Abstract
This study aimed to determine whether the addition of an aminoglycoside to a ß-lactam antibiotic increases the antimicrobial effect during the early phase of Gram-negative severe sepsis/septic shock. A porcine model was selected that considered each animal’s individual blood bactericidal capacity. Escherichia coli, susceptible to both antibiotics, was given to healthy pigs intravenously during 3 h. At 2 h, the animals were randomized to a 20-min infusion with either cefuroxime alone (n = 9), a combination of cefuroxime+tobramycin (n = 9), or saline (control, n = 9). Blood samples were collected hourly for cultures and quantitative polymerase chain reaction (PCR). Bacterial growth in the organs after 6 h was chosen as the primary endpoint. A blood sample was obtained at baseline before start of bacterial infusion for ex vivo investigation of the blood bactericidal capacity. At 1 h after the administration of the antibiotics, a second blood sample was taken for ex vivo investigation of the antibiotic-induced blood killing activity. All animals developed severe sepsis/septic shock. Blood cultures and PCR rapidly became negative after completed bacterial infusion. Antibiotic-induced blood killing activity was significantly greater in the combination group than in the cefuroxime group (p<0.001). Growth of bacteria in the spleen was reduced in the two antibiotic groups compared with the controls (p<0.01); no difference was noted between the two antibiotic groups. Bacterial growth in the liver was significantly less in the combination group than in the cefuroxime group (p<0.05). High blood bactericidal capacity at baseline was associated with decreased growth in the blood and spleen (p<0.05). The addition of tobramycin to cefuroxime results in increased antibiotic-induced blood killing activity and less bacteria in the liver than cefuroxime alone. Individual blood bactericidal capacity may have a significant effect on antimicrobial outcome.
Introduction
Bacterial infections may progress to severe sepsis and septic shock, conditions associated with high mortality rates (20–60%) [1]–[5]. Initial treatment of septic shock includes fluid resuscitation and adequate antibiotic treatment [6]–[8]. In the initial empiric treatment of these severe infections a combination of antibiotics is commonly used to ensure that the causative organism is covered by at least one active drug. However, the advantage of covering the probable pathogen or pathogens with more than one active agent has not been without controversy. Several meta-analyses have failed to demonstrate beneficial effects of combination therapy in severe sepsis and Gram-negative bacteremia [9], [10]. However, a more advanced meta-regression analysis has recently shown that antibiotic combination therapy improves survival and clinical response in patients with life-threatening infections, particularly in those with septic shock [11]. That study was followed by a large retrospective propensity-matched multicenter cohort study evaluating the therapeutic benefit of early combination therapy with at least two antibiotics with activity against the pathogen isolated in patients with septic shock. Significant beneficial effects were observed, especially for ß-lactam antibiotics in combination with aminoglycosides, fluoroquinolones or macrolides [12]. Proposed principal mechanisms have been a synergistic antibacterial effect or immunomodulatory activity. Fluoroquinolones and macrolides have been shown to have direct immunomodulatory effects [13], whereas this effect is less obvious for aminoglycosides [12], [14]. For the ß-lactam/aminoglycoside combination, a faster bacterial clearance may be a more likely mechanism.
Whereas a synergistic effect of the ß-lactam/aminoglycoside combination has extensively been demonstrated in vitro [15], [16], in vivo experimental data are more limited. The in vivo studies have focused on local infections and mainly with Pseudomonas spp., which is a well-known difficult-to-treat organism and endpoints have usually been bacterial growth in organs after several days of treatment [17]–[19]. Increased rate of bacterial clearance in the blood and reduced growth in the organs during the early phase of treatment are probably crucial factors in the treatment of life-threatening severe sepsis and septic shock. To our knowledge, these phenomena have not been studied in either clinical studies or experimental settings.
The aim of this study was therefore to investigate whether the addition of an aminoglycoside to a ß-lactam antibiotic has an effect on the in vivo killing rate of a common Gram-negative pathogen during the early phase of treatment in a porcine intensive care model of severe sepsis/septic shock. Because genetic polymorphism leads to differences in the response to bacterial challenges [20], [21], a secondary aim was to analyze the effect of individual blood bactericidal capacity at baseline on subsequent bacterial growth in the blood and organs.
Materials and Methods
Animals and Ethic Statements
This study included 27 apparently healthy Swedish landrace-breed piglets of both sexes. The Animal Ethics Board in Uppsala, Sweden approved the experiment (permit number C 215/5). The piglets were handled in accordance with the Guide for the Care and Use of Laboratory Animals. All surgery was performed under general anesthesia and efforts were made to minimize suffering. Animals had water and food access ad libitum until 1 h before the experiment.
Anesthesia and Preparations
Anesthesia and ventilation in this study were performed as described in detail elsewhere [22]. In brief, the animals were sedated before transportation and preparations and then mechanically ventilated under intravenous general anesthesia. Acetated Ringer’s solution was administered, resulting in a total fluid administration rate of 15 mL×kg−1×h−1. All preparations were done under aseptic conditions. The following blood vessels were catheterized: auricular peripheral veins, the superior caval vein, the pulmonary artery (Swan Ganz catheter) and a cervical artery. Using vesicostomy, a urine catheter was inserted into the bladder. After completed preparations, the animals were allowed 40 min of stabilization before initiation of the experiment, i.e. the baseline. A bolus of 4% succinylated gelatin solution 30 mL×kg−1 was given 45–60 min before baseline.
Initial respiratory settings were: respiratory rate 25 min−1, inspiratory-expiratory ratio 1∶2, inspired oxygen fraction (FiO2) 0.3, positive end-expiratory pressure (PEEP) 5 cm H2O and tidal volume 10 mL×kg−1. Tidal volume was adjusted before the start of the protocol to result in an arterial partial pressure of carbon dioxide (PaCO2) of 38–41 torr (5.0–5.5 kPa). The ventilator used was either a Servo 900C or a Servo I (Siemens-Elema, Stockholm, Sweden).
To resemble an intensive care setting the animals were treated in accordance with a protocol to maintain vital parameters within preset limits (Table 1). Briefly, arterial partial pressure of oxygen (PaO2) was maintained at >10 kPa, mean arterial pressure (MAP) at ≥60 mm Hg and cardiac index (CI) at ≥2 L×min−1×m−2.
Table 1. Interventions performed to maintain vital parameters within preset limits.
| Parameter | Threshold values for intervention | Interventions |
| PaO2 | <10 kPa first time | Increase FiO2 to 0.6 |
| PaO2 | <10 kPa thereafter | 1. Increase FiO2 to the next level: 0.6→0.8→1.0 |
| AND | ||
| 2. Increase PEEP to the next level: 5→8→10→14 cmH20 | ||
| AND | ||
| 3. Lung recruitment maneuvera | ||
| PaO2 | >30 kPa | Decrease FiO2 to the next level: 1.0→0.8→0.6→0.3 |
| MAP and/or CI | MAP<60 mm Hg and/or CI <2.0 L×min−2×m−2 | Start norepinephrine infusion 0.07 µg×kg−1×min−1. If ongoing norepinephrine infusion, increase rate one step: 0.07→0.13→0.29→0.54 µg×kg−1×min−1 |
| MAP | MAP = MPAP (at <1 h after baseline) | Single dose of 40 µg norepinephrine i.v. |
| MAP | MAP = MPAP (at >1 h after baseline) | 1. Single dose of 20 µg norepinephrine i.v. |
| AND | ||
| 2. Start norepinephrine infusion 0.07 µg×kg−1×min−1. If ongoing, increase rate one step: 0.07→0.13→0.29→0.54 µg×kg−1×min−1 | ||
| AND | ||
| 3. Fluid bolus of 10 mL×kg−1 with 4% succinylated gelatin in normal saline | ||
| AND | ||
| 4. Increase FiO2 to the next level: 0.3→0.6→0.8→1.0 | ||
| AND | ||
| 5. Increase PEEP to the next level: 5→8→10→14 cmH20 | ||
| AND | ||
| 6. Lung recruitment maneuvera | ||
| MAP | >100 mm Hg | If ongoing norepinephrine infusion, decrease rate one step: 0.54→0.29→0.13→0.07 µg×kg−1×min−1 |
PaO2 = arterial partial pressure of oxygen, FiO2 = inspired fraction of oxygen, PEEP = positive end expiratory pressure, MAP = mean arterial pressure, CI = cardiac index, MPAP = mean pulmonary arterial pressure.
PEEP was increased stepwise until a peak pressure of 35 cm H2O was reached. At this point, an inspiratory hold was performed for 10 s. Thereafter, the PEEP was stepwise decreased to the PEEP defined by the protocol. If MAP decreased to the level of the MPAP, the recruitment maneuver was aborted.
Organism
Escherichia coli (E. coli), a common Gram-negative pathogen, was chosen for this study. The strain B09–11822 employed is a clinical isolate obtained from a patient with bloodstream infection and septic shock. This strain is encapsulated and serum resistant (analyzed to be serotype O-rough:K1:H7 at Statens Seruminstitut, Copenhagen, Denmark). In in vitro pilot studies prior to this study this strain demonstrated continued growth in both serum and whole blood from pigs as well as humans (data not shown). Minimal inhibitory concentrations (MICs) for cefuroxime and tobramycin were 4 µg×mL−1 and 0.5 µg×mL−1, respectively (Etest; Biodisk, Solna, Sweden). The bacteria were grown to logarithmic growth phase before the experiment.
Antibiotics
Cefuroxime was chosen as the ß-lactam antibiotic and purchased as Zinacef (GlaxoSmithKline, Solna, Sweden). The aminoglycoside chosen was tobramycin, which was purchased as Nebcina (Meda, Solna, Sweden). These antibiotics were preferred because their porcine pharmacokinetic profiles have been studied and shown to have similarities to those in humans [23]. The antibiotic doses selected are those commonly recommended as maximal doses for the treatment of human clinical sepsis.
Experimental Design
The experimental design of the study was prospective, parallel-grouped, randomized and placebo-controlled. In this non-lethal model an infusion of live E. coli of 5×108 colony-forming units (CFUs) in 20 ml normal saline was administered at baseline via a central vein catheter at a constant infusion rate for 3 h (Figure 1 ). The number of bacteria of the infusate was controlled and the accepted range was 3.5–7.1×108 CFU (8.70±0.15 log10 CFU). To secure that the bacteria remained in log phase the infusate was replaced hourly. Immediately before baseline, physiologic data were recorded and blood and urine samples obtained for laboratory analyses, including quantitative bacterial analysis. At baseline, the sealed envelope technique was applied to randomize the animals to one of three groups. The cefuroxime group received 750 mg cefuroxime in 50 ml saline plus 50 ml saline. The combination group received 750 mg cefuroxime in 50 ml saline plus 7 mg×kg−1 tobramycin in 50 ml saline simultaneously. The control group received placebo in the form of 100 ml saline alone. Antibiotics were given at 2 h as 20-min infusions in separate veins (Figure 1).
Figure 1. Experimental design.
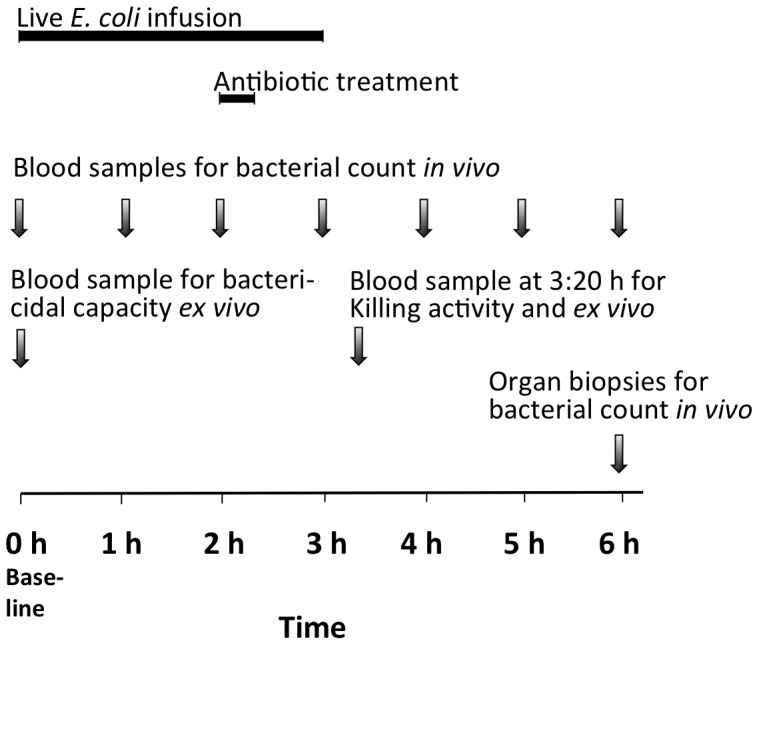
Black bars represent infusions while arrows indicate time points for sampling for bacterial analyses.
Hourly bacterial counts were taken from arterial blood samples (Figure 1). In addition, blood from three animals was analyzed for bacterial count at 15, 30 and 45 min after completion of the bacterial infusion.
Physiologic data were recorded and blood samples for the determination of hypoperfusion and organ dysfunction collected hourly. Blood samples for antibiotic concentrations were obtained at 3 h after baseline and then hourly. At 6 h after baseline, the animals were killed by a potassium chloride injection. Biopsies for bacterial count were obtained under aseptic conditions from standardized localizations in the spleen, right kidney and right lobe of the liver.
Arterial blood was collected for ex vivo experiments at 0 h to determine blood bactericidal capacity at baseline and at 3∶20 h for the antibiotic-induced activity in the blood after 1 h of treatment.
Starting at baseline, heart rate, MAP and mean pulmonary arterial pressure (MPAP) were continuously monitored and registered hourly. Cardiac output, assessed using the thermodilution method, and urine output were registered at the same time points. Calculations from registered values generated left ventricular stroke index (LVSWI) and CI using their regular formulas [24].
Arterial blood was analyzed for pH, gas tensions (PaO2, PaCO2), oxygen saturation and hemoglobin, using an ABL 5 and a Hemoximeter (Radiometer, Brønhøj, Denmark). Lactate concentration was analyzed by an i-STAT 1 (Abbott Scandinavia, Solna, Sweden). Urine and plasma creatinine analyses as well as plasma tobramycin were performed on an Architect Ci8200 analyzer (Abbott Scandinavia). Plasma concentration of cefuroxime was analyzed by reversed phase high-performance liquid chromatography and detected by mass spectrometry on an Agilent 1100 LC-MS (Agilent Technologies, Palo Alto, CA, USA).
Determination of the Bacterial Killing Rate
In vitro bacterial killing
To compare the magnitude of the in vivo effects of the combination treatment the in vitro effect of the addition of tobramycin to cefuroxime was analyzed. Bacteria were resuspended to 107 CFU×mL−1 in a Lysogeny broth (LB) medium containing cefuroxime (0 or 10 mg×L−1) or cefuroxime (10 mg×L−1)+tobramycin (20 mg×L−1) in 37°C. The pharmacodynamic parameter to predict efficacy for cephalosporins is concentration-independent and related to the time during which the drug concentration is greater than the MIC [25]. To achieve a maximal cephalosporin effect the cefuroxime concentration chosen was well above the MIC. The pharmacodynamic effect of aminoglycosides is associated with the peak concentration [26] and the tobramycin concentration chosen was in the magnitude of that expected clinically. Bacterial survival was determined after 0–6 h by plating serial dilutions on LB agar plates. Colonies were counted the following day. The detection limit was 10 CFU×mL−1. The experiment was performed in triplicate.
In vivo bacterial killing
Bacterial count in blood was determined hourly by plating 0.1 ml blood in triplicate (Figure 1). Organ biopsies of 1–2 g obtained at the end of the experiment were placed in 3 mL phosphate-buffered saline and homogenized for 4 min in a Stomacher 80 Biomaster (Seward Ltd, West Sussex, England) and 0.2 ml of each solution was plated in triplicate to determine viable count. The detection limit was 10 CFU×g−1.
Blood ex vivo bactericidal capacity of the animals at baseline
To determine the blood bactericidal capacity at baseline lithium-heparinized blood was obtained before infection and inoculated ex vivo with 105 CFU×mL−1 E. coli in duplicate. Viable counts were plated after 0 and 6 h incubation at 37°C. The accepted range of the start inoculum was 5±0.15 log10 CFU×mL−1. The bactericidal capacity was assessed by the log10 count at 6 h.
Blood ex vivo killing activity of the animals after 1 h of treatment
Lithium-heparinized blood was drawn at 3∶20 h for determination of the ex vivo antibiotic-induced killing activity of the blood, 1 h after completion of the infusions of antibiotics or saline. The blood was inoculated with 105 CFU×mL−1 E. coli in duplicate and incubated in 37°C. The accepted range of the inoculum was 5±0.15 log10 CFU×mL−1. Viable count was determined hourly.
Quantitative PCR
DNA was extracted from 600 µl whole blood using a High Pure PCR template preparation kit (Roche diagnostics, Mannheim, Germany). To generate a standard curve different concentrations of E. coli B09–11822 (0–107 CFU×mL−1) were added to uninfected whole blood from which DNA was extracted as described above. The detection limit of the assay was 10 CFU×mL−1. Primers fwd-(5′-tagcaaacgttctattggtgc-3′) and rev-(5′-catccagacgataagcatgagca-3′) directed against the K1 capsule gene were used as previously described [27]. Amplification was done in a 20 µl reaction mixture containing 10 µl template DNA and 75 nM of each primer in SYBR Green Master Mix (Roche diagnostics GmbH, Mannheim, Germany). Each reaction was run in duplicates. A touchdown PCR protocol was used to increase sensitivity. The following conditions were applied: an initial denaturation step at 95°C for 10 min, four cycles at 95°C for 10 s, 66°C for 30 s, 72°C for 1 min, followed by four cycles with an annealing temperature of 64°C, four cycles with an annealing temperature of 62°C and 40 cycles with an annealing temperature of 63°C. Bacterial DNA concentration was expressed as CFU equivalents×mL−1.
Three animals in each group were assigned for the addition of hourly quantitative PCR analysis of the arterial in vivo blood. From the ex vivo blood killing activity experiment, blood from three animals in each group was selected for quantitative PCR analysis.
Calculations and Statistics
The difference in bacterial growth in the organs between the combination and cefuroxime regimen alone was chosen as primary endpoint. Because the logarithmic growth of bacteria approximates to normal distribution, Student’s t test was used in the comparison of bacterial growth. With nine animals in each group, a power of 0.8, an α-error of 0.05 and a standard deviation of 20%, the detectable difference was at least 30%. In the correlation analysis the Spearman rank order correlation was employed because the effect of the antibacterial treatment resulted in non-normally distributed organ bacterial counts when all three groups were combined. Statistica (StatSoft, Tulsa, OK, USA) was used for the statistical calculations and a p<0.05 was considered statistically significant.
Results
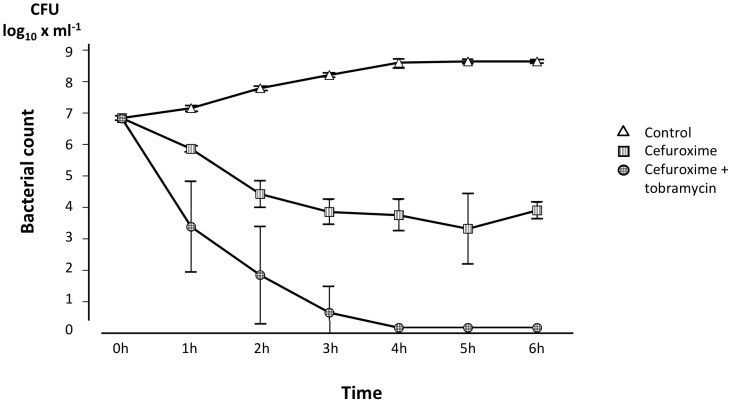
In vitro Bacterial Killing
The bacterial killing rate in vitro is depicted in Figure 2. Maximal bactericidal activity was achieved after 5 h of cefuroxime exposure in a concentration well above MIC. The addition of tobramycin in the concentration of 20 mg×L−1 was found to reach similar bactericidal activity already after 1 h.
Figure 2. In vitro bacterial killing rate of the live E. coli strain used in the experiment.
The bacteria were exposed to cefuroxime 10×L−1 alone, the combination of tobramycin 20 mg×L−1 and cefuroxime 10 mg×L−1 and control medium. The cefuroxime concentration chosen was well above the MIC, which should result in a maximal cephalosporin effect. The tobramycin concentration was >10 times the MIC and in the magnitude of that expected in clinical practice. Values are mean±SE (n = 3 for each treatment).
Animal Experiment
After start of the bacterial infusion, all animals developed signs of severe sepsis/septic shock with deteriorated circulation as manifested by increases in MPAP, decreases in CI and the need for vasopressor support in 12 animals and respiratory interventions in 16. Hypoperfusion was demonstrated by a modest increase in arterial blood lactate of 38% and organ dysfunction by reductions in PaO2/FiO2, creatinine clearance and LVSWI of 41%, 53% and 38% of baseline values, respectively (Table 2). There were no noteworthy differences between the groups (data not shown).
Table 2. Physiological and laboratory parameters reflecting circulation, hypoperfusion and organ dysfunction (n = 27).
| Time | MAP | CI | MPAP | Lactate | PaO2/FiO2 | Creatinine clearance | LVSWI |
| mm Hg | L×min−1×m−2 | mm Hg | mmol×L−1 | kPa | mL×min−1 | g×m−2 | |
| 0 h | 91±11 | 5.7±0.9 | 21±4 | 1.6±0.7 | 61±8 | 150 (88–196) | 56±11 |
| 1 h | 87±16 | 4.0±1.0 | 35±6 | 1.7±0.7 | 59±10 | 165 (77–216) | 41±12 |
| 2 h | 94±15 | 3.4±0.9 | 36±7 | 2.0±1.0 | 52±12 | 75 (33–99) | 40±13 |
| 3 h | 93±18 | 2.9±0.6 | 40±7 | 2.2±1.0 | 41±12 | 96 (64–117) | 34±13 |
| 4 h | 97±14 | 3.0±0.5 | 34±8 | 1.8±0.5 | 39±12 | 77 (54–94) | 37±8 |
| 5 h | 92±17 | 3.3±0.7 | 33±8 | 1.5±0.6 | 40±15 | 61 (47–76) | 36±8 |
| 6 h | 87±19 | 3.5±0.7 | 32±9 | 1.3±0.5 | 36±16 | 70 (50–88) | 35±11 |
Values are mean±SD, except creatinine clearance, which is given as median (interquartile range).
MAP = mean arterial pressure, CI = cardiac index, MPAP = mean pulmonary arterial pressure, PaO2 = arterial partial pressure of oxygen, FiO2 = inspired fraction of oxygen, LVSWI = left ventricular stroke work index.
Table 3 summarizes body weight, dose of infused bacteria, blood bactericidal capacity at baseline and in vivo blood bacterial count at 2 h, just before antibiotic treatment. No differences were observed between the groups in body weight or bacterial dose. A lower bactericidal activity of the blood was found, as manifested by a higher bacterial count at 6 h in the control group as compared with the other two groups (p = 0.08 and 0.03 vs. the cefuroxime and combination group, respectively). Bacterial concentrations at 2 h just before the start of the antibiotic treatment were also lower in the cefuroxime group compared with the combination (p = 0.01) and control (p = 0.003) groups. Bacterial count at 3 h was similar to that noted at 2 h and the same differences were seen (data not shown). Antibiotic concentrations are demonstrated in Table 4.
Table 3. Body weight, dose of infused E. coli, bactericidal capacity of the blood at baseline and in vivo blood bacterial count before start of antibiotic treatment at 2 h (mean±SD).
| All animals | Cefuroxime | Cefuroxime+tobramycin | Control | ||
| n = 27 | n = 9 | n = 9 | n = 9 | ||
| Body weight, kg | 24.8±2.7 | 24.9±2.0 | 24.6±4.3 | 25.0±1.2 | |
| Dose of infused bacteria, log10 CFU | 8.72±0.05 | 8.71±0.06 | 8.72±0.05 | 8.71±0.04 | |
| Blood bactericidalcapacity at baseline | Bacterial count at 0 h, log10 CFU×ml−1 | 4.87±0.06 | 4.89±0.07 | 4.88±0.06a | 4.84±0.04 |
| Bacterial count at 6 h, log10 CFU×ml−1 | 4.41±1.50 | 3.93±1.90 | 3.86±1.39a , b | 5.26±1.03 | |
| Blood bacterial count in vivo at 2 h, log10 CFU×ml−1 | 2.94±0.29 | 2.70±0.28b , c | 2.99±0.15a , b | 3.13±0.24 | |
n = 8. Start inoculum in one animal outside the accepted limits (see methods).
significant vs. control group, p<0.05.
significant vs. the combination group, p<0.05.
Table 4. Plasma concentration of cefuroxime and tobramycin (mean±SD).
| Time | Cefuroxime | Tobramycin | |
| Cefuroxime group mg×L−1 | Cefuroxime + tobramycin group mg×L−1 | Cefuroxime + tobramycin group mg×L−1 | |
| n = 9 | n = 9 | n = 9 | |
| 3 ha | 10.0±4.2 | 11.1±6.6 | 13.8±2.9 |
| 4 h | 3.6±1.6 | 4.1±3.6 | 7.9±2.2 |
| 5 h | 1.2±0.6 | 1.8±2.1 | 5.1±1.4 |
| 6 h | 0.6±0.4 | 0.9±1.2 | 3.7±1.3 |
time after baseline, i.e. 1 h after start of a 20-min infusion of antibiotics.
After completion of the bacterial infusion, there was a rapid bacterial clearance in all groups, including the controls, with no live bacteria detectable at 15 min post-infusion or later. Thus, no differences in the bacterial killing rate could be detected. However, in blood sampled at 3∶20 h, i.e. 1 h after administration of antibiotics, the ex vivo blood killing activity in the animals treated with the combination of a ß-lactam antibiotic and an aminoglycoside was markedly bactericidal, whereas blood from cefuroxime-treated animals exhibited a more gradual killing (Figure 3).
Figure 3. Ex vivo killing activity in blood obtained from treated animals.
Bacterial count at various time points after the addition of live E. coli to a concentration of 1×105 CFU×mL−1 to blood obtained from animals treated with cefuroxime alone or the combination of cefuroxime and tobramycin and from control animals at 3∶20 h, i.e. 1 h after completion of the administration of treatment. Values are mean±SE (n = 9 in each group).
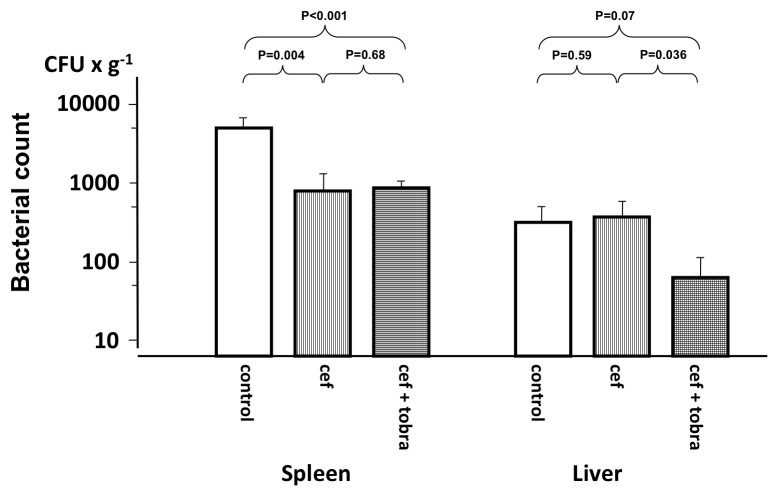
At the end of the experiment, growth of bacteria was seen in the liver and spleen; growth in the kidney was not detected in any of the animals. In the spleen both cefuroxime and the combination reduced growth significantly but there was no difference between the two groups (Figure 4). Growth of bacteria was lower in the liver than in the spleen (p<0.001 in the control group) and the combination regimen resulted in a significantly lower bacterial count than cefuroxime alone, which did not demonstrate any effect in comparison with the control group.
Figure 4. Bacterial count in the spleen and liver at the end of the experiment.
Animals treated 4[61] or the combination of cefuroxime and tobramycin (cef+tobra) and control animals. Values are mean±SE (n = 9 in each group).
Bacterial growth in the organs was not significantly related to body weight or dose of infused bacteria within the dose limits (Table 5). In contrast, growth in the spleen was associated with blood bacterial count at 2 and 3 h and with the blood bactericidal capacity at baseline. Although there was a correlation to growth in the spleen, growth in the liver was not similarly linked to blood bacterial count and blood bactericidal capacity. However, if analysis were performed only in the control animals not exposed to antibiotics, correlation coefficients for blood bactericidal capacity and growth in the spleen and liver were −0.43 and −0.33, respectively. In addition, blood bacterial count at 2 and 3 h correlated negatively to blood bactericidal capacity at baseline (Table 5).
Table 5. Spearman rank correlation between bacterial growth in the organs and body weight, dose of infused bacteria, blood bactericidal capacity at baseline and blood bacterial count in vivo at 2 and 3 h.
| Bodyweight | Dose of infusedbacteria | Blood bac-tericidalcapacity at baseline | Blood bac-terialcount at 2 h | Blood bac-terialcount at 3 h | Growth in theliver | |
| Growth in the spleen | −0.30 | −0.04 | −0.42* | 0.45* | 0.41* | 0.40* |
| Growth in the liver | −0.21 | −0.10 | −0.28 | −0.08 | −0.00 | – |
| Blood bac-terial countat 2 h | −0.31 | 0.10 | −0.41* | – | 0.94* | |
| Blood bac-terial countat 3 h | −0.36 | 0.10 | −0.46* | – |
*denotes a correlation coefficient that is higher than that required for p<0.05.
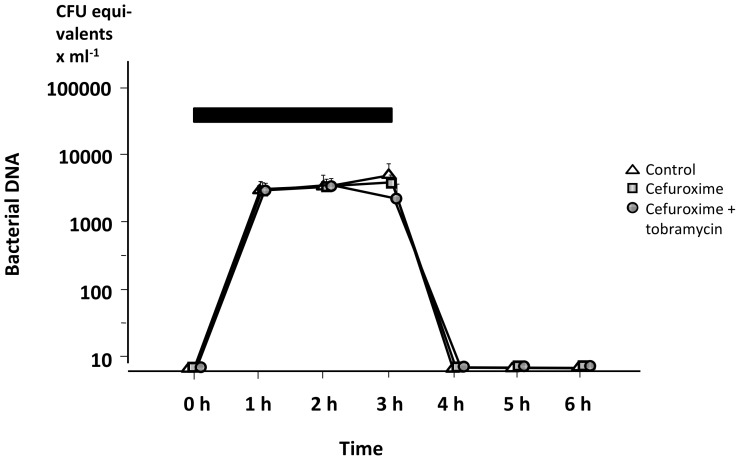
As demonstrated in Figure 5, there was a rapid fall in bacterial DNA in arterial in vivo blood after completion of the infusion of bacteria, irrespective of treatment. No bacterial DNA was found in blood additionally sampled from two animals every 15 min during the first hour (data not shown). In contrast, in blood from the ex vivo killing activity experiments no similar bacterial DNA reduction was detected in any of the groups, not even in the combination group in which the bacterial killing rate was high (Figure 6).
Figure 5. In vivo bacterial DNA in the blood of treated animals.
The treatment was either cefuroxime alone, a combination of cefuroxime+tobramycin, or saline (control), during the 6 h experiment. Black bar denotes the infusion of live E. coli. The quantity of bacterial DNA is expressed as CFU equivalents. Values are mean±SE (n = 3 in each group).
Figure 6. Bacterial DNA in the blood after ex vivo addition of live E. coli.
Bacteria added to a concentration of 1×105 CFU×mL−1 to blood obtained from animals treated with cefuroxime alone or the combination of cefuroxime and tobramycin and from control animals at 3∶20 h, i.e. 1 h after completion of the administration of treatment. The time points for sampling are the same as those in Figure 3, in which the antibiotic-induced killing activity significantly differed between the groups. The quantity of bacterial DNA is expressed as CFU equivalents. Values are mean±SE (n = 3 in each group).
Discussion
The addition of an aminoglycoside to a ß-lactam antibiotic has been widely used for years in the treatment of severe sepsis and septic shock. However, its role has been controversial because of aminoglycoside-induced nephrotoxic and ototoxic side effects [28]–[31] and it is not clear whether the potential adverse reactions override the advantages of the combination [32], [33]. One area considered especially important to readdress is whether this combination confers benefits beyond broadening the antimicrobial spectrum [32]. In the presence of the difficulties to perform prospective randomized clinical trials in patients with these life-threatening intensive care unit (ICU) infections within the time frame available for initiation of antibiotic treatment [8], clinically relevant experimental studies are essential.
The model used in this study was designed to focus on the bacteriological consequences of bacteria that have entered the bloodstream during the early phase of severe sepsis/septic shock. In our pilot experiments there was a strong dose effect with a substantial mortality rate when the dose exceeded 109 bacteria/3 h and therefore the variation of the dose of bacteria was kept at a minimum (Table 3). The intensive care protocol increases the clinical relevance of the study by adding the effects of sedation, mechanical ventilation and vasopressors on the innate immune response [34]–[38]. All animals developed severe sepsis with organ dysfunction necessitating intensive care. In pilot experiments biopsies from different tissues have been cultured and the only organs that demonstrated growth were the spleen and liver. In the final protocol kidneys were included as a control for sterility. Because several clinical studies have shown that treatment with an aminoglycoside alone results in worse outcome compared with treatment with ß-lactam antibiotics [39], [40], no tobramycin arm was included in the protocol. The cefuroxime concentration profile was consistent with that in patients with a sepsis-induced increase in extracellular volume and a slightly augmented renal clearance often observed during the initial phase in younger patients with activated systemic inflammatory response [41]. The tobramycin concentration was slightly lower than that reported from ICU patients but well above the pharmacodynamic target of a Cmax/MIC ratio of >10 [42], [43]. Thus, taken together, the concentrations achieved in the present model were clinically relevant to permit the same pharmacodynamics effects as those expected in patients with severe sepsis/septic shock after the first dose.
Additional to the bacterial dose, several factors may affect the number of bacteria in the blood at the time of treatment. In Table 5 a significant association to the blood bactericidal capacity at baseline and blood bacterial count at 2 h is demonstrated. Despite this and similar blood bactericidal capacities, there were a higher number of bacteria in the blood of the animals in the combination group than in the cefuroxime group at 2 h, the time when treatment was initiated (Table 3). Although standardized efforts were made to keep infused bacteria in the log phase and metabolically active, a difference in viability is probably the most likely source of explanation to this difference. However, even with a higher bacterial count at the start of antibiotic treatment, the addition of tobramycin resulted in significantly lower growth in the liver at the end of the experiment (Figure 4), indicating a beneficial antimicrobial effect of the combination treatment. In addition, combination treatment resulted in a considerably increased blood ex vivo killing activity (Figure 3).
An extremely rapid in vivo clearance of live bacteria from the blood with no relapse during the study period was observed in all animals, including the controls. The rapid bacterial clearance is further highlighted by the bacterial DNA analyses demonstrating that bacterial DNA was present in a nearly constant concentration after bacterial killing ex vivo, whereas none was detectable in vivo once the bacterial infusion had been completed (Figures 5 and 6). The implication of this finding is not clear but during the initial phase of severe sepsis both live and killed bacteria seemed to be rapidly eliminated from the circulation. This rapid elimination may help explain the surprisingly low sensitivity of bacterial PCR tests in suspected sepsis [44], [45]. The prompt elimination might have been caused by an intact and effective innate immune response in the otherwise healthy animals. In contrast, the elimination rate of both live bacteria and bacterial DNA might be slower in patients and experimental animals with more prolonged processes and increasing anti-inflammatory responses. However, this possibility needs further investigation.
Bacterial count in the liver was more than one log10 lower than in the spleen. At the end of the experiment, the bacteria are most probably located intracellularly in the phagocytic cells of the organs, where it is possible to escape from extracellularly distributed antibiotics. It may be speculated that the difference in bacterial count might be due to dissimilarities in the set up of these cells in the two organs. In the spleen bacteria leave the circulation in the red pulp and enter an open blood system without endothelial lining. In this compartment a large number of macrophages are residing that are well prepared for phagocytosis of bacteria before they pass through the endothelial slits of the splenic venous sinuses and re-enter the circulation [46], [47]. In the liver the Kupffer cells protrude into the lumen of the hepatic sinusoids and bacteria are mainly taken up directly from the circulating blood during bacteremia without any filtration or trapping mechanisms [48]. Thus, such a process may explain the lower bacterial uptake in the liver than in the spleen.
In the spleen cefuroxime alone and the combination both resulted in a significant decrease in bacterial count of similar magnitude, whereas in the liver the combination reduced bacterial count significantly more than cefuroxime alone (Figure 4). Free antibiotic concentrations in the extracellular fluid of different organs have been demonstrated to approximate those in plasma [49]. However, for cefuroxime alone to reach an identical killing activity as the combination, the bacteria have to be exposed for more than 3 h (Figure 3). Exposure to antibiotics in the liver must have been shorter to permit the superior blood ex vivo killing activity of the combination to play a role. Although we noted rapid elimination of bacteria from the blood, our data indicate that antibiotic exposure in the liver was long enough for the combination to exert its antimicrobial effect before the bacteria were fully phagocytized and inaccessible for antibiotics.
The blood killing activity ex vivo and the results from the liver indicate an antimicrobial advantage with the combination, whereas results from the spleen do not. Yet, it must be emphasized that growth in the spleen correlated significantly to the bacterial count in the blood before administration of treatment (Table 5) and that the higher amount of bacteria at this time point in the combination group (Table 3) might have masked a smaller difference in splenic bacterial growth in favor of the combination. Moreover, antimicrobial killing in the spleen might have occurred earlier in the combination group and, if so, it cannot be excluded that this might also be of some importance.
Several in vitro studies have demonstrated synergism between ß-lactam antibiotics and aminoglycosides [32], [50]. However, different host defense mechanisms play important roles and in vitro results are not always transferrable to the in vivo situation. In immunocompetent animal models previous studies have examined and compared single versus combination therapy of ß-lactam antibiotics and aminoglycosides for the treatment of Gram-negative bacterial infections in peritoneal infection [17], [51]–[53], pneumonia [54], [55], pyelonephritis [56] and endocarditis [57]–[59]. With few exceptions, these studies indicate that the combination of ß-lactam antibiotics and aminoglycosides results in improvements of either microbiological results or survival. Whereas these studies focus on prolonged treatment, the present study aims at empirical early treatment. In the absence of prospective randomized clinical trials the present findings are of clinical relevance and lend strong support to the results of the studies by Kumar et al [11], [12], indicating that the addition of an aminoglycoside to a ß-lactam antibiotic may result in beneficial antimicrobial effects in addition to merely broadening the antibacterial coverage.
This study has some potential limitations. The clot implantation technique of the bacteria into the peritoneum might have resulted in an even more clinical relevant model [60]. However, such a model first results in a local infection, which subsequently might be followed by a variable bacteremia. To maximally standardize the challenge of bacteria within the bloodstream and the development of severe sepsis/septic shock the intravenous administration route was chosen. Furthermore, in clinical practice cefuroxime has often been replaced by newer cephalosporins. Still, the pharmacodynamic effect on cephalosporin-susceptible bacteria is the same regardless of the cephalosporin used, and the reason for choosing cefuroxime was its known porcine pharmacokinetic profile with striking similarities to that in humans [23].
Conclusion
Bacteria and gene fragments are rapidly eliminated from the circulation, regardless of the treatment. The beneficial pharmacodynamic effects of the combination of a ß-lactam antibiotic and an aminoglycoside seen in vitro were also observed in the early phase of severe sepsis and septic shock. Furthermore, the individual blood bactericidal effect may confound the results in this type of experiment and hence should be taken into account when interpreting the findings.
Acknowledgments
The authors thank Monica Hall and Anders Nordgren for excellent technical assistance.
Funding Statement
The R&D funds of Uppsala University Hospital, the Swedish Research Council (2010–3826) and the Olinder-Nielsen Family fund contributed with financial support. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, et al. (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101: 1644–1655. [DOI] [PubMed] [Google Scholar]
- 2. Martin GS, Mannino DM, Eaton S, Moss M (2003) The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 348: 1546–1554. [DOI] [PubMed] [Google Scholar]
- 3. Engel C, Brunkhorst FM, Bone HG, Brunkhorst R, Gerlach H, et al. (2007) Epidemiology of sepsis in Germany: results from a national prospective multicenter study. Intensive Care Med 33: 606–618. [DOI] [PubMed] [Google Scholar]
- 4. Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, et al. (2010) The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med 36: 222–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brun-Buisson C, Meshaka P, Pinton P, Vallet B (2004) EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med 30: 580–588. [DOI] [PubMed] [Google Scholar]
- 6. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, et al. (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345: 1368–1377. [DOI] [PubMed] [Google Scholar]
- 7. Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, et al. (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34: 1589–1596. [DOI] [PubMed] [Google Scholar]
- 8. Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, et al. (2008) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 36: 296–327. [DOI] [PubMed] [Google Scholar]
- 9. Safdar N, Handelsman J, Maki DG (2004) Does combination antimicrobial therapy reduce mortality in Gram-negative bacteraemia? A meta-analysis. Lancet Infect Dis 4: 519–527. [DOI] [PubMed] [Google Scholar]
- 10. Paul M, Benuri-Silbiger I, Soares-Weiser K, Leibovici L (2004) Beta lactam monotherapy versus beta lactam-aminoglycoside combination therapy for sepsis in immunocompetent patients: systematic review and meta-analysis of randomised trials. BMJ 328: 668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kumar A, Safdar N, Kethireddy S, Chateau D (2010) A survival benefit of combination antibiotic therapy for serious infections associated with sepsis and septic shock is contingent only on the risk of death: a meta-analytic/meta-regression study. Crit Care Med 38: 1651–1664. [DOI] [PubMed] [Google Scholar]
- 12. Kumar A, Zarychanski R, Light B, Parrillo J, Maki D, et al. (2010) Early combination antibiotic therapy yields improved survival compared with monotherapy in septic shock: a propensity-matched analysis. Crit Care Med 38: 1773–1785. [DOI] [PubMed] [Google Scholar]
- 13. Tauber SC, Nau R (2008) Immunomodulatory properties of antibiotics. Curr Mol Pharmacol 1: 68–79. [PubMed] [Google Scholar]
- 14. Goscinski G, Lipcsey M, Eriksson M, Larsson A, Tano E, et al. (2004) Endotoxin neutralization and anti-inflammatory effects of tobramycin and ceftazidime in porcine endotoxin shock. Crit Care 8: R35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Eliopoulos GM, Moellering RC Jr (1982) Antibiotic synergism and antimicrobial combinations in clinical infections. Rev Infect Dis 4: 282–293. [DOI] [PubMed] [Google Scholar]
- 16. Giamarellou H (1986) Aminoglycosides plus beta-lactams against gram-negative organisms. Evaluation of in vitro synergy and chemical interactions. Am J Med 80: 126–137. [DOI] [PubMed] [Google Scholar]
- 17. Comber KR, Basker MJ, Osborne CD, Sutherland R (1977) Synergy between ticarcillin and tobramycin against Pseudomonas aeruginosa and Enterobacteriaceae in vitro and in vivo. Antimicrob Agents Chemother 11: 956–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chusid MJ, Davis SD, Sarff LD (1983) Experimental Pseudomonas aeruginosa sepsis: absence of synergy between ticarcillin and tobramycin. J Lab Clin Med 101: 441–449. [PubMed] [Google Scholar]
- 19. Calandra T, Glauser MP (1986) Immunocompromised animal models for the study of antibiotic combinations. Am J Med 80: 45–52. [PubMed] [Google Scholar]
- 20. Arcaroli J, Fessler MB, Abraham E (2005) Genetic polymorphisms and sepsis. Shock 24: 300–312. [DOI] [PubMed] [Google Scholar]
- 21. Chung LP, Waterer GW (2011) Genetic predisposition to respiratory infection and sepsis. Crit Rev Clin Lab Sci 48: 250–268. [DOI] [PubMed] [Google Scholar]
- 22. Lipcsey M, Larsson A, Eriksson MB, Sjolin J (2006) Inflammatory, coagulatory and circulatory responses to logarithmic increases in the endotoxin dose in the anaesthetised pig. J Endotoxin Res 12: 99–112. [DOI] [PubMed] [Google Scholar]
- 23. Lipcsey M, Carlsson M, Larsson A, Algotsson L, Eriksson M, et al. (2009) Effect of a single dose of tobramycin on systemic inflammatory response-induced acute kidney injury in a 6-hour porcine model. Crit Care Med 37: 2782–2790. [DOI] [PubMed] [Google Scholar]
- 24.Clark C, Harman E (1988) Hemodynamic monitoring: pulmonary artery catheters. Critical Care 3rd ed Philadelphia: Lippincott Williams & Wilkins, 293Y302.
- 25. Kalman D, Barriere SL (1990) Review of the pharmacology, pharmacokinetics, and clinical use of cephalosporins. Tex Heart Inst J 17: 203–215. [PMC free article] [PubMed] [Google Scholar]
- 26. Moore RD, Lietman PS, Smith CR (1987) Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis 155: 93–99. [DOI] [PubMed] [Google Scholar]
- 27. Johnson JR, Stell AL (2000) Extended virulence genotypes of Escherichia coli strains from patients with urosepsis in relation to phylogeny and host compromise. J Infect Dis 181: 261–272. [DOI] [PubMed] [Google Scholar]
- 28. Pannu N, Nadim MK (2008) An overview of drug-induced acute kidney injury. Crit Care Med 36: S216–223. [DOI] [PubMed] [Google Scholar]
- 29. Lopez-Novoa JM, Quiros Y, Vicente L, Morales AI, Lopez-Hernandez FJ (2011) New insights into the mechanism of aminoglycoside nephrotoxicity: an integrative point of view. Kidney Int 79: 33–45. [DOI] [PubMed] [Google Scholar]
- 30. Brummett RE, Fox KE (1989) Aminoglycoside-induced hearing loss in humans. Antimicrob Agents Chemother 33: 797–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Perletti G, Vral A, Patrosso MC, Marras E, Ceriani I, et al. (2008) Prevention and modulation of aminoglycoside ototoxicity (Review). Mol Med Report 1: 3–13. [PubMed] [Google Scholar]
- 32. Tamma PD, Cosgrove SE, Maragakis LL (2012) Combination therapy for treatment of infections with gram-negative bacteria. Clin Microbiol Rev 25: 450–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hanberger H, Edlund C, Furebring M, Giske CG, Melhus A, et al. (2013) Rational use of aminoglycosides-Review and recommendations by the Swedish Reference Group for Antibiotics (SRGA). Scand J Infect Dis 45: 161–175. [DOI] [PubMed] [Google Scholar]
- 34. Castegren M, Lipcsey M, Soderberg E, Skorup P, Eriksson M, et al. (2012) Differences in organ dysfunction in endotoxin-tolerant pigs under intensive care exposed to a second hit of endotoxin. Shock 37: 501–510. [DOI] [PubMed] [Google Scholar]
- 35. Koff W, Fann A, Dunegan M, Lachman L (1986) Catecholamine-induced suppression of interleukin-1 production. Lymphokine research 5: 239. [PubMed] [Google Scholar]
- 36. Madera-Salcedo IK, Cruz SL, Gonzalez-Espinosa C (2011) Morphine decreases early peritoneal innate immunity responses in Swiss–Webster and C57BL6/J mice through the inhibition of mast cell TNF-α release. Journal of neuroimmunology 232: 101–107. [DOI] [PubMed] [Google Scholar]
- 37. Lovett EJ, Alderman J, Munster E, Lundy J (1980) Suppressive effects of thiopental and halothane on specific arms of the immune response. Journal of surgical oncology 15: 327–334. [DOI] [PubMed] [Google Scholar]
- 38. Castegren M, Skorup P, Lipcsey M, Larsson A, Sjolin J (2013) Endotoxin tolerance variation over 24 h during porcine endotoxemia: association with changes in circulation and organ dysfunction. PLoS One 8: e53221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Korvick JA, Bryan CS, Farber B, Beam TR Jr, Schenfeld L, et al. (1992) Prospective observational study of Klebsiella bacteremia in 230 patients: outcome for antibiotic combinations versus monotherapy. Antimicrob Agents Chemother 36: 2639–2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Leibovici L, Paul M, Poznanski O, Drucker M, Samra Z, et al. (1997) Monotherapy versus beta-lactam-aminoglycoside combination treatment for gram-negative bacteremia: a prospective, observational study. Antimicrob Agents Chemother 41: 1127–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Udy AA, Roberts JA, Lipman J (2011) Implications of augmented renal clearance in critically ill patients. Nat Rev Nephrol 7: 539–543. [DOI] [PubMed] [Google Scholar]
- 42. Deziel-Evans LM, Murphy JE, Job ML (1986) Correlation of pharmacokinetic indices with therapeutic outcome in patients receiving aminoglycosides. Clin Pharm 5: 319–324. [PubMed] [Google Scholar]
- 43. Buijk SE, Mouton JW, Gyssens IC, Verbrugh HA, Bruining HA (2002) Experience with a once-daily dosing program of aminoglycosides in critically ill patients. Intensive Care Med 28: 936–942. [DOI] [PubMed] [Google Scholar]
- 44. Avolio M, Diamante P, Zamparo S, Modolo ML, Grosso S, et al. (2010) Molecular identification of bloodstream pathogens in patients presenting to the emergency department with suspected sepsis. Shock 34: 27–30. [DOI] [PubMed] [Google Scholar]
- 45. Josefson P, Stralin K, Ohlin A, Ennefors T, Dragsten B, et al. (2011) Evaluation of a commercial multiplex PCR test (SeptiFast) in the etiological diagnosis of community-onset bloodstream infections. Eur J Clin Microbiol Infect Dis 30: 1127–1134. [DOI] [PubMed] [Google Scholar]
- 46. Groom AC, Schmidt EE, MacDonald IC (1991) Microcirculatory pathways and blood flow in spleen: new insights from washout kinetics, corrosion casts, and quantitative intravital videomicroscopy. Scanning Microsc 5: 159–173 discussion 173–154. [PubMed] [Google Scholar]
- 47. Mebius RE, Kraal G (2005) Structure and function of the spleen. Nat Rev Immunol 5: 606–616. [DOI] [PubMed] [Google Scholar]
- 48. Parker GA, Picut CA (2005) Liver immunobiology. Toxicol Pathol 33: 52–62. [DOI] [PubMed] [Google Scholar]
- 49. Ryan DM, Cars O, Hoffstedt B (1986) The use of antibiotic serum levels to predict concentrations in tissues. Scand J Infect Dis 18: 381–388. [DOI] [PubMed] [Google Scholar]
- 50.Gilbert DN, Legget JE (2009) Aminoglycosides. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7:th ed. New York: Churchill Livingstone. 359–384.
- 51. Nagatomo H, Kakizaki M, Tsuchiya K (1974) Combined action of sulbenicillin and gentamicin. J Antibiot (Tokyo) 27: 199–205. [DOI] [PubMed] [Google Scholar]
- 52. Kitaura K, Mineura K, Nakamizo N, Shiba K, Ohmori M, et al. (1984) Synergistic activity of astromicin and beta-lactam antibiotics against Pseudomonas aeruginosa in vitro and in vivo. J Antibiot (Tokyo) 37: 1681–1686. [DOI] [PubMed] [Google Scholar]
- 53. Valiant ME, Gilfillan EC, Gadebusch HH, Pelak BA (1989) L-658,310, a new injectable cephalosporin. II. In vitro and in vivo interactions between L-658,310 and various aminoglycosides or ciprofloxacin versus clinical isolates of Pseudomonas aeruginosa. J Antibiot (Tokyo) 42: 807–814. [DOI] [PubMed] [Google Scholar]
- 54. Gordin FM, Rusnak MG, Sande MA (1987) Evaluation of combination chemotherapy in a lightly anesthetized animal model of Pseudomonas pneumonia. Antimicrob Agents Chemother 31: 398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Croisier D, Martha B, Piroth L, Chavanet P (2008) In vivo efficacy of humanised intermittent versus continuous ceftazidime in combination with tobramycin in an experimental model of pseudomonal pneumonia. Int J Antimicrob Agents 32: 494–498. [DOI] [PubMed] [Google Scholar]
- 56. Glauser MP (1982) Bonard (1982) Treatment of experimental ascending Escherichia coli pyelonephritis with ceftriaxone alone and in combination with gentamicin. Chemotherapy 28: 410–416. [DOI] [PubMed] [Google Scholar]
- 58. Mainardi JL, Zhou XY, Goldstein F, Mohler J, Farinotti R, et al. (1994) Activity of isepamicin and selection of permeability mutants to beta-lactams during aminoglycoside therapy of experimental endocarditis due to Klebsiella pneumoniae CF104 producing an aminoglycoside acetyltransferase 6′ modifying enzyme and a TEM-3 beta-lactamase. J Infect Dis 169: 1318–1324. [DOI] [PubMed] [Google Scholar]
- 59. Fantin B, Pangon B, Potel G, Vallois JM, Caron F, et al. (1989) Ceftriaxone-netilmicin combination in single-daily-dose treatment of experimental Escherichia coli endocarditis. Antimicrob Agents Chemother 33: 767–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Goldfarb RD, Parker TS, Levine DM, Glock D, Akhter I, et al. (2003) Protein-free phospholipid emulsion treatment improved cardiopulmonary function and survival in porcine sepsis. Am J Physiol Regul Integr Comp Physiol 284: R550–557. [DOI] [PubMed] [Google Scholar]
- 61. Cantu TG, Fantozzi D (1988) Cefuroxime dosage in renal failure. Ann Intern Med 109: 989–990. [DOI] [PubMed] [Google Scholar]