Abstract
This prospective double blind randomized study evaluated the effect of clonidine when used as an adjuvant to local anaesthetic agents for infiltration block and measured its impact on the quality of anaesthesia, intraoperative bleeding and post-operative pain. We recruited 60 patients needing tympanoplasty, which were randomized them into two groups; group A patients received local infiltration of 12 ml 2 % xylocaine with adrenaline (1:200,000 dilution), while group B received 12 ml 2 % xylocaine with adrenaline with 30 μg of clonidine. Duration of block was significantly prolonged in group B (group A 53.66 ± 7.7 vs. group B 177.13 ± 48.9, p < 0.005). Mean pain scores were significantly lower in group B during the first hour following the block (3.43 in group A vs. 1.2 in group B, p < 0.005). Total number of analgesic doses over 24 h showed no significant difference (3.1 in group B vs. 3.26 in group A, p > 0.05). 93.3 % patients in group A required sedation with midazolam, compared to 10 % in group B. Grade of bleeding was significantly lower in group B. Patient and surgeon satisfaction scores were better in group B. It could be concluded that 30 μg clonidine added to lidocaine 2 % has a significant impact in decreasing the bleeding in the operative field and improving the quality of intraoperative anesthesia as well as prolonging the duration of postoperative analgesia without significant side effects.
Keywords: Lidocaine 2 % with adrenaline, Tympanoplasty, Local infiltration, Clonidine
Introduction
An ideal anaesthetic technique for middle ear surgeries should be such as to produce adequate analgesia for the surgical procedure, maximize patient comfort, reduce intraoperative bleeding as well as provide good pain relief and minimize nausea and vomiting postoperatively. Comparative merits and demerits of general versus local anesthesia in these surgeries have been debated [1]. General anesthesia is a more expensive option, associated with increased postoperative nausea and vomiting and hypotensive technique has to be ensured to minimize intraoperative bleeding. Also coughing or straining during extubation can dislodge the implanted graft. Hospital stay and consequently expenditure is also increased in general anesthesia patients. These complications could largely be easily avoided by use of local anesthesia in middle ear surgeries.
Many of the patients coming to our hospital are from far off places, which is a tertiary level referral centre. Day care surgery under local anesthesia is the preferred option for them as it implies rapid recovery, less expenditure, less hospital stay and thus minimum loss of their daily work. However, endomeatal and post auricular infiltration anesthesia with local anaesthetic is often inadequate in terms of ensuring adequate patient compliance for the procedure. Patients may complain of discomfort and intense pain specially during annulus lifting. In these cases local anesthesia has to be supplemented with intravenous anaesthetic agents to ensure the smooth completion of the surgery. Sedation has to be adequately titrated since airway access becomes a problem in the event of an emergency. In the postoperative period too, patients might complain of intense pain requiring multiple analgesic doses.
The addition of adjuvants like clonidine to improve the quality and duration of anesthetic blocks has been an established technique. Clonidine is a mixed α 1 and α 2 adrenoreceptor agonist with predominant α 2 activity, long used as an antihypertensive agent. By causing sympatholysis, it reduces peripheral norepinephrine release due to stimulation of the prejunctional α 2 adrenoreceptors [2]. It has been found to decrease anaesthetic and analgesic drug requirements when given systematically [3]. Apart from this its use as an adjuvant to nerve blocks has been documented [4, 5] but to date there is no literature citing its use in infiltrative blocks for middle ear surgeries like tympanoplasty.
The present study aimed to evaluate the effect of adding 30 μg of clonidine to the local anesthetic during infiltrative nerve block for tympanoplasty and assessed the patients in terms of quality of anaesthesia, intraoperative bleeding and postoperative pain.
Methodology
The study was done between April 2012 and March 2013. Written informed consent was taken from 60 patients (age 15–61 years) of American society of anaesthesiologists (ASA) grade 1 and 2, diagnosed to have chronic suppurative otitis media with dry central perforation scheduled for tympanoplasty. Exclusion criteria were patients needing mastoid exploration, revision ear surgeries, coagulation disorders or with local infection at the site of block.
Patients were allocated by envelop randomization to receive either 10 ml solution of xylocaine with adrenaline (LOX* 2 % with adrenaline 1:200,000, Neon Laboratories) with 2 ml normal saline (group A or control group), or 10 ml local anaesthetic with 30 μg clonidine hydrochloride (Cloneon*, Neon Laboratories) (group B or study group). Randomization and preparation of drug was done by a trained assistant not involved in data collection and surgery. The patients and investigators were unaware of which solution would be injected.
Standard fasting guidelines were followed. Preoperatively intravenous ranitidine 50 mg was administered after setting up an intravenous line. Routine patient monitoring was done with ECG, oxygen saturation and non-invasive blood pressure monitoring (Schillers Truscope II Monitor). Baseline haemodynamic parameters were noted, followed by those after giving the block, start of surgery and every 10 min subsequently.
After preparing the part, post auricular and endomeatal block was given by the surgeon with the above prepared solutions. Since no clear end point to injection has been described, we chose a standardized technique of infiltration administered by a same surgeon which would provide reliable distribution of local anaesthetic and eliminate operator bias. Block was considered to be effective if patient did not respond to painful stimulus at the surgical site following which surgery was started. Patients were given oxygen through ventimask but no sedation or analgesia was given, unless the patient was uncooperative or complained of pain thus hampering the surgery. In such cases midazolam (0.02–0.04 mg/kg IV) was given in doses necessary to ensure patient compliance. If patient was still not comfortable then injection diclofenac sodium 75 mg was given intravenously. Time to onset of analgesia, its duration and degree of bleeding in the surgical field was assessed. Onset of analgesia was tested as loss of sensation to pinprick in the retro auricular area. Total duration of analgesia was taken to be from the institution of the block to time of first analgesic dose. Duration of surgery was defined as the period between time of incision to the time of last suture. Intraoperative bleeding was evaluated on a five point grading system [6] (Table 1).
Table 1.
Grading system for bleeding in surgical field
| Grades | Surgical field |
|---|---|
| I | Cadaveric conditions with minimum suction required |
| II | Minimal bleeding with infrequent suction required |
| III | Brisk bleeding with frequent suction required |
| IV | Bleeding covers surgical field after removal of suction before surgical instrument can perform manoeuvre |
| V | Uncontrolled bleeding |
After the operation patients were observed for a 24 h period. Analgesia was assessed using a standard 10 point visual analogue scale (VAS). This pain score was explained to the patients preoperatively by the anaesthetist, and was assessed by a trained staff nurse who was unaware of the drug being given. The mean pain scores were calculated in the 1st, 2nd, 3rd, and 4th, 6th and 24 h in the postoperative period. Analgesic was given if pain score was 3 or more period and total analgesic demand was recorded. Side effects like hypotension, bradycardia, sedation and incidence of postoperative nausea and vomiting was noted. PONV free patients were defined as those who had no nausea or vomiting and were not given antiemetic drugs.
Patients were asked to rate the perioperative experience in terms of pain and nausea and vomiting as 1 = poor, 2 = good, 3 = excellent. Surgeon satisfaction scores were assessed in terms of surgical conditions and patient compliance and graded as 1 = poor, 2 = good, 3 = excellent.
Demographic data and perioperative details are summarized as mean ± SD. Bleeding grades are expressed as percentages. Statistical analysis for significance was done using two sample unpaired t test. Pain scores were analysed using Mann–Whitney Rank Sum test. p < 0.05 was considered as significant and p < 0.005 was considered as highly significant. Chi square test and Fischer exact test were applied as applicable.
Results
The demographic data and duration of surgery were comparable in both the groups (p > 0.05) (Table 2). Block characteristics analysis showed no difference in the time of onset of block, but a highly significant difference was observed in duration of block (group A 53.66 ± 7.7 vs. group B 177.13 ± 48.9, p < 0.005) between the two groups (Table 3).
Table 2.
Demographic data
| Variables | Group A (n = 30) | Group B (n = 30) |
|---|---|---|
| Age (year) | 32.9 ± 12.3 | 34 ± 12 |
| Weight (kg) | 55.8 ± 8.7 | 56.9 ± 8.6 |
| Sex (M/F) | 19/11 | 16/14 |
| Duration of surgery (min) | 69.16 ± 12.5 | 66.5 ± 11.41 |
| ASA PS (1/2)a | 12/3 | 13/2 |
Values are expressed as mean ± SD
aASA = American Society of Anaesthesiologist Grade 1 & 2
Table 3.
Intraoperative parameters
| Variable | Group A (n = 30) | Group B (n = 30) | p value (t test) |
|---|---|---|---|
| Onset of analgesia (s) | 94 ± 13.7 | 93.5 ± 14.3 | 0.893 |
| Total duration of analgesia (min) | 53.66 ± 7.7 | 177.13 ± 48.90 | <0.0005 |
| Sedation/analgesia (number) | 30/26 | 3/0 | |
| Grade 2 bleeding | 12 (40 %) | 21 (70 %) | |
| Grade 3 bleeding | 18 (60 %) | 9 (30 %) |
Data as mean ± SD
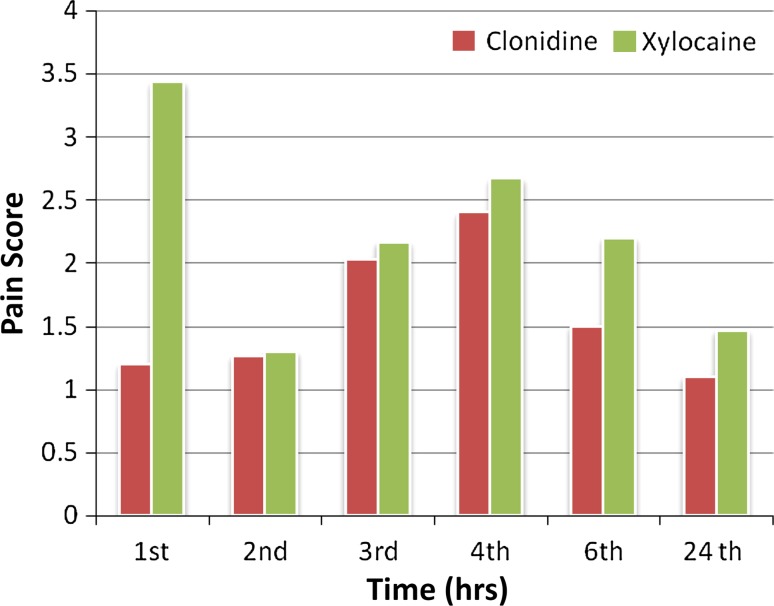
Analysis of pain scores reflected a significantly lower mean pain score in group B during the first hour following the block (1.2 in group B vs. 3.43 in group A, p < 0.005). During subsequent hours although mean pain scores remained lower in clonidine group, the difference in both groups was not significant statistically. In terms of number of total number of analgesic doses over 24 h also, no significant difference was observed between the groups (3.1 in group B vs. 3.26 in group A, p > 0.05).
A significant correlation was observed between type of drug used in the block and the requirement for sedation intraoperatively. In group A, sedation with intravenous midazolam (0.02–0.04 mg/ml) had to be given to 28/30 (93.33 %) patients. Analgesia with intravenous diclofenac was given to 26 patients at the time of annulus lifting. In group B sedation with IV midazolam had to be given to 3/30 patients. No other drug was required.
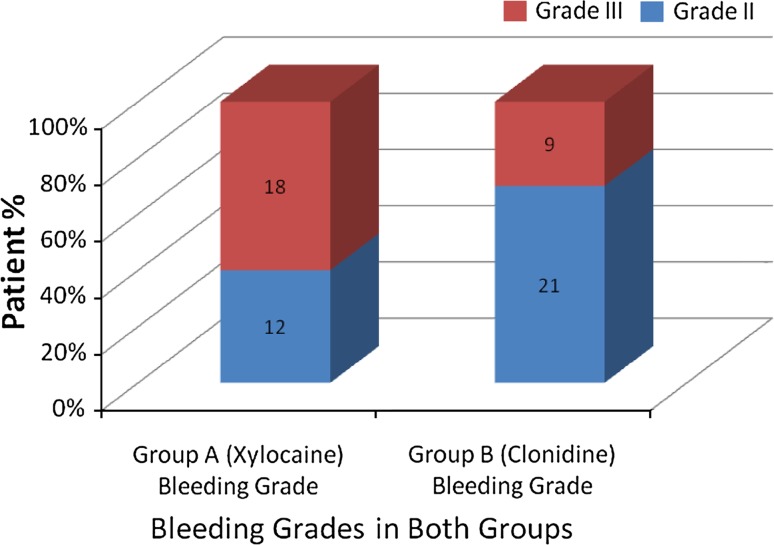
It was observed that when compared to group A, patients in group B had a lower bleeding grade. Only 30 % patients in group B had grade 3 bleeding compared to group A in which 60 % had grade 3 bleed (Fig. 1).
Fig. 1.
Bleeding in group A and B
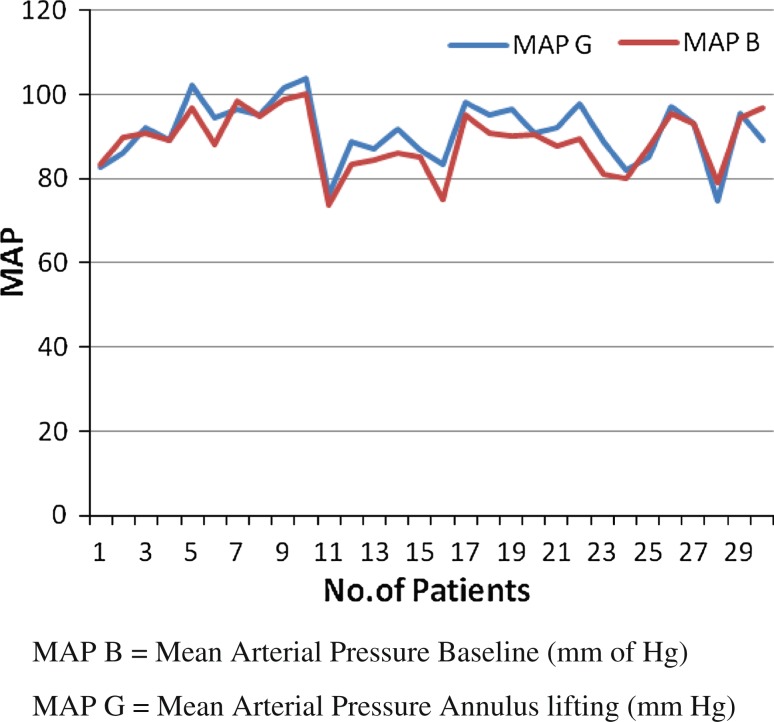
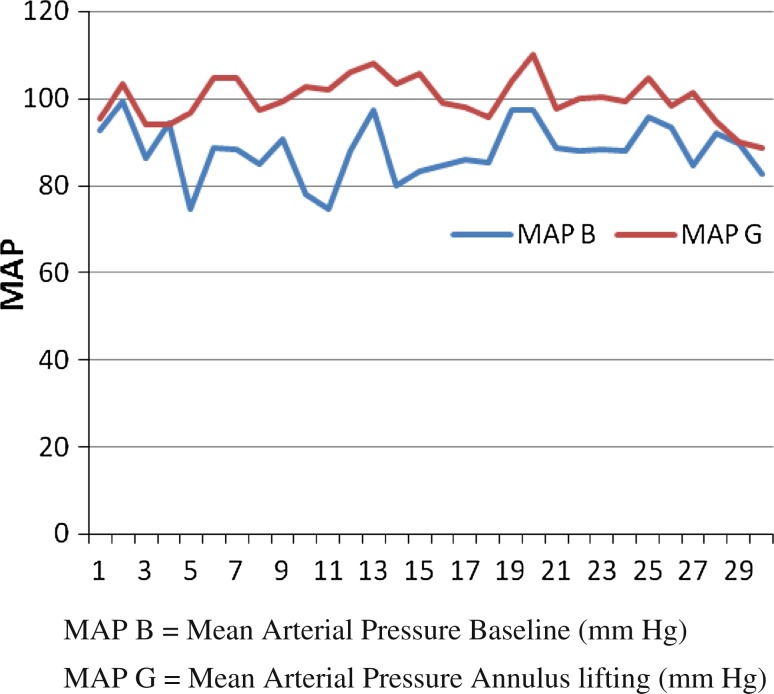
Haemodynamically, baseline mean blood pressure (MAP) and pulse rate between the two groups was comparable before surgery (p < 0.05). A higher rise in was noted in group A than group B when compared to base line at 10 and 20 min, but difference was not statistically significant. At the time of annulus lifting, patients in group B showed insignificant change in mean arterial pressure and pulse rate compared to baseline values, (p > 0.05) (Fig. 2) while patients in group A showed a significant rise in these parameters compared to baseline values (p < 0.05). Subsequently no difference was observed in the recovery unit as well as surgical ward over next 24 h. Bradycardia (heart rate = <40/min) was observed in 2 patients intraoperatively in group B, which was managed with inj. atropine 0.6 mg intravenously, and patient responded appropriately.
Fig. 2.
MAP in clonidine group: baseline (B) and annulus lifting (G)
Incidence of nausea and vomiting was higher in group A patients 0.17 patients remained post-operative nausea and vomiting (PONV) free in group A compared to 26 patients in group B in the first 6 h. After this, the number of patients who remained PONV free was still lower in group A, but no statistical significance could be detected. No other adverse event was observed in any patient (Table 4).
Table 4.
Postoperative nausea and vomiting
| Variable | Group A | Group B | p value (χ2) |
|---|---|---|---|
| Recovery unit (6 h) | |||
| NVF | 17 | 26 | 0.022 |
| Nausea | 13 | 4 | 0.022 |
| Vomiting | 6 | 0 | 0.065* |
| Surgical unit (24 h) | |||
| NVF | 18 | 20 | 0.789 |
| Nausea | 12 | 10 | 0.908 |
| Vomiting | 5 | 3 | 0.773 |
NVF nausea vomiting free
* Fischer’s exact test
Higher number of patients in group B rated their perioperative experience (quality of analgesia, PONV) as good (18/30) or excellent (9/30). Patients in group A rated their experience as poor (20/30) or good (8/30). Surgeon satisfaction was also higher in group B patients: excellent (19/30), good (7/30) and poor (4/30). In group A the ratings were excellent (6/30), good (16/30) and poor (9/30) (Figs. 3, 4).
Fig. 3.
MAP in xylocaine group: baseline (B) and annulus lifting (G)
Fig. 4.
Mean pain scores of group A and B
Discussion
We chose to study the role of clonidine in infiltration block techniques since literature is scarce regarding the effect of this drug when added to local anaesthetics in this technique. Studies demonstrating the beneficial effects of clonidine in extending the motor and sensory components of central [7] and peripheral nerve blocks have been published [8, 9]. The beneficial effect of clonidine in extending the duration of peripheral nerve blocks is believed to be a locally mediated effect, which is not reproduced by systemically administered clonidine [8]. Its synergistic action with lignocaine in prolonging the duration of peripheral nerve blocks has been attributed to an enhancing effect on lignocaine induced inhibition of the C-fibre action potential [10].
The use of clonidine as an adjuvant to wound infiltration with local anaesthetics prior to elective hernia surgery has been cited in literature [11]. Doses up to 150 μg added to 0.5 % bupivacaine for wound infiltration did not reveal any improvement in duration of postoperative analgesia, though initial pain scores in the postoperative period were seen to be better in these patients.
There are speculations about whether the theory of a synergistic action of clonidine and local anaesthetics also applies to the periphery, as it does in the case of major nerves. Singelyn et al. [9] have stated that clonidine has no effect on the absorption of amide local anaesthetics from their site of action, differentiating its mechanism of action from adrenaline which acts as a local vasoconstrictor, leading to delayed absorption and prolonged action of local anaesthetics. Although clonidine might have a vasoconstrictive effect in large concentrations, the role of vasoconstriction in prolonging sensory block seems to be minor, even in usual clinical doses (1–2 μg/kg) [12].
In a study done on 20 volunteers by Pratap et al. [13] infiltration of 10 μg of clonidine with lidocaine abolished normal sensation at the site for up till 6 h, compared with plain lidocaine. The authors support the view that there is the existence of a peripheral site of action of clonidine in prolonging local anaesthetic action in humans, independent of any neuraxial or systemic mechanisms.
In our study though improved pain scores were present in the first 6 h post block in clonidine group a statistically significant difference was observed only in the first hour. This difference was not observed in the subsequent hours probably because analgesia and sedation had then been administered to the patients, which reduced their pain scores. The definition of duration of block in our study (infiltration to first rescue analgesic) necessitated that our data be studied accordingly. Almost all patients in group A had to be given analgesia at the time of annulus lifting. In the clonidine group however, the procedure was tolerated extremely well and analgesic dose was administered postoperatively. This explains the highly significant difference in the mean duration of action of blocks in both groups. Since pain parameters were not confounded by administration of general anaesthesia or other analgesics in the intraoperative period, we attribute this prolongation of action to clonidine.
We started our observation period in the 1st intraoperative hour since surgery was conducted under the same block and continued it till patient discharge 24 h postoperatively. We thus observed the impact of clonidine on immediate pain scores and patient compliance, as well as its effect on duration of analgesia without any compounding factors like general anaesthesia affecting it. As the patients had been thoroughly explained the pain score with a request for cooperation intraoperatively, we did not experience great difficulty in recording pain scores intraoperatively. We used 30 μg clonidine which when calculated in context with the demographic profile of our patients works out to be between 0.5 and 1 μg/kg body weight. During single dose peripheral nerve block with short or medium acting local anaesthetic, the minimum dose of clonidine to significantly prolong the duration of both anaesthesia and analgesia is 0.5 μg/kg in previous studies [9]. At this dose it has been found to be effective without any side effects, even in outpatients similar to our study in whom middle ear surgery was conducted as a day care procedure.
In the doses used clonidine did not cause any haemodynamic instability. Patients in group B exhibited haemodynamic stability during the painful procedure of elevation of annulus than patients in group A. Cause of bradycardia in two patients in group B could not be accounted for. Even though clonidine causes bradycardia by central sympatholysis, no evidence of its causing such phenomena by its peripheral action exists.
Effect of clonidine on positively influencing bleeding in the surgical field as seen in our study has been observed by other authors as well, when clonidine was administered systematically [14, 15]. The contributory effect of clonidine in reducing the blood pressure by sympatholysis has been cited as a factor in these cases.
An interesting observation was the reduced incidence of post-operative nausea and vomiting in group B patients. To attribute it to a systemic action of clonidine on absorption would not be farfetched since previous authors have demonstrated significant antiemetic effect of clonidine when given as premedication orally in middle ear surgeries [16] and strabismus surgeries [17]. In our study we administered clonidine at the start of surgery, systemic absorption and subsequent effect may have been hence manifested in the postoperative period. Multiple causes have been attributed to this anti-emetic action of clonidine. High sympathetic tone and catecholamine release have been postulated as factors causing vomiting [18]. In our case it is debatable whether in the doses used, sympatholytic effects and catecholamine release suppression may have contributed to the effect.
Conclusion
Addition of 30 μg of clonidine to 2 % lignocaine with adrenaline for infiltration block provided better pain relief during initial hours and prolongs duration of sensory analgesia, but does not affect onset of anaesthesia or total analgesic consumption. It ensures better patient compliance and surgeon satisfaction in tympanoplasty.
Acknowledgments
Conflict of interests
None declared.
References
- 1.Mirko T. Manual of middle ear surgery. 1. New York: Thieme; 1993. pp. 7–10. [Google Scholar]
- 2.Basker S, Singh G, Jacob R. Clonidine in paediatrics—a review. Indian J Anaesth. 2009;53:270–280. [PMC free article] [PubMed] [Google Scholar]
- 3.Arora K, Singh S. Effect of oral clonidine premedication on perioperative haemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic cholecystectomy. Indian J Anaesth. 2011;55(1):26–30. doi: 10.4103/0019-5049.76583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duma A, Urbanek B, Sitzwohl C, Kreiger A, Zimpfer M, Kapral S. Clonidine as an adjuvant to local anaesthetic axillary brachial plexus block: a randomized controlled study. Br J Anaesth. 2005;94:112–116. doi: 10.1093/bja/aei009. [DOI] [PubMed] [Google Scholar]
- 5.Casati A, Magistris L, Fanelli G, Beccaria P, Cappelleri G, Aldegheri G, et al. Small dose clonidine prolongs postoperative analgesia after sciatic-femoral nerve block with 0.75 % ropivacaine for foot surgery. Anesth Analg. 2000;91:388–392. doi: 10.1097/00000539-200008000-00029. [DOI] [PubMed] [Google Scholar]
- 6.Boezaart AP, Vander MJ, Coetzee A. Comparison of sodium nitroprusside and esmolol induced controlled hypotension for functional endoscopic sinus surgery. Can J Anaesth. 1995;42:373–376. doi: 10.1007/BF03015479. [DOI] [PubMed] [Google Scholar]
- 7.Nishikawa T, Dohi S. Clinical evaluation of clonidine added to lidocaine solution for epidural anesthesia. Anesthesiology. 1990;73:853–859. doi: 10.1097/00000542-199011000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Singelyn FJ, Dangoisse M, Bartholomee S, Gouverneur JM. Adding clonidine to mepivacaine prolongs the duration of anaesthesia and analgesia after axillary plexus block. Reg Anaesth. 1992;17:148–150. [PubMed] [Google Scholar]
- 9.Singelyn FJ, Gouverneur JM, Robert A. A minimum dose of clonidine added to mepivacaine prolongs the duration of anaesthesia and analgesia after axillary brachial plexus block. Anesth Analg. 1996;83:1046–1050. doi: 10.1097/00000539-199611000-00025. [DOI] [PubMed] [Google Scholar]
- 10.Gaumann DM, Brunet PC, Jirounek P. Clonidine enhances the effects of lidocaine on C-fibre action potential. Anesth Analg. 1992;74:719–725. doi: 10.1213/00000539-199205000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Elliot S, Eckersall S, Fligelstone L, Jothilingam S. Does the addition of clonidine affect duration of analgesia of bupivacaine wound infiltration in inguinal hernia surgery? Br J Anaesth. 1997;79:446–449. doi: 10.1093/bja/79.4.446. [DOI] [PubMed] [Google Scholar]
- 12.Acalovschi I, Bodolea C, Manoiu C. Spinal anesthesia with meperidine: effects of added alpha-adrenergic agonists—epinephrine versus clonidine. Anesth Analg. 1997;84:1333–1339. doi: 10.1097/00000539-199706000-00029. [DOI] [PubMed] [Google Scholar]
- 13.Pratap JN, Shankar RK, Goroszeniuk T. Co-injection of clonidine prolongs the anesthetic effect of lidocaine skin infiltration by a peripheral action. Anesth Analg. 2007;104(4):982–983. doi: 10.1213/01.ane.0000257949.46444.a8. [DOI] [PubMed] [Google Scholar]
- 14.Welfringer P, Manel J, Garric J. Clonidine premedication and isoflurane anesthesia to reduce bleeding in otologic surgery. Ann Fr Anesth Reanim. 1992;11(2):125–131. doi: 10.1016/S0750-7658(05)80001-2. [DOI] [PubMed] [Google Scholar]
- 15.Marchal JM, Gomez-Luque A, Martos-Crespo F, et al. Clonidine decreases intraoperative bleeding in middle ear microsurgery. Acta Anaesthesiol Scand. 2001;45(5):627–633. doi: 10.1034/j.1399-6576.2001.045005627.x. [DOI] [PubMed] [Google Scholar]
- 16.Taheri A, Javadimaesh MA, Ashraf H. The effect of oral clonidine premedication on nausea and vomiting after ear surgery. Middle East J Anesthesiol. 2010;20:691–694. [PubMed] [Google Scholar]
- 17.Mikawa K, Nishina K, Maekawa N, Asano M, Obara H. Oral clonidine premedication reduces vomiting in children after strabismus surgery. Can J Anaesth. 1995;42(11):981–997. doi: 10.1007/BF03011068. [DOI] [PubMed] [Google Scholar]
- 18.Jenkins LC, Lahav D. Central mechanisms of vomiting related to catecholamine response: anaesthetic implication. Can Anaesth Soc J. 1971;18:434–441. doi: 10.1007/BF03025695. [DOI] [PubMed] [Google Scholar]