Abstract
Background
The number of hospitals offering invasive cardiac services (diagnostic angiography, percutaneous coronary intervention [PCI], and coronary artery bypass grafting [CABG]) has expanded, yet national patterns of service diffusion and their effect on geographic access to care are unknown.
Methods and Results
Retrospective cohort study of all hospitals in fee-for-service Medicare, 1996–2008. Logistic regression identified the relationship between cardiac service adoption and the proportion of neighboring hospitals within 40 miles already offering the service. From 1996–2008, 397 hospitals began offering diagnostic angiography, 387 PCI, and 298 CABG (increasing the proportion with services by 3%, 11%, and 4% respectively). This capacity increase led to little new geographic access to care; the population increase in geographic access to diagnostic angiography was 1 percentage point; PCI 5 percentage points, and CABG 4 percentage points. Controlling for hospital and market characteristics, a 10 percentage point increase in the proportion of nearby hospitals already offering the service increased the odds by 10% that a hospital would add diagnostic angiography (OR: 1.102; 95% CI: 1.018, 1.193), increased the odds by 79% that it would add PCI (OR: 1.794, 95% CI: 1.288, 2.498), and had no significant effect on adding CABG (OR 0.929, 95% CI, 0.608, 1.420).
Conclusions
Hospitals are most likely to introduce new invasive cardiac services when neighboring hospitals already offer such services. Increases in the number of hospitals offering invasive cardiac services have not led to corresponding increases in geographic access.
Keywords: access, diffusion of innovation, PCI, geographic variation
INTRODUCTION
Invasive cardiac services, including diagnostic angiography, percutaneous coronary interventions (PCI), and coronary-artery bypass grafting (CABG) are among the most common procedures performed in the United States.1 Yet, because individual facilities may profitably perform them once adopted, many hospitals make substantial investments in invasive cardiac treatments despite the possibility that the new capacity will be used in marginal populations and may contribute to growth in medical spending.2 Consequently, numerous payers, including the Centers for Medicare and Medicaid Services (CMS), have attempted to control invasive cardiac treatment costs while maintaining access to care.
Although previous research has shown a rapid growth of cardiac surgical services,3 it is unclear how and where the diffusion of invasive cardiac services is occurring in the U.S. On the one hand, adding new services to underserved areas may well benefit cardiac patients, particularly if the new facilities make patients more likely to get superior treatment.4 Alternatively, hospitals may adopt new cardiac services for competitive reasons – for example, because these services are profitable because they are well reimbursed, attract patients, or attract doctors -- although expansions may be in areas where services are already widely available. This would contribute to decreased local expertise from lower volume within a market, increased variation in treatment and outcomes(5,6) or possible overuse without clear medical indication. Prior studies on the cardiac technology diffusion have been limited either geographically7 or to a single service.8 Thus we currently do not know to what extent the number of hospitals offering diagnostic and therapeutic invasive cardiac services has grown (and the interrelationship of those twin services), and whether that growth has reduced the number of patients without geographic access to care. Accordingly, we examined the adoption patterns for three cardiovascular interventions—diagnostic angiography, PCI, and CABG—over 13 years. We determined: 1) the number of hospitals offering new services, 2) whether a hospital’s new service offering depends on the service mix at neighboring hospitals, and 3) the effect of new adoption on geographic access to care.
METHODS
STUDY DESIGN
Consistent with previous research,9 we identified hospitals in the Medicare Provider Analysis and Review (MedPAR) files (1996–2008) that billed CMS for at least five procedures (diagnostic angiography, PCI, or CABG) annually to patients with documented acute myocardial infarction. Our sample included all general medical and surgical hospitals in the continental U.S. listed in the American Hospital Association (AHA) files, excluding hospitals that serve restricted populations such as Veterans and single-service hospitals that were unlikely to compete with nearby hospitals for patients. We matched the AHA and MedPAR files using: 1) provider numbers listed in the AHA, 2) independent data-crosswalks, and 3) geographic coordinates determined by geocoding hospitals in the datasets. Our final sample accounted for 96 percent of relevant admissions in the AHA and 98 percent of relevant beds in the MedPAR data, leaving only 421 unmatched, individual hospitals in the AHA. For sensitivity testing we used ArcMap 10.0 to determine the driving distance from every hospital to the centroid of every Census tract that could be reached within sixty minutes.
STATISTICAL ANALYSIS
Diffusion of Services
We first identified hospitals offering: 1) no invasive cardiac services, 2) diagnostic angiography only, 3) diagnostic angiography and PCI, or 4) diagnostic angiography, PCI, and CABG.
Geographic Clustering Analysis
We used logistic-regression models to determine whether the probability that a hospital first adopted a new service depended on the proportion of neighboring hospitals already offering that service. Our analysis was based on discrete-time hazard models such that hospitals that have made the transition, e.g., from not offering PCI to offering PCI were removed from the risk pool in subsequent years. In such a discrete-time hazard model -- a logistic regression with a binary outcomes such as ours – 1) all hospitals at risk of making a transition in a year, including those who have not yet made the transition and those who already did were included, and 2) all hospitals that have made the transition in a prior year were removed from the regression because they were not at risk.
We accounted for different levels of patient demand by including independent variables based on the U.S. Census (1990, 2000) and the American Community Survey measuring the proportion of the population who were in the labor force, unemployed, college graduates, Caucasian (non- Hispanic), or poor. We defined the market as the census tracts with centroids within 40 miles of each hospital, based on boundaries from the 2000 U.S. Census. Although medical guidelines regarding recommended time to treatment vary, an average of 40 miles is a reasonable approximation of the market for emergent invasive cardiac treatment based on the recommended maximum one-hour travel time.10 We also accounted for hospital characteristics that may have influenced a hospital to offer a new service, including measures of hospital size, membership in a hospital system, teaching status, and ownership (nonprofit, for-profit, or government). In sensitivity testing, we controlled for Certificate of Need (CON) laws governing cardiac services to measure state regulatory regimes.
The key independent variable measured the proportion of nearby hospitals previously offering each service. As we hoped to investigate the probability of new entrants into a service line, we tried to identify the region from which potential patients might reasonably come to the hospital, not those who actually use the hospital. For this purpose, we looked at all hospitals within 40 miles of the observation hospital. In sensitivity testing, we applied alternative definitions of “nearby” such as considering all hospitals as possible competitors, while weighting closer hospitals more than distant hospitals.11 We focus on proportion of nearby hospitals offering a service rather than the absolute number of nearby hospitals doing so because the proportion of competitors offering a service takes into account the size and concentration of the market and, therefore, better represents the effect of any single hospital’s decision on another hospital in the market than does the absolute number.
We report both odds ratios and, for ease of interpretation, percentage increases in the probability that new services locate near existing services. This conversion is straightforward because when the probability of an event happening is small, as in the case of a hospital adopting a new service, the odds ratio approximates the relative risk, interpretable as the percentage chance of an event happening.12 All regression analyses were performed with Stata statistical software, v.11.2. Tests were two-sided, and p-values less than 0.05 indicated statistical significance.
Alternative Technology Diffusion Models
In simulations, we alternately allocated diagnostic angiography, PCI, and CABG to the same number of hospitals that actually adopted them over the study period, but we allocated them using various counterfactual approaches. In all cases, we counted a person as having geographic access if they resided in a census tract whose centroid was within 40 miles of a service, and varied this measure in sensitivity testing (alternately using 20 and 40 mile distances as well as 60 minutes driving time determined from mapping software for all, urban, or rural hospitals). First, we allocated new services using a public health planning approach, one that allocated the same number of new services that were adopted during the study period to hospitals so as to maximize the population gaining new access to care within 40 miles.
Second, in an alternative allocation approach, we allocated those services to existing hospitals fully at random. In constructing the simulation, we designated all hospitals that did not previously offer the service as eligible to offer it. This modeling choice rests on a somewhat unrealistic assumption since some hospitals to which we allocated new services are ill-equipped to offer invasive cardiac services and would be unlikely to do so. However, the assumption that all hospitals that did not previously offer the service were eligible to offer it is the most conservative modeling assumption it assigns new services to hospitals that are located in relatively unpopulated areas and, therefore, adds few potential patients to our estimates of the number of people who would be newly served. We performed this random simulation 500 times and averaged the results.
In determining both the population newly served by the actual addition of services by hospitals and the population that would be served if the two simulation methods were adopted (optimal diffusion and random diffusion), we used a fixed distance (40 miles or, in sensitivity testing other mileage or a 60 minute drive) to count the number of people newly served. Since the areas around some hospitals overlap with the areas around other hospitals, the newly served populations are counted more than once, making numerical estimates of the number of new people served inaccurate. This is necessary, as an effort to apportion each person in the United States to one and only one hospital’s potential market would be both arbitrary and a poor representation of how patients actually choose hospitals. However, since the manner of over-counting is identical for both the actual and hypothetical exercises, the comparisons among exercises are valid. Moreover, if there is any bias present it would be towards undercounting the number of people newly served by random placement of services because we included all hospitals without services as eligible to offer them, including rural hospitals that serve areas with few potential patients and are far from other hospitals.
RESULTS
Trends in Invasive Cardiac Service Provision
The rate of new, cardiac service offerings by hospitals varied by the particular service. From 1996 through 2008, 8 percent of hospitals provided new diagnostic angiography, 7 percent PCI, and 6 percent CABG (Table 1).
Table 1.
Trends in Hospital Provision of Invasive Cardiac Services, 1996–2008.
| No. Hospitals Adding Service | No. of Hospitals with Services | |||||||
|---|---|---|---|---|---|---|---|---|
| Year | None | DxCath | PCI | CABG | None | DxCath | PCI & DxCath |
DxCath& PCI & CABG |
| 1996 | 5,037 | 0 | 0 | 0 | 3,195 | 885 | 49 | 908 |
| 1997 | 4,863 | 68 | 9 | 25 | 3,076 | 896 | 59 | 934 |
| 1998 | 4,857 | 39 | 14 | 26 | 3,050 | 866 | 70 | 950 |
| 1999 | 4,797 | 34 | 20 | 22 | 3,004 | 832 | 82 | 955 |
| 2000 | 4,773 | 30 | 27 | 18 | 2,989 | 793 | 105 | 961 |
| 2001 | 4,739 | 26 | 25 | 32 | 2,947 | 761 | 125 | 989 |
| 2002 | 4,725 | 38 | 21 | 33 | 2,938 | 730 | 131 | 1,018 |
| 2003 | 4,675 | 35 | 47 | 32 | 2,870 | 685 | 181 | 1,053 |
| 2004 | 4,662 | 32 | 44 | 21 | 2,834 | 645 | 228 | 1,052 |
| 2005 | 4,896 | 25 | 50 | 21 | 3,020 | 603 | 285 | 1,084 |
| 2006 | 4,869 | 34 | 52 | 29 | 3,011 | 558 | 312 | 1,103 |
| 2007 | 4,884 | 20 | 37 | 22 | 2,980 | 523 | 345 | 1,115 |
| 2008 | 4,890 | 16 | 38 | 17 | 3,000 | 480 | 365 | 1,116 |
| Total | 397 | 387 | 298 | |||||
Many hospitals progressed from offering diagnostic services to treatments, and fewer hospitals offered only diagnostic services in 2008 (9.7 percent) than they did in 1996 (17.6 percent). However, adopting diagnostic angiography was not merely a first stage towards treatment (i.e., PCI or CABG). On average over the study period, almost 15 percent of the hospitals in the sample provided only diagnostic services. Among urban hospitals, one in five acute-care hospitals offered only diagnostic care, although that number was falling (25% to 18% over the study period).
Neighbor Effects
Larger hospitals were more likely than smaller hospitals to add new capabilities. However, hospitals were more likely to adopt new services if a hospital within 40 miles already offered that service, even after controlling for hospital size, population size, other market characteristics, and the proportion of people who already lived within 40 miles of a service. (Table 2) Hospitals with similar numbers of potential patients available, whether those patients already had geographic access or not, were more likely to offer a new cardiac service if a neighboring hospital was already offering it.
Table 2.
Odds ratios for Hospitals Offering Invasive Cardiac Services According to Hospital and Population Characteristics, 1996–2008.
| Diagnostic Angiography |
PCI | CABG | |
|---|---|---|---|
| Nearby proportion of hospitals with Diagnostic Angiography, per 10% | 1.102* | 0.775 | 0.808 |
| 95% Confidence Interval | 1.018–1.193 | 0.581–1.034 | 0.597–1.094 |
| Nearby proportion of hospitals with PCI, per 10% | 1.059 | 1.794*** | 1.442 |
| 95% Confidence Interval | 0.910–1.233 | 1.288–2.498 | 0.926–2.245 |
| Nearby proportion with CABG, per 10% | 0.920 | 0.726** | 0.929@ |
| 95% Confidence Interval | 0.787–1.075 | 0.575–0.916 | 0.608–1.420 |
| Recently added Diagnostic Angiography | 9.290*** | 2.302 | |
| 95% Confidence Interval | 4.485–19.241 | 0.629–8.421 | |
| Observations | 31,920 | 32,935 | 33,193 |
| Number of hospitals | 3,156 | 3,156 | 3,221 |
NB: Robust standard errors clustered at the hospital level. The logistic regression model was also adjusted for: total nearby population as reported by the census (within 40 miles), nearby population not already covered in the previous year for each service; Certificate of Need regime at the state level; hospital characteristics (admissions quintiles, system membership, rural location, teaching status, ownership status – government, for-profit, or nonprofit); population characteristics (unemployment rate, labor force participation, education, poverty, race); and baseline hazard control (log of time at risk).
In some alternative specifications the coefficient of nearby population with CABG on CABG was positive indicated a positive relationship; however, the results were non-significant in all alternative specifications.
p < 0.05,
p < 0.01,
p < 0.001.
The results were largest for PCI, with hospitals considerably more likely to adopt new PCI technology when a higher proportion of neighboring hospitals offered PCI. A 10 percentage point increase in the rate of nearby hospitals offering PCI increases the odds of offering PCI by a factor of 1.794, or a 79.4 percent increase (95% CI: 1.29–2.50). That is, a hospital is nearly twice as likely to offer PCI, conditional on characteristics of the neighboring population, in a market of ten equal-sized hospitals when one other hospital adds PCI. Hospitals are less likely to adopt new PCI technology if nearby hospitals already had CABG capability, after controlling for the fact that nearby hospitals that offer CABG also offer PCI (Odds Ratio: .726; 95% CI: 0.575–0.916).
The patterns are similar for diagnostic angiography. Hospitals were more likely to adopt new diagnostic angiography technology if more neighboring hospitals already had it, and they were less likely to do so if more neighboring hospitals offered PCI, a more sophisticated technology. A 10 percentage point increase in the rate of nearby hospitals offering diagnostic angiography corresponded to a 10.2 percent increase in the odds of offering diagnostic angiography (Odds Ratio 1.102, 95% CI: 1.02–1.19). The pattern was imprecisely estimated for CABG, with non-significant point estimates suggesting an increased likelihood of offering CABG if more nearby hospitals offered PCI (OR 1.44) or recently added PCI (OR 2.30), but somewhat less if nearby hospitals offered diagnostic angiography (0.81) or CABG (0.93).
Geographic Access to Care
Our results also demonstrated that existing diffusion methods lead to clusters of services, adding little geographic access to care. In 1997, 94% of the U.S. population lived within 40 miles of a hospital that provided diagnostic angiography, with 88% within 40 miles for both PCI and CABG. Despite widespread adoption of new services, by 2008 there was a one percentage point increase in the population with geographic access to diagnostic angiography (five percentage points for PCI, and four percentage points for CABG.
On average over the study period, about 90% of those people served by new cardiac services—i.e., residents within 40 miles of a newly offered service—already lived within 40 miles of other hospital with those services. Over the study period, the duplication of services increased; more services were added where at least one hospital previously offered the service. In 1996, about 80% of people who lived within 40 miles of a cardiac service newly added in the last year already had access to those services; by 2008 that number was number was 95%.
Alternative methods of service allocation would have generated greater geographic access to care. Compared to a method of service distribution optimized to increase geographic access, the efficiency of actual allocation (measured as the ratio of actual to simulated optimally allocated new coverage) was less than 1% percent in all years for all three services. For example, on average over the study period, new diagnostic angiography allowed access for 0.16 percent of the population that could have had new access to care (again defined as living in a census tract with a centroid within 40 miles of the new service) had diagnostic angiography been assigned to other existing hospitals so as to maximize geographic access. (Table 3) Similarly, new PCI (or CABG) services reached 0.23 percent (0.35 percent for CABG) of the potential population that could have had new access to care had PCI been assigned to maximize new access to care.
Table 3.
Access to New Cardiac Treatments, Duplication v. Newly Served Population.
| Year | 1997 | 2002 | 2008 | Annual Average 97-08 |
|---|---|---|---|---|
| Diagnostic Angiography | ||||
| Actual Increase / Public Health Planning Increase | 0.42% | 0.13% | 0.02% | 0.16% |
| Actual/Random | 135% | 105% | 44% | 132% |
| PCI | ||||
| Actual Increase / Public Health Planning Increase | 0.17% | 0.29% | 0.09% | 0.23% |
| Actual/Random | 125% | 170% | 47% | 97% |
| CABG | ||||
| Actual Increase / Public Health Planning Increase | 0.53% | 0.42% | 0.05% | 0.35% |
| Actual/Random | 154% | 124% | 41% | 131% |
Notes: Data and methods are described in the text. Random allocations are averaged over 500 random draws. Actual increases in each type of service are compared to alternative placement of the same number of new service locations, one planned to add the largest possible number of new population covered and one random. For example, new Diagnostic Angiography in 2002 (middle column) led to new access to care for those living within 40 miles, who were not already within 40 miles of a hospital offering it. This increase was an eighth of a percent of the increase that would have been possible had a public health planning approach been used. In contrast, it was 5% greater than the increase in newly accessibly population that would have occurred, on average, in a purely random allocation.
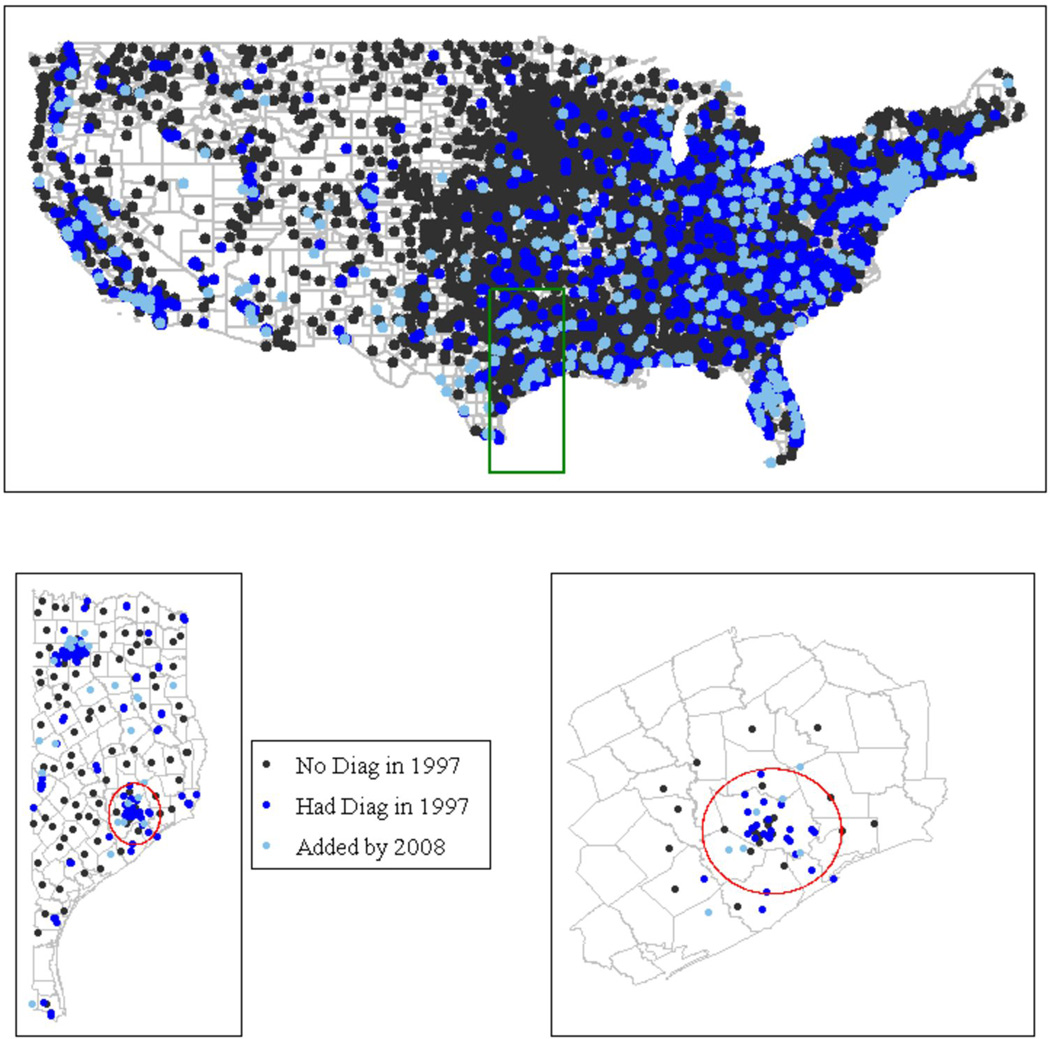
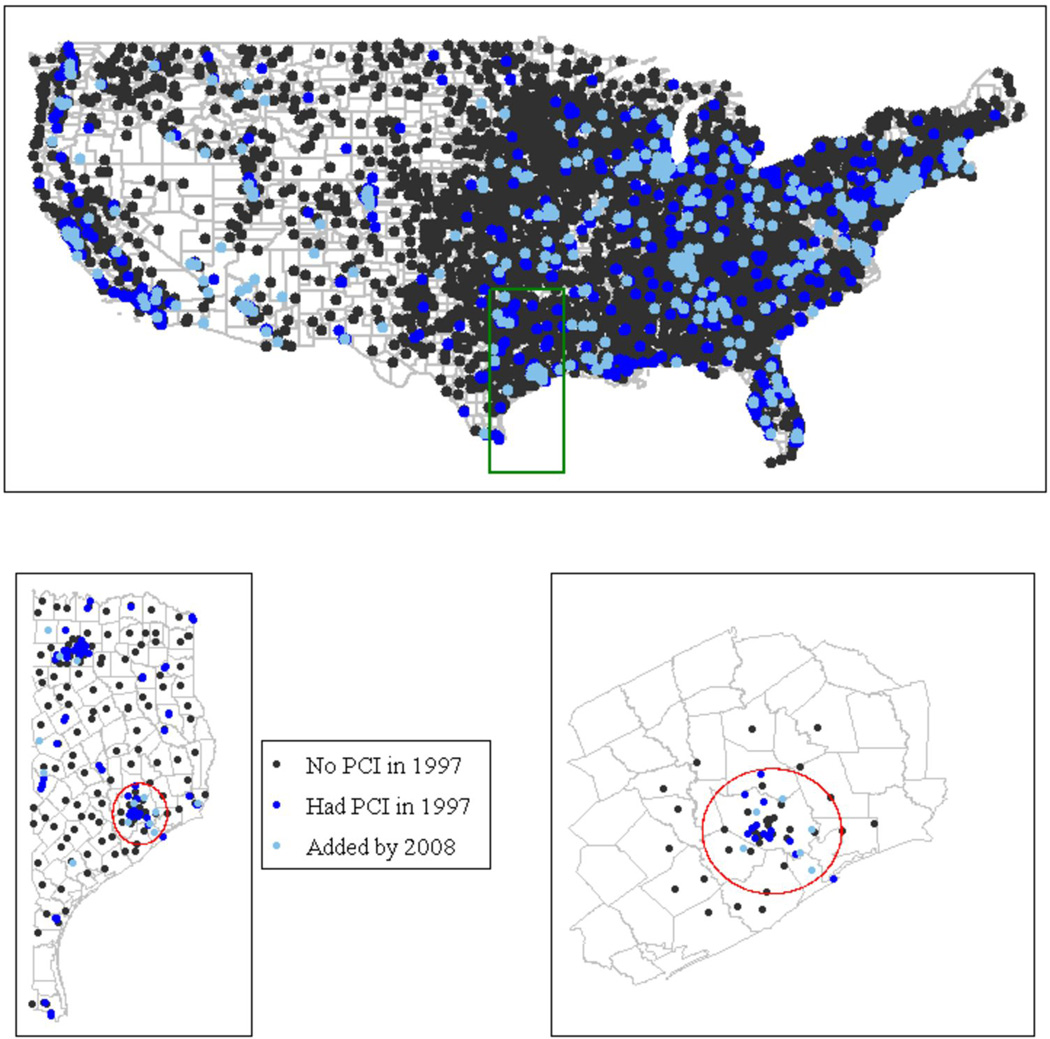
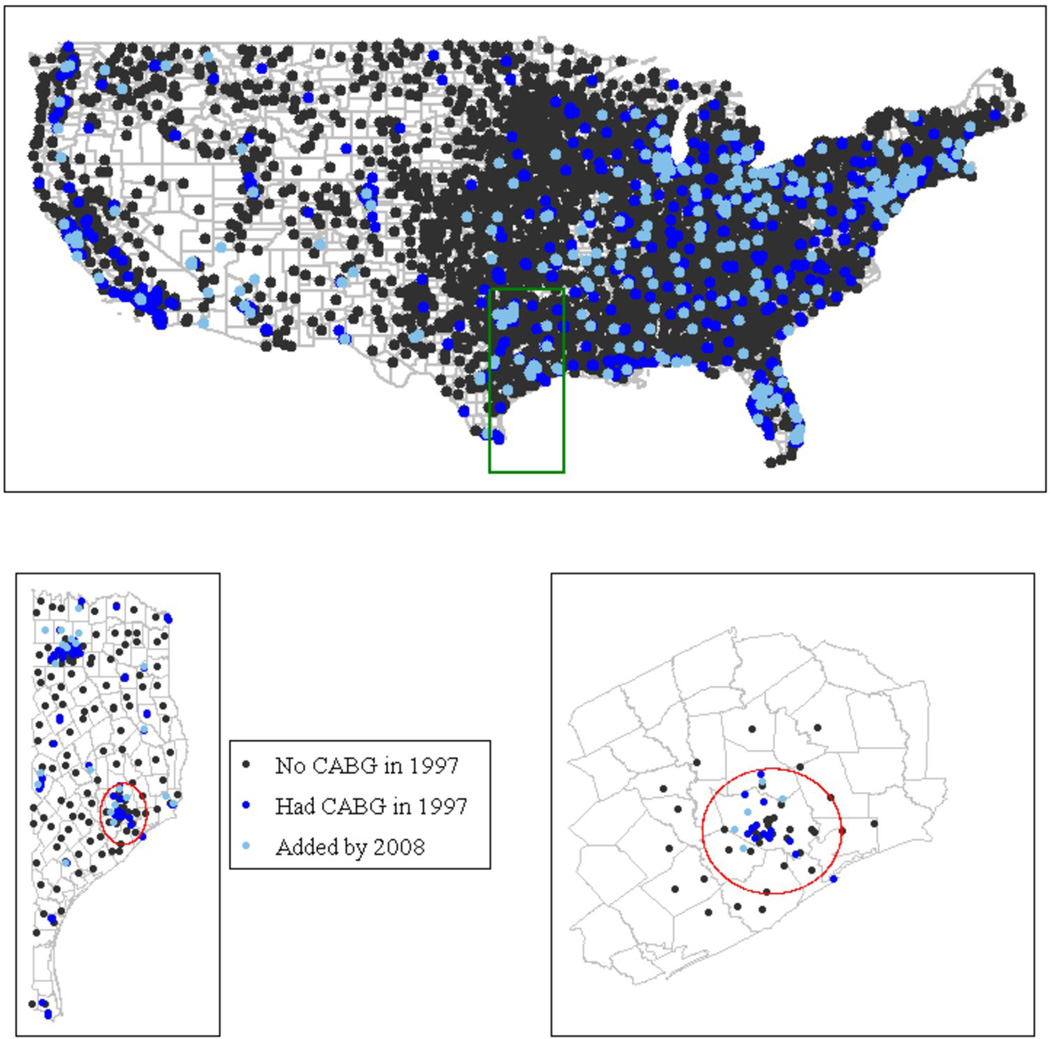
The geographic clustering of services can be seen most easily in Figures. The black dots indicate existing hospitals that did not offer diagnostic angiography (Figure 1) (or PCI – Figure 2 or CABG – Figure 3) in 1997, and the dark blue dots indicate hospitals that offered that service. The light blue dots identify hospitals that adopted that service by the end of the study period, 2008. All hospitals are located by their latitude and longitude. The substantial duplication of new service offerings is evident in both the U.S. map and the detailed Houston area map, chosen to give a clearer idea of duplicative adoption patterns. The red circle represents a radius of 40 miles, indicating the hospitals within the recommended distance of central Houston. Note that new service tends to be added near existing service, rather than outside the 40 mile radius.
Figure 1.
New Diagnostic Angiography Adoption 1997–2008. The black dots represent the location of hospitals that did not offer diagnostic angiography in 1997. The dark blue dots represent the location of hospitals that offered diagnostic angiography in 1997. The light blue dots indicate the hospitals that offered diagnostic angiography by the end of 2008. The close proximity of the light blue and dark blue dots indicates that services tend to cluster rather than expand geographic access to care. The small map represents the Houston area, with the red circle identifying a 40 mile radius (an approximation of the market for invasive cardiac treatment based on one-hour travel time). The new services (represented by light blue dots) tend to occur near previously existing services, rather than outside of the red circle, where they might serve patients otherwise without geographic access. All dots are located according the latitude and longitude of the hospitals.
Figure 2.
New PCI Adoption 1997–2008. The black dots represent the location of hospitals that did not offer PCI in 1997. The dark blue dots represent the location of hospitals that offered PCI in 1997. The light blue dots indicate the hospitals that offered PCI by the end of 2008. The close proximity of the light blue and dark blue dots indicates that services tend to cluster rather than expand geographic access to care. The small map represents the Houston area, with the red circle identifying a 40 mile radius (an approximation of the market for invasive cardiac treatment based on one-hour travel time). The new services (represented by light blue dots) tend to occur near previously existing services, rather than outside of the red circle, where they might serve patients otherwise without geographic access. All dots are located according the latitude and longitude of the hospitals.
Figure 3.
New CABG Adoption 1997–2008. The black dots represent the location of hospitals that did not offer CABG in 1997. The dark blue dots represent the location of hospitals that offered CABG in 1997. The light blue dots indicate the hospitals that offered CABG by the end of 2008. The close proximity of the light blue and dark blue dots indicates that services tend to cluster rather than expand geographic access to care. The small map represents the Houston area, with the red circle identifying a 40 mile radius (an approximation of the market for invasive cardiac treatment based on one-hour travel time). The new services (represented by light blue dots) tend to occur near previously existing services, rather than outside of the red circle, where they might serve patients otherwise without geographic access. All dots are located according the latitude and longitude of the hospitals.
Had the same number of new services been randomly distributed to existing hospitals without cardiac services, new geographic access to those services would not be statistically different from that which we observed. (Table 3) Although on average over the study period, new diagnostic angiography reached 32 percent more, PCI 3 percent fewer, and CABG 31 percent more people than a purely random allocation, the annual percentages were highly variable and all lie within the confidence intervals generated by the random distribution of new services to existing hospitals.
DISCUSSION
This analysis of national CMS, Census, and AHA data demonstrates at least two novel results. First, confirming other research demonstrating the increase in PCI services,13 we find that the number of hospitals offering diagnostic cardiac catheterization, PCI, and CABG increased substantially over the study period. Second, hospitals were more likely to adopt these technologies if more nearby hospitals already offered them, even controlling for the potential patient population of hospital markets. Third, despite widespread new cardiac capacity, there has been only modest increase in geographic access to care. The findings have implications for capacity planning, spending, and quality of care.
The rapidly aging population and developments in medical technology have led policy experts to predict workforce shortages,14 not only in primary care but also for specialty services15 such as cardiology.16 By demonstrating a growth in services, our results demonstrate that the system has overall capacity to address the needs of an aging population in aggregate, but also that the system struggles to match new capacity with population health needs.
Although our study does not directly address the health risks associated with current patterns of cardiac care diffusion, the mismatches we identified between technology supply and population suggest possible implications for both cost-effectiveness and quality.17 Previous research has demonstrated that the availability and use of cardiac services varies dramatically by region, yet cannot be explained by differences in patient indications.18 We extended these findings by showing that hospitals are more likely to adopt new services where they already exist. This suggests a possible competitive mechanism for the clustering of services and for why some areas remain without access to services while others appear to have greater capacity.
Moreover, our results may have quality and cost implications. Some of these implications suggest decreases in quality. First, some proponents argue that rapid access to treatments such as PCI leads to mortality reductions for acute myocardial infarction.19,20 While our data cannot speak to patient-level outcomes, if PCI is being expanded to improve population health by reducing door-to-balloon times in acute myocardial infarction, then our results suggest this is not being done very efficiently as many areas remain without these services. Second, geographic duplication of services likely leads to declines in hospital volume. In fact, Medicare patients have increasingly obtained CABG at low-volume hospitals.21 Given the positive, though attenuating, association between volume and outcomes,22 the diffusion patterns we identified could decrease quality, as some researchers have found that the lower volume occurring where hospitals have newly adopted CABG has caused increased mortality.23 And, although researchers have found that CABG mortality decreased in the 1990s despite decreases in volume, they point to quality and technology improvements as the cause.24
On the other hand, there is the potential for new competition to reduce the prices that hospitals charge for cardiac care, although this potential is limited to the extent that hospitals rely on government reimbursement for cardiac services. In addition, there is a body of research suggesting that competition can increase quality. In a study of the effects of hospital competition on AMI patients from 1985 to 1994, for example, Kessler and McClellan show that although the effects of competition on expenditures and outcomes were ambiguous in eh 1980s, competition led to lower expenditures on treatment and better outcomes in the 1990s.25 Moreover, Cutler et. al. have found that quality of care for CABG patients improved slightly after the repeal of CON in Pennsylvania, an improvement they attribute to the redistribution of operations to higher quality surgeons.26
The clustering patterns we observed raise potential policy interventions. Despite active CON programs in several states, we find no regulatory effect on clustering, suggesting that CON regulations could be more rigorously enforced or better designed to address geographic access. For example, programs could require a demonstration that new services will address geographic need, not only population need as is often the focus of such regulations. Moreover, since technology adoption regulation is primarily state-based, the system is subject to local regulatory capture and cannot account for cross-border effects. To address such problems, federal agencies such as CMS could play a more active role in licensing and, perhaps, tie reimbursement to geographic as well as other forms of access.
Our study has several limitations. First, the data introduced some challenges. Because we identified hospitals offering cardiac services from the MedPAR, our sample excludes hospitals serving only non-Medicare patients. Our population measures came from the U.S. Census, which is based on residence, not work location. We also relied on self-reported measures of hospital characteristics. Second, unlike our regression estimates, the simulation results define access only in geographic terms, unadjusted for population density; in metropolitan areas, sufficient access may require many hospitals to offer cardiac services. Third, because our focus is on hospitals that compete over many services, we excluded specialized cardiac hospitals. Since single-service hospitals tend to locate in a few regions, however, including them would likely have strengthened our findings.
Finally, and most important, we cannot determine whether the propensity of hospitals to adopt new services near existing services is a response to unmet demand in the market. Patients in geographic areas that appear to be underserved may obtain cardiac services through networks of hospitals that successfully provide services to geographically remote areas.27 And it may be that rural hospitals that wish to adopt cardiac services are unable to find doctors to provide those services. We can only conclude that such clustering of services did not expand geographic access in the sense that services tended to be opened in locations where the population was already located within 40 miles of existing services and not elsewhere.
To our knowledge, this is the first national assessment of new adoption of the three main invasive cardiac services and the resulting effects on geographic access. Significant new capacity for invasive cardiac services has been added to the U.S. in the thirteen years under study. However, current methods of cardiac technology diffusion—some combination of market competition and technology regulation—do not increase geographic access to care but rather lead to duplication of services. Innovative healthcare policies to develop a coordinated system of care which is based in part on increasing geographic access, within and across state borders, may be a next step in improving the diffusion of these life-saving cardiovascular technologies and ultimately improving the health of the population.
Acknowledgements
We thank Jon Skinner and Lemore Dafny for sharing data crosswalks, and Joseph Doherty for data advice. We thank Laetitia Shapiro for her expert programming.
Funding Sources: This work was supported by the University of Michigan Law School Cook Fund to J.R.H. and U.S. NIH K08 HL091249 to T.J.I. The views expressed here are not necessarily those of the U.S. Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures: None.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford E, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern S, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker L, Birnbaum H, Geppert J, Mishol D, Moyneur E. The relationship between technology availability and health care spending. Health Aff. 2003:W3-537–W3-551. doi: 10.1377/hlthaff.w3.537. [DOI] [PubMed] [Google Scholar]
- 3.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:2128–2137. doi: 10.1056/NEJMsa1010705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wharton TP., Jr Should patients with acute myocardial infarction be transferred to a tertiary center for primary angioplasty or receive it at qualified hospitals in the community? The case for community hospital angioplasty. Circulation. 2005;112:3509–3534. doi: 10.1161/CIRCULATIONAHA.104.478362. [DOI] [PubMed] [Google Scholar]
- 5.Skinner J, Staiger DO, Fisher ES. Is technological change in medicine always worth it? The case of acute myocardial infarction. Health Aff. 2006;25:w34–w47. doi: 10.1377/hlthaff.25.w34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buckley JW, Bates ER, Nallamothu BK. Primary percutaneous coronary intervention expansion to hospitals without on-site cardiac surgery in Michigan: a geographic information systems analysis. Am Heart J. 2008;155:668–672. doi: 10.1016/j.ahj.2007.10.051. [DOI] [PubMed] [Google Scholar]
- 7.Buckley JW, Bates ER, Nallamothu BK. Primary percutaneous coronary intervention expansion to hospitals without on-site cardiac surgery in Michigan: a geographic information systems analysis. Am Heart J. 2008;155:668–672. doi: 10.1016/j.ahj.2007.10.051. [DOI] [PubMed] [Google Scholar]
- 8.Lucas FL, Siewers A, Goodman DC, Wang D, Wennberg DE. New cardiac surgery programs established from 1993 to 2004 led to little increased access, substantial duplication of services. Health Aff. 2011;30:1569–1574. doi: 10.1377/hlthaff.2010.0210. [DOI] [PubMed] [Google Scholar]
- 9.Kansagra SM, Curtis LH, Schulman KA. Regionalization of percutaneous transluminal coronary angioplasty and implications for patient travel distance. JAMA. 2004;292:1717–1723. doi: 10.1001/jama.292.14.1717. [DOI] [PubMed] [Google Scholar]
- 10.Wilson CT, Fisher ES, Welch HG, Siewers AE, Lucas FL. U.S. trends in CABG hospital volume: the effect of adding cardiac surgery programs. Health Aff. 2007;26:162–168. doi: 10.1377/hlthaff.26.1.162. [DOI] [PubMed] [Google Scholar]
- 11.Horwitz JR, Nichols A. Hospital ownership and medical services: market mix, spillover effects, and nonprofit objectives. J Health Econ. 2009;28:924–937. doi: 10.1016/j.jhealeco.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 13.Langabeer JR, Henry T, Fraine JD, Emert J, King R, Stuart L, Segrest W. Geospatial analysis of percutaneous coronary intervention hospitals. J Am Coll Cardiol. 2012;59:E1804–E1804. [Google Scholar]
- 14.Iglehart JK. Despite tight budgets, boosting US health workforce may be policy that is ‘just right.’. Health Aff. 2011;30:191–192. doi: 10.1377/hlthaff.2011.0142. [DOI] [PubMed] [Google Scholar]
- 15.Cooper RA, Getzen TE, McKee HJ, Laud P. Economic and demographic trends signal an impending physician shortage. Health Aff. 2002;21:140–154. doi: 10.1377/hlthaff.21.1.140. [DOI] [PubMed] [Google Scholar]
- 16.Fye WB. Cardiology workforce: a shortage, not a surplus. Health Aff. 2004:W4-64–W4-66. doi: 10.1377/hlthaff.w4.64. [DOI] [PubMed] [Google Scholar]
- 17.Association Ad Hoc Task Force on Cardiac Catheterization ACC/AHA guidelines for cardiac catheterization and cardiac catheterization laboratories. Circulation. 1991;84:2213–2247. doi: 10.1161/01.cir.84.5.2213. [DOI] [PubMed] [Google Scholar]
- 18.Skinner J, Staiger DO, Fisher ES. Is technological change in medicine always worth it? The case of acute myocardial infarction. Health Aff. 2006;25:w34–w47. doi: 10.1377/hlthaff.25.w34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kushner FG, Hand M, Smith SC, Jr, King SB, III, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE, Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205–2241. doi: 10.1016/j.jacc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 20.Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ. Relationship of symptom-onset-to-balloon time and door-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–2947. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 21.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:2128–2137. doi: 10.1056/NEJMsa1010705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ross JS, Normand SL, Wang Y, Ko DT, Chen J, Drye EE, Keenan PS, Lichtman JH, Bueno H, Schreiner GC, Krumholz HM. Hospital volume and 30-day mortality for three common medical conditions. N Engl J Med. 2010;362:1110–1118. doi: 10.1056/NEJMsa0907130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilson CT, Fisher ES, Welch HG, Siewers AE, Lucas FL. U.S. trends in CABG hospital volume: the effect of adding cardiac surgery programs. Health Aff. 2007;26:162–168. doi: 10.1377/hlthaff.26.1.162. [DOI] [PubMed] [Google Scholar]
- 24.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:2128–2137. doi: 10.1056/NEJMsa1010705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kessler DP, McClellan MB. Is hospital competition socially wasteful? Quarterly J Econ. 2000;115:577–615. [Google Scholar]
- 26.Cutler DM, Huckman RS, Kolstad JT. Amer Econ J: Econ Policy. Vol. 2. American Economic Association; 2010. Input Constraints and the Efficiency of Entry: Lessons from Cardiac Surgery; pp. 51–76. [Google Scholar]
- 27.Iwashyna TJ, Kahn JM, Hayward RA, Nallamothu BK. Interhospital Transfers Among Medicare Beneficiaries Admitted for Acute Myocardial Infarction at Nonrevascularization Hospitals. Circulation-Cardiovascular Quality and Outcomes. 2010;3:468–475. doi: 10.1161/CIRCOUTCOMES.110.957993. [DOI] [PMC free article] [PubMed] [Google Scholar]