Abstract
The cellular prion protein PrPc is the normal counterpart of the scrapie prion protein PrP Sc, the main component of the infectious agent of transmissible spongiform encephalopathies. The recent discovery that PrP c can serve as a receptor for the amyloid beta (Aβ) peptide and relay its neurotoxicity is sparking renewed interest on this protein and its involvement in signal transduction processes. Disease-associated PrP Sc shares with Aβ the ability to hijack PrP c-dependent signaling cascades, and thereby instigate pathogenic events. Among these is an impairment of Aβ clearance, uncovered in prion-infected neuronal cells. These findings add another facet to the intricate interplay between PrP c and Aβ. Here, we summarize the connection between PrP-mediated signaling and Aβ clearance and discuss its pathological implications.
Keywords: cellular prion protein, prion infection, Aβ clearance, signal transduction, Alzheimer’s disease
INTRODUCTION
Up to recent years, commonalities between the amyloid precursor protein (APP) and the cellular prion protein PrPc were considered to mainly reside in their capacity to give rise to aggregation-prone proteins, amyloid beta (Aβ) and PrPSc (standing for scrapie isoform of the prion protein), both involved in neurodegenerative disorders, Alzheimer’s disease (AD) and transmissible spongiform encephalopathies (TSEs), respectively (Haass and Selkoe, 2007; Aguzzi and Calella, 2009). These two diseases share neuropathological features, including synaptic damage, neuronal loss and astrogliosis (Reiniger et al., 2011). As for AD, human prion diseases may have a genetic origin, while most cases are sporadic (Aguzzi and Calella, 2009). Sporadic human prion diseases are thought to arise from the spontaneous conformational conversion of PrPc into its pathogenic PrPSc counterpart (Aguzzi and Calella, 2009). PrPSc has a propensity to aggregate, form amyloid-like structures and can act as a seed to transmit its aberrant conformation to native PrPc molecules (Aguzzi and Calella, 2009). Such template-directed misfolding is also now established in the case of Aβ species [(Jucker and Walker, 2013) for review]. Like Aβ (Langer et al., 2011), much evidence suggests that PrPSc-associated toxicity is imparted by small oligomers (Silveira et al., 2005). This toxicity is assumed to be driven by the subversion of the normal function of PrPc (Harris and True, 2006), which now also emerges as a key event in Aβ-induced neuronal damage (Lauren et al., 2009). The discovery that PrPc may serve as a receptor for Aβ is calling for a better understanding of the role played by PrPc in neurons. The relationship between Aβ and PrPc actually extends beyond that of a ligand-receptor connection, since the prion-induced subversion of PrPc-dependent signaling causes impaired Aβ clearance (Pradines et al., 2013). In this review, we summarize the recent advances focusing on the Aβ-PrP duo and discuss the ensuing challenges.
THE BASICS OF PrPc
Understanding the interplay between Aβ and PrPc necessitates some focus on the latter protein. PrPc is encoded by a unique gene, Prnp, whose open reading frame is contained within a single exon (Aguzzi and Calella, 2009). While ubiquitous, this protein is most abundantly expressed in neurons (Linden et al., 2008). It is located at the outer leaflet of the plasma membrane, to which it is attached through a glycosyl-phosphatidylinositol (GPI) moiety. PrPc contains two potentially glycosylated aspargine residues, at the origin of a great diversity of isoforms (Ermonval et al., 2003). It can also undergo three types of proteolytical cleavages. The best studied are a so-called alpha-cleavage at position 111/112, yielding a N-terminal N1 fragment and a C-terminal C1 fragment, and a beta-cleavage in its N-terminal region giving rise to N2 and C2 fragments [reviewed in (Checler and Vincent, 2002), Figure 1]. The third cleavage leads to the release of a full-length anchorless isoform of PrPc through the action of the metalloprotease ADAM10 (Altmeppen et al., 2011; Figure 1). Of note, similarly to APP processing, the alpha-cleavage of PrPc occurs within a region bearing toxicity (residues 106 to 126), and may involve the TNF-alpha converting enzyme (TACE) metalloprotease (Checler and Vincent, 2002), although the nature of the proteases driving this alpha-cleavage is subject to controversy (Altmeppen et al., 2011; Beland et al., 2012). PrPc thus exists under a plethora of isoforms, whose distribution may vary in distinct brain regions, cell types or even subcellular compartments and whose respective functions remain to be thoroughly resolved (Linden et al., 2008). Clues as to PrPc normal function were greatly anticipated from the development of PrP-null mice. However, these mice are viable, develop normally and do not suffer from major abnormalities (Steele et al., 2007). Subtle behavioral and cognitive deficits were subsequently reported in PrP-deficient mice (Linden et al., 2008), in addition to an increased vulnerability to various types of stresses (Resenberger et al., 2011b). Noteworthy, these animals have been instrumental in substantiating the central role exerted by PrPc in the development of prion diseases, since the knockout of the Prnp gene confers resistance to prion infection (Bueler et al., 1993). Further, post-infection knockdown of PrPc in neurons is sufficient to counteract the progression of prion neuropathogenesis (Mallucci et al., 2003). Finally, transgenic mice expressing an anchorless variant of PrPc (ΔGPI-PrP) were found to efficiently replicate prions upon infection, while not showing any sign of neurodegeneration (Chesebro et al., 2005). Overall, it is now quite well established that neuronal, GPI-anchored PrPc serves as a relay of PrPSc-induced neuropathogenesis. On this basis, understanding the normal function held by PrPc in neurons appears as a necessary step to grasp how it is corrupted by its pathogenic counterpart, PrPSc. Actually, this notion now also applies to Aβ-related pathogenesis, as will be emphasized below.
FIGURE 1.
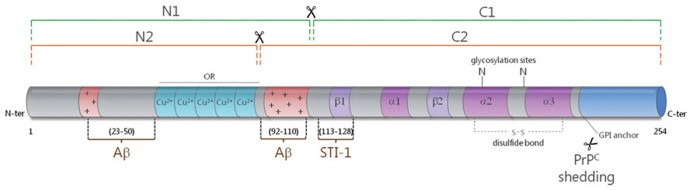
Schematic representation of the secondary structure of PrPc. The alpha-cleavage (green) occurs at position 111/112 and generates the N1 and C1 fragments. The beta-cleavage (orange) occurs in the vicinity of octapeptide repeats (ORs), which bind copper ions, and generates the N2 and C2 fragments. PrPc can also be shed from the plasma membrane through the action of ADAM10. The protective factor STI-1 binds to PrPc at amino acids 113–128. Two main binding sites have been mapped for Aβ to the very N-terminus (AA 23–50) and near the alpha-cleavage site at amino acids 92–110. The alpha helices (α) and beta sheets (β) are shown in purple and the polybasic regions (+) are shown in red.
PrPc-DEPENDENT SIGNALING IN NEURONS: FINDINGS AND IMPLICATIONS
The involvement of PrPc in signal transduction was initially suspected from its cell surface location, as well as its enrichment in lipid rafts (Lewis and Hooper, 2011), which allow the spatial segregation of cell signaling components (Parton and del Pozo, 2013). Using a neuronal cell line (1C11) endowed with the capacity to differentiate into either serotonergic (1C115-HT) or noradrenergic (1C11NE) neurons, we demonstrated that PrPc has the capacity to trigger the activation of the Fyn kinase in neuronal cells (Mouillet-Richard et al., 2000). This signaling cascade is exclusively imparted by PrPc molecules located on the neurites of differentiated cells and is relayed by the scaffold protein caveolin-1 (Mouillet-Richard et al., 2000). Downstream from Fyn, PrPc can mobilize the reactive oxygen species (ROS) generating enzyme NADPH oxidase, and the transcription factors ERK1/2, cAMP response element-binding protein (CREB), Egr-1 and c-Fos (Schneider et al., 2003; Pradines et al., 2008). From a functional point of view, the PrPc-Fyn coupling was shown to mediate neural cell adhesion molecule (NCAM)-dependent neurite outgrowth (Santuccione et al., 2005) and to control calcium influxes in hippocampal neurons (Krebs et al., 2007). As for NADPH oxidase-derived ROS, they can promote the catalytic activation of TACE, subsequent TNFα shedding and bioamine catabolism, thus exerting a neuromodulatory function (Pradines et al., 2009). The demonstration that PrPc could serve as a receptor for the chaperone protein STI-1 (Zanata et al., 2002) further set the stage for the identification of various cell signaling pathways involved in neuroprotection (Chiarini et al., 2002; Lopes et al., 2005), neurite outgrowth (Lopes et al., 2005), and/or memory consolidation (Coitinho et al., 2007). Interestingly, the contribution of PrPc to some of these processes may involve additional partners, such as laminin (Coitinho et al., 2006; Beraldo et al., 2011; Santos et al., 2013). The PrPc-STI-1 interaction was also reported to sustain neuronal protein synthesis via the mTOR pathway (Roffe et al., 2010). Finally, multiple connections have been depicted between PrPc and neurotransmitter signaling including crosstalk with serotonergic (Mouillet-Richard et al., 2005), nicotinic (Beraldo et al., 2010) and mostly glutamatergic receptors, whether metabotropic (Beraldo et al., 2011) or ionotropic (Stys et al., 2012). Collectively, there is now compelling evidence for the involvement of PrPc in multiple signal transduction cascades, whose deviation may drastically impact on neuronal function and activity.
PATHOGENIC PRIONS DEVIATE PrPcSIGNALING
While it is now acknowledged that PrPc is mandatory for the neurotoxic action of PrPSc, our current understanding of how prions corrupt the physiological function of PrPc is still far from complete (Harris and True, 2006). Achieving this goal is all the more challenging since PrPc encompasses a great variety of isoforms, which may be associated with distinct partners and sustain promiscuous functions. In addition, the repertoire of PrPc species eligible for de novo conversion into PrPSc may vary according to the prion strain and the cell type considered (Ermonval et al., 2003). Despite these hurdles, the development of in vitro modelsof prion infection has allowed to shed some light on this issue. Taking advantage of thecapacity of the 1C11 cell line to replicate various prion strains (Mouillet-Richard et al., 2008), we recently reported on the constitutive activation of signaling targets normally coupled with PrPc in chronically infected cells (Pradines et al., 2013). In these cells as well as in prion-infected neurospheres, prion accumulation is associated with increased activities of Fyn, ERK1/2 and CREB (Figure 2). Another consequence of prion infection is the recruitment of the stress-associated kinases p38 and JNK, as a result of unbalanced ROS production. Downstream from CREB, we documented that prion-infected cells exhibit a reduced activity of the matrix metalloprotease MMP-9. This observation led us to delineate an impact on the clearance of the Aβ peptide, as will be discussed below. Collectively, these findings support the view that PrPSc exerts a toxic gain of PrPc function. In line with this “gain of function” scheme, a central role of the NADPH oxidase NOX2 subunit in prion-induced neuronal damage was established using cerebellar organotypic culture slices (Falsig et al., 2012). Notwithstanding, some PrPc functions may conversely be disrupted within an infected context. One such example is the loss of TACE activity, which renders cells highly sensitive to TNFα-induced cell death (Pietri et al., 2013). The “loss of function” hypothesis accommodates well with the neuroprotective activity ascribed to PrPc (Resenberger et al., 2011b). Notably, the loss of PrPc protective function within an infected context may relate to the inability of PrPSc to undergo proteolytic processing at position 111/112 (McMahon, 2012), and thereby generate the N1 fragment, endowed with neuroprotective activity (Guillot-Sestier and Checler, 2012). Most likely, prion-associated neuropathogenesis involves both gain and loss of function events, that may altogether promote synaptic dysfunction, oxidative stress, loss of neuronal homeostasis and ultimately neurodegeneration (Kovacs and Budka, 2008).
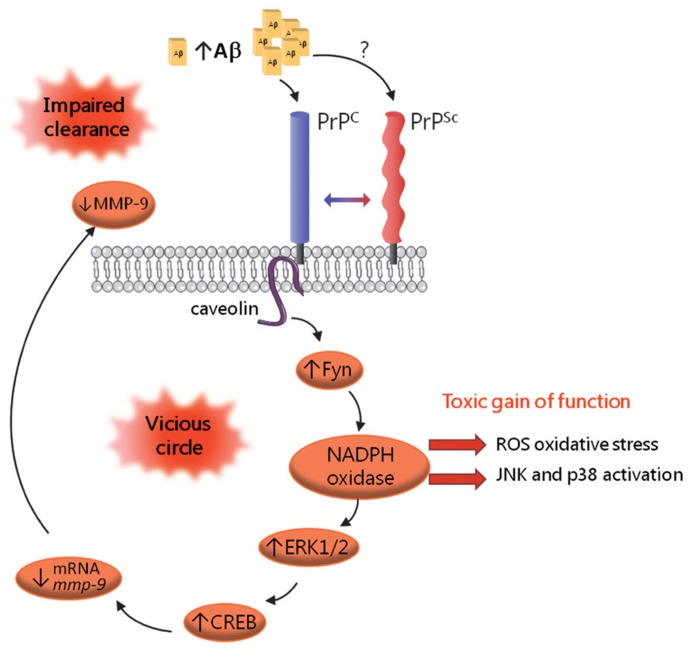
FIGURE 2.
Schematic representation of the corruption of PrPc-mediated signaling in prion-infected cells. PrPSc accumulation is associated with the constitutive recruitment of various effectors of PrPc, including the Fyn kinase, the MAP kinases ERK1/2 and the CREB transcription factor. Prion-infected cells also exhibit recruitment of the stress-associated kinases p38 and JNK, which mirrors oxidative stress conditions. A downstream event in this cascade is the drastic reduction in MMP-9 mRNAs and activity, which, in turn, causes an impairment in Aβ clearance, leading to Aβ accumulation. Aβ oligomers would bind PrPc and possibly PrPSc and further fuel the activation of this signaling cascade, thereby sustaining a vicious circle.
PrPcTRANSDUCES Aβ TOXICITY
The first demonstration that PrPc can bind Aβ came from the Strittmatter group in 2009, via an unbiased screening for receptors that could bind Aβ42 oligomers in the form of Aβ-derived diffusible ligands (ADDLs; Lauren et al., 2009). Lauren et al. (2009) mapped the interaction site to residues 92-110 in PrPc, i.e., the extremity of the N1 fragment (Figure 1), and showed that PrPc supports about 50% of Aβ binding, in line with the multiplicity of Aβ receptors (Benilova and De Strooper, 2013). In that study, the impairment of synaptic plasticity fostered by ADDL was shown to be PrPc-dependent. While the involvement of PrPc in Aβ-induced neurotoxicity was initially subject to controversy (Balducci et al., 2010; Calella et al., 2010; Kessels et al., 2010; Cisse et al., 2011), possibly as a result of distinct experimental paradigms, notably in the preparation of Aβ mixtures (Nicoll et al., 2013), all groups agreed that PrPc has very good affinity for Aβ (within the nanomolar range). Over the past three years, the contribution of PrPc as a relay of Aβ-dependent pathogenic effects has been corroborated and refined by several studies. For instance, targeting PrPc using neutralizing antibodies was shown to counteract the Aβ-mediated impairment in synaptic plasticity (Barry et al., 2011; Freir et al., 2011; Kudo et al., 2012). Molecular analyses have further revealed that Aβ oligomers crosslink PrPc to induce synaptic damage (Bate and Williams, 2011). As for PrPSc, Aβ-induced toxic signaling via PrPc requires its GPI-anchor, as well as lipid raft integrity (Resenberger et al., 2011a; Um et al., 2012; Rushworth et al., 2013). Besides, Aβ was shown to enhance the clustering of PrPc at the cell surface of neuronal cells (Caetano et al., 2011). Taken together, these studies argue that Aβ oligomers amplify the duration or strength of PrPc signaling. This scenario is also supported by several reports that have emphasized the corruption of the PrPc-Fyn signaling cascade by Aβ (Larson et al., 2012; Um et al., 2012, 2013). Um et al. (2013) were able to relate the Aβ-dependent subversion of the PrPc coupling to Fyn to overactivation of the mGluR5 or NMDA receptor (Um et al., 2012), the latter observation being recapitulated in various other studies (Resenberger et al., 2011a; You et al., 2012). Taking a step further, Larson et al. (2012) demonstrated that the PrPc-Fyn complex promotes tau hyperphosphorylation in response to oligomeric Aβ, thus providing some molecular explanation for the well-established role of Fyn as a mediator of Aβ/tau-associated toxicity (Ittner and Gotz, 2011; Roberson et al., 2011). Whether the recruitment of the PrPc-Fyn complex by Aβ impacts on additional signaling effectors such as NADPH oxidase, similarly to PrPSc (Pradines et al., 2013), deserves further investigation. Finally, the recent demonstration that the binding of Aβ to PrPc and the ensuing toxic events can be efficiently inhibited by the PrPc alternate ligand STI-1 is providing a tangible avenue to disrupt the deleterious Aβ-PrPc interaction (Ostapchenko et al., 2013).
MULTIFACETED CONTROL OF PrPc ON Aβ PRODUCTION AND AVAILABILITY
Aβ is generated from APP through the amyloidogenic processing pathway, which involves the beta-secretase BACE1 and occurs in a mutually exclusive fashion with the non-amyloidogenic pathway largely controlled by the alpha-secretase TACE (Checler and Vincent, 2002). In 2007, the Hooper group reported that PrPc decreases the amyloidogenic processing of APP, thereby decreasing Aβ levels, a property that is lost in the context of prion infection (Parkin et al., 2007). Griffiths et al. (2011) went on to show that PrPc interacts with BACE1 and controls its subcellular compartmentation. Of note, while this spatial control is protective toward the cleavage of wild-type APP, it does not prevent BACE1 from processing the Swedish mutant form of APP (Griffiths et al., 2011). Adding yet another layer of complexity to the picture, PrPc also regulates the activity of TACE, a function that is deviated in an Alzheimer’s context and causes an imbalance of APP cleavage toward the amyloidogenic pathway (Pietri et al., 2013). PrPc also regulates the availability of Aβ at several levels. For instance, PrPc could favor the accumulation of Aβ in the brain by contributing to its transcytosis across the blood brain barrier (Pflanzner et al., 2012). Finally, in accordance with the binding of Aβ to various sites located within the N-terminal region of PrPc (Chen et al., 2010; see Figure 1) and with the physiological processing of PrPc at position 111/112, the resulting PrPc-derived N1 fragment was reported to trap Aβ and thereby exert a protective action against Aβ-induced cell death (Beland et al., 2012; Guillot-Sestier et al., 2012).
HIJACKING PrPc SIGNALING BY PATHOGENIC PRIONS CAUSES IMPAIRED Aβ CLEARANCE
As mentioned above, we documented that the subversion of PrPc signaling by PrPSc in prion-infected cells leads to decreased activity of the MMP-9 metalloprotease (Pradines et al., 2013; Figure 2). MMP-9 exhibits alpha-secretase activity (Fragkouli et al., 2012) and also features among the Aβ degrading enzymes [(De Strooper, 2010) for review]. On this basis, we examined the potential outcome of the prion-dependent reduction in MMP-9 activity on Aβ metabolism. By assessing the production and elimination rates of Aβ peptides in prion-infected 1C11 cells, we substantiated an imbalance in the clearance of Aβ under prion infection, which was canceled after knockdown of the Fyn kinase (Pradines et al., 2013; Figure 2). We further observed a similarly impaired Aβ clearance in uninfected cells upon inhibition of MMP-9, highlighting the involvement of MMP-9 in this process. In agreement, we found increased levels of Aβ in the supernatants of prion-infected 1C11 cells or MMP-9 inhibitor-treated non-infected cells. Besides, we monitored an increase in the cerebrospinal fluid (CSF) levels of Aβ in mice treated with a MMP-9 inhibitor as well as in mice inoculated with prion-infected 1C11 cells. Altogether, these results delineate a reciprocal connection between PrP and Aβ that may sustain a pathogenic loop. Indeed, by promoting an accumulation of Aβ in the extracellular space, prion infection would fuel the recruitment of Fyn and its downstream targets through the interaction of Aβ with PrP, whether in its cellular or aggregated form (Chen et al., 2010; Zou et al., 2011). Whether the subversion of PrPc dependent signal transduction by Aβ in Alzheimer’s disease also negatively impacts on MMP-9 activity and thereby impinges on Aβ clearance remains to be investigated. Should it be confirmed, disrupting this vicious circle would appear as a promising avenue to combat both prion and Alzheimer’s neuropathogenesis.
CONCLUDING REMARKS
As outlined above, tremendous progress has been achieved in our understanding of the Aβ-PrPc interplay in very recent years. The bidirectional relationship between these two proteins in signal transduction cascades may account for some -once puzzling- observations that deposits of Aβ and PrP may co-occur in patients with mixed AD and CJD clinical manifestation (Muramoto et al., 1992; Hainfellner et al., 1998; Debatin et al., 2008). Beyond the various PrPc-Aβ connections summarized above, the possibility that the interaction between the two proteins may favor their aggregation in a “cross-seeding” fashion is beginning to be explored (Morales et al., 2010). Overall, the more we learn in the field, the more we appraise the complexity of the PrPc-Aβ relationship. The latest advance has further extended the points of convergence in the molecular pathogenic pathways at play in the two diseases, including loss of TACE activity (Pietri et al., 2013) and impairment of the unfolded protein response (Moreno et al., 2012; Ma et al., 2013). Striking differences however remain between the two disorders, most notably the infectious properties specific to prions (Jucker and Walker, 2013). The only partial overlap between the two pathologies may originate from the extremely diverse array of PrPc and Aβ species as well as their promiscuous partners (Linden et al., 2008; Benilova et al., 2012). Notwithstanding, the central role ascribed to PrPc in defined Aβ-related toxic pathways opens new avenues for therapeutic intervention in AD.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We apologize to colleagues in the field whose work we were unable to cite owing to space limitations. We acknowledge financial support from the ANR, INSERM, as well as the Region Ile de France (DIM-Stem Pôle).
REFERENCES
- Aguzzi A., Calella A. M. (2009). Prions: protein aggregation and infectious diseases. Physiol. Rev. 89 1105–1152 10.1152/physrev.00006.2009 [DOI] [PubMed] [Google Scholar]
- Altmeppen H. C., Prox J., Puig B., Kluth M. A., Bernreuther C., Thurm D., et al. (2011). Lack of a-disintegrin-and-metalloproteinase ADAM10 leads to intracellular accumulation and loss of shedding of the cellular prion protein in vivo. Mol. Neurodegener. 6 36 10.1186/1750-1326-6-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balducci C., Beeg M., Stravalaci M., Bastone A., Sclip A., Biasini E., et al. (2010). Synthetic amyloid-beta oligomers impair long-term memory independently of cellular prion protein. Proc. Natl. Acad. Sci. U.S.A. 107 2295–2300 10.1073/pnas.0911829107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry A. E., Klyubin I., Mc Donald J. M., Mably A. J., Farrell M. A., Scott M., et al. (2011). Alzheimer’s disease brain-derived amyloid-beta-mediated inhibition of LTP in vivo is prevented by immunotargeting cellular prion protein. J. Neurosci. 31 7259–7263 10.1523/JNEUROSCI.6500-10.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bate C., Williams A. (2011). Amyloid-beta-induced synapse damage is mediated via cross-linkage of cellular prion proteins. J. Biol. Chem. 286 37955–37963 10.1074/jbc.M111.248724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beland M., Motard J., Barbarin A., Roucou X. (2012). PrP(C) homodimerization stimulates the production of PrPC cleaved fragments PrPN1 and PrPC1. J. Neurosci. 32 13255–13263 10.1523/JNEUROSCI.2236-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benilova I, De Strooper B. (2013). Neuroscience. Promiscuous Alzheimer’s amyloid: yet another partner. Science 341 1354–1355 10.1126/science.1244166 [DOI] [PubMed] [Google Scholar]
- Benilova I., Karran E, De Strooper B. (2012). The toxic Abeta oligomer and Alzheimer’s disease: an emperor in need of clothes. Nat. Neurosci. 15 349–357 10.1038/nn.3028 [DOI] [PubMed] [Google Scholar]
- Beraldo F. H., Arantes C. P., Santos T. G., Machado C. F., Roffe M., Hajj G. N., et al. (2011). Metabotropic glutamate receptors transduce signals for neurite outgrowth after binding of the prion protein to laminin gamma1 chain. FASEB J. 25 265–279 10.1096/fj.10-161653 [DOI] [PubMed] [Google Scholar]
- Beraldo F. H., Arantes C. P., Santos T. G., Queiroz N. G., Young K., Rylett R. J., et al. (2010). Role of alpha7 nicotinic acetylcholine receptor in calcium signaling induced by prion protein interaction with stress-inducible protein 1. J. Biol. Chem. 285 36542–36550 10.1074/jbc.M110.157263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bueler H., Aguzzi A., Sailer A., Greiner R. A., Autenried P., Aguet M., et al. (1993). Mice devoid of PrP are resistant to scrapie. Cell 73 1339–1347 10.1016/0092-8674(93)90360-3 [DOI] [PubMed] [Google Scholar]
- Caetano F. A., Beraldo F. H., Hajj G. N., Guimaraes A. L., Jurgensen S., Wasilewska-Sampaio A. P., et al. (2011). Amyloid-beta oligomers increase the localization of prion protein at the cell surface. J. Neurochem. 117 538–553 10.1111/j.1471-4159.2011.07225.x [DOI] [PubMed] [Google Scholar]
- Calella A. M., Farinelli M., Nuvolone M., Mirante O., Moos R., Falsig J., et al. (2010). Prion protein and Abeta-related synaptic toxicity impairment. EMBO Mol. Med. 2 306–314 10.1002/emmm.201000082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Checler F., Vincent B. (2002). Alzheimer’s and prion diseases: distinct pathologies, common proteolytic denominators. Trends Neurosci. 25 616–620 10.1016/S0166-2236(02)02263-4 [DOI] [PubMed] [Google Scholar]
- Chen S., Yadav S. P., Surewicz W. K. (2010). Interaction between human prion protein and amyloid-beta (Abeta) oligomers: role of N-terminal residues. J. Biol. Chem. 285 26377–26383 10.1074/jbc.M110.145516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesebro B., Trifilo M., Race R., Meade-White K., Teng C., Lacasse R., et al. (2005). Anchorless prion protein results in infectious amyloid disease without clinical scrapie. Science 308 1435–1439 10.1126/science.1110837 [DOI] [PubMed] [Google Scholar]
- Chiarini L. B., Freitas A. R., Zanata S. M., Brentani R. R., Martins V. R., Linden R. (2002). Cellular prion protein transduces neuroprotective signals. EMBO J. 21 3317–3326 10.1093/emboj/cdf324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cisse M., Halabisky B., Harris J., Devidze N., Dubal D. B., Sun B., et al. (2011). Reversing EphB2 depletion rescues cognitive functions in Alzheimer model. Nature 469 47–52 10.1038/nature09635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coitinho A. S., Freitas A. R., Lopes M. H., Hajj G. N., Roesler R., Walz R., et al. (2006). The interaction between prion protein and laminin modulates memory consolidation. Eur. J. Neurosci. 24 3255–3264 10.1111/j.1460-9568.2006.05156.x [DOI] [PubMed] [Google Scholar]
- Coitinho A. S., Lopes M. H., Hajj G. N., Rossato J. I., Freitas A. R., Castro C. C., et al. (2007). Short-term memory formation and long-term memory consolidation are enhanced by cellular prion association to stress-inducible protein 1. Neurobiol. Dis. 26 282–290 10.1016/j.nbd.2007.01.005 [DOI] [PubMed] [Google Scholar]
- Debatin L., Streffer J., Geissen M., Matschke J., Aguzzi A., Glatzel M. (2008). Association between deposition of beta-amyloid and pathological prion protein in sporadic Creutzfeldt-Jakob disease. Neurodegener. Dis. 5 347–354 10.1159/000121389 [DOI] [PubMed] [Google Scholar]
- De Strooper B. (2010). Proteases and proteolysis in Alzheimer disease: a multifactorial view on the disease process. Physiol. Rev. 90 465–494 10.1152/physrev.00023.2009 [DOI] [PubMed] [Google Scholar]
- Ermonval M., Mouillet-Richard S., Codogno P., Kellermann O., Botti J. (2003). Evolving views in prion glycosylation: functional and pathological implications. Biochimie 85 33–45 10.1016/S0300-9084(03)00040-3 [DOI] [PubMed] [Google Scholar]
- Falsig J., Sonati T., Herrmann U. S., Saban D., Li B., Arroyo K., et al. (2012). Prion pathogenesis is faithfully reproduced in cerebellar organotypic slice cultures. PLoS Pathog. 8:e1002985 10.1371/journal.ppat.1002985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fragkouli A., Papatheodoropoulos C., Georgopoulos S., Stamatakis A., Stylianopoulou F., Tsilibary E. C., et al. (2012). Enhanced neuronal plasticity and elevated endogenous sAPPalpha levels in mice over-expressing MMP9. J. Neurochem. 121 239–251 10.1111/j.1471-4159.2011.07637.x [DOI] [PubMed] [Google Scholar]
- Freir D. B., Nicoll A. J., Klyubin I., Panico S., Mc Donald J. M., Risse E., et al. (2011). Interaction between prion protein and toxic amyloid beta assemblies can be therapeutically targeted at multiple sites. Nat. Commun. 2 336 10.1038/ncomms1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths H. H., Whitehouse I. J., Baybutt H., Brown D., Kellett K. A., Jackson C. D., et al. (2011). Prion protein interacts with BACE1 protein and differentially regulates its activity toward wild type and Swedish mutant amyloid precursor protein. J. Biol. Chem. 286 33489–33500 10.1074/jbc.M111.278556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillot-Sestier M. V., Checler F. (2012). α-Secretase-derived cleavage of cellular prion yields biologically active catabolites with distinct functions. Neurodegener. Dis. 10 294–297 10.1159/000333804 [DOI] [PubMed] [Google Scholar]
- Guillot-Sestier M. V., Sunyach C., Ferreira S. T., Marzolo M. P., Bauer C., Thevenet A., et al. (2012). α-Secretase-derived fragment of cellular prion, N1, protects against monomeric and oligomeric amyloid beta (Abeta)-associated cell death. J. Biol. Chem. 287 5021–5032 10.1074/jbc.M111.323626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haass C., Selkoe D. J. (2007). Soluble protein oligomers in neurodegeneration: lessons from the Alzheimer’s amyloid beta-peptide. Nat. Rev. Mol. Cell Biol. 8 101–112 10.1038/nrm2101 [DOI] [PubMed] [Google Scholar]
- Hainfellner J. A., Wanschitz J., Jellinger K., Liberski P. P., Gullotta F., Budka H. (1998). Coexistence of Alzheimer-type neuropathology in Creutzfeldt-Jakob disease. Acta Neuropathol. 96 116–122 10.1007/s004010050870 [DOI] [PubMed] [Google Scholar]
- Harris D. A., True H. L. (2006). New insights into prion structure and toxicity. Neuron 50 353–357 10.1016/j.neuron.2006.04.020 [DOI] [PubMed] [Google Scholar]
- Ittner L. M., Gotz J. (2011). Amyloid-beta and tau--a toxic pas de deux in Alzheimer’s disease. Nat. Rev. Neurosci. 12 65–72 10.1038/nrn2967 [DOI] [PubMed] [Google Scholar]
- Jucker M., Walker L. C. (2013). Self-propagation of pathogenic protein aggregates in neurodegenerative diseases. Nature 501 45–51 10.1038/nature12481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessels H. W., Nguyen L. N., Nabavi S., Malinow R. (2010). The prion protein as a receptor for amyloid-beta. Nature 466 E3–E4; discussion E4–E5. 10.1038/nature09217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs G. G., Budka H. (2008). Prion diseases: from protein to cell pathology. Am. J. Pathol. 172 555–565 10.2353/ajpath.2008.070442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs B., Wiebelitz A., Balitzki-Korte B., Vassallo N., Paluch S., Mitteregger G., et al. (2007). Cellular prion protein modulates the intracellular calcium response to hydrogen peroxide. J. Neurochem. 100 358–367 10.1111/j.1471-4159.2006.04256.x [DOI] [PubMed] [Google Scholar]
- Kudo W., Lee H. P., Zou W. Q., Wang X., Perry G., Zhu X., et al. (2012). Cellular prion protein is essential for oligomeric amyloid-beta-induced neuronal cell death. Hum. Mol. Genet. 21 1138–1144 10.1093/hmg/ddr542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer F., Eisele Y. S., Fritschi S. K., Staufenbiel M., Walker L. C., Jucker M. (2011). Soluble Abeta seeds are potent inducers of cerebral beta-amyloid deposition. J. Neurosci. 31 14488–14495 10.1523/JNEUROSCI.3088-11.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson M., Sherman M. A., Amar F., Nuvolone M., Schneider J. A., Bennett D. A., et al. (2012). The complex PrP(c)-Fyn couples human oligomeric Abeta with pathological tau changes in Alzheimer’s disease. J. Neurosci. 32 16857–16871a 10.1523/JNEUROSCI.1858-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauren J., Gimbel D. A., Nygaard H. B., Gilbert J. W., Strittmatter S. M. (2009). Cellular prion protein mediates impairment of synaptic plasticity by amyloid-beta oligomers. Nature 457 1128–1132 10.1038/nature07761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis V., Hooper N. M. (2011). The role of lipid rafts in prion protein biology. Front. Biosci. 16:151–168 10.2741/3681 [DOI] [PubMed] [Google Scholar]
- Linden R., Martins V. R., Prado M. A., Cammarota M., Izquierdo I., Brentani R. R. (2008). Physiology of the prion protein. Physiol. Rev. 88 673–728 10.1152/physrev.00007.2007 [DOI] [PubMed] [Google Scholar]
- Lopes M. H., Hajj G. N., Muras A. G., Mancini G. L., Castro R. M., Ribeiro K. C., et al. (2005). Interaction of cellular prion and stress-inducible protein 1 promotes neuritogenesis and neuroprotection by distinct signaling pathways. J. Neurosci. 25 11330–11339 10.1523/JNEUROSCI.2313-05.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma T., Trinh M. A., Wexler A. J., Bourbon C., Gatti E., Pierre P., et al. (2013). Suppression of eIF2alpha kinases alleviates Alzheimer’s disease-related plasticity and memory deficits. Nat. Neurosci. 16 1299–1305 10.1038/nn.3486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallucci G., Dickinson A., Linehan J., Klohn P. C., Brandner S., Collinge J. (2003). Depleting neuronal PrP in prion infection prevents disease and reverses spongiosis. Science 302 871–874 10.1126/science.1090187 [DOI] [PubMed] [Google Scholar]
- McMahon H. E. (2012). Prion processing: a double-edged sword? Biochem. Soc. Trans. 40 735–738 10.1042/BST20120031 [DOI] [PubMed] [Google Scholar]
- Morales R., Estrada L. D., Diaz-Espinoza R., Morales-Scheihing D., Jara M. C., Castilla J., et al. (2010). Molecular cross talk between misfolded proteins in animal models of Alzheimer’s and prion diseases. J. Neurosci. 30 4528–4535 10.1523/JNEUROSCI.5924-09.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno J. A., Radford H., Peretti D., Steinert J. R., Verity N., Martin M. G., et al. (2012). Sustained translational repression by eIF2alpha-P mediates prion neurodegeneration. Nature 485 507–511 10.1038/nature11058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouillet-Richard S., Ermonval M., Chebassier C., Laplanche J. L., Lehmann S., Launay J. M., et al. (2000). Signal transduction through prion protein. Science 289 1925–1928 10.1126/science.289.5486.1925 [DOI] [PubMed] [Google Scholar]
- Mouillet-Richard S., Nishida N., Pradines E., Laude H., Schneider B., Feraudet C., et al. (2008). Prions impair bioaminergic functions through serotonin- or catecholamine-derived neurotoxins in neuronal cells. J. Biol. Chem. 283 23782–23790 10.1074/jbc.M802433200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouillet-Richard S., Pietri M., Schneider B., Vidal C., Mutel V., Launay J. M., et al. et al. (2005). Modulation of serotonergic receptor signaling and cross-talk by prion protein. J. Biol. Chem. 280 4592–4601 10.1074/jbc.M406199200 [DOI] [PubMed] [Google Scholar]
- Muramoto T., Kitamoto T., Koga H., Tateishi J. (1992). The coexistence of Alzheimer’s disease and Creutzfeldt-Jakob disease in a patient with dementia of long duration. Acta Neuropathol. 84 686–689 10.1007/BF00227747 [DOI] [PubMed] [Google Scholar]
- Nicoll A. J., Panico S., Freir D. B., Wright D., Terry C., Risse E., et al. (2013). Amyloid-beta nanotubes are associated with prion protein-dependent synaptotoxicity. Nat. Commun. 4 2416 10.1038/ncomms3416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostapchenko V. G., Beraldo F. H., Mohammad A. H., Xie Y. F., Hirata P. H., Magalhaes A. C., et al. (2013). The prion protein ligand, stress-inducible phosphoprotein 1, regulates amyloid-beta oligomer toxicity. J. Neurosci. 33 16552–16564 10.1523/JNEUROSCI.3214-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkin E. T., Watt N. T., Hussain I., Eckman E. A., Eckman C. B., Manson J. C., et al. (2007). Cellular prion protein regulates beta-secretase cleavage of the Alzheimer’s amyloid precursor protein. Proc. Natl. Acad. Sci. U.S.A. 104 11062–11067 10.1073/pnas.0609621104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parton R. G, del Pozo M. A. (2013). Caveolae as plasma membrane sensors, protectors and organizers. Nat. Rev. Mol. Cell Biol. 14 98–112 10.1038/nrm3512 [DOI] [PubMed] [Google Scholar]
- Pflanzner T., Petsch B., Andre-Dohmen B., Muller-Schiffmann A., Tschickardt S., Weggen S., et al. (2012). Cellular prion protein participates in amyloid-beta transcytosis across the blood-brain barrier. J. Cereb. Blood Flow Metab. 32 628–632 10.1038/jcbfm.2012.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietri M., Dakowski C., Hannaoui S., Alleaume-Butaux A., Hernandez-Rapp J., Ragagnin A., et al. (2013). PDK1 decreases TACE-mediated alpha-secretase activity and promotes disease progression in prion and Alzheimer’s diseases. Nat. Med. 19 1124–1131 10.1038/nm.3302 [DOI] [PubMed] [Google Scholar]
- Pradines E., Hernandez-Rapp J., Villa-Diaz A., Dakowski C., Ardila-Osorio H., Haik S., et al. (2013). Pathogenic prions deviate PrP(C) signaling in neuronal cells and impair A-beta clearance. Cell Death Dis. 4:e456 10.1038/cddis.2012.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pradines E., Loubet D., Mouillet-Richard S., Manivet P., Launay J. M., Kellermann O., et al. (2009). Cellular prion protein coupling to TACE-dependent TNF-alpha shedding controls neurotransmitter catabolism in neuronal cells. J. Neurochem. 110 912–923 10.1111/j.1471-4159.2009.06176.x [DOI] [PubMed] [Google Scholar]
- Pradines E., Loubet D., Schneider B., Launay J. M., Kellermann O., Mouillet-Richard S. (2008). CREB-dependent gene regulation by prion protein: impact on MMP-9 and beta-dystroglycan. Cell. Signal. 20 2050–2058 10.1016/j.cellsig.2008.07.016 [DOI] [PubMed] [Google Scholar]
- Reiniger L., Lukic A., Linehan J., Rudge P., Collinge J., Mead S., et al. (2011). Tau, prions and Abeta: the triad of neurodegeneration. Acta Neuropathol. 121 5–20 10.1007/s00401-010-0691-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resenberger U. K., Harmeier A., Woerner A. C., Goodman J. L., Muller V., Krishnan R., et al. (2011a). The cellular prion protein mediates neurotoxic signalling of beta-sheet-rich conformers independent of prion replication. EMBO J. 30 2057–2070 10.1038/emboj.2011.86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resenberger U. K., Winklhofer K. F., Tatzelt J. (2011b). Neuroprotective and neurotoxic signaling by the prion protein. Top. Curr. Chem. 305 101–119 10.1007/128_2011_160 [DOI] [PubMed] [Google Scholar]
- Roberson E. D., Halabisky B., Yoo J. W., Yao J., Chin J., Yan F., et al. (2011). Amyloid-beta/Fyn-induced synaptic, network, and cognitive impairments depend on tau levels in multiple mouse models of Alzheimer’s disease. J. Neurosci. 31 700–711 10.1523/JNEUROSCI.4152-10.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roffe M., Beraldo F. H., Bester R., Nunziante M., Bach C., Mancini G., et al. (2010). Prion protein interaction with stress-inducible protein 1 enhances neuronal protein synthesis via mTOR. Proc. Natl. Acad. Sci. U.S.A. 107 13147–13152 10.1073/pnas.1000784107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rushworth J. V., Griffiths H. H., Watt N. T., Hooper N. M. (2013). Prion protein-mediated toxicity of amyloid-beta oligomers requires lipid rafts and the transmembrane LRP1. J. Biol. Chem. 288 8935–8951 10.1074/jbc.M112.400358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos T. G., Beraldo F. H., Hajj G. N., Lopes M. H., Roffe M., Lupinacci F. C., et al. (2013). Laminin-gamma1 chain and stress inducible protein 1 synergistically mediate PrPC-dependent axonal growth via Ca2+ mobilization in dorsal root ganglia neurons. J. Neurochem. 124 210–223 10.1111/jnc.12091 [DOI] [PubMed] [Google Scholar]
- Santuccione A., Sytnyk V., Leshchyns’ka I., Schachner M. (2005). Prion protein recruits its neuronal receptor NCAM to lipid rafts to activate p59fyn and to enhance neurite outgrowth. J. Cell Biol. 169 341–354 10.1083/jcb.200409127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider B., Mutel V., Pietri M., Ermonval M., Mouillet-Richard S., Kellermann O. (2003). NADPH oxidase and extracellular regulated kinases 1/2 are targets of prion protein signaling in neuronal and nonneuronal cells. Proc. Natl. Acad. Sci. U.S.A. 100 13326–13331 10.1073/pnas.2235648100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silveira J. R., Raymond G. J., Hughson A. G., Race R. E., Sim V. L., Hayes S. F., et al. (2005). The most infectious prion protein particles. Nature 437 257–261 10.1038/nature03989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele A. D., Lindquist S., Aguzzi A. (2007). The prion protein knockout mouse: a phenotype under challenge. Prion 1 83–93 10.4161/pri.1.2.4346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stys P. K., You H., Zamponi G. W. (2012). Copper-dependent regulation of NMDA receptors by cellular prion protein: implications for neurodegenerative disorders. J. Physiol. 590 1357–1368 10.1113/jphysiol.2011.225276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Um J. W., Kaufman A. C., Kostylev M., Heiss J. K., Stagi M., Takahashi H., et al. (2013). Metabotropic glutamate receptor 5 is a coreceptor for Alzheimer abeta oligomer bound to cellular prion protein. Neuron 79 887–902 10.1016/j.neuron.2013.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Um J. W., Nygaard H. B., Heiss J. K., Kostylev M. A., Stagi M., Vortmeyer A., et al. (2012). Alzheimer amyloid-beta oligomer bound to postsynaptic prion protein activates Fyn to impair neurons. Nat. Neurosci. 15 1227–1235 10.1038/nn.3178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- You H., Tsutsui S., Hameed S., Kannanayakal T. J., Chen L., Xia P., et al. (2012). Abeta neurotoxicity depends on interactions between copper ions, prion protein, and N-methyl-D-aspartate receptors. Proc. Natl. Acad. Sci. U.S.A. 109 1737–1742 10.1073/pnas.1110789109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanata S. M., Lopes M. H., Mercadante A. F., Hajj G. N., Chiarini L. B., Nomizo R., et al. (2002). Stress-inducible protein 1 is a cell surface ligand for cellular prion that triggers neuroprotection. EMBO J. 21 3307–3316 10.1093/emboj/cdf325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou W. Q., Xiao X., Yuan J., Puoti G., Fujioka H., Wang X., et al. (2011). Amyloid-beta42 interacts mainly with insoluble prion protein in the Alzheimer brain. J. Biol. Chem. 286 15095–15105 10.1074/jbc.M110.199356 [DOI] [PMC free article] [PubMed] [Google Scholar]