Abstract
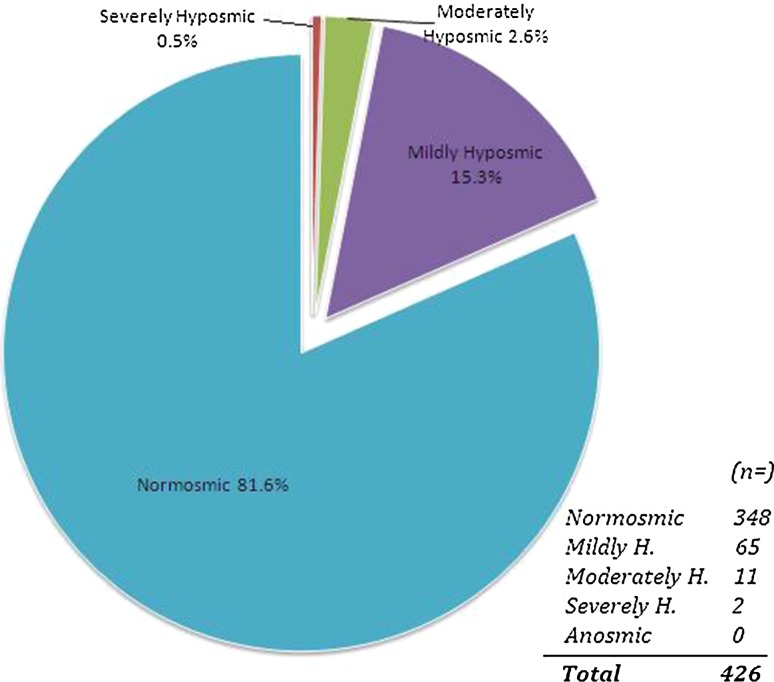
Application of Connecticut Chemosensory Clinical Research Center (CCCRC) olfactory test to healthy Turkish volunteers, obtain normative data set and analyse the role of age, sex and smoking on olfactory scores. The present study was conducted at Bezmialem Vakif University, Department of Otorhinolaryngology. Total of 426 healthy volunteers were subjected to CCCRC olfactory test which consists of n-butanol smell threshold test and smell identification test. Olfactory function score was assessed (0: worst score; 7: best score) and mean scores were calculated. Mean age was (36.7 ± 11.1; range, 17–68). 46.2 % of the subjects were male and 53.8 % were female; 37.1 % were smokers and 62.9 % were non-smokers. Mean n-butanol threshold score was 6.36 out of 7, mean identification score was 6.34 and mean total score was 6.35. According to CCCRC score: there were no anosmic individuals, 0.5 % were severely hyposmic, 2.6 % were moderately hyposmic,15.3 % were mildly hyposmic and 81.6 % were normosmic. CCCRC olfactory test is cost-effective, simple and practical. It can be easily applied in clinical settings. The CCCRC olfactory test is appropriate for assessment of olfactory function: Turkish population is familiar in terms of the odors used in CCCRC test. The power of this study is that it provides a normative data set against which many factors can be compared.
Keywords: Olfactory function, Olfactory dysfunction, Olfactory test, CCCRC, Odor identification, Odor threshold
Introductıon
Although olfaction, combined with chemogustatory perception, has a fundamental role in quality of life; complaints regarding olfactory dysfunction are often neglected by the physicians. Quantitative olfactory assessment can guide diagnosis and explanation of many morbidities, but assessment of olfactory function in daily clinical practice is subjective, qualitative and lacks standardization.
With commercially available quantitative olfactory tests, olfactory function is easily evaluated in daily practice [1–5]. The Connecticut Chemosensory Clinical Research Center test (CCCRC test) defined by the CCCRC consists of smell detection threshold and smell identification test [6]. The aim of this study was to evaluate CCCRC scores of healthy Turkish volunteers, investigate whether the odors used in CCCRC test are familiar with Turkish population, and obtain normative data set against which many factors can be compared and analysed.
Materials and Methods
The present study was performed at Bezmialem Vakif University, Medical Faculty, Department of Otorhinolaryngology and Head and Neck Surgery according to the Helsinki Decleration (WMA 2010). All participants were tested for olfactory function with the approval of University Ethics Committee and in accordance with the guidelines of the National Health and Medical Research. All volunteers were provided with information about the procedures and written informed consents were taken prior to study.
All potential volunteers underwent a detailed nasoendoscopical examination and any condition that could cause olfactory dysfunction such as septum deviation, nasal polyposis, acute rhinosinusitis were excluded from the study. History of head trauma, chronic rhinosinusitis, allergic rhinitis, or psychiatric or neurological disorders, such as Parkinson’s and Alzheimer’s disease, were criteria of exclusion. Also potential volunteers reporting symptoms of an upper respiratory tract infection on the test day had been excluded from the study.
426 healthy Turkish volunteers were included in the study from February 2011 to May 2012. A well-established test of orthonasal olfaction developed at the CCCRC was used. The CCCRC test includes butanol threshold test and odor identification test using common odors: these tests were conducted as described previously [6, 7]
Butanol Threshold Test
For each trial, two glass bottles were presented to the subject. One contained water and the other a dilute concentration of butanol. The bottles were of identical appearance and were presented simultaneously. Subjects were instructed to occlude one nostril and place the tip of the first bottle immediately beneath the other nostril. The second bottle was then sampled in a similar manner, and the subject had to choose which of the bottles contained something other than water. If the choice was incorrect, the next stronger concentration of butanol was presented along with a bottle containing only water. Once the subject identified correctly the same butanol concentration five times in a row, the score was recorded for that nostril. The other nostril was then tested separately, and the scores for both nostrils were averaged to arrive at the final score. The strongest butanol concentration (bottle 0) was 4 % butanol in deionized water. Each subsequent dilution (bottles 1–9) was a 1:3 dilution with deionized water. Possible scores ranged from 0 to 9, but all scores 7 and higher were scored as 7 per the CCCRC test.
Identification Test
Common household odorants: Peanut butter, soap, mothballs, Vicks, chocolate, coffee, cinnamon and baby powder were within opaque jars. Subjects then chose from a printed list containing the correct items as well as an equal number of distractor items. The forced choice items included the following: Vicks, burnt paper, wood shavings, coffee, baby powder, peanut butter, spearmint, cinnamon, soap, chocolate, mothballs, grape jam, ketchup, black pepper, and rubber. The ability to sense Vicks indicates intact trigeminal nerve function. It was easily identified by all subjects and was not included in the final score. Possible scores ranged from 0 to 7 items correctly identified. Scores for both nostrils were averaged to arrive at the final score. Scores for the butanol threshold test and identification tests were subsequently averaged to arrive at a composite score for orthonasal olfactory ability. As in the CCCRC test, scores were grouped by category as detailed in Fig. 1.
Fig. 1.
Evaluation of CCCRC olfactory test scores, patient distribution (%) Normosmic: 6.00–7.00, Mildly hyposmic: 5.00–5.75, Moderately hyposmic: 4.00–4.75, Severely Hyposmic: 2.00–3.75, Anosmic: 0–1.75 (Out of 7)
Statistical Analysis
Data was analysed using Medcalc Software v. 12.3 software (Mariakerke, Belgium). All values were calculated as mean ± standard deviation. Student’s t test was used for statistical analysis for independent groups; p value of less than 0.05 was accepted as statistically significant.
Results
CCCRC olfactory test was carried out on 426 healthy volunteers, mean age was (36.7 ± 11.1; range,17–68). 46.2 % of the subjects were male and 53.8 % were female; 37.1 % were smokers and 62.9 % were non-smokers. Mean n-butanol threshold score was 6.36 ± 0.7 (range, 3.00–7.00) out of 7, mean identification score was 6.34 ± 0.8 (range, 3.00–7.00) and mean total score was 6.35 ± 0.6 (range, 3.25–7.00). Olfactory function was evaluated based on CCCRC olfactory scores as detailed previously [6] (Fig. 1).
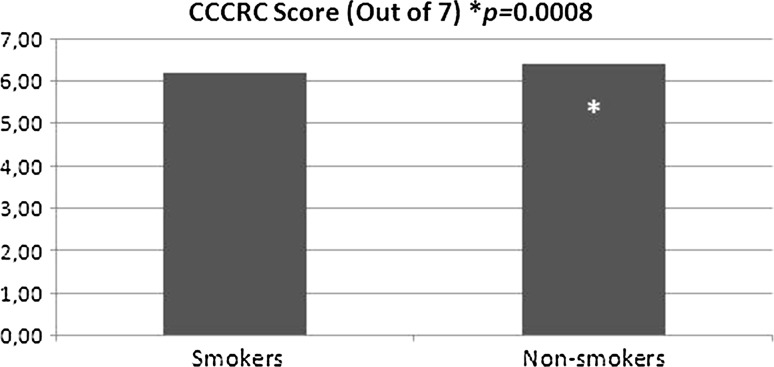
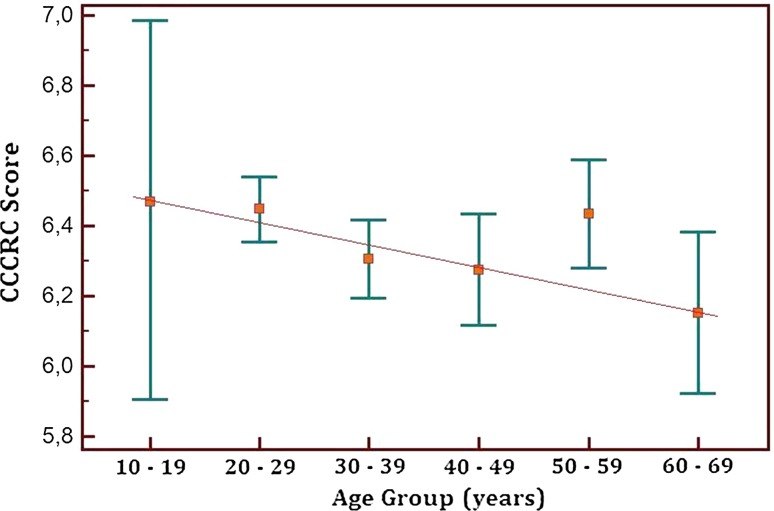
Mean CCCRC score of male subjects was 6.29 ± 0.7, whereas female subjects scored 6.38 ± 0.6. Female subjects scored higher compared to males but the difference was not statistically significant (p = 0.09) (Fig. 2). The effect of smoking on olfactory function was analysed: smokers scored lower compared to non-smokers, (6.21 ± 0.7) versus (6.42 ± 0.6) respectively, the difference was very significant (p = 0.0008) (Fig. 3). CCCRC scores were evaluated in terms of age groups; gradually lowered olfactory scores were observed with increased age (Fig. 4).
Fig. 2.
Total CCCRC test score (out of 7, males vs. females) Female subjects scored higher compared to males but the difference was not statistically significant(p = 0.09)
Fig. 3.
Total CCCRC test score (out of 7, smokers vs. non-smokers) Very significant difference in terms of total CCCRC score (p = 0.0008)
Fig. 4.
CCCRC Scores evaluated based on decades (CCCRC Score vs. Age groups) Lower olfactory scores were observed with increased age, except for the 50–59 age group
Dıscussıon
Assessment of olfactory function in daily practice is subjective, qualitative and lacks in standardization. For the clinician, quantitative olfactory assessment can substantiate diagnosis and guide explanation of many disorders [8–10]. Many tests have been developed and are commercially available for olfactory screening such as the University of Pennsylvania Smell IdentificationTest (UPSIT), Cross Cultural Smell Identification Test (CCSIT), CCCRC test and Sniffin’ Sticks Test (SST) [1–5].
Odor familiarity is an important factor while evaluating olfactory function, because a person should be familiar with an odor in order to identify it correctly [11–13]. A current study performed with UPSIT test showed importance of familiarity to odours included in the olfactory test: odors familiar to the Turkish population were identified correctly by up to 98 % of the subjects, whereas some unfamiliar odors such as root beer, fruit punch, wintergreen and dill pickle had a correct identification rate in the vicinity of 12 % [14]. This is an important factor that may decrease the overall identification score of participants and lead to misdiagnosis. The present study shows CCCRC is compatible with Turkish population, Fig. 1 shows high olfactory scores similar to other normative data [15].
The gradual, idiopathic, decrease in sensory function with older age has been described in many studies [16]. With increased age, surface area of olfactory epitelium decreases and is gradually replaced by respiratory epithelium. In addition, number of mitral cells in olfactory bulbus diminishes [17]. Just like the term presbyacusia is used for age-associated auditory deficits, “presbyosmia” is a term used for age-associated idiopathic olfactory deficiency that takes place with older age [18]. Our results detailed in Fig. 4 are concordant with current literature: total CCCRC score decreases with older age, this downward slope is only interrupted by 50–59 age group which is interestingly similar to results of Mackay et al. [18].
Similar to the literature, female subjects scored higher compared to males but the difference was not statistically significant. Statistically significant olfactory deficit associated with smoking is concordant with the literature: smoking has been found to be adversely associated with the olfactory ability in a dose-related manner. Smokers were found to be nearly six times as likely to evidence an olfactory deficit as non-smokers, depending on the duration and the amount of cigarettes smoked. A study conducted by Katotomichelakis et al. [19] assessed smokers with SST and found lower olfactory threshold, olfactory discrimination, olfactory identification scores compared with non-smokers.
Conclusıon
CCCRC olfactory test is cost-effective, simple and practical. It can be easily applied in clinical settings. The CCCRC olfactory test is appropriate for assessment of olfactory function: Turkish population is familiar with the odors used in CCCRC test. This study provides a normative data set against which many potential olfactory dysfunctions can be compared.
Acknowledgments
Conflict of interest
None
References
- 1.Doty RL. Olfactory dysfunction and its measurement in the clinic and workplace. Int Arch Occup Environ Health. 2006;79:268–282. doi: 10.1007/s00420-005-0055-6. [DOI] [PubMed] [Google Scholar]
- 2.Kobayashi M, Reiter ER, DiNardo LJ, Costanzo RM. A new clinical olfactory function test: crosscultural influence. Arch Otolaryngol Head Neck Surg. 2007;133:331–336. doi: 10.1001/archotol.133.4.331. [DOI] [PubMed] [Google Scholar]
- 3.Nordin S, Brämerson A, Lidén E, Bende M. The Scandinavian odor-identification test: development, reliability, validity and normative data. Acta Otolaryngol. 1998;118:226–234. doi: 10.1080/00016489850154946. [DOI] [PubMed] [Google Scholar]
- 4.Hummel T, Sekinger B, Wolf SR, Pauli E, Kobal G. ‘Sniffin’ sticks’: olfactory performance assessed by the combined testing of odor identification, odordiscrimination and olfactory threshold. Chem Senses. 1997;22:39–52. doi: 10.1093/chemse/22.1.39. [DOI] [PubMed] [Google Scholar]
- 5.Doty RL, Shaman P, Kimmelman CP, Dann MS. University of Pennsylvania Smell Identification Test: a rapid quantitative olfactory function test for the clinic. Laryngoscope. 1984;94:176–178. doi: 10.1288/00005537-198402000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Cain WS, Gent JF, Goodspeed RB, Leonard G. Evaluation of olfactory dysfunction in the Connecticut Chemosensory Clinical Research Center. Laryngoscope. 1988;98:83–88. doi: 10.1288/00005537-198801000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Leon EA, Catalanotto FA, Werning JW. Retronasal and orthonasal olfactory ability after laryngectomy. Arch Otolaryngol Head Neck Surg. 2007;133:32–36. doi: 10.1001/archotol.133.1.32. [DOI] [PubMed] [Google Scholar]
- 8.Yousem DM, Geckle RJ, Doty RL (1995) Evaluation of olfactory deficits in neurodegenerative disorders. In: Abstract of The Radiological Society of North America Scientific Program, Chicago, 1995
- 9.Veyseller B, Aksoy F, Yildirim YS, Acikalin RM, Gurbuz D, Ozturan O. Olfactory dysfunction and olfactory bulb volume reduction in patients with leprosy. Indian J Otolaryngol Head Neck Surg. 2012;64(3):261–265. doi: 10.1007/s12070-011-0284-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Callahan CD, Hinkebein JH. Assessment of anosmia after traumatic brain injury: performance characteristics of the University of Pennsylvania Smell Identification Test. J Head Trauma Rehabil. 2002;17:251–256. doi: 10.1097/00001199-200206000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Jiang RS, Su MC, Liang KL, Shiao JY, Wu SH, Hsin CH. A pilot study of a traditional Chinese version of the University of Pennsylvania Smell Identification Test for application in Taiwan. Am J Rhinol Allergy. 2010;24(1):45–50. doi: 10.2500/ajra.2010.24.3388. [DOI] [PubMed] [Google Scholar]
- 12.Mackay-Sim A, Grant L, Owen C, Chant D, Silburn P. Australian norms for a quantitative olfactory function test. J Clin Neurosci. 2004;11(8):874–879. doi: 10.1016/j.jocn.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Parola S, Liberini P. Assessing olfaction in the Italian population: methodology and clinical application. Ital J Neurol Sci. 1999;20:287–296. doi: 10.1007/s100720050043. [DOI] [PubMed] [Google Scholar]
- 14.Yücepur C, Ozücer B, Değirmenci N, Yıldırım Y, Veyseller B, Ozturan O. University of Pennsylvania smell identification test: application to Turkish population. Kulak Burun Bogaz Ihtis Derg. 2012;22(2):77–80. doi: 10.5606/kbbihtisas.2012.014. [DOI] [PubMed] [Google Scholar]
- 15.Toledano A, et al. The Connecticut Chemosensorial Clinical Research Center olfaction test: values in healthy volunteers. Acta Otorrinolaringol Esp. 2003;54(10):678–685. doi: 10.1016/S0001-6519(03)78467-2. [DOI] [PubMed] [Google Scholar]
- 16.Nusbaum NJ. Aging and sensory senescence. South Med J. 1999;92:267–275. doi: 10.1097/00007611-199903000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Doty RL, Shaman P, Applebaum SL, et al. Smell ıdentifiction ability: changes with age. Science. 1984;226:1441–1443. doi: 10.1126/science.6505700. [DOI] [PubMed] [Google Scholar]
- 18.Mackay-Sim A, Johnston AN, Owen C, Burne TH. Olfactory ability in the healthy population: reassessing presbyosmia. Chem Senses. 2006;31(8):763–771. doi: 10.1093/chemse/bjl019. [DOI] [PubMed] [Google Scholar]
- 19.Katotomichelakis M, Balatsouras D, Tripsianis G, Davris S, Maroudias N, Danielides V, Simopoulos C. The effect of smoking on the olfactory function. Rhinology. 2007;45(4):273–280. [PubMed] [Google Scholar]