Abstract
Background
Accumulation of β-amyloid protein (Aβ) and tau protein is the main feature of Alzheimer disease neuropathogenesis. Anesthetic isoflurane, but not desflurane, may increase Aβ levels in vitro and in animals. Therefore, we set out to determine the efects of isoflurane and desflurane on cerebrospinal fuid (CSF) levels of Aβ and tau in humans.
Methods
The participants were assigned into spinal anesthesia (N = 35), spinal plus desflurane anesthesia (N = 33), or spinal plus isoflurane anesthesia (N = 38) group by randomization using computer-generated lists. Pre- and postoperative human CSF samples were obtained through an inserted spinal catheter. The levels of Aβ (Aβ40 and Aβ42) and total tau in the CSF were determined.
Results
Here, we show that isoflurane, but not desflurane, was associated with an increase in human CSF Aβ40 levels (from 10.90 to 12.41 ng/ml) 24 h after the surgery under anesthesia compared to spinal anesthesia (from 11.59 to 11.08 ng/ml), P = 0.022. Desflurane, but not isoflurane, was associated with a decrease in Aβ42 levels 2 h after the surgery under anesthesia (from 0.39 to 0.35 ng/ml) compared to spinal anesthesia (from 0.43 to 0.44 ng/ml), P = 0.006. Isoflurane and desflurane did not significantly affect the tau levels in human CSF.
Conclusions
These studies have established a system to study the effects of anesthetics on human biomarkers associated with Alzheimer disease and cognitive dysfunction. These findings have suggested that isoflurane and desflurane may have different effects on human CSF Aβ levels.
An estimated 234 million patients worldwide undergo anesthesia and surgery each year. Even though the incidence of Alzheimer disease (AD) may not be increased by anesthesia,1 the age of AD onset was reported to be inversely related to cumulative exposure to anesthesia and surgery before the age of 50 yrs.2 Several other studies have also suggested general anesthesia as one of the risk factors for AD.3,4 Opposing findings, however, do exist,5–7 and therefore more research, especially human studies aimed to define the role of anesthesia in AD neuropathogenesis, is necessary.8,9
Excessive production and/or accumulation of β-amyloid protein (Aβ), predominantly including Aβ40 and Aβ42, plays a fundamental role in the neuropathogenesis of AD.10–13 In addition, recent studies have suggested the contribution of Aβ40 in AD neuropathogenesis.14,15 Furthermore, Aβ40 has been shown to induce caspase activation and apoptosis16–18 and to impair synaptic plasticity and memory function..19,20
In addition to Aβ, the accumulation, abnormal aggregation, and deposition of tau play a key role in AD neuropathogenesis.21 As the major protein component of intraneuronal neurofibrillary tangles, elevation of total tau levels (two- to threefold) is seen in the cerebrospinal fluid (CSF) of AD patients compared to nondemented elderly adults.22,23 Moreover, a reduced ratio of Aβ42 to tau in the CSF has been suggested as one of the biomarkers of AD.23,24
Several studies have suggested that the commonly used inhalation anesthetic isoflurane can increase Aβ accumulation in cultured cells, neurons, and animals.9,25–29 The isoflurane has been shown to increase levels of phosphorylated, but not total, tau in brain tissues of mice.30 In contrast, another commonly used inhalation anesthetic desflurane has been shown not to increase Aβ levels in cultured cells.31 However, the in vivo relevance of these acute effects of isoflurane on Aβ levels in humans has not yet been assessed. In this study, we set out to determine the effects of surgery under spinal (S) anesthesia alone, spinal plus desflurane (SD) anesthesia, and spinal plus isoflurane (SI) anesthesia on the acute changes in CSF Aβ levels in human participants. We also assessed the effects of surgery under S, SD, and SI anesthesia on total tau levels in human CSF and calculated the ratios of Aβ40 or Aβ42 to tau. We hypothesized, based on the in vitro and animal studies, that isoflurane, but not desflurane, would increase the human CSF Aβ levels.
Materials and Methods
The Participants
The protocol was approved by the research Ethics Committee in the Capital Medical University in Beijing, P.R. China, and the institutional review board of Partners Human Research Committee, Boston, Massachusetts. Eligible participants were American Society of Anesthesiologists I or II patients between 60 and 75 yrs of age who had either lower extremity or lower abdominal surgery under S anesthesia alone, SD anesthesia, or SI anesthesia in the Beijing Friendship Hospital, Capital Medical University, Beijing, China. The exclusion criteria included (1) patients below 64 yr and over 73 yr of age; (2) patients who cannot accept continuous spinal anesthesia; (3) patients with neurological or psychiatric disorders; (4) American Society of Anesthesiologists III or IV patients; (5) patients with contraindications for spinal anesthesia and the local anesthetics; (6) patients with serious anxiety and depression or with pulmonary infection; pulmonary embolism; cerebral thrombosis/ hemorrhage; (7) patients participating in other clinical trials.
The Anesthesia
The study has a parallel arm trial design. After obtaining the signed consent form, all the participants had spinal anesthesia with a spinal anesthesia catheter (Fajunk, Geisingen, Germany) and were assigned to the spinal anesthesia alone (S, N = 35), the SD anesthesia (SD, N = 33), or the SI anesthesia (SI, N = 38) group by randomization using computer-generated lists. The numbers of patients in the current studies were simply enrolled and no patients were lost for observation because they all need anesthesiologists to remove the spinal catheters at 24 h after the anesthesia. In all, 1.5 ml CSF was obtained before the administration of local anesthetic (2 ml of 1% tetracaine) in the patients in S, SD, and SI anesthesia groups. The participants in S anesthesia group did not receive sedative medicines. General anesthesia was induced with 1.5–2.0 mg/kg propofol (AstraZeneca, Beijing, China) to the participants in the SD and SI anesthesia groups. The patients were not intubated, rather a laryngeal mask airway (a device to help patient to breath) was inserted in the mouth of participants who had general anesthesia. Desflurane (Baxter, Deerfield, IL) or isoflurane (Baxter) was administrated to the participants in SD or SI anesthesia groups from an anesthesia machine through the laryngeal mask airway, respectively. Standard anesthesia care was applied, including routine monitors with electrocardiogram, blood pressure, and oxygen saturation. All of the participants had Bispectral Index monitor to determine the relative depth of the general anesthesia. The desflurane or isoflurane concentration was adjusted to maintain the bispectral index value between 50 and 60. Desflurane or isoflurane anesthesia was given for 2 h and no other anesthetics was administrated. The CSF was obtained again at 2 and 24 h after the start of the S, SD, or SI anesthesia through the inserted spinal catheter. The spinal catheter was removed immediately following the CSF withdrawal at 24 h after the anesthesia. There was no significant difference in pain scale or opiate usage in patients among S, SD, and SI anesthesia groups after the surgery. We only included patients who had the first surgery of the day in our studies. Thus, the times at which CSF was collected (baseline, 2 h, and 24 h after the anesthesia and surgery) were similar among the patients, which avoids the confounding influence from the normal hour-to-hour variation in CSF Aβ levels as described in previous studies.32
CSF Aβ and Tau Measurement
Aβ levels (including Aβ40 and Aβ42) in the CSF were measured using enzyme-linked immunosorbent assay kits (Wako, Richmond, VA) as described by Zhang et al.31 with modification. Briefly, the collected CSF was stored in a −80° freezer and was thawed before measurement. The sample was centrifuged at 3,000 rpm for 5 min, and then was diluted to 5- and 50-fold for the Aβ42 and Aβ40 measurements, respectively, with artificial CSF. Then, 96-well plates were coated with human monoclonal antibodies specific to Aβ40 (BA27) or Aβ42 (BC05). Following the blocking with Block Ace, wells were incubated overnight at 4°C with test samples of CSF, and then an anti-Aβ (α-Aβ-HR1) conjugated to horseradish peroxidase was added. The plates were developed with 3,3’,5,5’ tetramethylbenzidine reagent, and the well absorbance was measured at 450 nm. The Aβ levels in the test samples were determined by comparison with the signals from unconditioned artificial CSF spiked with known quantities of Aβ40 and Aβ42. The levels of tau in human CSF were determined with an enzyme-linked immunosorbent assay kit (Invitrogen, San Francisco, CA). Specifically, a monoclonal antibody specific for human tau was coated onto the wells of the provided microtiter strips. Standards of known human tau content, CSF, and control specimens were pipetted into these wells overnight. After washing, a rabbit polyclonal antibody specific for human tau was added. During the second incubation, this antibody bound to the immobilized human tau captured during the first incubation. After removal of the excess of the second antibody, a horseradish peroxidase-labeled anti-rabbit antibody was added. This bound to the rabbit polyclonal antibody to complete the four-member sandwich. After a third incubation and washing to remove the excess anti-rabbit antibody, a substrate solution was added, which was acted upon by the bound enzyme to produce a change in color. The intensity of this colored product was directly proportional to the concentration of human tau present in the CSF. The range of detection for total tau was 0–20,000 pg/ml. All of the assays were performed in triplicates and the average from the triplicates was obtained. The effects of S, SD, or SI anesthesia on the human CSF Aβ (and tau) levels were presented as raw data.
Statistics
Since the in vitro and the animal studies have suggested that isoflurane, but not desflurane, can increase Aβ levels, the primary outcomes in our human relevant studies were Aβ40 and Aβ42 levels in human CSF. We also measured tau levels in the CSF. The data were presented as mean ± standard deviation. We applied one two-way repeated measures ANOVA to compare the differences in changes in the outcome (e.g., Aβ40) among the S, SD, and SI anesthesia groups. Bonferroni adjustment was applied to account for multiple comparisons. The one-way ANOVA with post hoc Bonferroni test was used to compare the difference in bispectral index value and admission characteristics (e.g., age and heart rate) in the participants of S, SD, and SI anesthesia groups. We initially enrolled 17, 15, and 20 participants in the S, SD, and SI anesthesia groups, respectively. An article based on the findings from the study was reviewed and the study was determined to be underpowered. In response to reviewers’ criticism, we performed power analysis based on the results from the original studies and found that at least 33 participants in each arm would be needed to achieve 80% power to determine the difference in Aβ and tau values between each arm. We therefore performed additional studies and increased 18 participants in each group to the sample size of 35, 33, and 38 participants in the S, SD, and SI groups, respectively. To control the overall type 1 error in the two phases of analysis, we decided to use a conservative threshold of P < 0.025 for statistical significance in the analysis of the data obtained from the combination of both original and second set of participants. We used SAS software (Cary, NC) to analyze the data.
Results
A total of 106 participants were included in the studies. Among them, 55 participants were men and 51 were women. The age of these participants were between 64 and 73 yrs. These participants were randomly assigned into three groups (S, SD, and SI). There was no significant difference in age, height, body weight, education, sex ratio, American Society of Anesthesiologists classification, length of anesthesia, length and type of surgery, estimated blood loss, heart rate, or mean arterial pressure in the participants among the S, SD, and SI anesthesia groups (table 1). The study procedures were well tolerated and there were no adverse events associated with anesthesia in any of the participants.
Table 1.
Admission Characteristics of Study Population
| S (N = 35) | SD (N = 33) | SI (N = 38) | |
|---|---|---|---|
| Age, yr | 69.2 ± 2.1 | 68.8 ± 2.5 | 69.3 ± 3.1 |
| Height, cm | 168.2 ± 7.9 | 167.6 ± 8.1 | 168.3 ± 8.3 |
| Body weight, kg | 67.8 ± 6.1 | 67.3 ± 7.1 | 66.9± 7.9 |
| Education, yr | 8.4 ± 2.3 | 8.1 ± 2.7 | 8.2 ± 2.5 |
| Sex (M/F) | 19/16 | 16/17 | 20/18 |
| ASA I | 12 | 11 | 13 |
| ASA II | 23 | 22 | 25 |
| Length of anesthesia, min | 172.5 ± 22.9 | 173.03 ± 23.1 | 171.8 ± 21.9 |
| Length of surgery, min | 133.3 ± 22.6 | 132.8 ± 23.1 | 134.2 ± 22.8 |
| Orthopedic surgery | 25 | 23 | 26 |
| Abdominal surgery | 10 | 10 | 12 |
| Estimated blood loss, ml | 190.8 ± 161.2 | 182.3 ± 162.8 | 174.9± 158.7 |
| Heart rate | 74.7 ± 7.4 | 73.1 ± 7.0 | 72.7 ± 5.4 |
| Mean arterial pressure | 78.5 ± 7.2 | 76.2 ± 4.3 | 76.1 ± 4.4 |
The age, height, body weight, education, sex ratio, ASA classification, length of anesthesia, length and type of surgery, and estimated blood loss are similar between the surgery under S (N = 35), SD (N = 33), and SI (N = 38) anesthesia group.
ASA = American Society of Anesthesiologists; S = spinal; SD = spinal plus desflurane; SI = spinal plus isoflurane.
The preoperative baseline Aβ40 and Aβ42 levels among the S, SD, and SI anesthesia groups were not significantly different (table 2), Aβ40: F = 2.37, P = 0.10; and Aβ42: F = 1.68, P = 0.19. The concentration of isoflurane (between 1 and 1.5%) or desflurane (between 6 and 9%) was adjusted to maintain a bispectral index value between 50 and 60. These bispectral index values indicate a satisfactory level of anesthesia. Bispectral index value was similar between SD (57% ± 7) and SI (59 ± 6) anesthesia groups, but both of them were lower than that of the S (96% ± 4) anesthesia group. There was no significant difference between baseline and postoperative 2- or 24-h human CSF levels of Aβ40, Aβ42, and tau in all of the participants (grouping effects) (data not shown). These data suggested that the surgery might not signiificantly alter the CSF Aβ and tau levels in the current studies.
Table 2.
Preoperative Baseline CSF Aβ Levels between S, SD, and SI Anesthesia Groups
| S (N = 35) | SD (N = 33) | SI (N = 38) | F Values | P Values | |
|---|---|---|---|---|---|
| Aβ40, ng/ml | 11.59 ± 2.73 | 12.35 ± 2.90 | 10.90 ± 2.6 | 2.37 | 0.10 |
| Aβ42, ng/ml | 0.43 ± 0.95 | 0.39 ± 0.09 | 0.39 ± 0.11 | 1.68 | 0.19 |
The preoperative baseline Aβ40 and Aβ42 levels are not significantly different among surgery under S (N = 35), SD (N = 33), and SI (N = 38) anesthesia groups.
Aβ = β-amyloid protein; CSF = cerebrospinal fluid; S = spinal; SD = spinal plus desflurane; SI = spinal plus isoflurane.
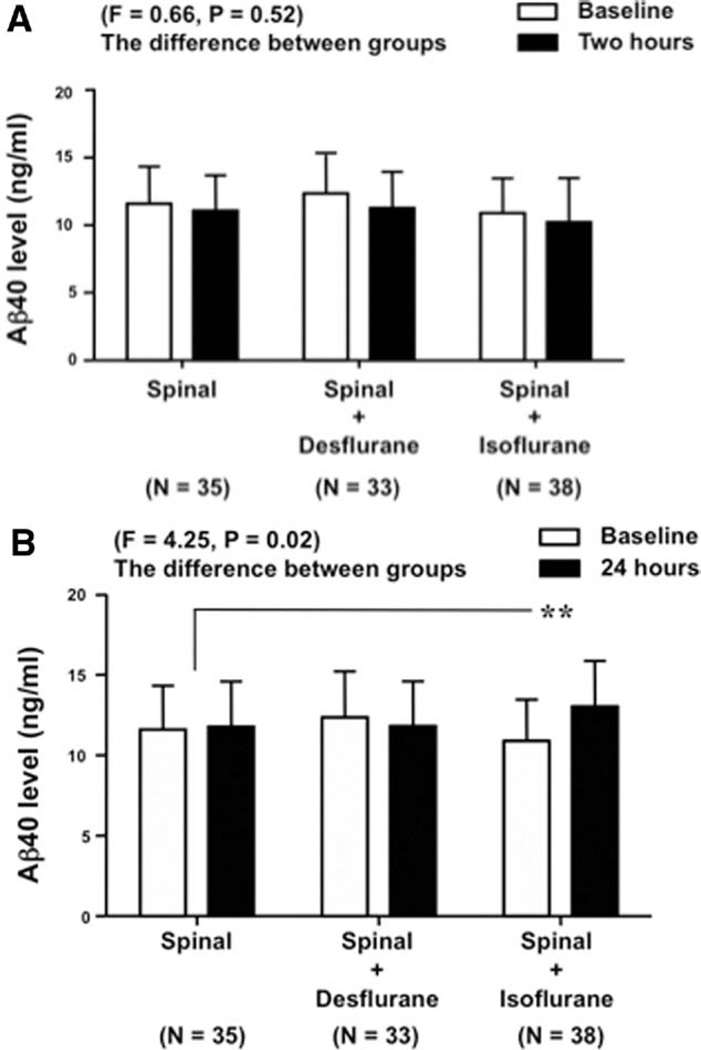
We first assessed the effects of isoflurane and desflurane on CSF Aβ40 levels at 2 and 24 h after the surgery under anesthesia. The mean of preoperative baseline and the 2-h postoperative CSF Aβ40 levels in the S, SD, and SI anesthesia groups were 11.59 ± 2.73 and 11.08 ± 2.59, 12.35 ± 2.86 and 11.28 ± 2.67, and 10.90 ± 2.56 and 10.23 ± 3.25 ng/ml, respectively (fig. 1A). Two-way repeated measures ANOVA showed no significant difference in human CSF Aβ40 levels between SI or SD with S at 2 h after the surgery under anesthesia (F = 0.66, P = 0.52, N.S.). The difference between the 2-h postoperative and the preoperative baseline CSF Aβ40 levels following SI (F = 0.12, P = 0.73, N.S.) or SD (F = 1.26, P = 0.26, N.S.) was not statistically different from that following S anesthesia. These findings suggest that isoflurane or desflurane may not alter the CSF Aβ40 levels at 2 h after the surgery under the anesthesia.
Fig. 1.
Surgery under isoflurane anesthesia is associated with increases in human cerebrospinal fluid (CSF) β-amyloid protein (Aβ)40 levels 24 h after the anesthesia. The preoperative baseline, the 2- and 24-h postoperative human CSF Aβ40 levels following spinal (S), spinal plus desflurane (SD), and spinal plus isoflurane (SI) anesthesia are presented. A, The differences between the 2-h postoperative and preoperative baseline human CSF Aβ40 levels are not significantly different among the S, SD, or SI anesthesia group (F = 0.66, P = 0.52, N.S.). B, The differences between the 24-h postoperative and the preoperative baseline human CSF Aβ40 levels are signifi-cantly different among the S, SD, or SI anesthesia group (F = 4.25, * P = 0.02). Specifically, the difference between the 24-h postoperative and the preoperative baseline human CSF Aβ40 levels following SI anesthesia is positively greater than that following S anesthesia, F = 7.62, ** P = 0.006.
Given the findings that isoflurane increases Aβ levels in brain tissues of mice at 24, but not 6, h after the anesthesia,26 next, we investigated the effects of isoflurane and desflurane on CSF Aβ40 levels at a longer time (24 h) after the surgery under anesthesia. The mean of preoperative baseline and the 24-h postoperative CSF Aβ40 levels in the S, SD, and SI anesthesia groups were 11.59 ± 2.73 and 11.77 ± 2.81, 12.35 ± 2.86 and 11.81 ± 2.78, and 10.90 ± 2.56 and 12.41 ± 2.82 ng/ml, respectively (fig. 1B). Two-way repeated measures ANOVA showed that there was a statistically significant difference in CSF Aβ40 levels among S, SD, and SI at 24 h after the surgery under anesthesia (F = 4.25, * P = 0.02). Post hoc Bonferroni test showed that the difference between the 24-h postoperative and the preoperative baseline CSF Aβ40 levels following SI anesthesia (1.51 ± 2.76 ng/ml) was higher than that following S anesthesia (0.18 ± 1.89 ng/ml) (fig. 1B) (F = 7.62, ** P = 0.006). In contrast, post hoc Bonferroni test showed that the difference in CSF Aβ40 levels following SD anesthesia was not statistically different from that following S anesthesia (F = 0.34, P = 0.56, N.S.). Given that there was no significant difference in baseline CSF Aβ40 levels among S, SD, and SI groups, these results suggest that isoflurane (SI anesthesia), but not desflurane anesthesia (SD anesthesia), may be associated with increases in human CSF Aβ40 levels at 24 h after the surgery under anesthesia.
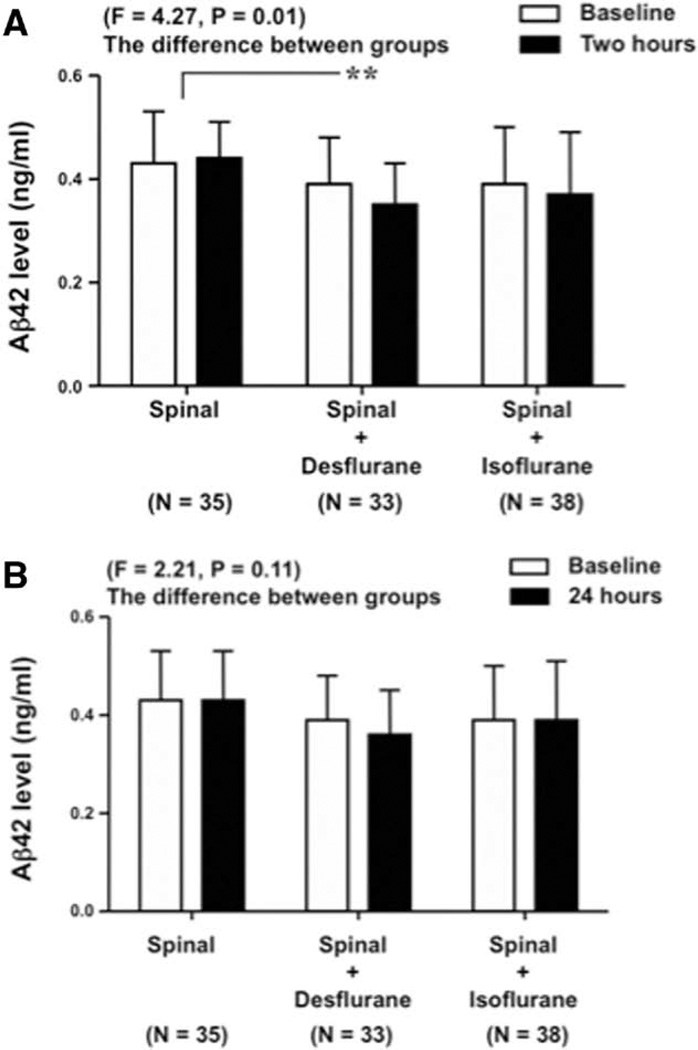
Next, we assessed the effects of S, SD, and SI anesthesia on CSF Aβ42 levels at 2 and 24 h after the surgery under anesthesia. The mean of preoperative baseline and the 2-h postoperative CSF Aβ42 levels in the S, SD, and SI anesthesia groups were 0.43 ± 0.10 and 0.44 ± 0.07, 0.39 ± 0.09 and 0.35 ± 0.08, and 0.39 ± 0.11 and 0.37 ± 0.12 ng/ml, respectively (fig. 2A). Two-way repeated measures ANOVA showed that there was a statistically significant difference in CSF Aβ42 levels among S, SD, and SI groups at 2 h after the surgery under anesthesia (F = 4.27, * P = 0.01). Post hoc Bonferroni test showed that the difference between the 2-h postoperative and the preoperative baseline CSF Aβ42 levels following SD anesthesia (−0.04 ± 0.05 ng/ml) was lower than that following S anesthesia (0.01 ± 0.07 ng/ml) (fig. 2A) (F = 8.41, ** P = 0.004). In contrast, post hoc Bonferroni test showed that the difference in CSF Aβ42 levels following SI anesthesia was not statistically different from that following S anesthesia (fig. 2A) (F = 3.17, P = 0.08, N.S.). Given that there was no significant difference in baseline CSF Aβ42 levels among S, SD, and SI groups, these results suggest that isoflurane (SI anesthesia) may not significantly alter CSF Aβ42 levels at 2 h after the surgery under anesthesia. Interestingly, desflurane (SD anesthesia) may be associated with decreases in the CSF Aβ42 levels at 2 h after the surgery under anesthesia.
Fig. 2.
Surgery under desflurane anesthesia is associated with decreases in human cerebrospinal fluid (CSF) β-amyloid protein (Aβ)42 levels 2 h after the anesthesia. The preop-erative baseline, the 2- and 24-h postoperative human CSF Aβ42 levels following spinal (S), spinal plus desflurane (SD), and spinal plus isoflurane (SI) anesthesia are presented. A, The differences between the 2-h postoperative and the preoperative baseline human CSF Aβ42 levels are significantly different among the S, SD, or SI anesthesia group (F = 4.27, P = 0.01). Specifically, the difference between the 2-h postoperative and the preoperative baseline human CSF Aβ42 levels following SD anesthesia is negatively greater than that following S anesthesia (F = 8.41, ** P = 0.004). B, The differences between the 24-h postoperative and the preoperative baseline human CSF Aβ42 levels are not significantly different among the S, SD, or SI anesthesia group (F = 2.21, P = 0.11).
Finally, we found that neither desflurane nor isoflurane significantly altered the CSF Aβ42 levels 24 h after the surgery under anesthesia: F = 2.21, P = 0.11, N.S. (fig. 2B). The mean of preoperative baseline and the 24-h postoperative CSF Aβ42 levels in the S, SD, and SI anesthesia groups were 0.43 ± 0.10 and 0.43 ± 0.10, 0.39 ± 0.09 and 0.36 ± 0.09, and 0.39 ± 0.11 and 0.39 ± 0.12 ng/ml, respectively (fig. 2B). These findings suggest that isoflurane, but not desflurane, may be associated with an increase in human CSF Aβ levels at a longer, but not shorter, time after the surgery under anesthesia, which is consistent with the results from the animal studies that isoflurane increases Aβ levels in mouse brain tissue at 24, but not 6 or 12, h after the anesthesia.26
Given that tau also plays roles in AD neuropathogenesis and that the ratio of Aβ42 to tau in CSF has been suggested as a biomarker of AD,21,23 we also assessed the effects of S, SD, and SI anesthesia on the levels of total tau, the ratio of Aβ40 or Aβ42 to tau in human CSF. The preoperative baseline tau levels among the S, SD, and SI anesthesia groups were not significantly different (F = 1.67, P = 0.19, table 3). We then found that SD and SI anesthesia did not increase the levels of total tau in human CSF compared to S anesthesia at 2 (F = 0.58, P = 0.56, N.S.) or 24 h (F = 1.03, P = 0.36, N.S.) after the surgery under anesthesia (table 3).
Table 3.
Neither Ioflurane nor Desflurane Affects Human CSF Tau Levels at 2 or 24 Hours after the Anesthesia
| S (N = 35) | SD (N = 33) | SI (N = 38) | F Values | P Values | |
|---|---|---|---|---|---|
| Tau (ng/ml)—baseline | 0.48 ± 0.13 | 0.49 ± 0.17 | 0.43 ± 0.12 | 1.67 | 0.19 |
| Tau (ng/ml) —2 h | 0.45 ± 0.17 | 0.48 ± 0.17 | 0.41 ± 0.13 | 0.58 | 0.56 |
| Tau (ng/ml) —24 h | 0.51 ± 0.15 | 0.49 ± 0.18 | 0.44 ± 0.12 | 1.03 | 0.36 |
The baseline tau protein levels in CSF are not signifcantly different among the surgery under S (N = 35), SD (N = 33), and SI (N = 38) anesthesia groups. The differences between the 2- or 24-h postoperative and the preoperative baseline human CSF tau levels are not significantly different among the S, SD, or SI anesthesia groups.
CSF = cerebrospinal fluid; S = spinal; SD = spinal plus desflurane; SI = spinal plus isoflurane.
One two-way repeated measures ANOVA showed that there was no statistically significant difference in the ratio of Aβ40 to tau among S, SD, and SI at 2 (F = 3.48, P = 0.04, N.S.) or 24 h (F = 2.43, P = 0.09, N.S.) after the anesthesia (table 4). However, the one two-way repeated measures ANOVA illustrated that there was a statistically significant difference in the ratio of Aβ42 to tau among S, SD, and SI groups at 2 h after the surgery under anesthesia, F = 6.83, ** P = 0.001 (table 5). Post hoc Bonferroni test suggested that the Aβ42 to tau ratio following SD was lower than that following S: 0.84 ± 0.37 versus 1.10 ± 0.41, F = 13.28, ** P = 0.0003, at 2 h after the surgery under anesthesia.
Table 4.
Neither Desflurane nor Isoflurane Alters Aβ40 to Tau Ratio in Human CSF at 2 Hours after the Anesthesia
| S (N = 35) | SD (N = 33) | SI (N = 38) | F Values | P Values | |
|---|---|---|---|---|---|
| Aβ40/Tau—2 h | 27.45 ± 9.94 | 25.88 ± 9.63 | 27.10 ± 11.14 | 3.48 | 0.04 |
| Aβ40/Tau—24 h | 24.75 ± 8.53 | 29.07 ± 9.87 | 30.11 ± 10.25 | 2.43 | 0.09 |
The Aβ40 to tau ratio in human CSF is not significantly different among the surgery under S (N = 35), SD (N = 33), and SI (N = 38) anesthesia groups at 2 or 24 h after the surgery under anesthesia.
Aβ = β-amyloid protein; CSF = cerebrospinal fluid; S = spinal; SD = spinal plus desflurane; SI = spinal plus isoflurane.
Table 5.
Desflurane, but Not Isoflurane, Reduces Human CSF Aβ42 to Tau Ratio at 2, but Not 24, Hours after the Anesthesia
| S (N = 35) | SD (N = 33) | SI (N = 38) | F Values | P Values | |
|---|---|---|---|---|---|
| Aβ42/Tau—2 h | 1.10 ± 0.41 | 0.83 ± 0.33** | 1.02 ± 0.52 | 6.83 | 0.001 |
| Aβ42/Tau—24 h | 0.91 ± 0.36 | 0.84 ± 0.37 | 0.97 ± 0.46 | 0.13 | 0.88 |
The Aβ42 to tau ratio in human CSF is lower following the surgery under SD (N = 33), but not SI (N = 38), compared to S (N = 35) anesthesia group at 2, but not 24, h after the surgery under anesthesia, F = 13.28,
P = 0.0003.
Aβ = β-amyloid protein; CSF = cerebrospinal fluid; S = spinal; SD = spinal plus desflurane; SI = spinal plus isoflurane.
Finally, one two-way repeated measures ANOVA showed that there was no statistically significant difference in the ratio of Aβ42 to tau among S, SD, and SI groups at 24 h after the surgery under anesthesia, F = 0.13, P = 0.88, N.S. (table 5).
Discussion
We have found that isoflurane (SI anesthesia) might be associated with higher levels of human CSF Aβ40 levels at 24 h after the surgery under anesthesia. Isoflurane may increase neither CSF Aβ40 levels at 2 h after the surgery under anesthesia nor CSF Aβ42 levels at 2 or 24 h after the surgery under anesthesia. These findings are consistent with the in vitro and animal studies that isoflurane can increase Aβ levels,25,26 and particularly the findings that isoflurane increases Aβ levels in mouse brain tissue at 24, but not 6 or 12, h after anesthesia.26
In contrast to isoflurane, desflurane (SD anesthesia) may not be associated with increases in CSF Aβ40 or Aβ42 levels. Rather, desflurane is associated with a decrease in CSF Aβ42 levels at 2 h after the surgery under anesthesia. These results are consistent with the findings that desflurane does not increase Aβ levels in vitro.31
Given that it is difficult to directly measure human brain Aβ levels following surgery under anesthesia, we used the human CSF Aβ levels as an alternative approach. The findings that isoflurane anesthesia may be associated with an increase in CSF Aβ levels suggest that isoflurane may increase brain Aβ levels. Many studies have suggested that low CSF Aβ level, at nonintervention status, represents high brain Aβ amounts, owing to the sequestration of Aβ into brain amyloid plaques,33 and is a biomarker for AD and AD progress.23,24 However, the CSF Aβ levels in the current studies represent acute changes following the intervention of surgery under anesthesia. Therefore, it could be postulated that isoflurane may increase human brain Aβ levels at 24 h following the surgery under anesthesia, which likely leak into the CSF, leading to the elevation of human CSF Aβ levels.
We did not observe that isoflurane increased the levels of total tau protein in human CSF in the current studies. These findings are consistent with the observations that isoflurane does not increase the total tau levels.30,34 However, a recent study has illustrated that the intravenous anesthetic propofol35 and isoflurane30 can induce tau phosphorylation in brain tissues of mice. Future human relevance studies may include assessing the effects of propofol anesthesia and isoflurane anesthesia on the levels of phosphorylated tau in human CSF.
Previous animal studies showed that isoflurane induced caspase-3 activation and increased levels of β-site amyloid precursor protein–cleaving enzyme (BACE, the enzyme for the generation of Aβ) at 6 h after the anesthesia, but enhanced Aβ levels at 24, but not 6 or 12, h after the anesthesia in the brain tissues of mice.26 These results suggest that isoflurane may induce caspase activation and apoptosis, which in turn increase BACE activity, leading to Aβ generation in a time-dependent manner. This hypothesis is further supported by the in vitro mechanistic studies that isoflurane may induce a cycle of caspase activation/apoptosis and increases in BACE levels and Aβ generation.36 The findings from the current human studies that isoflurane might increase Aβ levels at longer, but not shorter, time after the surgery under anesthesia also suggest that isoflurane may induce a time-dependent increase in Aβ levels potentially via this caspase/ apoptosis–BACE–Aβ cascade.
Alternatively, isoflurane may increase the Aβ levels via noncaspase/apoptosis–BACE–Aβ cascade. Wan et al.37 showed that surgery under anesthesia might induce neuroinflammation, leading to Aβ accumulation in brain tissues of mice. Isoflurane has been shown to increase the levels of proinflammatory cytokines in mouse brain tissues.38 We therefore postulate that isoflurane increases Aβ levels through the isoflurane-induced neuroinflammation and we will test this hypothesis in the future studies.
Interestingly, we found that desflurane might decrease the Aβ42 levels in human CSF 2 h after the surgery under SD anesthesia (fig. 2A). Furthermore, at 2 h after the surgery under anesthesia, both isoflurane (SI) and desflurane (SD) seem to decrease Aβ40 and Aβ42 levels, even though some of the decreases did not reach statistically significant levels (figs. 1A and 2A). The underlying mechanisms of these findings remain to be determined. It has been shown that reduction in brain synaptic activity39,40 and brain function41 leads to decreases in Aβ levels. The findings that human CSF Aβ levels decrease at 2, but not at 24, h following the surgery under isoflurane or desflurane anesthesia suggest that the anesthesia-induced reduction in brain function, as evidenced by the reduction in the bispectral index value, may lead to the decreases in the Aβ levels. Future research should include time course studies of the effects of isoflurane, desflurane, and other anesthetics (e.g., intravenous anesthetic propofol) on human CSF Aβ levels to further test this hypothesis. We may determine the CSF Aβ levels every hour between 2 and 24 h postoperatively.
It is interesting that isoflurane only increased the levels of Aβ40, but not Aβ42, in the human CSF in the current experiments. Although Aβ42 seems more pathogenic than Aβ40,42 several studies have shown that Aβ40 is neurotoxic and can induce caspase activation and apoptosis.16–18 In addition, Aβ40 has been shown to induce impairment of synaptic plasticity and memory function.19,20 Finally, increased Aβ40 levels in animal brains can occur after stroke and brain ischemia43 and following energy inhibition.44 Thus, the acute increase in Aβ40 may also cause neurotoxicity, impair synapse function, and induce learning and memory impairment.
In the present pilot studies, we have established a system to determine the effects of anesthesia on Aβ and tau levels in human CSF and have demonstrated the in vivo relevance in humans of our in vitro and animal findings that isoflurane, but not desflurane, may increase Aβ levels. These results suggest that isoflurane and desflurane may affect human CSF Aβ levels differently. Specifically, isoflurane may increase human CSF Aβ40 levels at 24 h after the surgery under anesthesia, and desflurane may decrease Aβ42 levels at 2 h after the surgery under anesthesia. These findings could have a significant impact on clinical practice of anesthesia and suggest that further studies to determine the effects of anesthesia on AD biomarkers are warranted.
There are two pioneer studies in investigating the effects of anesthesia and surgery on human CSF biomarkers associated with AD. Palotas et al.45 determined the effects of coronary artery bypass under general anesthesia on human CSF level of Aβ42, Tau, and S100β and found that Aβ42, Tau, and S100β significantly increased at 1 week after the surgery. However, 6 months after the surgery, the Aβ42 levels in the human CSF significantly decreased although the human CSF levels of tau and S100β still increased.45 In another study, Tang et al.46 found that the idiopathic nasal CSF leak correction under anesthesia with propofol, remifentanil, or sevoflurane increased the human CSF levels of tau and proinflammatory cytokines, but not Aβ42, 48 h after the surgery. Our current human studies are different from these two studies in postoperative time intervals (2 and 24 h vs. 48 h, 1 week, and 6 months), anesthesia (isoflurane or desflurane vs. propofol, remifentanil, or sevoflurane), surgery (orthopedic or abdominal surgery vs. coronary artery bypass or idiopathic nasal CSF leak correction), and measurement (Aβ40 vs. Aβ42). Future studies to determine whether different anesthesia, surgery, and postoperative time intervals may have different effects on specific human CSF biomarkers associated with AD are warranted.
There are several caveats in the current studies. First, we did not plan to perform the interim analysis before the proposed studies. We recruited a second set of subjects when we realized that we could have type 1 error in the analysis of the data from the original set of subjects. To control the overall type 1 error rate to no more than 0.05, we chose to use P < 0.025 as the criterion for statistical significance for each analysis of the data obtained from the combination of both the original and the second set of participants. Second, the effects of isoflurane on the elevation of human CSF Aβ levels are moderate (smaller than diurnal variation of human CSF Aβ levels); therefore, it is uncertain that the isofluraneor desflurane-induced changes in brain or CSF Aβ levels account for the isoflurane- or desflurane-induced changes in cognitive function. Future studies will determine the potential association between the isoflurane-induced changes in cognitive function and in brain, CSF, or plasma Aβ levels, which may illustrate the role of anesthetic isoflurane in the neuropathogenesis of AD, as well as in the decline of postoperative cognitive function.
In conclusion, our studies have established a system to investigate the effects of anesthesia on human biomarkers associated with AD and cognitive dysfunction. The findings from these studies have suggested that surgery under isoflurane anesthesia may be associated with increases, but surgery under desflurane anesthesia may be associated with decreases in human CSF Aβ levels. These results will promote more human biomarker studies to either rule in or rule out the role of anesthesia in the neuropathogenesis of AD and postoperative cognitive dysfunction.
What We Already Know about This Topic
Isoflurane, but not desflurane, increases β-amyloid proteins (Aβ) in animals, and this may participate in postoperative cognitive effects of anesthesia in humans
What This Article Tells Us That Is New
In 106 patients randomized to receive spinal anesthesia for surgery without general anesthetics or with isoflurane or desflurane, isoflurane was associated with an increase in cerebrospinal fuid concentrations of Aβ40 and desflurane with a decrease in Aβ42
This clinical work parallels observations in animals, but its relevance to cognition after surgery remains uncertain
Acknowledgments
This research was supported by Beijing science and technology development plan of the education committee, Keji Mian (KM) 200910025016 (Beijing, P.R. China) (to Ming Tian), National Science Foundation of China Oversea young scholar collaboration research award, National Science Foundation of China (NSFC) 30928026 (Beijing, P. R. China) (to Zhongcong Xie and Yun Yue), R21AG029856, R21AG038994, and R01 GM088801 from the National Institutes of Health, Bethesda, Maryland; from Cure Alzheimer’s Fund, Wellesley, Massachusetts (to Zhongcong Xie), and a Mid-Career Investigator Award (K24AG035075) from the National Institutes of Health, Bethesda, Maryland (to Edward R. Marcantonio).
Footnotes
Part of this work was presented at the annual meeting of the American Society of Anesthesiologists, on October 16, 2010, in San Diego, California.
References
- 1.Bohnen NI, Warner MA, Kokmen E, Beard CM, Kurland LT. Alzheimer’s disease and cumulative exposure to anesthesia: A case-control study. J Am Geriatr Soc. 1994;42:198–201. doi: 10.1111/j.1532-5415.1994.tb04952.x. [DOI] [PubMed] [Google Scholar]
- 2.Bohnen N, Warner MA, Kokmen E, Kurland LT. Early and midlife exposure to anesthesia and age of onset of Alzheimer’s disease. Int J Neurosci. 1994;77:181–185. doi: 10.3109/00207459408986029. [DOI] [PubMed] [Google Scholar]
- 3.Lee TA, Wolozin B, Weiss KB, Bednar MM. Assessment of the emergence of Alzheimer’s disease following coronary artery bypass graft surgery or percutaneous transluminal coronary angioplasty. J Alzheimers Dis. 2005;7:319–324. doi: 10.3233/jad-2005-7408. [DOI] [PubMed] [Google Scholar]
- 4.Bufill E, Bartés A, Moral A, Casadevall T, Codinachs M, Zapater E, Carles Rovira J, Roura P, Oliva R, Blesa R. [Genetic and environmental factors that may influence in the senile form of Alzheimer’s disease: Nested case control studies] Neurologia. 2009;24:108–112. [PubMed] [Google Scholar]
- 5.Knopman DS, Petersen RC, Cha RH, Edland SD, Rocca WA. Coronary artery bypass grafting is not a risk factor for dementia or Alzheimer disease. Neurology. 2005;65:986–990. doi: 10.1212/01.wnl.0000171954.92119.c7. [DOI] [PubMed] [Google Scholar]
- 6.Gasparini M, Vanacore N, Schiaffini C, Brusa L, Panella M, Talarico G, Bruno G, Meco G, Lenzi GL. A case-control study on Alzheimer’s disease and exposure to anesthesia. Neurol Sci. 2002;23:11–14. doi: 10.1007/s100720200017. [DOI] [PubMed] [Google Scholar]
- 7.Avidan MS, Searleman AC, Storandt M, Barnett K, Vannucci A, Saager L, Xiong C, Grant EA, Kaiser D, Morris JC, Evers AS. Long-term cognitive decline in older subjects was not attributable to noncardiac surgery or major illness. ANESTHESIOLOGY. 2009;111:964–970. doi: 10.1097/ALN.0b013e3181bc9719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris RA, Eger EI., 2nd Alzheimer’s disease and anesthesia: Out of body, out of mind.or not? Ann Neurol. 2008;64:595–597. doi: 10.1002/ana.21575. [DOI] [PubMed] [Google Scholar]
- 9.Bittner EA, Yue Y, Xie Z. Brief review: Anesthetic neurotoxicity in the elderly, cognitive dysfunction and Alzheimer’s disease. Can J Anaesth. 2011;58:216–223. doi: 10.1007/s12630-010-9418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bertram L, Lill CM, Tanzi RE. The genetics of Alzheimer disease: Back to the future. Neuron. 2010;68:270–281. doi: 10.1016/j.neuron.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Tanzi RE, Bertram L. Twenty years of the Alzheimer’s disease amyloid hypothesis: A genetic perspective. Cell. 2005;120:545–555. doi: 10.1016/j.cell.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Selkoe DJ. Alzheimer’s disease: Genes, proteins, and therapy. Physiol Rev. 2001;81:741–766. doi: 10.1152/physrev.2001.81.2.741. [DOI] [PubMed] [Google Scholar]
- 13.Xie Z, Tanzi RE. Alzheimer’s disease and post-operative cognitive dysfunction. Exp Gerontol. 2006;41:346–359. doi: 10.1016/j.exger.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 14.Gao CM, Yam AY, Wang X, Magdangal E, Salisbury C, Peretz D, Zuckermann RN, Connolly MD, Hansson O, Minthon L, Zetterberg H, Blennow K, Fedynyshyn JP, Allauzen S. Aβ40 oligomers identified as a potential biomarker for the diagnosis of Alzheimer’s disease. PLoS ONE. 2010;5:e15725. doi: 10.1371/journal.pone.0015725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mawuenyega KG, Sigurdson W, Ovod V, Munsell L, Kasten T, Morris JC, Yarasheski KE, Bateman RJ. Decreased clearance of CNS beta-amyloid in Alzheimer’s disease. Science. 2010;330:1774. doi: 10.1126/science.1197623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang CA, Chen YH, Ke SC, Chen YR, Huang HB, Lin TH, Chen YC. Correlation of copper interaction, copper-driven aggregation, and copper-driven h(2)o(2) formation with aβ40 conformation. Int J Alzheimers Dis. 2010;2011:607861. doi: 10.4061/2011/607861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakagawa T, Zhu H, Morishima N, Li E, Xu J, Yankner BA, Yuan J. Caspase-12 mediates endoplasmic-reticulum-specific apoptosis and cytotoxicity by amyloid-beta. Nature. 2000;403:98–103. doi: 10.1038/47513. [DOI] [PubMed] [Google Scholar]
- 18.Awasthi A, Matsunaga Y, Yamada T. Amyloid-beta causes apoptosis of neuronal cells via caspase cascade, which can be prevented by amyloid-beta-derived short peptides. Exp Neurol. 2005;196:282–289. doi: 10.1016/j.expneurol.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 19.Walsh DM, Klyubin I, Fadeeva JV, Cullen WK, Anwyl R, Wolfe MS, Rowan MJ, Selkoe DJ. Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo . Nature. 2002;416:535–539. doi: 10.1038/416535a. [DOI] [PubMed] [Google Scholar]
- 20.Shankar GM, Li S, Mehta TH, Garcia-Munoz A, Shepardson NE, Smith I, Brett FM, Farrell MA, Rowan MJ, Lemere CA, Regan CM, Walsh DM, Sabatini BL, Selkoe DJ. Amyloid-beta protein dimers isolated directly from Alzheimer’s brains impair synaptic plasticity and memory. Nat Med. 2008;14:837–842. doi: 10.1038/nm1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Small SA, Duff K. Linking Abeta and tau in late-onset Alzheimer’s disease: A dual pathway hypothesis. Neuron. 2008;60:534–542. doi: 10.1016/j.neuron.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blennow K, Vanmechelen E, Hampel H. CSF total tau, Abeta42 and phosphorylated tau protein as biomarkers for Alzheimer’s disease. Mol Neurobiol. 2001;24:87–97. doi: 10.1385/MN:24:1-3:087. [DOI] [PubMed] [Google Scholar]
- 23.Tarawneh R, Holtzman DM. Biomarkers in translational research of Alzheimer’s disease. Neuropharmacology. 2010;59:310–322. doi: 10.1016/j.neuropharm.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shaw LM, Vanderstichele H, Knapik-Czajka M, Clark CM, Aisen PS, Petersen RC, Blennow K, Soares H, Simon A, Lewczuk P, Dean R, Siemers E, Potter W, Lee VM, Trojanowski JQ. Alzheimer’s Disease Neuroimaging Initiative: Cerebrospinal fluid biomarker signature in Alzheimer’s disease neuroimaging initiative subjects. Ann Neurol. 2009;65:403–413. doi: 10.1002/ana.21610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xie Z, Dong Y, Maeda U, Alfille P, Culley DJ, Crosby G, Tanzi RE. The common inhalation anesthetic isoflurane induces apoptosis and increases amyloid beta protein levels. ANESTHESIOLOGY. 2006;104:988–994. doi: 10.1097/00000542-200605000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Xie Z, Culley DJ, Dong Y, Zhang G, Zhang B, Moir RD, Frosch MP, Crosby G, Tanzi RE. The common inhalation anesthetic isoflurane induces caspase activation and increases amyloid beta-protein level in vivo . Ann Neurol. 2008;64:618–627. doi: 10.1002/ana.21548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y, Dong Y, Wu X, Lu Y, Xu Z, Knapp A, Yue Y, Xu T, Xie Z. The mitochondrial pathway of anesthetic isoflurane-induced apoptosis. J Biol Chem. 2010;285:4025–4037. doi: 10.1074/jbc.M109.065664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bianchi SL, Tran T, Liu C, Lin S, Li Y, Keller JM, Eckenhoff RG, Eckenhoff MF. Brain and behavior changes in 12-month-old Tg2576 and nontransgenic mice exposed to anesthetics. Neurobiol Aging. 2008;29:1002–1010. doi: 10.1016/j.neurobiolaging.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tang J, Eckenhoff MF, Eckenhoff RG. Anesthesia and the old brain. Anesth Analg. 2010;110:421–426. doi: 10.1213/ANE.0b013e3181b80939. [DOI] [PubMed] [Google Scholar]
- 30.Dong Y, Wu X, Xu Z, Zhang Y, Xie Z. Anesthetic isoflurane increases phosphorylated tau levels mediated by caspase activation and Aβ generation. PLoS ONE. 2012;7:e39386. doi: 10.1371/journal.pone.0039386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang B, Dong Y, Zhang G, Moir RD, Xia W, Yue Y, Tian M, Culley DJ, Crosby G, Tanzi RE, Xie Z. The inhalation anesthetic desflurane induces caspase activation and increases amyloid beta-protein levels under hypoxic conditions. J Biol Chem. 2008;283:11866–11875. doi: 10.1074/jbc.M800199200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bateman RJ, Wen G, Morris JC, Holtzman DM. Fluctuations of CSF amyloid-beta levels: Implications for a diagnostic and therapeutic biomarker. Neurology. 2007;68:666–669. doi: 10.1212/01.wnl.0000256043.50901.e3. [DOI] [PubMed] [Google Scholar]
- 33.Blennow K, Zetterberg H. Cerebrospinal fuid biomarkers for Alzheimer’s disease. J Alzheimers Dis. 2009;18:413–417. doi: 10.3233/JAD-2009-1177. [DOI] [PubMed] [Google Scholar]
- 34.Planel E, Bretteville A, Liu L, Virag L, Du AL, Yu WH, Dickson DW, Whittington RA, Duff KE. Acceleration and persistence of neurofibrillary pathology in a mouse model of tauopathy following anesthesia. FASEB J. 2009;23:2595–2604. doi: 10.1096/fj.08-122424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whittington RA, Virág L, Marcouiller F, Papon MA, El Khoury NB, Julien C, Morin F, Emala CW, Planel E. Propofol directly increases tau phosphorylation. PLoS ONE. 2011;6:e16648. doi: 10.1371/journal.pone.0016648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xie Z, Dong Y, Maeda U, Moir RD, Xia W, Culley DJ, Crosby G, Tanzi RE. The inhalation anesthetic isoflurane induces a vicious cycle of apoptosis and amyloid beta-protein accumulation. J Neurosci. 2007;27:1247–1254. doi: 10.1523/JNEUROSCI.5320-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wan Y, Xu J, Meng F, Bao Y, Ge Y, Lobo N, Vizcaychipi MP, Zhang D, Gentleman SM, Maze M, Ma D. Cognitive decline following major surgery is associated with gliosis, β-amyloid accumulation, and τ phosphorylation in old mice. Crit Care Med. 2010;38:2190–2198. doi: 10.1097/CCM.0b013e3181f17bcb. [DOI] [PubMed] [Google Scholar]
- 38.Wu X, Lu Y, Dong Y, Zhang G, Zhang Y, Xu Z, Culley DJ, Crosby G, Marcantonio ER, Tanzi RE, Xie Z. The inhalation anesthetic isoflurane increases levels of proinflammatory TNF-α, IL-6, and IL-1β. Neurobiol Aging. 2012;33:1364–1378. doi: 10.1016/j.neurobiolaging.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cirrito JR, Yamada KA, Finn MB, Sloviter RS, Bales KR, May PC, Schoepp DD, Paul SM, Mennerick S, Holtzman DM. Synaptic activity regulates interstitial fluid amyloid-beta levels in vivo . Neuron. 2005;48:913–922. doi: 10.1016/j.neuron.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 40.Cirrito JR, Kang JE, Lee J, Stewart FR, Verges DK, Silverio LM, Bu G, Mennerick S, Holtzman DM. Endocytosis is required for synaptic activity-dependent release of amyloid-beta in vivo . Neuron. 2008;58:42–51. doi: 10.1016/j.neuron.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brody DL, Magnoni S, Schwetye KE, Spinner ML, Esparza TJ, Stocchetti N, Zipfel GJ, Holtzman DM. Amyloid-beta dynamics correlate with neurological status in the injured human brain. Science. 2008;321:1221–1224. doi: 10.1126/science.1161591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kuperstein I, Broersen K, Benilova I, Rozenski J, Jonckheere W, Debulpaep M, Vandersteen A, Segers-Nolten I, Van Der Werf K, Subramaniam V, Braeken D, Callewaert G, Bartic C, D’Hooge R, Martins IC, Rousseau F, Schymkowitz J, De Strooper B. Neurotoxicity of Alzheimer’s disease Aβ peptides is induced by small changes in the Aβ42 to Aβ40 ratio. EMBO J. 2010;29:3408–3420. doi: 10.1038/emboj.2010.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van Groen T, Puurunen K, Mäki HM, Sivenius J, Jolkkonen J. Transformation of diffuse beta-amyloid precursor protein and beta-amyloid deposits to plaques in the thalamus after transient occlusion of the middle cerebral artery in rats. Stroke. 2005;36:1551–1556. doi: 10.1161/01.STR.0000169933.88903.cf. [DOI] [PubMed] [Google Scholar]
- 44.Velliquette RA, O’Connor T, Vassar R. Energy inhibition elevates beta-secretase levels and activity and is potentially amy-loidogenic in APP transgenic mice: Possible early events in Alzheimer’s disease pathogenesis. J Neurosci. 2005;25:10874–10883. doi: 10.1523/JNEUROSCI.2350-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Palotás A, Reis HJ, Bogáts G, Babik B, Racsmány M, Engvau L, Kecskeméti E, Juhász A, Vieira LB, Teixeira AL, Mukhamedyarovi MA, Rizvanov AA, Yalvaç ME, Guimarães MM, Ferreira CN, Zefrov AL, Kiyasov AP, Wang L, Janka Z, Kálmán J. Coronary artery bypass surgery provokes Alzheimer’s disease-like changes in the cerebrospinal fluid. J Alzheimers Dis. 2010;21:1153–1164. doi: 10.3233/jad-2010-100702. [DOI] [PubMed] [Google Scholar]
- 46.Tang JX, Baranov D, Hammond M, Shaw LM, Eckenhoff MF, Eckenhoff RG. Human Alzheimer and inflammation biomarkers after anesthesia and surgery. ANESTHESIOLOGY. 2011;115:727–732. doi: 10.1097/ALN.0b013e31822e9306. [DOI] [PMC free article] [PubMed] [Google Scholar]