in pro-social activities in order to compete with substance use through social and recreational activities that were reinforcing to patients (both CM and ACC); (c) specific skills-training to improve caregiver-adolescent relationships, assigning homework to practice skills and pro-social activities (ACC); and (d) providing case management to improve adherence to school and probation requirements (ACC). In all conditions, there were direct measures of engagement and pro-social activities. A feature of the three experimental conditions was rapid engagement through home or other community visits; thus patients were significantly more likely to engage in continuing care treatment than the UCC condition. Each experimental condition also emphasized engaging in pro-social activities, and relative to UCC, these behaviors were positively associated with better substance use outcomes. Although mediation analysis was attempted, this study was underpowered to detect such an effect.
Despite the fact that research on CM and the community reinforcement approach for AOD treatment is extensive, few published studies have examined the above potential mechanisms of change. Litt, Kadden, Kabela-Cormier, & Petry (2008) found partial mediation of long-term abstinence by increased self-efficacy; however, this effect was not unique to a specific treatment condition and was conditional upon achieving early abstinence during treatment. Such a finding supports combining CBT for improving social skills with CM to achieve early abstinence; however, two recent trials with various combinations of CBT and CM tested the Litt et al. (2008) findings, and either failed to provide experimental support for causal mechanisms (Carroll et al., 2012) or provided limited support (Litt, Kadden, & Petry, 2013).
A strength of the present study is the relatively large sample, high follow-up rates, and broadly inclusive enrollment criteria (i.e., successful discharge from residential treatment was not required). Participants were youth who were normally referred to residential treatment and were representative of small urban and rural areas. In addition, clinicians serving in the CM and ACC conditions had similar training and experience as those working in treatment programs, with less than half having graduate degrees. The inclusion of all drugs of abuse in randomized trials is rare; however, in practice, clinicians typically focus on abstinence from all illicit substances. This study demonstrated significant improvement across the most commonly used drugs (alcohol and marijuana) as well as a summative measure of all AOD use. Since no attempt was made to standardize UCC, this condition was as it exists outside of this study, which strengthened external validity. Site was controlled for in the analyses, and validity of self-reported substance use was optimized by providing urine test results immediately prior to follow-up interviews.
The study also had limitations. No attempt was made to collect weekly urine specimens in the ACC or UCC conditions, and such data would have allowed for assessment of during-treatment sustained abstinence and group differences on AOD use. Given the study location and target population, it is unclear to what extent these results apply to large urban areas. Similarly, the small percentage of participants identifying themselves as Hispanic makes generalization of results to this population of adolescents more tentative. In addition, data collection was almost complete by the time awareness of synthetic marijuana (e.g., K2; spice) use was a significant concern, and there was no testing conducted for its use. Finally, while the condition sample sizes are large for this type of study, they are still relatively small for the purpose of calculating exact 95% CI of effect sizes. Although the impact on any use was statistically significant and the point estimate was in the small to moderate range, the 95% CI was very broad and included 0 (−.01 to .63). This suggests the need for further replication.
Given the reliance on home visits, this may present a challenge for provider organizations to implement ACC and CM. The community visits conducted in the experimental conditions were supported by grant funds; however, provider reimbursement for travel to do community visits may not be allowed, depending upon the specific Medicaid or other reimbursement rules within each state. Returning to the issue of family sessions, the planned sessions for the adolescent and caregiver together were difficult to achieve (<40%) even though multiple efforts to accommodate missed appointments were attempted in all cases. It should be noted that reluctance of caregivers to participate in the family sessions was not an exclusion criterion in either the prior ACC study or the present study. Nevertheless, caregivers were asked at intake to indicate their willingness to participate in family sessions. In the first ACC study, 67% (Godley et al., 2007) agreed to participate, while only 50% agreed in the present study. It is likely that reduced caregiver agreement at intake to participate in this study’s family sessions was reflected in the relatively low engagement in family sessions after residential discharge. Other possible reasons for the difficulty in completing family sessions include the expectation that residential treatment would be sufficient, or in some cases, disappointment over a less than optimal residential experience. These factors may have interacted with one or more of the following: a) a high percentage (50+%) of single parent families in which employment and other childcare responsibilities may make participation difficult; b) while the background, degree, and training of clinicians in both studies was about the same, it is possible that better skilled clinicians may have been more successful engaging families in the first study; and c) perhaps there was greater oversight from juvenile justice authorities in the first study, which may have led to better caregiver compliance with family sessions. We note, however, that the family engagement rates in this study may reflect actual practice, as prior research suggests that in UCC, only 32% of youth reported family involvement in continuing care treatment (Godley et al., 2007). Other researchers have successfully provided incentives for parent involvement in their child’s addiction treatment (Kamon, Budney, & Stanger, 2005; Stanger et al., 2009), and this strategy may prove useful in future efforts to improve engagement in caregiver-adolescent sessions. Alternatively, clear expectations and oversight from the court for caregivers to participate in family sessions may prove useful as high numbers of youth are referred to treatment by juvenile justice authorities.
Although continuing care is commonly recommended for patients leaving residential treatment, little is known about its effectiveness for adolescents, and the application of prospective research designs to test interventions is new in this area. The present study is significant in that both the CM and ACC conditions produced improvements in abstinence across the most commonly used drugs (marijuana and alcohol) and increased remission compared to UCC alone; however, future research is needed to better test the contribution of the improved outcomes of continuing care engagement and pro-social activities and to evaluate better ways to implement CM in continuing care, including teaching CM skills to caregivers (Azrin et al., 2001; Donohue et al., 2009; Henggeler et al., 2006). Future investigations of ACC or its combination with CM should also include self-efficacy measures based on the CBT components of ACC and sustained early abstinence to assess whether or not increased self-efficacy mediates substance use outcomes. In addition, researchers need to test whether continuing care engagement, increased pro-social activities, and improved parent-child relationships mediate longer term treatment outcomes. In terms of intervention cost, research is needed to analyze the cost-effectiveness of CM vs. ACC, and, given the significant reductions in time spent in institutional settings by youth receiving both CM and ACC, future research should examine the extent to which these interventions may result in net savings to society. Finally, researchers designing future continuing care studies should coordinate with residential providers to withhold referral to UCC for patients assigned to an experimental continuing care condition in order to reduce patient and family burden and streamline protocols. Notwithstanding the need for replication, results of the present study suggest that both CM and ACC offer continuing care strategies to improve abstinence outcomes across all drug categories and reduce time in costly controlled environments for adolescents following discharge from residential care.
Acknowledgments
This research was supported by Grants AA010368 and AA021118 from the National Institute on Alcohol Abuse and Alcoholism. We thank the clinical and project staff, especially Courtney Hupp, Christin Bair, and Kelli Wright, and Stephanie Merkle for assisting with manuscript preparation. We dedicate this article to the late Dr. Nathan H. Azrin, whose seminal contributions to learning-based therapies made this work possible.
Contributor Information
Mark D. Godley, Chestnut Health Systems
Susan H. Godley, Chestnut Health Systems
Michael L. Dennis, Chestnut Health Systems
Rodney R. Funk, Chestnut Health Systems
Lora L. Passetti, Chestnut Health Systems
Nancy M. Petry, University of Connecticut School of Medicine
References
- Azrin NH, Donohue B, Teichner GA, Crum T, Howell J, DeCato LA. A controlled evaluation and description of individual-cognitive problem solving and family-behavior therapies in dually-diagnosed conduct-disordered and substance-dependent youth. Journal of Child and Adolescent Substance Abuse. 2001;11:1–43. doi: 10.1300/J029v11n01_01. [DOI] [Google Scholar]
- Azrin NH, McMahon PT, Donohue B, Besalel VA, Lapinski KJ, Kogan ES, Galloway E. Behavior therapy for drug abuse: A controlled treatment outcome study. Behaviour Research and Therapy. 1994;32:857–866. doi: 10.1016/0005-7967(94)90166-X. [DOI] [PubMed] [Google Scholar]
- Azrin NH, Sisson RW, Meyers R, Godley M. Alcoholism treatment by disulfiram and community reinforcement therapy. Journal of Behavior Therapy and Experimental Psychiatry. 1982;13:105–112. doi: 10.1016/0005-7916(82)90050-7. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Brown SA, Vik PW, Creamer VA. Characteristics of relapse following adolescent substance abuse treatment. Addictive Behaviors. 1989;14(3):291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, LaPaglia DM, Peters EN, Easton CJ, Petry NM. Combining cognitive behavioral therapy and contingency management to enhance their effects in treating cannabis dependence: Less can be more, more or less. Addiction. 2012;107:1650–1659. doi: 10.1111/j.1360-0443.2012.03877.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Scott CK. Managing addiction as a chronic condition. Addiction Science and Clinical Practice. 2007;4(1):45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Funk R, Godley SH, Godley MD, Waldron H. Cross-validation of the alcohol and marijuana use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction. 2004;99(2):120–128. doi: 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, Funk RR. The Cannabis Youth Treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27(3):197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Titus JC, White M, Unsicker J, Hodgkins D. Global Appraisal of Individual Needs (GAIN): Administration guide for the GAIN and related measures. Bloomington, IL: Chestnut Health Systems; 2003. (Version 5) [Google Scholar]
- Dennis ML, White M, Ives ML. Individual characteristics and needs associated with substance misuse of adolescents and young adults in addiction treatment. In: Leukefeld C, Gullotta T, Tindall MS, editors. Adolescent substance abuse: Evidence-based approaches to prevention and treatment. New York: Springer; 2009. pp. 45–72. [Google Scholar]
- Donohue B, Azrin N, Allen DN, Romero V, Hill HH, Tracy K, Van Hasselt VB. Family Behavior Therapy for substance abuse and other associated problems: A review of its intervention components and applicability. Behavior Modification. 2009;33:495–519. doi: 10.1177/0145445509340019. [DOI] [PubMed] [Google Scholar]
- Donovan DM. Continuing care: Promoting maintenance of change. In: Miller WR, Heather N, editors. Treating addictive behaviors. 2. New York: Plenum Press; 1998. pp. 317–336. [Google Scholar]
- Epstein DH, Hawkins WE, Covi L, Umbricht A, Preston KL. Cognitive-behavioral therapy plus contingency management for cocaine use: Findings during treatment and across 12-month follow-up. Psychology of Addictive Behaviors. 2003;17(1):73–82. doi: 10.1037/0893-164X.17.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnick DW, Lee MT, Chalk M, Gastfriend D, Horgan CM, McCorry F, Merrick EL. Establishing the feasibility of performance measures for alcohol and other drugs. Journal of Substance Abuse Treatment. 2002;23(4):375–385. doi: 10.1016/S0740-5472(02)00303-3. [DOI] [PubMed] [Google Scholar]
- Godley MD, Godley SH. Assertive Continuing Care for adolescents. In: Kelly JF, White WL, editors. Addiction recovery management: Theory, science, and practice. New York: Springer Science; 2011. pp. 103–126. [Google Scholar]
- Godley MD, Godley SH. Continuing care following residential treatment: History, current practice, critical issues, and emerging approaches. In: Jainchill N, editor. Understanding and treating adolescent substance use disorders: Assessment, treatment, juvenile justice responses. Kingston, NJ: Civic Research Institute; 2012. pp. 14-2–14-24. [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk R, Passetti L. Preliminary outcomes from the Assertive Continuing Care experiment for adolescents discharged from residential treatment. Journal of Substance Abuse Treatment. 2002;23(1):21–32. doi: 10.1016/S0740-5472(02)00230-1. [DOI] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL. The effect of Assertive Continuing Care (ACC) on continuing care linkage, adherence and abstinence following residential treatment for adolescents. Addiction. 2007;102(1):81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- Godley SH, Godley MD, Dennis ML. The Assertive Aftercare protocol for adolescent substance abusers. In: Wagner E, Waldron H, editors. Innovations in adolescent substance abuse interventions. New York: Elsevier Science; 2001. pp. 313–331. [Google Scholar]
- Godley SH, Godley MD, Wright KL, Funk RR, Petry N. Contingent reinforcement of personal goal activities for adolescents with substance use disorders during post-residential continuing care. American Journal on Addictions. 2008;17(4):278–286. doi: 10.1080/10550490802138798. [DOI] [PubMed] [Google Scholar]
- Godley SH, Meyers RJ, Smith JE, Godley MD, Titus JC, Karvinen T, Kelberg P. Cannabis Youth Treatment (CYT) Manual Series Volume 4. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2001. The Adolescent Community Reinforcement Approach (A-CRA) for adolescent Marijuana users. (DHHS Publication No. (SMA) 01-3489) [Google Scholar]
- Henggeler SW, Halliday-Boykins CA, Cunningham PB, Randall J, Shapiro SB, Chapman JE. Juvenile drug court: Enhancing outcomes by integrating evidence-based treatments. Journal of Consulting and Clinical Psychology. 2006;74(1):42–54. doi: 10.1037/0022-006X.74.1.42. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Silverman K, Heil SH. Contingency management in substance abuse treatment. New York: Guilford Press; 2007. [Google Scholar]
- Hser YI, Grella CE, Hubbard RL, Hsieh SC, Fletcher BW, Brown BS, Anglin D. An evaluation of drug treatments for adolescents in 4 US cities. Archives of General Psychiatry. 2001;58(7):689–695. doi: 10.1001/archpsyc.58.7.689. [DOI] [PubMed] [Google Scholar]
- Hunt GM, Azrin NH. A community-reinforcement approach to alcoholism. Behavior Research and Therapy. 1973;11:91–104. doi: 10.1016/0005-7967(73)90072-7. [DOI] [PubMed] [Google Scholar]
- Kadden RM, Litt MD, Kabela-Cormier E, Petry NM. Abstinence following behavioral treatments for marijuana dependence. Addictive Behaviors. 2007;32:1220–1236. doi: 10.1016/j.addbeh.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, Burke RH. Can assessment reactivity predict treatment outcome among adolescents with alcohol and other substance use disorders? Substance Abuse. 2008;29(2):63–69. doi: 10.1080/08897070802093262. [DOI] [PubMed] [Google Scholar]
- Kamon J, Budney A, Stanger C. A contingency management intervention for adolescent marijuana abuse and conduct problems. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:513–521. doi: 10.1097/01.chi.0000159949.82759.64. [DOI] [PubMed] [Google Scholar]
- Kim TW, Saitz R, Cheng DM, Winter MR, Witas J, Samet JH. Initiation and engagement in chronic disease management care for substance dependence. Drug and Alcohol Dependence. 2011;115(1–2):80–86. doi: 10.1016/j.drugalcdep.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Coping skills training and contingency management treatments for marijuana dependence: Exploring mechanisms of behavior change. Addiction. 2008;103:638–648. doi: 10.1111/j.1360-0443.2008.02137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Petry NM. Behavioral treatment for marijuana dependence: Randomized trial of contingency management and self-efficacy enhancement. Addictive Behaviors. 2013;38:1764–1775. doi: 10.1016/j.addbeh.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermeit [Ives] M, Funk R, Dennis ML. Data cleaning and replacement of missing values (LI Analysis Training Series) Bloomington, IL: Chestnut Health Systems; 1999. Retrieved from http://www.chestnut.org/LI/Downloads/Training_Memos/ [Google Scholar]
- McKay JR. Continuing care research: What we have learned and where we are going. Journal of Substance Abuse Treatment. 2009;36(2):131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Coviello D, Morrison R, Cary MS, Skalina L, Plebani J. Randomized trial of continuing care enhancements for cocaine-dependent patients following initial engagement. Journal of Consulting and Clinical Psychology. 2010;78(1):111–120. doi: 10.1037/a0018139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers RJ, Smith JE. Clinical guide to alcohol treatment: The Community Reinforcement Approach. New York: Guilford Press; 1995. [Google Scholar]
- Petry NM. A comprehensive guide for the application of contingency management procedures in standard clinic settings. Drug and Alcohol Dependence. 2000;58(1–2):9–25. doi: 10.1016/S0376-8716(99)00071-X. [DOI] [PubMed] [Google Scholar]
- Petry NM, Stitzer ML. Contingency management: Using motivational incentives to improve drug abuse treatment. West Haven, CT: Yale University Psychotherapy Development Center; 2002. (Yale University Psychotherapy Development Center Training Series No. 6) [Google Scholar]
- Rawson RA, Huber A, McCann M, Shoptaw S, Farabee D, Reiber C, Ling W. A comparison of contingency management and cognitive-behavioral approaches during methadone maintenance treatment for cocaine dependence. Archives of General Psychiatry. 2002;59(9):817–824. doi: 10.1001/archpsyc.59.9.817. [DOI] [PubMed] [Google Scholar]
- Saitz R, Larson MJ, LaBelle C, Richardson J, Samet JH. The case for chronic disease management for addiction. Journal of Addiction Medicine. 2008;2(2):55–65. doi: 10.1097/ADM.0b013e318166af74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPSS. Statistical Program for the Social Sciences, Version 17. Chicago: SPSS; 2007. [Google Scholar]
- Stanger C, Budney AJ, Kamon JL, Thostensen J. A randomized trial of contingency management for adolescent marijuana abuse and dependence. Drug and Alcohol Dependence. 2009;105(3):240–247. doi: 10.1016/j.drugalcdep.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality. Treatment Episode Data Set – Discharges (TEDS-D) 2009 doi: 10.3886/ICPSR33621.v1. ICPSR33621-v1, 2012-10-25. [DOI] [Google Scholar]
- Winters KC, Stinchfield R, Latimer WW, Lee S. Long-term outcome of substance-dependent youth following 12-step treatment. Journal of Substance Abuse Treatment. 2007;33:61–69. doi: 10.1016/j.jsat.2006.12.003. [DOI] [PubMed] [Google Scholar]