Abstract
Purpose
To analyze the diagnostic criteria used in the scientific literature published in the past 25 years for accommodative and nonstrabismic binocular dysfunctions and to explore if the epidemiological analysis of diagnostic validity has been used to propose which clinical criteria should be used for diagnostic purposes.
Methods
We carried out a systematic review of papers on accommodative and non-strabic binocular disorders published from 1986 to 2012 analysing the MEDLINE, CINAHL, PsycINFO and FRANCIS databases. We admitted original articles about diagnosis of these anomalies in any population. We identified 839 articles and 12 studies were included. The quality of included articles was assessed using the QUADAS-2 tool.
Results
The review shows a wide range of clinical signs and cut-off points between authors. Only 3 studies (regarding accommodative anomalies) assessed diagnostic accuracy of clinical signs. Their results suggest using the accommodative amplitude and monocular accommodative facility for diagnosing accommodative insufficiency and a high positive relative accommodation for accommodative excess. The remaining 9 articles did not analyze diagnostic accuracy, assessing a diagnosis with the criteria the authors considered. We also found differences between studies in the way of considering patients’ symptomatology. 3 studies of 12 analyzed, performed a validation of a symptom survey used for convergence insufficiency.
Conclusions
Scientific literature reveals differences between authors according to diagnostic criteria for accommodative and nonstrabismic binocular dysfunctions. Diagnostic accuracy studies show that there is only certain evidence for accommodative conditions. For binocular anomalies there is only evidence about a validated questionnaire for convergence insufficiency with no data of diagnostic accuracy.
Keywords: Accommodation, ocular; Diagnosis; Review literature as topic; Vision, binocular; Vision disorders
Resumen
Objetivo
Analizar los criterios diagnósticos utilizados en la literatura científica publicada en los últimos 25 años en relación a las disfunciones acomodativas y binoculares no estrábicas, así como explorar si se han utilizado los análisis epidemiológicos de validez diagnóstica para proponer qué criterios clínicos deberían utilizarse a fines diagnósticos.
Métodos
Llevamos a cabo una revisión sistemática de los artículos científicos sobre disfunciones acomodativas y binoculares no estrábicas publicados desde 1986 a 2012, analizando las bases de datos de MEDLINE, CINAHL, PsycINFO y FRANCIS. Admitimos artículos originales acerca de los diagnósticos de dichas anomalías en cualquier población. Identificamos 839 artículos e incluimos 12 estudios. Se evaluó la calidad de los artículos incluidos utilizando la herramienta QUADAS-2.
Resultados
La revisión mostró una amplia gama de signos clínicos y sus puntos de corte diagnósticos entre autores. Únicamente 3 estudios (relativos a anomalías acomodativas) abordaron la exactitud diagnóstica de los signos clínicos. Sus resultados sugieren el uso de la amplitud de acomodación y la flexibilidad acomodativa binocular para el diagnóstico de la insuficiencia acomodativa y una alta acomodación relativa positiva para el exceso de acomodación. Los 9 artículos restantes no analizaban la exactitud diagnóstica, abordando el diagnóstico con los criterios considerados por los autores. También hallamos diferencias entre los estudios en cuanto al modo de considerar la sintomatología de los pacientes. 3 estudios de los 12 analizados llevaron a cabo una validación de una encuesta de sintomatología para la insuficiencia de convergencia.
Conclusiones
La literatura científica revela ciertas diferencias entre los distintos autores en cuanto a los criterios diagnósticos para las disfunciones acomodativas y binoculares no estrábicas. Los estudios de exactitud diagnóstica muestran que existe sólo cierta evidencia relativa a las condiciones acomodativas. En cuanto a las anomalías binoculares solo existe cierta evidencia relativa a un cuestionario validado para la insuficiencia de convergencia, sin datos sobre la exactitud diagnóstica.
Palabras clave: Acomodación, ocular; Diagnóstico; Revisión de la literatura; Visión, binocular; Desórdenes de la visión
Introduction
Accommodative and nonstrabismic binocular anomalies are visual dysfunctions which can interfere with a subject's performance or impair one's ability to function efficiently at work. In fact, those persons who perform considerable amounts of close vision, such as reading or computer work, are more likely to develop symptoms and signs related to accommodative or vergence dysfunctions.1 The most common classification to categorize vergence disorders was originally developed by Duane2 for application to strabismus and was later extended to nonstrabismic binocular vision anomalies by Tait.3 Other authors have included the need to regard vergence anomalies as syndromes of deterioration or have proposed classifications based on graphical analysis.4 However, these categorizations have been descriptive which does not necessarily imply etiology and they only consider vergence mechanism in its unfused or open loop state4 but, as other authors have shown,5 these models do not estimate the contribution of proximal factor. For this reason, several authors state that predictions about binocular anomalies should be based on measurements under fusion conditions,4 so that the classification of vergence anomalies should specify binocular status with fusion present.
In this sense, Wick6 described a classification system for nonstrabismic binocular anomalies that represents an expansion of Duane's classification and is based on consideration of the distance phoria (tonic vergence) and the AC/A ratio. In this system, the possible diagnoses can be divided into three main categories of binocular vision problems based on the AC/A ratio. Low AC/A ratio anomalies refer to convergence insufficiency (CI) and divergence insufficiency (DI), normal AC/A ratio are basic exophoria, basic esophoria and fusional vergence dysfunction (FVD) and high AC/A ratio disorders include convergence excess (CE) and divergence excess (DE). According to accommodative anomalies, the classification used is originally from Donders7 and has been popularized by several authors.4,8–11 It includes the anomalies of accommodative insufficiency (AI), accommodative excess (AE) and accommodative infacility (AIN).
In general, accommodative and binocular dysfunctions tend to provoke difficulties related mainly to activities requiring close vision. Symptoms commonly associated with these anomalies may include blurred far or near vision, headaches, diplopia, difficulty in reading, loss of concentration, and in many cases, impossibility to maintain clear vision for a reasonable period of time.12–15 Results of several accommodative and binocular tests, which may be altered, are named as the signs used for diagnosing these anomalies.11
Although research has suggested that these dysfunctions are commonly found in clinical practice,16–27 the scientific literature provides different clinical diagnostic criteria used for these conditions, sometimes with dissimilar diagnoses among authors.4,28,29 A good example is observed for convergence insufficiency condition. Dwyer4 uses a large exophoria of 12 Δ in addition to the clinical signs of reduced positive fusional vergence (PFV), reduced vergence facility (VF) and a fixation disparity curve Type III with no allusion to the near point of convergence (NPC). Other authors28 make the diagnosis of convergence insufficiency using the signs of a greater exophoria at near vision rather than distance (≥4 Δ), a failure of Sheard's criterion or a minimum normative PFV at near vision, and receded NPC.
The exact impact of these anomalies on quality of life is not known. Several studies have found some association between vergence disorders and attention deficit hyperactivity disorder30,31 and there is also some indication that convergence insufficiency can be related to reading problems.32 In any case, considering their symptoms, it seems obvious that clinical recognition would be important to prevent unnecessary frustration among patients. In that sense, vision clinicians diagnose and treat a wide range of visual and ocular anomalies, including not only refractive problems, but also accommodative and binocular vision problems, among others. Treatment of patients with accommodative and binocular disorders is based on interpreting and analyzing the results of visual examination. Accordingly, it is important that accurate information about the diagnosis is available, as the treatment prescribed will depend on the diagnosis. For this reason it is essential not only for researchers but also for clinicians to know the diagnostic validity of the clinical criteria often used for these conditions.
Diagnostic validity (or diagnostic accuracy) of clinical diagnostic tests is usually examined by means of predictive values, sensitivity and specificity or analyzing the receiver operator curve (ROC).33 A ROC curve shows how severe the trade-off is between sensitivity and specificity and can be used to help decide where the best cut-off point should be for a particular test. It shows the accuracy of a diagnostic test which can be described as the area under the ROC curve. In epidemiological terms the diagnostic validity represents the scientific evidence33 about the way to diagnose these visual conditions. In relation to clinical practice, the term ‘evidence’ is used specifically to refer to sources of knowledge that are relevant to the practical solution for a clinical problem.34 Such problems may be more general or specific. It should be a decision on which available treatment will provide the best outcome for a particular condition and patient. Or even they might be such as the choice of the best examination procedure to minimize risk of misdiagnosis or failure to detect a particular disease or condition.34
In that sense, the strongest form of clinical evidence is a “systematic review” of a number of trials or studies addressing the one clinical question.35 Suitable trials or studies are extracted from the literature by a well-designed search strategy.34 A systematic review is then an overview of primary studies, which is conducted according to explicit and reproducible methodology which may contain a meta-analysis but not necessarily.36
Therefore, the aim of this study is to analyze the diagnostic criteria used in the scientific literature for accommodative and nonstrabismic binocular dysfunctions by means of a systematic review of papers published in the past years about the diagnosis of these conditions.
Specific aims are to explore which symptoms and clinical signs are used by different studies; to explore if an epidemiological analysis of diagnostic validity has been used in different studies related to the diagnosis of these conditions and to evaluate if authors utilize these results to recommend the clinical criteria to diagnose these anomalies or use other diagnostic criteria.
Methods
We carried out an exhaustive search on content published in four health-science databases from 1986 to January 25, 2012. The search was carried out using MEDLINE, CINAHL, Francis and PsycINFO databases. We decided to study this large time frame in order to avoid omission of possible relevant information on these anomalies.
The search strategy was based on the use of terms in free language related to these visual anomalies, searching in all fields of the databases. The search equation included Boolean operators, truncated symbols and wildcard characters which are specific signs used in information sciences and in databases selected. As we wanted to examine the anomalies of accommodative excess, accommodative insufficiency, accommodative infacility, convergence insufficiency, convergence excess, divergence excess, divergence insufficiency, basic esophoria, basic exophoria, fusional vergence dysfunction and hyperphoria, the search terms used were the following:
-
•
(Accommodative excess) OR (excess of accommodation)
-
•
(Accommodative spasm) OR (spasm of accommodation)
-
•
(Accommodative insufficiency) OR (insufficiency of accommodation)
-
•
(Accommodative infacility) OR (infacility of accommodation)
-
•
(Accommodative disorder*) OR (accommodative anomal*) OR (accommodative dysfunction*)
-
•
(Disorder* of accommodation) OR (anomal* of accommodation) OR (dysfunction* of accommodation)
-
•
(Convergence insufficiency) OR (insufficiency of convergence)
-
•
(Convergence excess) OR (excess of convergence)
-
•
(Convergence spasm) OR (spasm of convergence)
-
•
(Divergence excess) OR (excess of divergence)
-
•
(Divergence insufficiency) OR (insufficiency of divergence)
-
•
Basic e?ophoria
-
•
(Vergence disorder*) OR (vergence anomal*) OR (vergence dysfunction*)
-
•
(Binocular disorder*) OR (binocular anomal*) OR (binocular dysfunction*)
-
•
(Vergence infacility) OR (reduced fusional vergence) OR (fusional vergence dysfunction*) OR (fusional vergence anomal*) OR (fusional vergence disorder*)
-
•
Hyperdeviation* OR hypodeviation* OR hypophoria* OR hyperphoria* OR (vertical deviation*) OR vertical disorder*) OR (vertical anomal*) OR (vertical dysfunction*) not surgery.
The inclusion criteria were original articles whose purpose were to study the diagnosis of accommodative and nonstrabismic binocular dysfunctions. They could be descriptive studies or clinical studies with sample populations including all ages from children to adults. As the aim of this review was only related to diagnosis of these conditions and we wanted to know if the scientific literature published had analyzed the diagnostic validity of clinical criteria used, we excluded papers about the prevalence and treatment of these conditions. We also excluded studies not fundamentally concerned with the diagnosis of accommodative and nonstrabismic binocular disorders; publications related to the performance of optometric tests but not related to diagnosis of anomalies; expert guides or opinions; non-original articles and studies on strabismic binocular disorders or ocular pathologies.
Using the search terms, we found 839 articles. Following the inclusion and exclusion criteria, we initially selected 42 articles for exhaustive study and to confirm inclusion. Of the 797 articles we excluded 326 (40.9%) which mentioned but were not fundamentally related to diagnosis of these anomalies, 195 (24.5%) dealt with strabismic anomalies, 125 (15.7%) were concerned with ocular pathologies, 75 (9.4%) concerning treatment and prevalence of dysfunctions and 76 (9.5%) were studies about the assessment of several tests.
Of the 42 articles, 30 did not fulfill the inclusion criteria and were excluded from further analysis. The remaining included articles (n = 12) were analyzed.4,28,29,37–45
As selected studies were not related to any intervention and were not homogeneous, no meta-analysis was performed. Accordingly, included articles were reviewed using a range of variables. We examined the methodological characteristics, showing the characteristics of the sample and exploring if studies had analyzed the diagnostic validity of the criteria used. We also examined and registered information regarding the clinical signs and the cut-off points taken into account for each anomaly. We also explored the results of each study, compiling data about their conclusions, biases and limitations. Finally, to examine the quality of included articles, we used the QUADAS-2 tool which is used to test the quality of studies about diagnostic accuracy included in systematic reviews46 and recommended by the Cochrane Collaboration.47 The QUADAS tool consists of 4 key domains that discuss: patient selection, index test, reference standard, and flow of patients through the study and timing of the index tests and reference standard (flow and timing). For each domain there are signaling questions which aid the reviewer to judge the risk of bias (high, low or unclear) and concern regarding applicability of each study. For the domain of patient selection is considered if the sample is consecutive or randomized. The index test consider if an index test result is interpreted without the knowledge of the results of the reference standard as the potential for bias is related to the subjectivity of interpreting index test and the order of testing. The domain of reference standard is considered to know if the reference standard, its conduct or its interpretation may have introduced bias. Thus the aim is to know if the reference standard is likely to correctly classify the target condition and if the reference standard results are interpreted without knowledge of the results of the index test. The last domain (flow and timing) is considered if there is an appropriate interval between the index test and reference standard, if all patients receive the same reference standard, and if all patients are included in the analysis. Finally, the QUADAS-2 tool includes also data of applicability so that the aim is to know if there are concerns that the included patients and setting, the index test, and the target condition defined by the reference standard match the review question. These QUADAS-2 results are suggested to be shown in a tabular presentation and with a graphical display.
Results
Table 1 contains the methodological characteristics of each of the studies reviewed. It shows the characteristics of the sample and study population, the type of dysfunction analyzed, the information about the validation of symptoms and if each study analyses the diagnostic validity of clinical signs.
Table 1.
Methodological characteristics of the 12 studies included.
| Study | Characteristics of the sample | Study population | Dysfunction | Diagnostic validity of symptoms | Diagnostic validity of clinical signs |
|---|---|---|---|---|---|
| 2006, Marran LF37 | 299 children (46.1% male, 53.9% female) Age range not specified Mean age: 11.5 ± 0.63 years |
19 schools | CI AI |
||
| 2006, Sterner B38 | First examination: 72 children (43 male, 29 female) Age: 5.8–10 years Mean age not specified |
School | AI | ROC analysis using symptoms at near as the gold standard | |
| Second examination: 59 children after 1.8 years (34 male, 25 female) Age: 7.8–11.8 years Mean age not specified |
Positive and negative predictive values | ||||
| 2004, Rouse MW39 | 46 patients with CI (28% male, 72% female) Age: 19–30 years Mean age: 24.3 ± 3.6 years |
6 optometric clinics | CI | ROC analysis to test the ability of CISS V-15 questionnairea to discriminate between CI and NBV groups | |
| 46 patients with normal binocular vision (23% male, 77% female) Age: 19–30 year Mean age: 24.4 ± 3.2 years |
|||||
| 2003, Borsting EJ40 | 47 children with CI 62.5% male, 57.5% female Age: 9–18 years Mean age: 11.5 ± 2.2 years 56 children with NBV (54.5% male, 45.5% female) Age: 9–18 years Mean age: 11.4 ± 2.2 years |
5 optometric clinics | CI | Sensitivity and specificity for the CISSb score | |
| 2002, García A41 | 69 patients (29 male, 40 female) Age: 13–35 years Mean age: 20.8 ± 4.7 years |
Optometric clinic | AI, AE, CI, CE | Sensitivity and specificity analysis | |
| 2002, Cacho P29 | 41 patients with diminished AA 40 patients with normal AA Sex not specified Age: 13–35 years Mean age not specified |
Optometric clinic | AI | Sensitivity and specificity analysis | |
| 1999, Borsting E28 | 14 children with CI (8 male, 5 female) Age: 8–13 years Mean age: 10.75 ± 1.8 years 14 children with NBV (5 male, 9 female) Age: 8–13 years Mean age: 11.2 ± 1.75 years |
Optometric clinic | CI | Sensitivity and specificity analysis of CIRSc symptom survey and Odds ratio | |
| 1991, Dwyer PS4 | Sample not used | – | AI, AE, AIN, CI, CE, DI, DE, BExo, BEso | ||
| 1988, Rutsein RP42 | 17 patients (6 male, 11 female) Age: 7–39 years Mean age: 17.9 years |
University optometric clinic | AE | ||
| 1988, Chrousos GA45 | 10 patients (4 male, 6 female) Age: 10–19 years Mean age not specified |
Not specified | AI | ||
| 1986, Scheiman M43 | Sample not used | – | DI | ||
| 1986, Daum KM44 | 179 patients (69 male, 110 female) Age: 2–56 years Mean age: 19.7 years |
Optometric clinic | CI, BExo, DE | ||
NBV: normal binocular vision, AI: accommodative insufficiency, AE: accommodative excess, CI: convergence insufficiency, CE: convergence excess, AIN: accommodative infacility, DI: divergence insufficiency, DE: divergence excess, BExo: basic exophoria, BEso: basic esophoria, NPC: near point of convergence, AA: accommodative amplitude, NFV/PFV: negative/positive fusional vergence, MAF/BAF monocular/binocular accommodative facility, PRA/NRA: positive/negative relative accommodation.
CISS V-15: 15-item version of CISS, Convergence Insufficiency Symptom Survey.
CISS: 13-item of CISS, Convergence Insufficiency Symptom Survey.
CIRS symptom survey: Convergence Insufficiency and Reading Study symptom survey.
Of the twelve articles reviewed, five of them are prospective clinical studies which select patients and several optometric tests are carried out.29,37,38,41,45 Two studies collect data retrospectively from the patients’ optometric records42,44 and two reports make a descriptive analysis of the dysfunctions.4,43 On the other hand, three papers28,39,40 also study the diagnosis, although their aim is to validate a symptom questionnaire related to these anomalies. According to the samples, most of the articles refer to clinical populations,28,29,39–42,44 with two studies37,38 in which the population is collected from schools. Four studies28,37,38,40 deal with child populations and other six studies29,39,41,42,44,45 refer to adult populations.
According to the type of dysfunctions, CI is the most studied condition when considering binocular anomalies, with seven studies.4,28,37,39–41,44 There are two studies about CE,4,41 DI,4,43 DE,4,44 basic exophoria4,44 and only one related to basic esophoria.4 For accommodative conditions there are more studies on AI, with six studies,4,29,37,38,41 compared with AE with three reports4,41,42,45 and only one about AIN.4
Regarding the validity of diagnostic criteria, three reports28,39,40 perform a validation of the symptoms used for convergence insufficiency. There are also three studies29,38,41 in which several epidemiological tools are used to test the diagnostic accuracy of clinical signs used for several conditions.
Tables 2–4 show the diagnostic criteria used for convergence insufficiency, other binocular anomalies, and accommodative dysfunctions, respectively. They show both the clinical signs and the cut-off points used to diagnose these conditions by each author. The tables also include how the authors collected patients’ symptoms. As we can observe the authors use more than one test to diagnose the anomalies, ranging from one to seven clinical signs for both binocular and accommodative dysfunctions. There are also differences in the cut-offs used to decide if a patient fails a test.
Table 2.
Diagnostic criteria used for convergence insufficiency.
| Dysfunction | Study | Diagnostic criteria |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Clinical signs |
||||||||||
| Phoria | PFV | NPC | AC/A | BAF | MEM | PRA | VF | FD curve | |||
| NFV | NRA | ||||||||||
| Convergence insufficiency | 2006, Marran LFa 37 | CISS V-15 symptom questionnaire | Exophoria at near ≥4 Δ greater than at distance Von Graefe method |
PFV failures to reach Sheard's 11criteria or failure to have minimum normative PFV at near, ≤15Δ for break | ≥6 cm break | ||||||
| 2004, Rouse MW39 | CISS V-15 symptom questionnaire score ≥ 21 | Exophoria at near ≥4 Δ greater than at distance Von Graefe method |
PFV failures to reach Sheard's 11criteria or failure to have minimum normative PFV at near, ≤15Δ for break |
≥6 cm | |||||||
| 2003, Borsting EJ40 | CISS V-15 symptom questionnaire score ≥ 16 | Exophoria at near ≥4 Δ greater than at distance Von Graefe method |
PFV failures to reach Sheard's 11criteria or failure to have minimum normative PFV at near, ≤15Δ for break | ≥6 cm | |||||||
| 2002, García,Ab 41 | Reported without questionnaire | Exophoria at near >6 Δ. Cover test method | PFV ≤ 11/14/3 Δ, at least one of three responses of blur/break/recovery | >10 cm break or >17.5 recovery | Calculated AC/A < 3/1 | ≤3 cpm Difficulty clearing +2 D (±2 D) |
<+0.25 D | NRA ≤1.50 D |
|||
| 1999, Borsting E28 | CIRS symptom questionnaire score ≥9 | Exophoria at near ≥4 Δ greater than at distance Method not specified |
Failed Sheard's criterion or minimum PFV at near, ≤12/15/4 Δ | ≥7.5 cm break | |||||||
| 1991, Dwyer PS4 | Not reported | Exophoria at near = 12 Δ | PFV = 0 blur/break and recovery | ≤3/1 | Diplopia with 12 Δ Base-out | Type 3 curve | |||||
| 1986, Daum KM44 | Reported without questionnaire | If the angle at far is ≤5 Δ exophoria, it must be at near at least 4 Δ more exo If the angle at far is ≥6 exophoria, it must be at near at least 10 Δ more exo Cover test method |
|||||||||
NPC: near point of convergence, NFV/PFV: negative/positive fusional vergence, BAF: binocular accommodative facility, MEM: MEM dynamic retinoscopy, PRA/NRA: positive/negative relative accommodation, Δ: prism diopters.
Authors consider having an exophoria at near a fundamental sign and CI may be diagnosed with one, two or three clinical signs.
Authors diagnose CI considering exophoria, PFV and NPC as fundamental signs and patients must have at least two signs of the remaining four signs.
Table 3.
Diagnostic criteria used for other binocular anomalies.
| Dysfunction | Study | Diagnostic criteria |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms |
Clinical signs |
||||||||||
| Phoria | NFV | NPC | AC/A | BAF | MEM | PRA | VF | FD curve | |||
| PFV | NRA | ||||||||||
| Convergence excess | 2002, García Aa 41 | Reported without questionnaire | Esophoria at near > 2 Δ. Cover test method |
NFV ≤ 8/16/7 Δ, at least one of three responses of blur/break/recovery | Calculated AC/A > 7/1 | ≤3 cpm Difficulty clearing −2 D (±2 D) |
<+0.25 D | PRA ≤ 1.25 D | |||
| 1991, Dwyer PS4 | Not reported | Esophoria at near = 6 Δ | NFV = 0 blur/break and recovery | ≥6/1 | Diplopia with 10 Δ Base-in | Type 2 curve | |||||
| Divergence insufficiency | 1991, Dwyer PS4 | Not reported | Esophoria at far = 3 Δ | NFV = 0 blur/break and recovery | ≤3/1 | =0 Δ with Base-in | |||||
| 1986, Scheiman M43 | Reported without questionnaire | Greater esodeviation at far than near (values not specified) | NFV diminished at far | Low AC/A | |||||||
| Divergence excess | 1991, Dwyer PS4 | Not reported | Exophoria at far = 5 Δ | PFV = 0 blur/break and recovery | ≥6/1 | =0 Δ with Base-out | |||||
| 1986, Daum KM44 | Reported without questionnaire | If the angle at far is ≤5 Δ exophoria, it must be at near at least 4 Δ less exo If the angle at far is ≥6 exophoria, it must be at near at least 10 Δ less exo Cover test method |
|||||||||
| Basic exophoria | 1991, Dwyer PS4 | Not reported | Uncompensated exophoria at far and near | =4.5/1 | |||||||
| 1986, Daum KM44 | Reported without questionnaire | If the angle at far is ≤5 Δ exophoria, it can be at near between 0 and 3 Δ more or less exo If the angle at far is ≥6 exophoria, it can be at near between 0 and 9 Δ less exo or between 0 and 3 Δ more exo Cover test method |
|||||||||
| Basic esophoria | 1991, Dwyer PS4 | Not reported | Uncompensated esophoria at far and near | =4.5/1 | |||||||
NFV/PFV: negative/positive fusional vergence, NPC: near point of convergence BAF: binocular accommodative facility, MEM: MEM dynamic retinoscopy, PRA/NRA: positive/negative relative accommodation, VF: vergence facility, FD: fixation disparity, Δ: prism diopters.
Authors diagnose CE considering esophoria, NFV as fundamental signs and patients must have at least two signs of the remaining four signs).
Table 4.
Diagnostic criteria used for accommodative anomalies.
| Dysfunction | Study | Diagnostic criteria |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Clinical signs |
|||||||||
| AA | MAF | BAF | MEM | PRA | NRA | Visual acuity | Refractive error | |||
| Accommodative insufficiency | 2006, Marran LF37 | CISS V-15 symptom questionnaire | Monocular AA 2 D ≤ Hofstetter's minimum age formula: 15–0.25 × age Monocular Push up method |
|||||||
| 2006, Sterner B38 | Reported by several questions | AA < 8 D monocular and < 10 D binocular AA Monocular Push-up method |
||||||||
| 2002, García, Aa 41 | Reported without questionnaire | Reduced AA: at least 2 D < minimum age appropriate amplitude of Hofstetter's formula (15–0.25 × age) Monocular Push-up method |
≤6 cpm Difficulty clearing −2 D (±2 D) |
≤3 cpm Difficulty clearing −2 D (±2 D) |
>+0.75 D | ≤1.25 D | ||||
| 2002, Cacho Pb 29 | Reported without questionnaire | Reduced AA: at least 2 D < minimum age appropriate amplitude of Hofstetter's formula (15–0.25 × age) Monocular Push-up method |
≤6 cpm Difficulty clearing −2 D (±2 D) |
≤3 cpm Difficulty clearing −2 D (±2 D) |
>+0.75 D | ≤1.25 D | ||||
| 1991, Dwyer PS4 | Not reported | AA 3 D < Hofstetter's formula: 15–0.25 × age | Blurred with −2 D (±2 D) | ≥+1.00 D | ≤1.00 D | |||||
| 1988, Chrousos GA45 | Reported without questionnaire | AA below the normal for the patients’ ages Monocular push-up method |
||||||||
| Accommodative excess | 2002, García, Ac 41 | Reported without questionnaire | ≤6 cpm Difficulty clearing −2 D (±2 D) |
≤3 cpm Difficulty clearing +2 D (±2 D) |
<0 D | High finding ≥3.50 D |
≤1.50 D | Variable | Variable retinoscopy and subjective refraction | |
| 1991, Dwyer PS4 | Not reported | Blurred with +2 D (±2 D) | ≤−0.50 D | ≤1.00 D | ||||||
| 1988, Rutsein RP42 | Reported without questionnaire | A lead movement. Value not specified | Varies. May be somewhat reduced | Varies (frequently emmetropia) | ||||||
| Accommodative infacility | 1991, Dwyer PS4 | Not reported | Disorder of facility (values not specified) | |||||||
AA: accommodative amplitude, MAF: monocular accommodative facility, BAF: binocular accommodative facility, MEM: MEM dynamic retinoscopy, PRA: positive relative accommodation, NRA: negative relative accommodation.
Authors consider AA and MAF as fundamental signs and patients must have at least two signs of the rest of three signs.
Authors consider AA and MAF fundamental signs, being BAF, MEM and PRA complementary signs.
Authors consider VA, Refractive error and MAF as fundamental signs and patients must have at least two signs of the rest of three signs.
Table 5 shows the conclusions obtained, biases and limitations identified in the papers. Several studies related to accommodative dysfunctions29,38,41,42 obtain specific conclusions, suggesting the use of several diagnostic tests. The conclusions obtained for binocular dysfunctions are more general and less focused on suggesting the use of particular tests. There is also a notable absence of validated symptom questionnaires used to diagnose the anomalies.
Table 5.
Conclusions, bias and limitations of the studies.
| Year of publication and author | Conclusions | Bias/limitations identified by the authors | Bias/limitations observed in the review |
|---|---|---|---|
| 2006, Marran LF37 | CI is a separate and unique clinical condition and can occur without a comorbid AI condition. However, CI by itself is not a highly symptomatic condition. Only when the CI is comorbid with AI, do children with CI score higher than children with normal binocular vision, strongly suggesting that the high score is driven by the AI condition. | – | – |
| 2006, Sterner B38 | The ROC analysis illustrate that the AA has potential discrimination ability for accommodative insufficiency. Values of 8 D monocular or 11 D binocular are values which could be used as reference values since they clearly imply a high risk of symptoms for children with results below these limits. |
Children below 7.5 years with no reported symptoms could have been biased as they tend to give the “correct” reply just to please the interviewer. The population could be described as an invited population. Perhaps children with symptoms were more willing to take part in the study implying that the prevalence is higher than it would be if a true screening was applied. The choice of references values of AA is somewhat arbitrary. |
No validated symptom questionnaire used. Binocular accommodative amplitude considered. Accommodative amplitude results interpreted with the knowledge of the results of subjective symptoms of patients. |
| 2004, Rouse MW39 | Adults with symptomatic CI have a significantly higher CISS score than adults with NBV. The CISS is a valid and reliable instrument that can be used clinically or as an outcome measure for research studies of adults with CI. A CISS score ≥ 21 distinguish between adults with normal and abnormal levels of symptoms. |
– | Clinical population. Conclusions are not representative of general population. Questionnaire results interpreted with the knowledge of the results of diagnosis. |
| 2003, Borsting E J40 | Children with CI show a significantly higher CISS symptom score than children with normal binocular vision. The CISS is a valid and reliable instrument to use as an outcome measure for children aged 9 to 18 who are enrolled in clinical research concerning CI. A CISS score of ≥16 distinguish between children with normal and abnormal levels of symptoms associated with CI. |
– | Clinical population. Conclusions are not representative of general population. Questionnaire results interpreted with the knowledge of the results of diagnosis. |
| 2002, García, A41 | There is no sign strongly associated with the presence of diminished AA. However, failing MAF with −2 D lenses seems to be the sign mostly associated with AI. Authors propose using MAF together with diminished AA for diagnosing AI. |
– | No validated symptom questionnaire used. Clinical population. Conclusions are not representative of general population. Diagnosis interpreted with the knowledge of the results of tests. |
| 2002, Cacho P29 | Anomalous results of NRA are not clearly associated with any dysfunction. High values of PRA are related to disorders associated with accommodative excess, so that a high value of PRA (≥3.50 D) should be considered as one of the diagnostic signs associated with accommodative excess. | – | No validated symptom questionnaire used. Clinical population. Conclusions are not representative of general population. Diagnosis interpreted with the knowledge of the results of tests (sensitivity and specificity obtained with tests used for diagnosing the anomalies). |
| 1999, Borsting E28 | The CIRS symptom survey is useful for identifying the type and frequency of symptoms in children with convergence insufficiency (CI) and also able to differentiate between the CI and normal binocular vision (NBV) groups. | Sample size of 14 subjects relatively small. Results could be explained by experimenter bias in the administration of the survey to the parent and child. Other source of potential bias is that the CI group could have had a co-occurring condition that affected the responses to the survey. |
Clinical population. Conclusions are not representative of general population. Normal binocular subjects were recruited through advertisements at the teaching clinic. Questionnaire results interpreted with the knowledge of the results of diagnosis. |
| 1991, Dwyer PS4 | Measuring binocular function under fused conditions give a more complete measure of the status of binocularity. A system of nomenclature of accommodative and vergence disorders consistent with the concept of vergence-accommodation “adaptability” rather than visual axis deviation is suggested. |
– | No validated symptom questionnaire used. |
| 1988, Rutsein RP42 | Diagnosis of accommodative excess should be based on dynamic retinoscopy. | – | No validated symptom questionnaire used. It is proposed that diagnosis should be based on dynamic retinoscopy that it has been previously used to diagnose patients with accommodative excess. Clinical population. Conclusions are not representative of general population. |
| 1988, Chrousos GA45 | The AA of patients with AI is considerably below the normal for the patients’ ages. The range of the deficiency is from 3.5 D to 8 D with an average of 6 D below the minimum normal for their respective ages. The clinical recognition of AI is important to prevent unnecessary frustration in these individuals. |
– | No validated symptom questionnaire used. It is not reported the value of the minimal accommodative amplitude used for considering accommodative insufficiency. |
| 1986, Scheiman M43 | Divergence insufficiency must be differentiated from divergence paralysis as well as from sixth nerve palsy, convergence excess and basic esophoria, all of which can present with an esodeviation at distance. The differential diagnosis depends very much upon the nature of the patient's symptoms. |
– | No validated symptom questionnaire used. |
| 1986, Daum KM44 | Patients with exodeviations, when divided into three classes on the basis of the relation between the near and distance angles of deviation, show significant differences in various clinical parameters. Patients with equal exodeviations have the largest angles of deviations overall and those with CI generally have smaller angles than the other groups. Differences in the AC/A ratios are to be expected on the basis of the classification criteria. | The data should not be considered exactly representative of the general population because the clinic form which the records were drawn is a referral clinic. | No validated symptom questionnaire used. Clinical population. Conclusions are not representative of general population. |
CI: convergence insufficiency, AI: accommodative insufficiency, AA: accommodative amplitude, MAF: monocular accommodative facility, NRA/PRA: negative and positive relative accommodation, D: diopters.
As only 6 of 12 included studies show the diagnostic validity, QUADAS-2 results are only presented for them (Tables 6 and 7). Furthermore, to better understand results of quality rating, the 6 studies analyzed by the QUADAS-2 tool were divided into two categories: those designed to assess the accuracy of clinical signs and those investigating the validation of a questionnaire for convergence insufficiency. These results are also presented in a graphical display, showing the proportion of studies with high, low or unclear risk of bias. Figs. 1 and 2 show the QUADAS-2 domain for articles related to clinical signs and those related to symptoms, respectively.
Table 6.
Quality rating of the 3 included studies related to clinical signs (QUADAS −2 results).
| Study | Risk of bias |
Applicability concerns |
|||||
|---|---|---|---|---|---|---|---|
| Patient selection | Index test | Reference standard | Flow and timing | Patient selection | Index test | Reference standard | |
| 2006, Sterner B38 | |||||||
| 2002, García A41 | ? | ||||||
| 2002, Cacho P29 | ? | ? | |||||
( ) low risk; (
) low risk; ( ) high risk; (?) unclear risk.
) high risk; (?) unclear risk.
Table 7.
Quality rating of the 3 included studies related to symptoms (QUADAS −2 results).
| Study | Risk of bias |
Applicability concerns |
|||||
|---|---|---|---|---|---|---|---|
| Patient selection | Index test | Reference standard | Flow and timing | Patient selection | Index test | Reference standard | |
| 2004, Rouse MW39 | |||||||
| 2003, Borsting EJ40 | |||||||
| 1999, Borsting E28 | |||||||
( ) low risk; (
) low risk; ( ) high risk; (?) unclear risk.
) high risk; (?) unclear risk.
Fig. 1.
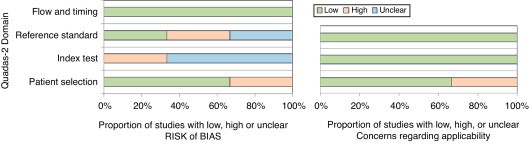
QUADAS-2 domain for articles related to clinical signs.29,38,41.
Fig. 2.
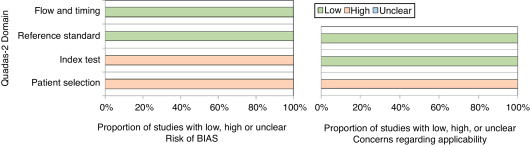
QUADAS-2 domain for articles related to symptoms.28,39,40.
Discussion
The scientific literature targeting the field addressed in this review is extensive. The review reveals differences between authors according to diagnostic criteria used in the scientific literature for accommodative and nonstrabismic binocular dysfunctions. However, most of the publications consist of narrative overviews describing methods, techniques, symptoms, for the clinical evaluation of general binocular anomalies. In contrast, only a few studies were designed for assessing the accuracy of clinical tests and symptoms. Diagnostic accuracy studies show that there is only certain evidence for accommodative conditions. For binocular anomalies there is only evidence about a validated questionnaire for convergence insufficiency with no data of diagnostic accuracy about binocular anomalies so that the evidence of diagnostic criteria for binocular dysfunctions cannot be found within papers that have been published over the past years. In any case, we should consider that these arguments may only be applied within the framework of this study. The data supplied refers to the past 25 years and the articles analyzed have been published in scientific journals. Therefore, there may be data in earlier publications or publications not listed within the databases we used. Anyway the papers we reviewed were all in peer-reviewed journals.
According to binocular conditions, no study was found in which the authors assessed the diagnostic validity33 of the clinical signs used. That is, no one used data of predictive values, sensitivity and specificity or assessed the ROC curve.
Although CI is one of the binocular anomalies most referred to,4,28,37,39–41,44 in no case the authors validate the tests used by comparison against an established reference standard (gold standard). They reach their diagnoses on the basis of the criteria they consider patients should have, but fail to specify why certain clinical signs are taken into account and others are not. The same is true for the other binocular anomalies, although they are the subject of fewer studies. Thus, Marran et al.,37 adopt the classification system used by the Convergence Insufficiency Treatment Trial (CITT) Group20,22 for CI. It includes the signs of an exophoria at near vision greater than at far at least 4 Δ, insufficient positive fusional vergence (PFV), and receded near point of convergence (NPC). This classification system, as the authors declare in their study,20 is based on the signs most often associated with convergence insufficiency. However, there is no analysis of the validity of these signs to confirm the accuracy of them. The studies which deal with a validation of the convergence insufficiency symptom survey (CISS)28,39,40 also use this classification of CI.
Similarly, in Daum44 retrospective study the exodeviations are classified into three classes without an explanation of this classification. The study of García et al.,41 follows a diagnostic criteria based upon the authors particular consideration. Dwyer4 study describes a diagnostic model for vergence accommodation disorders taking into account the convergence-accommodation interactions. The author suggests a system of nomenclature consistent with the concept of vergence-accommodation adaptability rather than visual axis deviation. Similarly, other authors43 make a descriptive analysis about the characteristics and differential diagnosis of DI. They define this condition by referring to the signs according to different authors, but they do not validate the clinical signs.
As it can be observed, studies about binocular anomalies show that it is difficult to provide information on what current criteria should be considered reliable for clinician. The reason is that none of the studies reviewed analyses which clinical signs have the best diagnostic accuracy for each binocular dysfunction. For that reason, future studies related to binocular anomalies should address this issue, that is, the diagnostic validity of different clinical signs used for each anomaly. Knowing this evidence, clinicians could apply diagnostic criteria being aware of their decision for each individual case.
Considering accommodative conditions, there are only three of the seven studies which use diagnostic criteria based on epidemiological analysis. For this reason only these articles were assessed using the QUADAS-2 tool. Thus, in the study by Sterner et al.,38 the authors test with ROC analysis the discrimination ability of accommodative amplitude and relative accommodations for accommodative insufficiency (AI). ROC analysis illustrates that the amplitude of accommodation (AA) is a test that has potential discrimination ability for AI. The authors state that as they have found a relationship between AA and subjective symptoms, there is reasonable evidence to use reference values of AA. The choice with ROC analysis is 8 D for monocular and 11 D for binocular which implies that children with results below these limits have a high risk of symptoms. If either 8 D monocular or 11 D binocular are used as diagnostic criteria, to have a joint diagnosis of AI should be considered an AA below these values together with the presence of symptoms. In any case, the authors state that the choice of these values for AA is somewhat arbitrary and should be investigated by others.
The authors of Cacho et al.,29 analyze the condition of AI. They determine as the most sensitive tests of MEM retinoscopy, monocular and binocular accommodative facility (MAF, BAF) and positive and negative relative accommodation (PRA, NRA), together with AA, for classifying this condition. The authors recommend the use of MAF along with AA for their diagnosis based on sensitivity results. However, the authors do not assess the ROC analysis or predictive values to test the accuracy of these tests. Conclusions are related to sensitivity results which consider that failing the ±2.00 D monocular accommodative facility (with a value ≤3 cpm) seems to be the sign most associated with accommodative insufficiency. The risk of bias of this study is that the authors do not clarify the order of the tests, so that is unclear if the index test were interpreted without knowledge of the results of reference standard and conversely.
Similarly, García et al.,41 analyze different tests associated with accommodative excess (AE). They find that high values of PRA are related to disorders associated with AE. While their conclusions are based on sensitivity and specificity results, there is an important bias in this study since sensitivity and specificity values are obtained through the same tests previously used to diagnose the anomalies. That is, the reference standard results (the diagnosis of each condition) were interpreted with knowledge of the results of the index tests (each clinical test assessed), situation that could have introduced bias in the study.
The other four studies about accommodative anomalies do not analyze their diagnostic criteria using epidemiological analysis and thus there is no analysis of the diagnostic accuracy of diagnostic criteria used. Thus, Marran et al.,37 define AI referring to Daum12 study as having an amplitude of accommodation at least 2 D below Hofstetter's age-based norms on the Donder's monocular push-up test. Dwyer4 makes a classification for accommodative disorders based on optometric literature but without an explanation of the values of accommodative tests used for diagnosing anomalies. The reader of this study must make an effort to understand which signs need to be present to affirm a particular diagnosis. In addition, other authors as Chrousos et al.,45 report a series of ten healthy patients with AI making only an analysis of their vision findings.
These results show that there is certain evidence according to diagnostic criteria for accommodative anomalies. Although there are three studies29,38,41 which test the diagnostic accuracy for clinical signs, QUADAS-2 tool results show that there are certain shortcomings in the design, conduct and reporting of these studies. Good results are shown about the population and flow and timing items. Patients were consecutively chosen in two studies29,41 since the other analyzed invited population. All studies have no risk of bias when considering the item of flow and timing, as all patients received the index test and reference standard, all were included in the analysis and there were a good time interval between index tests and reference standard. However, there is a high risk of bias when considering reference standard and index test. Thus, only one study38 interprets reference standard without knowledge of the results of the index test. According to index test, none of the studies interpret the index test without the knowledge of reference standard. However, these studies have good applicability when considering patients who would benefit of these considerations.
With this quality analysis we should only state that there is certain evidence to use the amplitude of accommodation and monocular accommodative facility for diagnosing accommodative insufficiency. Similarly, for accommodative excess there is certain evidence, although with a risk of bias, that a high positive relative accommodation should be used as a clinical diagnostic sign.
According to the role played by patients’ symptomatology, the review shows that all the studies consider the presence of symptoms essential to diagnose anomalies. However, there are differences in the way of asking about symptoms as well as to calibrate their severity. Several studies manage symptoms according to the authors’ criteria. Some authors simply refer to symptoms or asthenopia in general.4,29,41,45 Other studies use small patient symptom questionnaires,38 and others simply compile or present the symptoms described by the patients.42–44 However, there are four studies which refer to the use of a validated symptom questionnaire.28,37,39,40 Particularly, three of them are studies whose purpose is to validate a questionnaire of symptoms. Rouse et al.,39 perform a ROC analysis to test the ability of CISS V-15 to discriminate between patients with convergence insufficiency and those with normal binocular vision. Borsting et al.,40 use the sensitivity and specificity analysis to test the CISS score, and Borsting et al.,28 use the sensitivity and specificity analysis and Odds ratio to test the CIRS score. All of these three studies28,39,40 conclude that the CISS is a valid and reliable instrument for evaluating symptoms in adults and children with CI. The appropriate epidemiological methods applied establish that there is a validated symptom questionnaire for convergence insufficiency. However, the lack of specific questionnaires for the other accommodative and binocular anomalies makes difficult the task of calibrating the severity of their symptoms which may be useful for diagnostic purposes.
QUADAS-2 results for articles in which a validation of a questionnaire for convergence insufficiency has been studied also show certain quality rating. For articles related to symptoms28,39,40, we can observer that there is a risk of bias when considering index test and patient selection. This is because all three studies interpret the index text (the questionnaire) with knowledge of the results of the reference standard (diagnosis of convergence insufficiency) and furthermore because in any case patients of these three studies were consecutive or randomized. These results imply that in general there is certain concern regarding applicability related to patient selection. These results also suggest that there is certain evidence according to a validated questionnaire for convergence insufficiency that should be used when considering patients’ symptomatology for this condition.
In addition to the lack of diagnostic validity, the review also reveals the coincidences and differences according to the clinical signs and the cut-off used by each author.
As we can observe, to diagnose CI all the authors4,28,37,39–41,44 agree to consider the exophoria at near vision. The other clinical tests most commonly used are the PFV and the NPC. For the other binocular dysfunctions, the tests most frequently mentioned are the phoria measurement, the fusional vergences for CE and DI, and the AC/A ratio for CE and DI. However, the other binocular tests are used less frequently. We can deduce that the authors consider the phoria measurement necessary to diagnose a binocular anomaly, and the tests classified as monocular and binocular at the same time, such as BAF, MEM dynamic retinoscopy and PRA and NRA, are not so required.
Similarly, for AI, all the authors4,29,37,38,41,45 use the low amplitude of accommodation (AA) to diagnose it. The other clinical tests commonly used are MEM retinoscopy, BAF and PRA.4,29,41 However, only two authors29,41 mention the monocular accommodative facility (MAF) which is an exclusively accommodative test. The same occurs with AE in which the MEM retinoscopy is the most frequently used clinical sign4,41,42 but the MAF testing is not as commonly used as it should be expected for an accommodative dysfunction, with only one study in which this test is used.41 These results highlight the need to investigate the role of accommodative tests made under binocular conditions to diagnose accommodative anomalies, as well as to establish whether they should be used more or less frequently than exclusively monocular tests.
According to the cut-offs, this review also shows the lack of uniformity in the cut-off points used to decide if a patient fails a particular test. The most significant examples are for CI and AI. In the case of CI there are four different cut-off points used for exophoria at near vision, ranging from 5Δ28,37,39,40 to 16Δ.44 Thus, some studies use the cut-off of having a greater exophoria at near than distance of ≥4 Δ.28,37,39,40 Others consider an exophoria at near >6 Δ.41 One study4 uses the cut-off of 12 Δ and the other author44 classifies CI based upon the angle of deviation at far. If at far is ≤5 Δ of exophoria, it must be at near at least 4 Δ more exo. If the angle of deviation at far is ≥6 Δ of exophoria, it must be at near at least 10 Δ more exo. These differences also occur for NPC, considering a receded NPC with values of ≥6 cm,37,39,40 ≥7.5 cm28 and >10/17.5 cm for break and recovery.41
The same happens with the low AA used for diagnosing AI. Some authors consider that the patient must have an AA 2 D below Hofstetter's minimum age formula 15 – 0.25 × age.29,37,41 Others consider having 3 D below the Hofstetter's minimum age formula.4 There is one study in which the authors use a monocular AA < 8 D and <10 D for binocular AA.38 And there are other authors who consider that it is necessary to have an AA below the normal for the patient's age, but do not specify which value.45
Obviously, discrepancies about the clinical signs and their cut-offs may cause the same patient to be diagnosed with a particular anomaly or not, depending on the criteria applied.
Another important issue observed in this review is related to the limitation of the type of population used in the studies. Seven reports reveiwed28,29,39–42,44 examine sample populations obtained from optometric clinics or centers. As these populations are selected and not randomized they do not represent the general population. Furthermore, only two studies37,38 analyze school populations, which are considered less biased. It should be taken into account that the population studied at school is very similar to the general child population. Accordingly, the conclusions reached for each study can only be applied in the context of these populations and should not be extrapolated to the general population.
Conclusions
In summary, this review reveals that although the authors apply a wide range of diagnostic criteria, there is a lack of uniformity for the type and number of clinical signs used for each dysfunction as well as for the cut-off used.
There is certain evidence to use the amplitude of accommodation and monocular accommodative facility for diagnosing accommodative insufficiency and a high positive relative accommodation for accommodative excess. However, there is a lack of studies which have evaluated the diagnostic accuracy of clinical signs used for binocular anomalies so that the evidence about the diagnostic clinical signs cannot be found within papers that have been published over the last years. This implies that currently used clinical diagnostic criteria should assess diagnostic validity.
The review also shows that there is evidence according to a validated symptom questionnaire for convergence insufficiency with a lack of specific questionnaires to calibrate the severity of symptoms for the other accommodative and nonstrabismic binocular anomalies.
Further research should be carried out on accommodative and binocular dysfunctions, with properly designed studies, with good epidemiological analysis to validate the criteria necessary for the accurate diagnosis of general binocular disorders. It should be necessary not only for professionals, as they will be sure of a particular diagnosis, but also for patients as they will benefit from receiving the best treatment option.
Conflicts of interest
The authors declare not to have any conflicts of interest.
References
- 1.Cooper J., Burns C., Cotter S., Daum J., Griffin J., Scheiman M. American Optometric Association; St. Louis: 2006. Care of the patient with accommodative and vergence dysfunction. [Google Scholar]
- 2.Duane A. A new classsification of the motor anomalies of the eye, based upon physiologic principles. Part 2. Pathology. Ann Ophthalmol. 1897;6:247–260. [Google Scholar]
- 3.Tait E.F. Accommodative convergence. Am J Ophthalmol. 1951;34:1093–1107. doi: 10.1016/0002-9394(51)90683-6. [DOI] [PubMed] [Google Scholar]
- 4.Dwyer P. Clinical criteria for vergence accommodation dysfunction. Clin Exp Optom. 1991;74:112–119. [Google Scholar]
- 5.Wick B., London R. Analysis of binocular visual function using tests made under binocular conditions. Am J Optom Physiol Opt. 1987;64:227–240. doi: 10.1097/00006324-198704000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Wick B.C. Horizontal deviation. In: Amos J., editor. Diagnosis and management in vision care. Butterworth-Heinemann; Boston: 1987. pp. 461–510. [Google Scholar]
- 7.Donders F. New Syndeham Society; London: 1864. On the anomalies of accommodtion and refraction of the eye. [Google Scholar]
- 8.London R. Accommodation in ocular assessment. In: Barresi B., editor. Ocular assessment: the manual of diagnosis for office practice. Butterworth-Heinemann; Boston: 1984. pp. 123–130. [Google Scholar]
- 9.Cooper J. Accommodative dysfunction. In: Amos J., editor. Diagnosis and management in vision care. Butterworth-Heinemann; Boston: 1987. pp. 431–454. [Google Scholar]
- 10.Zellers J., Alpert T., Rouse M. A review of the literature and a normative study of accommodative facility. J Am Optom Assoc. 1984;55:31–37. [PubMed] [Google Scholar]
- 11.Scheiman M., Wick B. Lippincott Williams & Wilkins; Philadelphia: 2008. Clinical management of binocular vision. [Google Scholar]
- 12.Daum K. Accommodative dysfunction. Doc Ophthalmol. 1983;55:177–198. doi: 10.1007/BF00140808. [DOI] [PubMed] [Google Scholar]
- 13.Weisz C., How to find and treat accommodative disorders Optometry. 1983;(January):48–53. [Google Scholar]
- 14.Scheiman M., Mitchell G., Cotter S. A randomized clinical trial of treatments for convergence insufficiency in children. Arch Ophthalmol. 2005;123:14–24. doi: 10.1001/archopht.123.1.14. [DOI] [PubMed] [Google Scholar]
- 15.Daum K. Convergence insufficiency. Am J Optom Physiol Opt. 1984;61:16–22. doi: 10.1097/00006324-198401000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Hokoda S. General binocular dysfunctions in an urban optometry clinic. J Am Optom Assoc. 1985;56:560–562. [PubMed] [Google Scholar]
- 17.Scheiman M., Gallaway M., Coulter R. Prevalence of vision and ocular disease conditions in a clinical pediatric population. J Am Optom Assoc. 1996;67:193–202. [PubMed] [Google Scholar]
- 18.Porcar E., Martinez-Palomera A. Prevalence of general binocular dysfunctions in a population of university students. Optom Vis Sci. 1997;74:111–113. doi: 10.1097/00006324-199702000-00023. [DOI] [PubMed] [Google Scholar]
- 19.Lara F., Cacho P., García A., Megías R. General binocular disorders: prevalence in a clinic population. Ophthalmic Physiol Opt. 2001;21:70–74. doi: 10.1046/j.1475-1313.2001.00540.x. [DOI] [PubMed] [Google Scholar]
- 20.Rouse M., Hyman L., Hussein M., Solan H. Frequency of convergence insufficiency in optometry clinic settings. Convergence Insufficiency and Reading Study (CIRS) Group. Optom Vis Sci. 1998;75:88–96. doi: 10.1097/00006324-199802000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Abdi S., Rydberg A. Asthenopia in schoolchildren, orthoptic and ophthalmological findings and treatment. Doc Ophthalmol. 2005;111:65–72. doi: 10.1007/s10633-005-4722-4. [DOI] [PubMed] [Google Scholar]
- 22.Borsting E., Rouse M., Deland P. Association of symptoms and convergence and accommodative insufficiency in school-age children. Optometry. 2003;74:25–34. [PubMed] [Google Scholar]
- 23.Rouse M., Borsting E., Hyman L. Frequency of convergence insufficiency among fifth and sixth graders. The Convergence Insufficiency and Reading Study (CIRS) group. Optom Vis Sci. 1999;76:643–649. doi: 10.1097/00006324-199909000-00022. [DOI] [PubMed] [Google Scholar]
- 24.Dwyer P. The prevalence of vergence accommodation disorders in a school-age population. Clin Exp Optom. 1992;75:10–18. [Google Scholar]
- 25.Letourneau J., Duci S. Prevalence of convergence insufficiency among elementary school children. Can J Optom. 1988;50:194–197. [Google Scholar]
- 26.Pickwell L., Viggars M., Jenkins T. Convergence insufficiency in a rural population. Ophthalmic Physiol Opt. 1986;6:339–341. doi: 10.1016/0275-5408(86)90096-7. [DOI] [PubMed] [Google Scholar]
- 27.Cacho-Martínez P., García-Muñoz Á., Ruiz-Cantero M.T. Do we really know the prevalence of accomodative and nonstrabismic binocular dysfunctions? J Optom. 2010;3:185–197. doi: 10.1016/j.optom.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borsting E., Rouse M.W., De Land P.N. Prospective comparison of convergence insufficiency and normal binocular children on CIRS symptom surveys. Convergence Insufficiency and Reading Study (CIRS) group. Optom Vis Sci. 1999;76:221–228. doi: 10.1097/00006324-199904000-00025. [DOI] [PubMed] [Google Scholar]
- 29.Cacho P., García A., Lara F., Seguí M. Diagnostic signs of accommodative insufficiency. Optom Vis Sci. 2002;79:614–620. doi: 10.1097/00006324-200209000-00013. [DOI] [PubMed] [Google Scholar]
- 30.Granet D., Gomi C., Ventura R., Miller-Scholte A. The relationship between convergence insufficiency and ADHD. Strabismus. 2005;13:163–168. doi: 10.1080/09273970500455436. [DOI] [PubMed] [Google Scholar]
- 31.Grönlund M., Aring E., Landgren M., Hellström A. Visual function and ocular features in children and adolescents with attention deficit hyperactivity disorder, with and without treatment with stimulants. Eye (Lond) 2007;21:494–502. doi: 10.1038/sj.eye.6702240. [DOI] [PubMed] [Google Scholar]
- 32.Simons H., Grisham J. Binocular anomalies and reading problems. J Am Optom Assoc. 1987;58:578–587. [PubMed] [Google Scholar]
- 33.Fletcher R.H., Fletcher S.W. Lippincott Williams & Wilkins; Philadelphia: 2007. Clinical Epidemiology: The Essentials. [Google Scholar]
- 34.Anderton P.J. Implementation of evidence-based practice in optometry. Clin Exp Optom. 2007;90:238–243. doi: 10.1111/j.1444-0938.2007.00153.x. [DOI] [PubMed] [Google Scholar]
- 35.Canadian Task Force on Preventive Health Care New grades for recommendations from the Canadian Task Force on Preventive Health care. CMAJ. 2003;169:207–208. [PMC free article] [PubMed] [Google Scholar]
- 36.Graham A.M. Finding retrieving and evaluating journal and web-based information for evidence-based optometry. Clin Exp Optom. 2007;90:244–249. doi: 10.1111/j.1444-0938.2007.00148.x. [DOI] [PubMed] [Google Scholar]
- 37.Marran L., De Land P., Nguyen A. Accommodative insufficiency is the primary source of symptoms in children diagnosed with convergence insufficiency. Optom Vis Sci. 2006;83:281–289. doi: 10.1097/01.opx.0000216097.78951.7b. [DOI] [PubMed] [Google Scholar]
- 38.Sterner B., Gellerstedt M., Sjöström A. Accommodation and the relationship to subjective symptoms with near work for young school children. Ophthalmic Physiol Opt. 2006;26:148–155. doi: 10.1111/j.1475-1313.2006.00364.x. [DOI] [PubMed] [Google Scholar]
- 39.Rouse M., Borsting E., Mitchell G. Validity and reliability of the revised convergence insufficiency symptom survey in adults. Ophthalmic Physiol Opt. 2004;24:384–390. doi: 10.1111/j.1475-1313.2004.00202.x. [DOI] [PubMed] [Google Scholar]
- 40.Borsting E., Rouse M., Mitchell G. Validity and reliability of the revised convergence insufficiency symptom survey in children aged 9 to 18 years. Optom Vis Sci. 2003;80:832–838. doi: 10.1097/00006324-200312000-00014. [DOI] [PubMed] [Google Scholar]
- 41.García A., Cacho P., Lara F. Evaluating relative accommodations in general binocular dysfunctions. Optom Vis Sci. 2002;79:779–787. doi: 10.1097/00006324-200212000-00010. [DOI] [PubMed] [Google Scholar]
- 42.Rutstein R., Daum K., Amos J. Accommodative spasm: a study of 17 cases. J Am Optom Assoc. 1988;59:527–538. [PubMed] [Google Scholar]
- 43.Scheiman M., Gallaway M., Ciner E. Divergence insufficiency: characteristics diagnosis treatment. Am J Optom Physiol Opt. 1986;63:425–431. [PubMed] [Google Scholar]
- 44.Daum K. Characteristics of exodeviations: I. A comparison of three classes. Am J Optom Physiol Opt. 1986;63:237–243. [PubMed] [Google Scholar]
- 45.Chrousos G., O’Neill J., Lueth B., Parks M. Accommodation deficiency in healthy young individuals. J Pediatr Ophthalmol Strabismus. 1988;25:176–179. doi: 10.3928/0191-3913-19880701-07. [DOI] [PubMed] [Google Scholar]
- 46.Whiting P.F., Rutjes A.W., Westwood M.E. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 47.Reitsma J., Rutjes A., Whiting P., Vlassov V., Leeflang M., Deeks J. Assessing methodological quality. In: Deeks J., Bossuyt P., Gatsonis C., editors. Cochrane handbook for systematic reviews of diagnostic test accuracy version 100: the cochrane collaboration. 2009. [Google Scholar]


