Abstract
Experimental autoimmune uveoretinitis (EAU) is an organ-specific T cell-mediated disease induced by immunizing mice with interphotoreceptor retinoid binding protein (IRBP). Autoaggressive CD4+ T cells are the major pathogenic population for EAU. We investigated the contribution of Notch signaling in T cells to EAU pathogenesis because Notch signaling regulates various aspects of CD4+ T cell functions. Rbpj is required for Notch signaling, and Rbpj deficiency in T cells inhibited EAU disease severity. The amelioration of EAU in T cell-specific Rbpj-deficient mice correlated with low levels of IL-22 production from CD4+ T cells, although IRBP-specific CD4+ T cell proliferation and Th17 differentiation were unaffected. Administration of recombinant IL-22 during the late phase, but not the early phase, of EAU increased EAU clinical scores in T cell-specific Rbpj-deficient mice. Notch inhibition in mice immunized with IRBP with a γ-secretase inhibitor (GSI) suppressed EAU progression, even when GSI was administered as late as 13 days after IRBP immunization. Our data demonstrate that Rbpj/Notch-mediated IL-22 production in T cells has a key pathological role in the late phase of EAU, and suggest that Notch blockade might be a useful therapeutic approach for treating EAU.
Introduction
Experimental autoimmune uveoretinitis (EAU) is an organ-specific, T cell-mediated disease initiated by immunizing mice with retinal antigens or their fragments [1] [2] [3] [4]. EAU represents a breakdown in tolerance to immunologically privileged retinal antigens, such as interphotoreceptor retinoid binding protein (IRBP) and arrestin, which function in the visual cycle. EAU is a model for human ocular diseases including Behcet's disease, Vogt-Koyanagi-Harada syndrome, and Birdshot retinochoroidopathy [1] [4]. CD4+ T cells are crucial for EAU development, which is supported by the finding that EAU can be elicited by adoptive transfer of retinal-specific CD4+ T cells [5]. Although Th1 cells are activated in EAU, it has been reported that IL-12 down regulates EAU, and treatment of mice with EAU with anti-IFN-γ antibodies aggravated the disease [6] [7]. Subsequent reports have demonstrated the importance of Th17 in EAU pathogenesis [8] [9]. In therapeutic settings, it is essential to identify which T cells or which cytokines are crucial for each phase during EAU progression or human autoimmune uveoretinitis.
Notch is an evolutionarily conserved molecule that controls cell fate decisions in a variety of cells [10]. Notch molecules are cleaved in their transmembrane region by γ-secretase through interaction with Notch ligands, after which the intracellular domain translocates into the nucleus [10]. We and other groups have demonstrated that Notch signaling controls CD4+ T cell effector functions [11] [12] [13] [14] [15]. Moreover, it has been reported that inhibition of γ-secretase or Delta-like 4 (Dll4) blocked the development of experimental autoimmune encephalomyelitis [16] [17] [18], suggesting that Notch signaling in T cells is involved in the progression of autoimmune responses. Although anti-Dll4 antibody ameliorates EAU [19], the roles of Notch signaling in T cells for EAU progression remain unclear.
These earlier reports led us to investigate the role of Notch signaling in the development of EAU. In this study, we show that T cell-specific Rbpj-deficient mice are resistant to EAU, and that this dramatic outcome derives from low IL-22 production by CD4+ T cells without affecting T cell priming and Th17 differentiation. Treatment of mice with a γ-secretase inhibitor (GSI) attenuated the progression of EAU. The resistance of Rbpj conditional knockout mice to developing EAU and the successful treatment of EAU by GSI suggest that the Notch pathway is a potential therapeutic target in inflammatory ocular disease.
Materials and Methods
Animals
Six- to 8-wk-old C57BL/6 mice were purchased from Japan SLC (Hamamatsu, Japan). Rbpj flox/flox mice crossed CD4-Cre transgenic mice or E8I-Cre transgenic mice are described elsewhere [12] [20]. All mice were housed under specific pathogen-free conditions in the Animal Research Center of the University of Tokushima. Animal care and use was in compliance with institutional guidelines and was approved by the Animal Research Committee of the University of Tokushima.
Antibodies and flow cytometry
Monoclonal antibodies specific for mouse CD4 (GK1.5) or CD8 (53-6.7) were purchased from BioLegends (San Diego, CA, USA). Flow cytometry data were acquired on a FACSCaliber (BD Biosciences, CA, USA) and CellQuest (BD Biosciences) software was used for analysis.
Induction of EAU
Mice were immunized subcutaneously with 50 µg of IRBP emulsified with CFA (St. Louis, MO) that had been supplemented with M. tuberculosis strain H37RA (Difco, Detroit, MI) to a final IRBP concentration of 2.5 mg/ml. Concurrent with immunization, 0.5 µg of pertussis toxin was injected intraperitoneally. The severity of eye disease was evaluated by fundoscopic examination. Mice were anesthetized and their pupils dilated. The fundus was observed using a stereoscopic microscope. Disease severity was scored on a scale of 0 (no disease) to 4 (maximum disease) depending on the degree of inflammation and retinal damage using established criteria.
Treatment of mice with GSI or rIL-22
Mice immunized with IRBP were treated with GSI LY-411575 (Stemgent, San Diego, CA) (5 mg/kg/d, dissolved in DMSO) at 2-day intervals that began on the day of IRBP immunization. Recombinant IL-22 (Peprotec) (2 µg/dose) was administered to mice that had been immunized with IRBP at 3-day intervals that began one day after IRBP immunization and stopped 13 days after immunization, began 14 days after immunization and continued throughout the entire experiment, or began one day after IRBP immunization and continued throughout the entire experiment.
T cell proliferation assay
Draining lymph nodes were collected and pooled within each group. For purification of total CD4+ cells, lymph node cells were incubated with anti-B220 (RA3-6B2), anti-CD32/16 (2.4G2), anti-CD11b (M1/70) and anti-CD8 (53-6.7) mAbs (BioLegends) followed by incubation with anti-rat IgG-coated Dynabeads (Dynal Inc.). CD4+ T cells were further purified by magnetic separation using biotin-conjugated anti-CD4 and streptavidin microbeads (Miltenyi Biotech). CD4+ T cells were cultured with irradiated spleen cells with 0.1, 1 or 10 µg/ml IRBP in 96-well round-bottom plates at a concentration of 5×105 cells/well in RPMI 1640 supplemented with 2-ME, glutamine, nonessential amino acids, sodium pyruvate, and antibiotics, and 10% fetal bovine serum. For T cell proliferation assays, the cultures were incubated for 72 h and were pulsed with [3H]-thymidine (1.0 µCi/10 µl/well) for the last 6 h.
Cytokine assay
Purified CD4+ T cells were cultured with irradiated spleen cells in 96-well flat-bottom plates at a concentration of 1×106 cells/well in 0.2 ml of medium. Cells were stimulated with 50 µg/ml of IRBP. ELISAs for IFN-γ, IL-17 and IL-22 were performed on 72-h supernatants using ELISA kits from eBiosciences or R&D systems, respectively.
PCR
Total RNA was extracted with Trizol (Invitrogen). After reverse-transcription with Omniscript RT Kits (Qiagen), cDNA was amplified by primers for Hes1, 5′- GTGGGTCCTAACGCAGTGTC-3′ and R5′-GTCAGAAGAGAGAGGTGGGCTA-3′; For real-time PCR, after reverse-transcription with Omniscript RT Kits (Qiagen), SYBR premix Ex Taq II (Takara Bio) was used for quantitative PCR. All data were normalized to HPRT (hypoxanthine-guanine phosphoribosyl transferase) and were presented as fold increase relative to the background value. The sequences for primers were as follows: 5′-CACGGCCCTGGTTCTCAT-3′; reverse primer, 5′-CAGATGTTCCACTCTCCTCTTCTCT-3′, Actin, 5′-TGGGAATGGGTCAGAAGGACT-3′ and 5′-TTTCACGGTTGGCCTTAGGGT-3′
Statistical analysis
Student's t-test was performed for statistical analyses.
Results
Rbpj deficiency in T cells suppresses EAU development
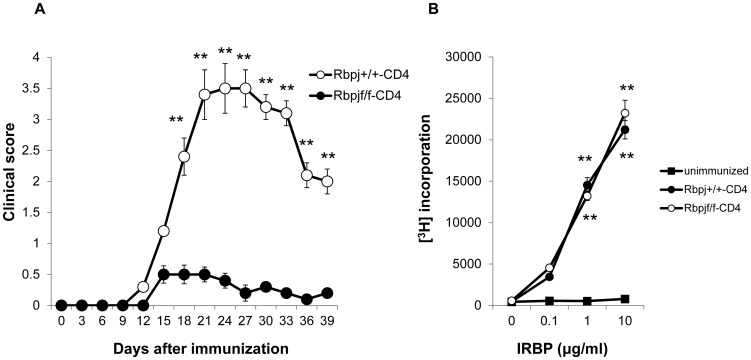
Rbpj is crucial for Notch signaling [21]. In order to evaluate if Notch signaling in T cells is involved in EAU development, we attempted to induce EAU in Rbpj flox/flox mice crossed with CD4-Cre transgenic mice (Rbpjf/f-CD4) that do not express Rbpj in mature CD4+ and CD8+ T cells [12]. Rbpj +/+ mice crossed with CD4-Cre transgenic mice (Rbpj+/+-CD4) were used as controls. These two strains were immunized with interphotoreceptor retinal binding protein (IRBP) using the standard uveitogenic protocol described in the Material and Methods. Rbpjf/f-CD4 mice exhibited lower EAU clinical scores compared to Rbpj+/+-CD4 mice over the course of disease progression (Fig. 1A). To test if the initial priming of T cells is impaired in Rbpjf/f-CD4 mice, CD4+ T cell proliferation was examined seven days after immunization with IRBP. CD4+ T cells from Rbpjf/f-CD4 mice exhibited similar proliferative responses against IRBP to those of Rbpj+/+-CD4 mice (Fig. 1B). These data indicate that deficiency of Rbpj in T cells decreases the susceptibility for EAU and suggest that the initial CD4+ T cell priming or proliferation against IRBP is not affected by Rbpj deficiency.
Figure 1. Rbpj deficiency in T cells ameliorates the induction of EAU.
(A) Rbpjf/f-CD4 and Rbpj+/+-CD4 mice were immunized with IRBP to induce EAU and EAU clinical scores were evaluated until day 39. The data are the mean ± SD with five mice per group. **p<0.01. The score for each mouse was the average for both eyes. (B) Purified CD4+ T cells from Rbpjf/f-CD4 and Rbpj+/+-CD4 mice immunized with IRBP were stimulated with increasing doses of IRBP protein and their proliferative responses to antigen were measured by [3H] thymidine uptake. The results shown are the mean ± SD for triplicate cultures. **p<0.01. The data in this Figure are representative of three independent experiments.
Rbpj deficiency decreases IL-22 production in CD4+ T cells after induction of EAU
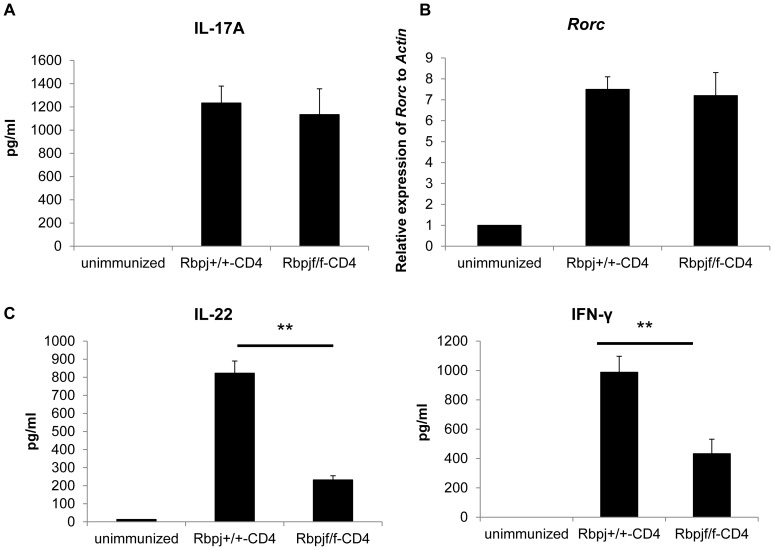
We next examined whether Rbpj affects the differentiation of IL-17- (Th17) producing CD4+ T cells because that T cell population is involved in EAU development [8] [9] [22]. Either Rbpjf/f-CD4 or Rbpj+/+-CD4 mice were immunized with an uveitogenic protocol with IRBP. On day 7, IL-17 production from CD4+ T cells stimulated with IRBP was analyzed by ELISA. IL-17 production was comparable between the 2 groups on day 7 (Fig. 2A). As Th17 differentiation requires the transcription factor Rorc, we investigated the mRNA expression of Rorc in CD4+ T cells from Rbpjf/f-CD4 and Rbpj+/+-CD4 mice 7 days after IRBP immunization. We found that the mRNA expression of Rorc is comparable between CD4+ T cells from Rbpjf/f-CD4 and Rbpj+/+-CD4 mice (Fig. 2B). These data suggest that Th17 differentiation is not affected by Rbpj deficiency in T cells at least 7 days after IRBP immunization.
Figure 2. Rbpj deficiency in T cells reduces of IL-22 production.
Rbpjf/f-CD4 and Rbpj+/+-CD4 mice were immunized with IRBP and CD4+ T cells were purified from draining lymph nodes 7 days after immunization. Purified CD4+ T cells were cultured with irradiated spleen cells from B6 mice in the presence of IRBP protein (50 µg/ml) for 3 days. (A) IL-17 in culture supernatants was evaluated by ELISA. (B) mRNA was purified from CD4+ T cells 7 days after immunization and the relative levels of Rorc against Actin were evaluated by real-time PCR. (C) IL-22 and IFN-γ in culture supernatants 72 hours after stimulation of purified CD4+ T cells from Rbpjf/f-CD4 and Rbpj+/+-CD4 mice immunized with IRBP (7 days previously) was evaluated by ELISA. The data are the mean ± SD from triplicate cultures. **p<0.01. The data in this Figure are representative of three independent experiments.
As we have previously reported that Rbpj deficiency in T cells reduces IL-22 production from T cells [23], we investigated the production of IL-22 in CD4+ T cells from Rbpjf/f-CD4 mice 7 days after immunization by IRBP. IL-22 production by CD4+ T cells from Rbpjf/f-CD4 mice was much less than from control mice (Fig. 2C). The INF-γ production was also impaired by Rbpj deficiency (Fig. 2C). These data demonstrate that Rbpj is required for the production of IL-22 from CD4+ T cells while not affecting the differentiation of Th17 cells in the EAU model.
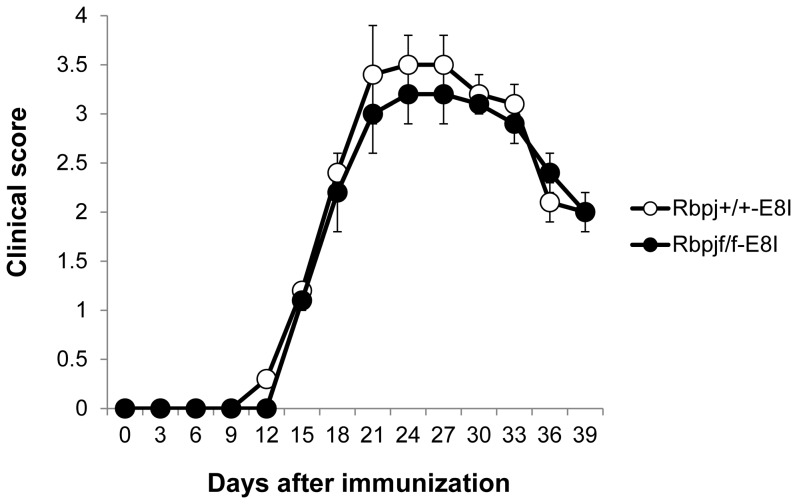
Notch signaling in CD8+ T cells is not involved in the susceptibility for EAU
Rbpjf/f-CD4 mice lack Rbpj in both mature CD4+ and CD8+ T cells. Although previous studies have not revealed a clear contribution of CD8+ T cells to EAU progression [24], we investigated whether Rbpj deficiency in only mature CD8+ T cells impacts EAU susceptibility. Rbpj flox/flox mice were crossed with E8I-Cre transgenic mice (Rbpjf/f-E8I) in which Rbpj is deleted in mature CD8+ but not CD4+ T cells [20]. Rbpjf/f-E8I and Rbpj+/+-E8I mice were immunized with IRBP and EAU development was monitored. We observed that Rbpjf/f-E8I mice developed EAU similar to controls over the course of the disease (Fig. 3). Therefore, Rbpj in mature CD8+ T cells does not play a major role in the development of EAU.
Figure 3. Rbpj deficiency in CD8+ T cells does not alter EAU susceptibility.
Rbpjf/f-E8I and Rbpj+/+-E8I mice were immunized with IRBP to induce EAU and EAU clinical scores were evaluated until day 39. The data are the mean ± SD with five mice per group. The score for each mouse was the average for both eyes. The data in this Figure are representative of three independent experiments.
IL-22 contributes to the progression of EAU
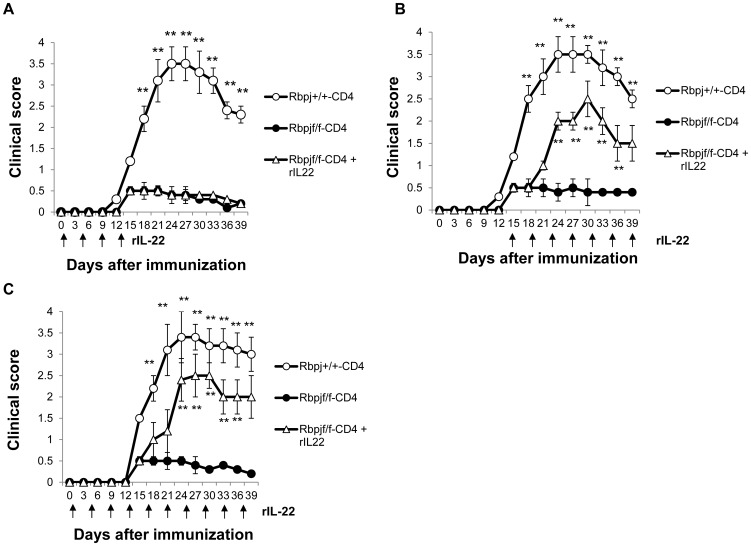
We next sought to investigate if IL-22 is involved in the progression of EAU. Recombinant IL-22 (rIL-22) was administered to Rbpjf/f-CD4 mice that had been immunized with IRBP at 3-day intervals beginning one day after IRBP immunization and ceased 13 days after immunization, beginning 14 days after immunization and continued throughout the course of the experiment, or beginning one day after IRBP immunization and continued over the course of the experiment. The administration of rIL-22 during the early phase of EAU in Rbpjf/f-CD4 mice did not change the clinical scores of EAU compared to that of Rbpj+/+-CD4 mice (Fig. 4A). In contrast, the administration of rIL-22 during the late phase of EAU aggravated EAU clinical scores (Fig. 4B), with measurable differences being observed 6 days after the initial rIL-22 administration. The rIL-22 administration during the late phase of EAU did not cause chronic EAU because mice that received rIL-22 recovered from EAU at day 60 (data not shown). The administration of rIL-22 over the course of EAU also aggravated EAU clinical scores, although it still did not reach the scores of Rbpj+/+-CD4 mice (Fig. 4C). These data demonstrate that Notch-mediated IL-22 from T cells is crucial for the development of late phase EAU progression, rather than the early phase.
Figure 4. IL-22 is involved in the progression of late-phase EAU.
Rbpjf/f-CD4 and Rbpj+/+-CD4 mice were immunized with IRBP to induce EAU and EAU clinical scores were evaluated until day 39. rIL-22 was administered to the mice according to the following schedules; the day of IRBP immunization is day 0. (A) 3-day intervals (from day 1 to day 13), (B) 3-day intervals (from day 14 to day 39), (C) 3-day intervals (from day 1 to day 39). The data are the mean ± SD with five mice per group. **p<0.01. The data in this Figure are representative of three independent experiments.
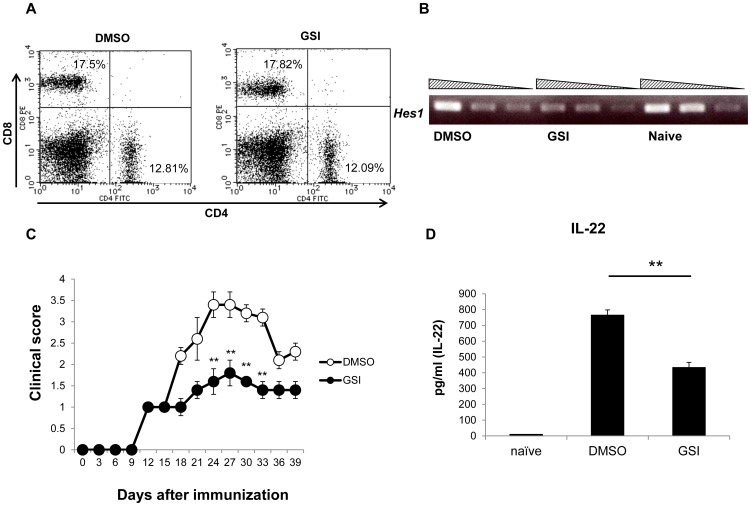
Treatment with GSI during later disease stages inhibited EAU
We next examined if a γ-secretase inhibitor that blocks Notch signaling is able to suppress EAU in order to evaluate the potential of Notch modulation as a therapy for EAU. GSI was administered intraperitoneally daily from day 12 to day 18. GSI treatment did not change any mouse activity at a glance or body weight (data not shown), nor did it affect the ratio of CD4+ and CD8+ T cells (Fig. 5A). GSI treatment reduced the expression of Hes1, one of the Notch target genes, compared to the control, indicating that this dose of GSI could inhibit Notch signaling in vivo (Fig. 5B). GSI treatment significantly decreased disease progression compared with the control DMSO-treated group (Fig. 5C). CD4+ T cells from GSI-treated mice produced lower levels of IL-22 than those from DMSO-treated mice (Fig. 5D). These results indicate that inhibition of Notch signaling by GSI could suppress late-stage EAU.
Figure 5. GSI treatment is useful to treat EAU.
B6 mice were immunized with IRBP to induce EAU and EAU clinical scores were evaluated until day 39. GSI was administered to the mice according to the following schedules; the day of IRBP immunization is day 0. 2-day intervals (from day 13 to day 39). (A) CD4 and CD8 expression in the draining lymph nodes at day 14 were evaluated by flow cytometry. (B) CD4+ T cells were purified from draining lymph nodes of mice that received GSI or DMSO 1 day before and expression of Hes1 was evaluated by PCR (from left to right; 100 ng, 10 ng, 1 ng of mRNA). (C) EAU clinical scores, (D) CD4+ T cells were purified from draining lymph nodes on day 12. Purified CD4+ T cells were cultured with irradiated spleen cells from B6 mice in the presence of IRBP protein (50 µg/ml) for 3 days. IL-22 in culture supernatants was evaluated by ELISA. The data are the mean ± SD of triplicate cultures. **p<0.01. The data in this Figure are representative of three independent experiments.
Discussion
The present study aimed to investigate the role of Notch signaling in the development of EAU. Rbpj deficiency in T cells impaired EAU development by inhibiting IL-22 production from CD4+ T cells without affecting IRBP-specific T cell proliferation or Th17 differentiation. IL-22 acted as an inflammatory cytokine during the late phase but not the early phase of EAU progression. The inhibition of Notch signaling by GSI even after EAU was established suppressed EAU clinical scores. These data suggest that the Notch-Rbpj axis regulates the production of IL-22 from CD4+ T cells, which is associated with the progression of EAU development.
Previous research has demonstrated that Notch signaling controls the functional differentiation of CD4+ T cells [11] [12] [13] [14] [23] [15]. Consistent with our previous study [23], IL-22 production from CD4+ T cells after immunizing T cell-specific Rbpj-deficient mice with IRBP was impaired, which was associated with enhanced EAU susceptibility. IL-22 is an IL-10 family cytokine that has pleiotropic roles in inflammatory responses, depending on the disease context [25] [26] [23] [27]. For instance, IL-22 has protective roles in ConA-induced hepatitis [26] [23]. In contrast, IL-22 regulates the development of the skin inflammation pathology seen in psoriasis [27]. The present study showed that administration of rIL-22 during the late phase aggravated EAU in Rbpjf/f-CD4 mice, while clinical scores were unaffected when rIL-22 was administered only during the early phase. These data suggest that Notch-mediated IL-22 production has a pathological role only during the late stage of EAU, although we cannot exclude the possibility that the amount of rIL-22 during the early phase is not enough to impact EAU susceptibility. This finding raises the questions of how IL-22 contributes to late-phase EAU pathology without affecting the initial T cell proliferation. A previous report suggested that primary human keratinocytes exposed to IL-22-producing cells expressed a variety of genes involved in innate immune pathways and the induction and modulation of adaptive immunity [28]. These findings suggest that IL-22 may act as a direct inducer for aggravating EAU pathology by interacting with various cells. The second possibility is that IL-22 may have a suppressive effect on the immune inhibitory functions of immune or non-immune cells that are relevant to EAU pathology. In addition, it should be noted that the clinical scores of T cell-specific Rbpj deficient mice that received rIL-22 over the course of EAU could not reach those of control mice, suggesting that Notch signaling in T cells has IL-22 independent pathological roles in the progression of EAU.
A previous study revealed that mice treated with IL-22 generated decreased numbers of IFN-γ+ and IL-17+ uveitogenic T cells with increased numbers of Foxp3+ regulatory T cells, which are induced by CD11b+ antigen-presenting cells [29]. This study revealed that rIL-22 treatment attenuates EAU. The discrepancy over the roles of IL-22 in EAU between this study and our present study might be due to the distinct mouse strain used for EAU induction because the past study used B10RIII mice and we used B6 mice. The difference of mouse strain might be attributable to the distinct responses to rIL-22 or a differential requirement of IL-22 for inflammatory responses. Another possibility is the distinct schedule of rIL-22 treatment, because IL-22 has proinflammatory roles or anti-inflammatory roles in different disease contexts [27] [26] [23], which suggests that the roles of IL-22 or the required amount of IL-22 for inhibiting or promoting inflammation might be different during the course of EAU.
It is noteworthy that treatment of EAU with GSI could significantly suppress EAU clinical scores. This treatment with GSI also reduced the production of IL-22, and the suppression of EAU by GSI was reverted by administrating rIL-22 (data not shown). Although Rbpj interacts with p53 [30] and Rbpj-independent Notch signaling was reported [31] [32], these data strongly suggest that Rbpj-Notch pathway is involved in EAU development. These data also suggest that Notch blockade would be useful in treating autoimmune uveitis. However, Notch signaling is crucial for regulating non-immune cells in addition to immune cells. Therefore, it is necessary to determine the concentration of GSI for exerting positive drug effects while avoiding negative side effects. In addition, GSI is not a specific inhibitor of Notch because many other molecules use γ-secretase for signaling. Therefore, we cannot fully exclude the possibility that GSI treatment is also involved in the suppression of a Notch-independent pathway in our study, which might have some role in the suppression of EAU.
In conclusion, the idea that Notch-mediated IL-22 is involved in the progression of late-phase EAU development supports our hypothesis that Notch blockade might be useful as a therapeutic strategy for treating EAU. Indeed, our data in the mouse EAU model indicate that GSI treatment could attenuate EAU even after IRBP immunization. These results highlight the potential usefulness of Notch blockade as a therapy for autoimmune uveitis. Finally, even though EAU progression was prevented by Notch blockade, the question remains of whether memory T cells that differentiate into IL-22-producing T cells would also be blocked under these conditions. Since memory T cells are already present in human ongoing autoimmune uveitis, this situation will also need to be taken into account in clinical settings, and this issue should be analyzed in future studies.
Acknowledgments
We thank Mrs. Kinouchi and Mrs. Tomari for their editorial and technical assistance.
Funding Statement
This work was supported by a Grant-in-Aid for Young Scientists (S) from the Japan Society for the Promotion of Science. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Caspi RR (2003) Regulation, counter-regulation, and immunotherapy of autoimmune responses to immunologically privileged retinal antigens. Immunologic research 27: 149–160. [DOI] [PubMed] [Google Scholar]
- 2. Sonoda KH, Sasa Y, Qiao H, Tsutsumi C, Hisatomi T, et al. (2003) Immunoregulatory role of ocular macrophages: the macrophages produce RANTES to suppress experimental autoimmune uveitis. J Immunol 171: 2652–2659. [DOI] [PubMed] [Google Scholar]
- 3. Kitamura M, Iwabuchi K, Kitaichi N, Kon S, Kitamei H, et al. (2007) Osteopontin aggravates experimental autoimmune uveoretinitis in mice. J Immunol 178: 6567–6572. [DOI] [PubMed] [Google Scholar]
- 4. Caspi R (2008) Autoimmunity in the immune privileged eye: pathogenic and regulatory T cells. Immunologic research 42: 41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shao H, Liao T, Ke Y, Shi H, Kaplan HJ, et al. (2006) Severe chronic experimental autoimmune uveitis (EAU) of the C57BL/6 mouse induced by adoptive transfer of IRBP1-20-specific T cells. Experimental eye research 82: 323–331. [DOI] [PubMed] [Google Scholar]
- 6. Tarrant TK, Silver PB, Wahlsten JL, Rizzo LV, Chan CC, et al. (1999) Interleukin 12 protects from a T helper type 1-mediated autoimmune disease, experimental autoimmune uveitis, through a mechanism involving interferon gamma, nitric oxide, and apoptosis. The Journal of experimental medicine 189: 219–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Caspi RR, Silver PB, Chan CC, Sun B, Agarwal RK, et al. (1996) Genetic susceptibility to experimental autoimmune uveoretinitis in the rat is associated with an elevated Th1 response. Journal of immunology 157: 2668–2675. [PubMed] [Google Scholar]
- 8. Luger D, Silver PB, Tang J, Cua D, Chen Z, et al. (2008) Either a Th17 or a Th1 effector response can drive autoimmunity: conditions of disease induction affect dominant effector category. The Journal of experimental medicine 205: 799–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yoshimura T, Sonoda KH, Miyazaki Y, Iwakura Y, Ishibashi T, et al. (2008) Differential roles for IFN-gamma and IL-17 in experimental autoimmune uveoretinitis. International immunology 20: 209–214. [DOI] [PubMed] [Google Scholar]
- 10. Radtke F, Raj K (2003) The role of Notch in tumorigenesis: oncogene or tumour suppressor? Nat Rev Cancer 3: 756–767. [DOI] [PubMed] [Google Scholar]
- 11. Maekawa Y, Tsukumo S, Chiba S, Hirai H, Hayashi Y, et al. (2003) Delta1-Notch3 interactions bias the functional differentiation of activated CD4+ T cells. Immunity 19: 549–559. [DOI] [PubMed] [Google Scholar]
- 12. Tanigaki K, Tsuji M, Yamamoto N, Han H, Tsukada J, et al. (2004) Regulation of alphabeta/gammadelta T cell lineage commitment and peripheral T cell responses by Notch/RBP-J signaling. Immunity 20: 611–622. [DOI] [PubMed] [Google Scholar]
- 13. Amsen D, Blander JM, Lee GR, Tanigaki K, Honjo T, et al. (2004) Instruction of distinct CD4 T helper cell fates by different notch ligands on antigen-presenting cells. Cell 117: 515–526. [DOI] [PubMed] [Google Scholar]
- 14. Tanaka S, Tsukada J, Suzuki W, Hayashi K, Tanigaki K, et al. (2006) The interleukin-4 enhancer CNS-2 is regulated by Notch signals and controls initial expression in NKT cells and memory-type CD4 T cells. Immunity 24: 689–701. [DOI] [PubMed] [Google Scholar]
- 15. Bailis W, Yashiro-Ohtani Y, Fang TC, Hatton RD, Weaver CT, et al. (2013) Notch simultaneously orchestrates multiple helper T cell programs independently of cytokine signals. Immunity 39: 148–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Minter LM, Turley DM, Das P, Shin HM, Joshi I, et al. (2005) Inhibitors of gamma-secretase block in vivo and in vitro T helper type 1 polarization by preventing Notch upregulation of Tbx21. Nature immunology 6: 680–688. [PubMed] [Google Scholar]
- 17. Reynolds ND, Lukacs NW, Long N, Karpus WJ (2011) Delta-like ligand 4 regulates central nervous system T cell accumulation during experimental autoimmune encephalomyelitis. Journal of immunology 187: 2803–2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bassil R, Zhu B, Lahoud Y, Riella LV, Yagita H, et al. (2011) Notch ligand delta-like 4 blockade alleviates experimental autoimmune encephalomyelitis by promoting regulatory T cell development. Journal of immunology 187: 2322–2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ishida W, Fukuda K, Sakamoto S, Koyama N, Koyanagi A, et al. (2011) Regulation of experimental autoimmune uveoretinitis by anti-delta-like ligand 4 monoclonal antibody. Investigative ophthalmology & visual science 52: 8224–8230. [DOI] [PubMed] [Google Scholar]
- 20. Maekawa Y, Minato Y, Ishifune C, Kurihara T, Kitamura A, et al. (2008) Notch2 integrates signaling by the transcription factors RBP-J and CREB1 to promote T cell cytotoxicity. Nature immunology 9: 1140–1147. [DOI] [PubMed] [Google Scholar]
- 21. Radtke F, Wilson A, Mancini SJ, MacDonald HR (2004) Notch regulation of lymphocyte development and function. Nature immunology 5: 247–253. [DOI] [PubMed] [Google Scholar]
- 22. Amadi-Obi A, Yu CR, Liu X, Mahdi RM, Clarke GL, et al. (2007) TH17 cells contribute to uveitis and scleritis and are expanded by IL-2 and inhibited by IL-27/STAT1. Nat Med 13: 711–718. [DOI] [PubMed] [Google Scholar]
- 23. Alam MS, Maekawa Y, Kitamura A, Tanigaki K, Yoshimoto T, et al. (2010) Notch signaling drives IL-22 secretion in CD4+ T cells by stimulating the aryl hydrocarbon receptor. Proc Natl Acad Sci U S A 107: 5943–5948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Calder VL, Zhao ZS, Wang Y, Barton K, Lightman SL (1993) Effects of CD8 depletion on retinal soluble antigen induced experimental autoimmune uveoretinitis. Immunology 79: 255–262. [PMC free article] [PubMed] [Google Scholar]
- 25. Kolls JK, McCray PB Jr, Chan YR (2008) Cytokine-mediated regulation of antimicrobial proteins. Nat Rev Immunol 8: 829–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zenewicz LA, Yancopoulos GD, Valenzuela DM, Murphy AJ, Karow M, et al. (2007) Interleukin-22 but not interleukin-17 provides protection to hepatocytes during acute liver inflammation. Immunity 27: 647–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ma HL, Liang S, Li J, Napierata L, Brown T, et al. (2008) IL-22 is required for Th17 cell-mediated pathology in a mouse model of psoriasis-like skin inflammation. The Journal of clinical investigation 118: 597–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Eyerich S, Eyerich K, Pennino D, Carbone T, Nasorri F, et al. (2009) Th22 cells represent a distinct human T cell subset involved in epidermal immunity and remodeling. The Journal of clinical investigation 119: 3573–3585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ke Y, Sun D, Jiang G, Kaplan HJ, Shao H (2011) IL-22-induced regulatory CD11b+ APCs suppress experimental autoimmune uveitis. Journal of immunology 187: 2130–2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Boggs K, Henderson B, Reisman D (2009) RBP-Jkappa binds to and represses transcription of the p53 tumor suppressor gene. Cell Biol Int 33: 318–324. [DOI] [PubMed] [Google Scholar]
- 31. Jin S, Mutvei AP, Chivukula IV, Andersson ER, Ramskold D, et al. (2013) Non-canonical Notch signaling activates IL-6/JAK/STAT signaling in breast tumor cells and is controlled by p53 and IKKalpha/IKKbeta. Oncogene 32: 4892–4902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Andersen P, Uosaki H, Shenje LT, Kwon C (2012) Non-canonical Notch signaling: emerging role and mechanism. Trends Cell Biol 22: 257–265. [DOI] [PMC free article] [PubMed] [Google Scholar]