Abstract
The tumor necrosis factor alpha is a cytokine related to immune and inflammatory processes by acting on different parts of the body. It is secreted by several cell types including macrophages, lymphocytes, monocytes, neutrophils, dendritic cells, among others. Infliximab is a chimeric monoclonal antibody that specifically binds to soluble and transmembrane tumor necrosis factor alpha form blocking its action. In rheumatoid arthritis it is used because the cytokines that cause inflammation in this disease are regulated by tumor necrosis factor alpha and IL-1. We report the case of a 46-year-old patient with rheumatoid arthritis who developed segmental vitiligo after two months using infliximab. The event aims to alert to the existence of this adverse effect that can be induced with the use of this medication.
Keywords: Arthritis, rheumatoid; Tumor necrosis factor-alpha; Vitiligo
INTRODUCTION
Rheumatoid arthritis (RA) is an autoimmune disease of unknown etiology, which affects the synovial membranes and is characterized by peripheral symmetrical polyarthritis, leading to deformity and destruction of joints by bone and cartilage erosion.1
After the discovery that on the synovial membrane of patients with RA occurs the expression of several cytokines implicated in inflammatory reactions, the TNFα became the ideal target for joint inflammation control. Infliximab is a chimeric monoclonal antibody anti-TNFα of chimeric profile, that is, 75% human and 25% murine, which confers to it greater specificity, affinity and high avidity due to both soluble and transmembrane forms of TNFα.2
Several adverse effects have already been observed with the use of infliximab. The main ones include allergic complications during or after the infusion, infections, autoimmune events and lymphoproliferative diseases.3
Among the autoimmune complications, central nervous system demyelinating syndromes, diabetes mellitus type 1, psoriasis, lupus-like cases and even systemic lupus erythematosus, including laboratory alterations like ANF increase and development of other autoantibodies.3,4,5,6
Vitiligo is a cutaneous disease, characterized by the presence of achromic macules of different sizes and forms with the tendency of increasing centrifugally.7,8
Its etiopathogeny is related to autoimmunity, with occurrence of association with thyroiditis, diabetes mellitus, alopecia areata and with HLA DR4, DW7, DR1, B13, A2, B21, CW6, DR53, A19 and DR52. It can be classified as localized or generalized, the localized form being divided into focal, when in a determined area without specific distribution, and segmental when it involves a unilateral segment of the body following a dermatome.7
Several cutaneous diseases have already been described with the use of immunobiologic drugs, such as psoriasis, lichenoid eruptions, herpes zoster, vasculitis, alopecias and cutaneous lymphomas;5 however, the relation between vitiligo and the use of anti-TNFα is rare and few cases have been described, all of them associated with the use of infliximab. It is demonstrated for the first time, in the segmental form and nationwide, in this report.3,4,5,6,9
CASE REPORT
A forty-six-year old female patient, of mixed race, diabetic, with rheumatoid arthritis for seven years. Denies personal or familial history of vitiligo. She mentioned the onset of achromic macules six months ago, initially on the left hand, which progressed in the craniocaudal direction involving all the left hemithorax and upper left limb.
She was using infliximab every eight weeks for eight months.
She was also using propranolol 20mg/day, metformin 850mg/day and glibenclamide 5mg/day.
For this cutaneous state she had used topical 10% phenylalanine, clobetasol 0.025%, 2% vitamin E and Polipodium leucotomos 240 mg/day orally for 30 days, at another service, with no improvement.
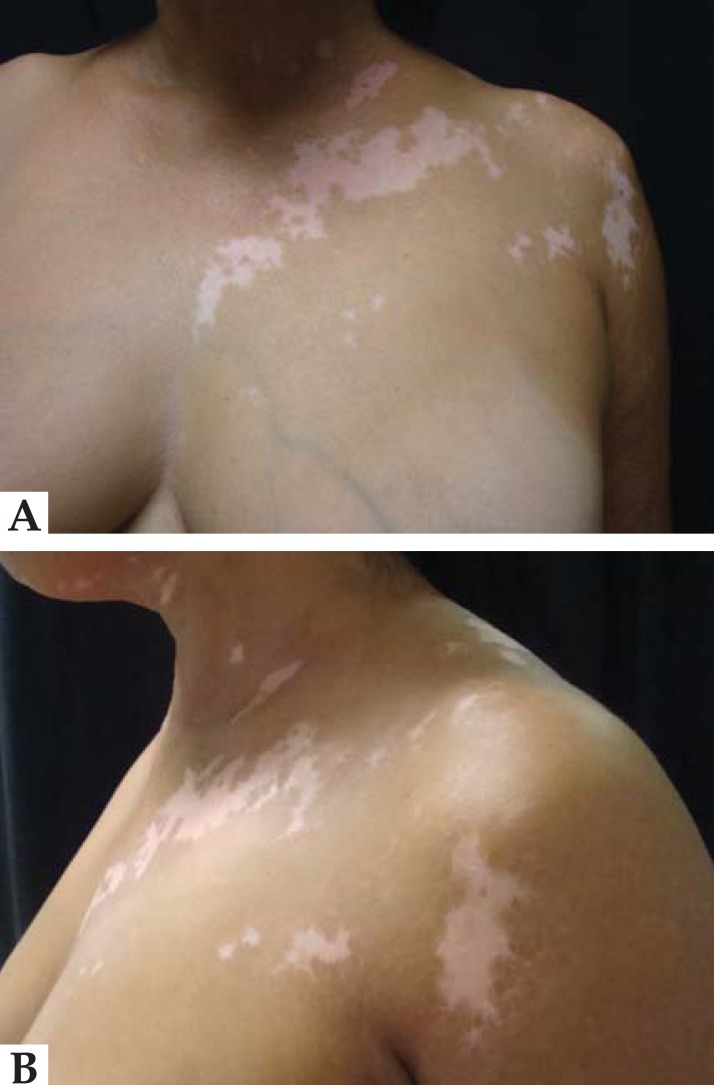
At the dermatological examination achromic macules were observed on the left upper limb and left hemithorax, which under Wood's light presented nacreous white coloration (Figure 1).
FIGURE 1.
A - Pre-treatment vitiligo on left hemibody; B - Pre-treatment vitiligo on left hemibody
There were no abnormalities detected in the remainder of the physical exam.
Among the laboratory exams she presented hemogram, biochemistry and thyroid hormones without changes, serologies for HIV, hepatitis and syphilis negative and one ANF 1: 640 of mixed pattern, nuclear dense fine speckled and cytoplasmic dotted reticular, with native anti-DNA autoantibodies, anti Jo, anticardiolipin, anti-centromere, anti Sm, anti Ro, anti La, anti TPO negative.
DISCUSSION
The use of TNFα inhibiting agents has already been associated with cutaneous and also autoimmune manifestations several times, from laboratory alterations of asymptomatic nature to the presence of systemic diseases, including findings of autoantibodies like ANF and anti-DNA.3,4,5,6
Among the hypotheses raised to explain the positivity of AFN with the usage of infliximab is the induction of TNFα-producing cells lysis, exposing intracellular particles to the immunesystem and leading to increase of this factor.3,6
The presence of autoantibodies against melanocytes in the bloodstream of patients with vitiligo raises the theory of autoimmunity as its cause, and the presence of these autoantibodies seems to be related to the extent of the disease in affected patients.8
The skin damaged by vitiligo presents enhanced expression of TNFα and IL6 when compared to perilesional skin; TNFα blocks the differentiation of melanocytic stem cells and can induce the apoptosis of melanocytes which suggests that the blockage of these cytokines might be the key to its treatment. However, to the contrary of what was suggested, the case in question progressed with the onset of vitiligo.10
Vitiligo is an autoimmune disease, therefore the development of this infirmity associated with the use of infliximab can be explained by the same lupus-like syndrome mechanism.3
After searching databases, few cases were found reporting infliximab use as triggering vitiligo; this was the first with progression to segmental form and also the first nationwide.
The patient here reported had never presented cutaneous lesions that would suggest vitiligo and also denies familial history, developing the lesion after two months using the drug, besides the ANF positivity.
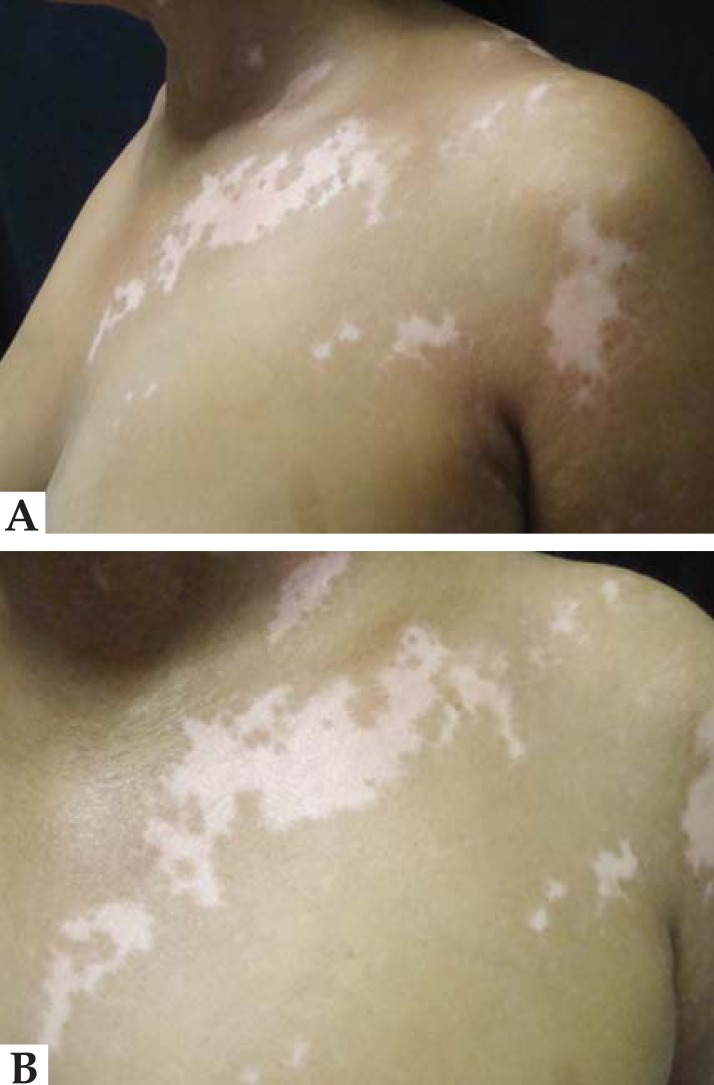
Since there was marked improvement of the articular clinical picture, we opted for non-interruption of the drug and treatment of vitiligo with 8-methoxypsoralen 0.001% in topical hydroalcoholic solution, followed by solar exposure and dexamethasone cream on the macules at night (Figure 2).
FIGURE 2 .
A - Vitiligo on left hemibody during treatment; B - Vitiligo on left hemibody during treatment
Infliximab is as important for dermatology as it is for rheumatology and gastroenterology, enhancing the quality of life of patients under treatment. However, we should be always alert, not only to systemic collateral effects, but also to possible cutaneous adverse effects associated with its use which will be more and more evident.
Footnotes
Work performed at Hospital Regional de Presidente Prudente - Universidade do Oeste Paulista (HRPP- UNOESTE) - Presidente Prudente (SP), Brazil.
Financial funding: None
Conflict of interest: None
REFERENCES
- 1.Mota LMH, Laurindo IMM, Neto LLS. Artrite Reumatóide Inicial - Conceitos. Rev Assoc Med Bras. 2010;56:227–229. doi: 10.1590/s0104-42302010000200024. [DOI] [PubMed] [Google Scholar]
- 2.Silva LC, Ortigosa LC, Benard G. Anti-TNF agents in the treatment of immuneme-diated inflammatory diseases: mechanisms of actions and pitfalls. Immunotherapy. Immunotherapy. 2010;2:817–833. doi: 10.2217/imt.10.67. [DOI] [PubMed] [Google Scholar]
- 3.Ramírez-Hernández M, Marras C, Martínez-Escribano JA. Infliximab-Induced Vitiligo. Dermatology. 2005;210:79–80. doi: 10.1159/000081494. [DOI] [PubMed] [Google Scholar]
- 4.Lahita RG, Vernace MA. Vasculitis, Vitiligo, Thyroiditis, and Altered Hormone Levels After Anti-Tumor Necrosis Factor Therapy. J Rheumatol. 2011 Mar;38(3):579–580. doi: 10.3899/jrheum.100968. [DOI] [PubMed] [Google Scholar]
- 5.Hernández MV, Meineri M, Sanmartí R. Skin Lesions and Treatment With Tumor Necrosis Factor Alpha Antagonists. Reumatol Clin. 2013;9:53–61. doi: 10.1016/j.reuma.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 6.Duarte AA, Chehin FB. Moderate to severe psoriasis treated with infliximab - 53 patients: patients profile, efficacy and adverse effects. An Bras Dermatol. 2011;86:257–263. doi: 10.1590/s0365-05962011000200008. [DOI] [PubMed] [Google Scholar]
- 7.Steiner D, Bedin V, Moraes MB, Villas RT, Steiner T. Vitiligo. An Bras Dermatol. 2004;79:335–351. [Google Scholar]
- 8.Correa MCT, Vargas LMG. Vitiligo. Rev Asoc Col Dermatol. 2009;17:76–86. [Google Scholar]
- 9.Bonnet N, Guis S, Koeppel MC, Roudier J, Grimaud JC, Jean-Pastor MJ, et al. Cutaneous events during anti-TNF alpha therapy: a prospective observational study of 41 cases. Ann Dermatol Venereol. 2010;137:12–20. doi: 10.1016/j.annder.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Alghamdi KM, Khurrum H, Rikabi A. Worsening of vitiligo and onset of new psoriasiform dermatitis following treatment with infliximab. J Cutan Med Surg. 2011;15:280–284. doi: 10.2310/7750.2011.10068. [DOI] [PubMed] [Google Scholar]
- 11.Machado-Filho CDS, Almeida FA, Proto RS, Landman G. Vitiligo: analysis of grafting versus curettage alone, using melanocyte morphology and reverse transcriptase polymerase chain reaction for tyrosinase mRNA. Sao Paulo Med J. 2005;123:187–191. doi: 10.1590/S1516-31802005000400006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rao A, Gupta S, Dinda AK, Sharma A, Sharma VK, Kumar G, et al. Study of clinical, biochemical and immunological factors determining stability of disease in patients with generalized vitiligo undergoing melanocyte transplantation. Br J Dermatol. 2012;166:1230–1236. doi: 10.1111/j.1365-2133.2012.10886.x. [DOI] [PubMed] [Google Scholar]