Abstract
We used electrophysiological measures to investigate the effects of obstructive sleep apnea on attention, learning, and memory. Thirty subjects (OSA group, n = 15, control group n = 15) participated in n-back tests, accompanied by P300 recordings, to investigate working memory and attention. The mirror-drawing test was used to study procedural memory, and the trail-making test (TMT) was used to evaluate divided attention and executive function. No significant group difference in reaction time was found in the 0-back and 1-back tests. In the 2-back test, reaction times of patients were longer than those of the control group. No P300 wave was obtained in the OSA group in any (0-, 1-, or 2-back) n-back test. In contrast, in the control group, significant P300 waves were recorded except for the 2-back test. The mirror-drawing scores were unaffected by sleep apnea. There was no difference between groups in the TMT-A test on any of the trials. Although no group difference was found in the first or second trials of the TMT-B test, OSA patients were less successful in learning on the third trial. According to our study results, OSA affects attention and executive function adversely however, we could not detect a significant effect on working or procedural memory.
Introduction
Obstructive sleep apnea (OSA) is a condition characterized by episodes of sleep apnea (cessation of breathing 10 s or longer) or hypopnea (significant reduction in breathing), oxygen desaturation, and frequent arousal [1]. It is one of the most common sleep disorders, found in at least 2–4% of subjects 30–60 years old [2]. Untreated OSA is associated with cardiovascular, metabolic, and cerebrovascular morbidity [1], [3]. OSA patients may have respiratory disturbances, such as hypoxemia and hypercapnia due to airway occlusion. Additionally, a series of neuropsychological deficits has been reported in OSA patients, including impairment in working memory (WM) [4] and long-term memory [5], alterations in a wide spectrum of attentional processes [6], and dysfunction in cognitive executive function [7]. Hypoxemia associated with OSA may be a factor contributing to this neuropsychological impairment.
However, the results of studies on executive function in OSA syndrome are varied. Some studies have reported diminished or impaired cognition, executive function, and attention [8]–[12], whereas others have not [13]–[16]. One method that has been extensively used to assess cognitive and attentional deficits is measurements of event-related potentials (ERP). The most common tasks used in ERP studies is the “oddball paradigm,” in which subjects are requested to respond to target stimuli randomly scattered among non-target ones. [17]. P300 characteristics (i.e., amplitude and latency) have been evaluated using visual or auditory oddball paradigms in a few ERP studies of OSA patients. However, the interpretation of P300 results is controversial [18]–[22].
Distinct aspects of cognition are assessed by different tests (e.g., n-back task, trail-making test, mirror-drawing test) in OSA patients. Memory is usually assessed by the n-back task, which requires maintenance of the previous n stimuli in WM until the present response can be executed [12]. The trail-making test (TMT) is widely used to test executive function, such as complex attention, planning, cognitive set shifting, and response inhibition [23]. The mirror-drawing (MD) test, another commonly used method, analyzes implicit learning abilities and requires fast and repetitive processing of visuospatial stimuli but no acquisition of sequence [24].
Our review of the literature found no study that assessed both electrophysiological and behavioral aspects of cognitive functioning in OSA patients. The aim of this study was to investigate the electrophysiological indications of the effects of obstructive sleep apnea on attention, learning, and memory. We also assessed the relationship of these cognitive characteristics with the apnea-hypopnea index (AHI) and overnight mean O2 saturation (SpO2mean). We believe this is the first reported study to extensively assess cognitive and attentional deficits in OSA patients.
Methods
Ethics Statement
Hacettepe University Institutional Ethical Committee approved the study, and all procedures were carried out according to the Declaration of Helsinki. All subjects provided written informed consent prior to participating in the study.
Experimental Design
All subjects spent one night in the sleep laboratory with polysomnography. The polysomnography setup began at 21∶00 and lights-off time occurred between 22∶00 and midnight. The next morning, participants were awakened at 6∶00 and polysomnography recording equipment was removed. Upon completion of polysomnography recordings, participants meeting all criteria were scheduled to return at a later date (within 2 weeks) for behavioral and electrophysiological tests. At the behavioral test day, we started to record ERPs simultaneously during n-back tasks at 13∶30. It took approximately 1 hour to complete these two tests. After 15 minute break, we continued with the mirror-drawing test and gave another 15 minute break. We completed the behavioral tests with the trail-making A and B tests.
Participants
We prospectively selected full-night polysomnographic studies from the patients’ record registry of Ankara Diskapi Sleep Clinic. Fifteen newly diagnosed OSA patients and 15 non-apneic controls were enrolled in this study. Cigarette smoking status, history of chronic diseases, drugs, and habits were obtained using a standardized questionnaire before the sleep study. Sleepiness was assessed by the Epworth Sleepiness Scale. In total, 30 volunteer male subjects participated. Participants with an apnea–hypopnea index higher than 18 were assigned to the “OSA” group (n = 15), and participants with an apnea–hypopnea index lower than 5 were assigned to the “control” group (n = 15). Participants in both groups were right-handed with no co-morbidities, and no past treatment for OSA. The groups were matched for age. Participants were also selected to minimize any education effect by requiring that they had graduated from elementary school and had no education beyond high school. Exclusion criteria were the presence of any significant deviation from average in polysomnographic sleep parameters, clinically significant medical disorders (i.e., neurological or psychiatric diseases including depression, primary perception disorder), the use of drugs known to affect sleep or daytime sleepiness, and substance or alcohol abuse. Fasting blood samples were taken for complete blood count and liver, renal and, thyroid function tests as routine tests for all subjects. However, we did not test participants for alcohol and illicit drugs. Subjects were instructed to refrain from ingesting any caffeinated beverages in the 12 h prior to measurements.
Polysomnography
All participants underwent standardized sleep center clinical procedures. Standard surface electrodes were used to record electroencephalographic (four EEG derivations: C3, C4, O1, and O2), electrooculographic, electromyographic (submental and anterior tibialis muscles), and electrocardiographic data. Nasal–oral thermocouples were used to monitor airflow, and thoracic and abdominal movements were used as indications of respiratory effort. Blood oxygen saturation was monitored with pulse oximetry (with the sensor placed on the earlobe). Sleep latency, sleep efficiency, percentage of sleep time in each sleep stage, and other polysomnographic parameters were calculated. Currently published standard techniques for humans were used for recording and scoring, including procedures for sleep stages [25], [26] and leg movement [27].
Behavioral and Electrophysiological Protocols
All subjects performed three sessions of visuo-spatial n-back tests (0-back, 1-back, and 2-back). Event-related potentials were recorded simultaneously during n-back tasks. Subsequently, subjects were asked to complete mirror-drawing and TMT-A and TMT-B tests. Prior studies demonstrated that both circadian phase and time awake are important factors influencing mental performance. In order to control for potential circadian rhythm effects, experimental protocols were always conducted between 13∶30 and 17∶30.
N-back Test
We used a visually presented verbal n-back sequential letter task to probe working memory. In this task, subjects saw a string of upper or lower case letters (A, B, C, D, E, H), presented at a rate of one every 2300 ms, with each letter displayed for 200 ms. Three conditions were presented: 0-back, 1-back, and 2-back. On every trial, the subjects had to make a decision as to whether the current letter matched according to the rule, which changed between blocks. Strings of letters occurred in a pseudo-random order such that the same condition did not occur twice in a row. After a concise introduction of the n-back task, all participants were trained prior to actual tests until they reach 70% accuracy on the one-back task. All participants achieved this in their first attempt. Subjects were asked to decide whether the current letter matched a single target letter that was specified before the block began. The 0-back condition required that participants press a button each time the same letter seen (e.g., “H”) was presented in the series of letters [28]. Under the 1-back condition, they were asked to decide whether the current letter matched the previous letter. Under the 2-back condition, the task was to decide whether the currently presented letter matched the letter that had been presented two back in the sequence. Subjects responded to all items with a button press. Experimental tasks were presented by PC interface and were programmed using the STIM 2.0 software package (Compumedics Neuroscan, Inc., El Paso, TX). The PC also recorded subjects’ responses and reaction times (RTs) in s. The n-back tests lasted approximately 40 min, including short breaks. The 1-back condition consisted of 160 trials with 48 matches (30% hit rate) and never contained more than one consecutive hit in a row. The 2-back condition consisted of 250 trials with 60 matches (24% hit rate) and never contained more than two consecutive hits in a row.
P300 Recording
P300 experiments were conducted in an acoustically and electrically shielded chamber. Event-related potentials (ERPs) were recorded using a Neuroscan NuAmps (Compumedics) digital amplifier. ERPs were recorded from Fz, Pz, Cz, and O1 scalp electrodes using the Electro-Cap System (Eaton, OH) and referenced to linked earlobe electrodes. Impedances were kept below 10 kΩ. The sampling rate was 1000 Hz. The EEG was band-pass filtered between 0.5 and 70 Hz. An online band-pass filter (1–30 Hz) was also used. Data were epoched from 0 ms pre-stimulus to 1000 ms post-stimulus. Eye-blink artifacts were monitored using two electrodes just above and below the right eye. Epochs in which the amplitude exceeded ±100 µV in any channel were rejected automatically. The amplitude used in our study was calculated relative to absolute zero.
Mirror-drawing Test
The subjects participated in three successive test conditions within a single experimental session. The mirror was located at the left (front) of the sheet of paper and was placed perpendicular to the graphic workplane. During the tests, a mask prevented the subjects from having a direct view of the model or of their drawing movements. Subjects were asked to use a pencil to trace a shape while looking at it in a mirror. Five templates used in the study were straight-line shapes with horizontal and oblique lines forming 2, 4, 6, 8, and 10 corners. All templates had a total line length of 22 cm and a width between guide lines of 6.6 mm.
Subjects immediately traced the template, under instruction to move as fast and accurately as possible, attempting to stay within the line of templates. At the end of the line, they lifted the pen away from the paper, providing a clear indication of the end of their tracing action. Templates were presented in pseudorandom order, balanced across control subjects, with three repetitions of the five basic shapes (15 total trials). The time (s) to complete the task was recorded as the initial score for the mirror-drawing tests. Some subjects crossed the borders even though they completed the test. To equalize the scores of subjects who completed the test quickly but with errors and those of subjects who did the test more slowly with no errors, initial score were recalculated by dividing the completion time by the percentage of completed drawing within the total area.
Trail-making Test
The TM test had two parts. In Part A, the participant was asked to connect disordered circles enclosing the numbers 1 to 25 on the test form with direct lines to obtain a correct sequential alignment. Similarly, in Part B, the participant was asked to connect disordered circles enclosing both numbers from 1 to 13 and letters from A to L on the test form with direct lines to obtain a correct alignment such that the corresponding number followed each letter (i.e., 1-A, 2-B, 3-C, etc.). The testing equipment included four A4-size sheets of paper and a pencil. The first sheet was the practice page for Part A, and the second was the test page for Part A; similarly, the third sheet was the practice page for Part B, and the last was the test page for Part B. All tests were repeated three times, and the averages of measurements were used for statistical analyses. Score A, the time spent to complete Part A, and Score B, the time spent to complete Part B, both in s, were determined by the tester with the help of a digital hand chronometer. In addition to these two scores, we also used two derivative scores previously proposed [29] to evaluate the subjects. The derivative parameters were Score B – A (difference between time spent completing Parts B and A, in s) and Score A+B (sum of time taken to complete Parts A and B, in s).
Statistical Analysis
Statistical analyses were performed using GraphPad InStat 3.1 and Prism 5.03 (GraphPad Software, San Diego, CA, USA). The Kolmogorov–Smirnov test was used to analyze the normal distribution of the variables (P>0.05). The age and BMI of subjects and numerical test results of polysomnographic data, amplitude of P300 wave, n-back performance, and mirror-drawing and trail-making test results of the two groups were compared using the unpaired Student’s t-test. Intra-group comparisons of n-back results and TMT-A and -B results were analyzed by repeated-measures analysis of variance (ANOVA) followed by a post hoc Tukey test. P-values less than 0.05 were considered to indicate statistical significance. Correlations between numerical variables were determined using Spearman’s correlation coefficient.
Results
Clinical and Behavioral Measurements
Table 1 summarizes the polysomnographic data. All the patients and controls were men. The patients’ mean age was 41.5±2.5 (range, 26–53) years, and that of the controls was 35.8±2.5 (range, 27–50) years. The groups were not statistically significantly different in terms of age, body mass index (BMI), SpO2mean, percentage of rapid eye movement (REM) sleep, or total sleep time (TST). AHI and pulse oxygen saturation nadir in sleep (SpO2nadir) percentage in the OSA group were significantly different from those for the control group (P<0.05; Table 1).
Table 1. Subject characteristics.
| Demographic characteristics and sleep parameters | Control (n = 15) | OSA (n = 15) |
| Age | 35.9±2.5 | 41.5±2.5 |
| BMI | 28.1±1.1 | 30.7±1.1 |
| AHI | 3.0±0.5 | 36.1±6.9* |
| SpO2mean (%) | 91.5±1.5 | 91.1±0.9 |
| SpO2nadir (%) | 83.5±3.4 | 77.2±3.0* |
| REM sleep (%) | 15.8±1.2 | 12.3±1.1 |
| TST (min) | 388.1±9.8 | 374.7±6.9 |
Values are presented as means ± SEM.
AHI = apnea–hypopnea index, REM = rapid eye movement, TST = total sleep time.
*Significantly different compared with control group, P<0.05.
The n-back Test
The n-back test results are given in Table 2. There was a decline in performance accuracy and an increase in the RT as we increased the working memory load in both control and OSA groups (p<0.05). No significant difference was found between the accuracy values of the OSA and control groups at any level of the task load. Only RT of the 2-back test was significantly different between the control and OSA groups (p<0.05). There was no correlation between n-back test results and age or AHI (p>0.05). SpO2mean and SpO2nadir values were positively correlated with the number of incorrect responses during the n-back test at the 0-back level (r = 0.535, p<0.05 and r = 0.579, p<0.05, respectively).
Table 2. N-back task behavioral performance.
| Control (n = 15) | OSA (n = 15) | |
| N -back Performance (s) | ||
| 0-back, percentage correct | 92.6±2.6† | 95.4±0.8¥ |
| 1-back, percentage correct | 89.2±3.5† | 91.4±1.7¥ |
| 2-back, percentage correct | 62.5±7.0 | 63.1±6.8 |
| Reaction Time (s) | ||
| 0-back RT | 382.2±17.8 | 409.4±23.7 |
| 1-back RT | 449.7±31.5‡ | 511.2±27.0§ |
| 2-back RT | 473.2±29.3‡ | 591.4±43.8* § |
N-back performance and reaction times are presented as means ± SEM.
*p<0.05, vs. Control.
p<0.001, vs. 2-back, percentage correct (Control).
p<0.05, vs. 0-back RT (Control).
p<0.001, vs. 2-back, percentage correct (OSA).
p<0.05, vs. 0-back RT (OSA).
P300
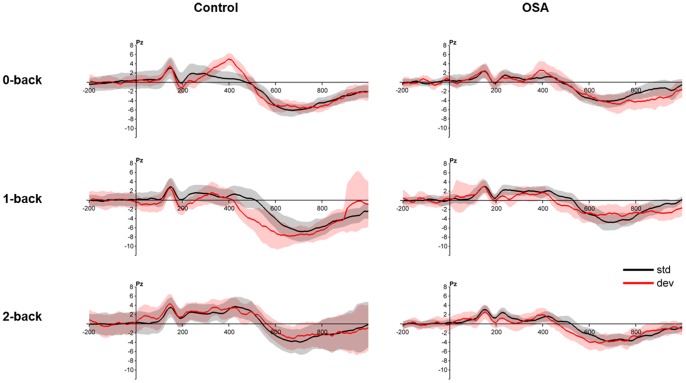
Results of the n-back P300 recordings are shown in Figure 1. P300 waves could only be recorded in the 0-back condition. The latency of the P300 wave was 400 ms. In the control group, the mean difference between the peak amplitudes of the deviant and standard responses was 4.3 µV. The standard error of this mean was 0.6 µV, and the difference was statistically significant (t = 7.5, p<0.001, df = 16). For the patient group, the mean and the standard error of the mean for this difference were 1.6 µV and 1.0 µV, respectively, which was close to being significant (t = 1.6, p = 0.14, df = 16). The mean peak amplitude of the P300 wave for the control group was 2.7 µV greater than that for the patient group (S.E. of the difference = 1.2, t = 2.2, p<0.05, df = 24.8).
Figure 1. Statistically significant P300 waves were recorded only under the 0-back condition.
Grand average for subjects in control and OSA groups. Top row: control, bottom row: OSA. Results are shown for the Pz electrode. Black: responses to standard (non-target) stimuli, red: responses to deviant (target) stimuli. Shaded regions indicate the confidence interval of the responses (mean ±2 SEM).
Mirror-drawing and Trail-making Tests
No statistically significant difference was found between the groups in the mirror-drawing test (data not shown). TMT results are provided in Table 3. When the groups were compared, only the TMT-B third trial showed a significant difference (p<0.05); no statistically significant difference was found for any TMT-A trial or the first or second trials of TMT-B. TMT performance improved generally in both groups over the trials (p<0.05).
Table 3. Trail-making test results.
| Control (n = 15) | OSA (n = 15) | |
| TMT-A1 time (s) | 23.4±1.5† | 30.2±3.2 |
| TMT-B1 time (s) | 74.7±9.7 | 72.4±7.5 |
| B1-A1 (s) | 51.3±8.6 | 42.2±6.7 |
| B1/A1 (s) | 3.2±0.3 | 2.5±0.2 |
| TMT-A2 time (s) | 22.8±2.4† | 24.3±1.9¥ |
| TMT-B2 time (s) | 60.9±8.2‡ | 59.4±4.6§ |
| B2-A2 (s) | 38.0±6.7 | 35.1±3.8 |
| B2/A2 (s) | 2.7±0.3 | 2.5±0.2 |
| TMT-A3 time (s) | 18.2±1.3 | 21.180±1.8¥ |
| TMT-B3 time (s) | 42.7±2.9‡ | 64.9±7.1* § |
| B3-A3 (s) | 33.6±8.9 | 43.8±5.6 |
| B3/A3 (s) | 2.890±0.4 | 3.078±0.1 |
TMT-A and TMT-B values are given as means ± SEM.
*p<0.05, vs. Control.
p<0.05, vs. TMT-A3 (Control).
p<0.05, vs. TMT-B1 (Control).
p<0.01, vs. TMT-A1 (OSA).
p<0.001, vs. TMT-B1 OSA.
Discussion
The aim of the current study was to examine the effects of OSA on cognitive ability. We also sought to understand any association between hypoxemia and cognitive performance in patients with OSA. There was no difference between the groups in n-back tests at any level of the task load. However, similar to the results reported by Thomas et al., we also found that the 2 -back response time in the OSA group was longer than that in the control group. However, the 2-back results were not correlated with AHI or SpO2 in our study or in others [30], [31]. Moreover, we found no correlation between age and the 2-back test results. Thomas et al. had similar results; they also reported that the 2-back test results were not correlated with age or BMI [30].
The P300 component is considered an index of general cognitive functioning or attention resources [17], [32], [33]. Previous studies using event-related potentials (ERP) have consistently shown changes in P300 suggesting attention deficits in OSA [34]. Most previous studies used 0-back tests in ERP studies. In 0-back tests, we measured the amplitude of the P300 wave as 1.6 µV in the OSA group and 4.3 µV in the control group. Our results suggest that the P300 changes observed in OSA are associated with decreased vigilance. In 1-back and 2-back tests, we could not detect a meaningful P300 wave in either group because of the increased memory load.
The mirror-drawing test results were unaffected by OSA, similar to the findings of Rouleau et al. [35]. The mirror-drawing test has been shown to be significantly affected by age, and this is interpreted as consumption of cognitive sources [36]. Our OSA parameters were unrelated to mirror-drawing test performance, perhaps because all of our subjects were relatively young. Possibly in older subjects, apnea-induced hypoxia, along with other age-related neurological problems, may cause deterioration in procedural function and working memory.
Our trail-making test results showed no difference between the groups in TMT-A. However, the OSA group was slower than the control group in trail making test B. No reported study has shown a deficiency in TMT-A in OSA patients [15]. The results for TMT-B vary. Some studies have reported no deficiency [37], whereas others have found the opposite [14], [35]. Although trail-making tests have typically been conducted once in previous studies, we repeated the tests three times and investigated the effect of OSA on learning ability. According to our results, there was no difference between the two groups at the beginning, but in subsequent tests, we found that control group Score B (time spent to complete Part B in s) was significantly shorter relative to that of the OSA group. This finding suggests that the learning process was negatively affected in the OSA group. Some declarative memory components of the trail making test differ from the mirror-drawing test. Because of this, OSA patients may have difficulty in the trail-making test, although they have no problem in the mirror-drawing test.
In summary, according to our study results, OSA does not appear to affect cognitive function as measured by the n-back test (working memory) and mirror-drawing test (procedural memory). However, in the 0-back test, the amplitude of the P300 (attention) was smaller in the OSA group than in the control group, and TMT-B (executive function) results in OSA patients were significantly slower than those in the control group. These results suggest that OSA affects attention and executive function adversely. In this study, we did not consider the duration or severity of OSA, which might affect the results. We do not think that the connection between OSA and the deterioration in cognitive function is a simple cause-and-effect relationship. Other factors in addition to OSA and age may be involved; the best candidate is genetics. For example, the APOE4 gene, a risk factor for Alzheimer disease, is also a risk factor for OSA. We did not investigate this gene in our subjects. In the light of our results and those of other studies, we think that research should be supported by genetic studies because age and OSA severity alone would not seem to sufficiently explain this connection.
Funding Statement
This study was funded by The Scientific and Technological Research Council of Turkey (TUBITAK). Grant number: 107S122. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Beebe DW (2005) Neurobehavioral effects of obstructive sleep apnea: an overview and heuristic model. Current opinion in pulmonary medicine 11 (6): 494–500. [DOI] [PubMed] [Google Scholar]
- 2. Prilipko O, Huynh N, Schwartz S, Tantrakul V, Kim JH, et al. (2011) Task positive and default mode networks during a parametric working memory task in obstructive sleep apnea patients and healthy controls. Sleep 34 (3): 293–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ryan CM, Bradley TD (2005) Pathogenesis of obstructive sleep apnea. Journal of applied physiology (Bethesda, Md : 1985) 99 (6): 2440–2450 10.1152/japplphysiol.00772.2005 [DOI] [PubMed] [Google Scholar]
- 4. Adams N, Strauss M, Schluchter M, Redline S (2001) Relation of measures of sleep-disordered breathing to neuropsychological functioning. American journal of respiratory and critical care medicine 163 (7): 1626–1631 10.1164/ajrccm.163.7.2004014 [DOI] [PubMed] [Google Scholar]
- 5. Salorio CF, White DA, Piccirillo J, Duntley SP, Uhles ML (2002) Learning, memory, and executive control in individuals with obstructive sleep apnea syndrome. Journal of clinical and experimental neuropsychology 24 (1): 93–100 10.1076/jcen.24.1.93.973 [DOI] [PubMed] [Google Scholar]
- 6. Mazza S, Pepin JL, Naegele B, Plante J, Deschaux C, et al. (2005) Most obstructive sleep apnoea patients exhibit vigilance and attention deficits on an extended battery of tests. The European respiratory journal : official journal of the European Society for Clinical Respiratory Physiology 25 (1): 75–80 10.1183/09031936.04.00011204 [DOI] [PubMed] [Google Scholar]
- 7. Beebe DW, Gozal D (2002) Obstructive sleep apnea and the prefrontal cortex: towards a comprehensive model linking nocturnal upper airway obstruction to daytime cognitive and behavioral deficits. Journal of sleep research 11 (1): 1–16. [DOI] [PubMed] [Google Scholar]
- 8. Bedard MA, Montplaisir J, Richer F, Rouleau I, Malo J (1991) Obstructive sleep apnea syndrome: pathogenesis of neuropsychological deficits. Journal of clinical and experimental neuropsychology 13 (6): 950–964 10.1080/01688639108405110 [DOI] [PubMed] [Google Scholar]
- 9. Feuerstein C, Naegele B, Pepin JL, Levy P (1997) Frontal lobe-related cognitive functions in patients with sleep apnea syndrome before and after treatment. Acta neurologica Belgica 97 (2): 96–107. [PubMed] [Google Scholar]
- 10. Naegele B, Thouvard V, Pepin JL, Levy P, Bonnet C, et al. (1995) Deficits of cognitive executive functions in patients with sleep apnea syndrome. Sleep 18 (1): 43–52. [PubMed] [Google Scholar]
- 11. Aloia MS, Arnedt JT, Davis JD, Riggs RL, Byrd D (2004) Neuropsychological sequelae of obstructive sleep apnea-hypopnea syndrome: a critical review. Journal of the International Neuropsychological Society : JINS 10 (5): 772–785 10.1017/s1355617704105134 [DOI] [PubMed] [Google Scholar]
- 12. Lis S, Krieger S, Hennig D, Röder C, Kirsch P, et al. (2008) Executive functions and cognitive subprocesses in patients with obstructive sleep apnoea. Journal of sleep research 17 (3): 271–280. [DOI] [PubMed] [Google Scholar]
- 13. Redline S, Strauss ME, Adams N, Winters M, Roebuck T, et al. (1997) Neuropsychological function in mild sleep-disordered breathing. Sleep 20 (2): 160–167. [DOI] [PubMed] [Google Scholar]
- 14. Verstraeten E, Cluydts R, Pevernagie D, Hoffmann G (2004) Executive function in sleep apnea: controlling for attentional capacity in assessing executive attention. Sleep 27 (4): 685–693. [PubMed] [Google Scholar]
- 15. Saunamaki T, Jehkonen M (2007) A review of executive functions in obstructive sleep apnea syndrome. Acta neurologica Scandinavica 115 (1): 1–11 10.1111/j.1600-0404.2006.00744.x [DOI] [PubMed] [Google Scholar]
- 16. Decary A, Rouleau I, Montplaisir J (2000) Cognitive deficits associated with sleep apnea syndrome: a proposed neuropsychological test battery. Sleep 23 (3): 369–381. [PubMed] [Google Scholar]
- 17. Picton TW (1992) The P300 wave of the human event-related potential. Journal of clinical neurophysiology : official publication of the American Electroencephalographic Society 9 (4): 456–479. [DOI] [PubMed] [Google Scholar]
- 18. Gosselin N, Mathieu A, Mazza S, Petit D, Malo J, et al. (2006) Attentional deficits in patients with obstructive sleep apnea syndrome: an event-related potential study. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology 117 (10): 2228–2235 10.1016/j.clinph.2006.07.130 [DOI] [PubMed] [Google Scholar]
- 19. Sangal RB, Sangal JM (1997) Abnormal visual P300 latency in obstructive sleep apnea does not change acutely upon treatment with CPAP. Sleep 20 (9): 702–704. [DOI] [PubMed] [Google Scholar]
- 20. Walsleben JA, Squires NK, Rothenberger VL (1989) Auditory event-related potentials and brain dysfunction in sleep apnea. Electroencephalography and clinical neurophysiology 74 (4): 297–311. [DOI] [PubMed] [Google Scholar]
- 21. Rumbach L, Krieger J, Kurtz D (1991) Auditory event-related potentials in obstructive sleep apnea: effects of treatment with nasal continuous positive airway pressure. Electroencephalography and clinical neurophysiology 80 (5): 454–457. [DOI] [PubMed] [Google Scholar]
- 22. Inoue Y, Nanba K, Kojima K, Mitani H, Arai AH (2001) P300 abnormalities in patients with severe sleep apnea syndrome. Psychiatry and clinical neurosciences 55 (3): 247–248 10.1046/j.1440-1819.2001.00844.x [DOI] [PubMed] [Google Scholar]
- 23. Cangoz B, Karakoc E, Selekler K (2009) Trail Making Test: normative data for Turkish elderly population by age, sex and education. Journal of the neurological sciences 283 (1–2): 73–78 10.1016/j.jns.2009.02.313 [DOI] [PubMed] [Google Scholar]
- 24. Vicari S, Finzi A, Menghini D, Marotta L, Baldi S, et al. (2005) Do children with developmental dyslexia have an implicit learning deficit? Journal of neurology, neurosurgery, and psychiatry 76 (10): 1392–1397 10.1136/jnnp.2004.061093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rechtschaffen A, Kales A (1968) A manual of standardized techniques and scoring system for sleep stages in human subjects. U.S. Government Printing Office, Washington D.C.
- 26.Bornstein SK (1982) Respiratory monitoring during sleep: Polysomnography. In: Guilleminault C, editor. Sleeping and Waking Disorders: Indications and Techniques. Addison-Wesley, Menlo Park, CA pp: 183–212.
- 27. Bonnet M, Carley D, Carskadon G, Easton P, Guilleminault C, et al. (1993) Recording and scoring leg movements. The Atlas Task Force. Sleep 16 (8): 748–759. [PubMed] [Google Scholar]
- 28. Archbold KH, Borghesani PR, Mahurin RK, Kapur VK, Landis CA (2009) Neural activation patterns during working memory tasks and OSA disease severity: preliminary findings. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 5 (1): 21–27. [PMC free article] [PubMed] [Google Scholar]
- 29. Arbuthnott K, Frank J (2000) Trail making test, part B as a measure of executive control: validation using a set-switching paradigm. Journal of clinical and experimental neuropsychology 22 (4): 518–528 10.1076/1380-3395(200008)22:41-0ft518 [DOI] [PubMed] [Google Scholar]
- 30. Thomas RJ, Rosen BR, Stern CE, Weiss JW, Kwong KK (2005) Functional imaging of working memory in obstructive sleep-disordered breathing. Journal of applied physiology (Bethesda, Md : 1985) 98 (6): 2226–2234 10.1152/japplphysiol.01225.2004 [DOI] [PubMed] [Google Scholar]
- 31. Felver-Gant JC, Bruce AS, Zimmerman M, Sweet LH, Millman RP, et al. (2007) Working memory in obstructive sleep apnea: construct validity and treatment effects. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 3 (6): 589–594. [PMC free article] [PubMed] [Google Scholar]
- 32. Kramer AF, Strayer DL (1988) Assessing the development of automatic processing: an application of dual-task and event-related brain potential methodologies. Biological psychology 26 (1–3): 231–267. [DOI] [PubMed] [Google Scholar]
- 33. Wickens C, Kramer A, Vanasse L, Donchin E (1983) Performance of concurrent tasks: a psychophysiological analysis of the reciprocity of information-processing resources. Science (New York, NY) 221 (4615): 1080–1082. [DOI] [PubMed] [Google Scholar]
- 34. Raggi A, Ferri R (2012) Cognitive evoked potentials in obstructive sleep apnea syndrome: a review of the literature. Reviews in the neurosciences 23 (3): 311–323 10.1515/revneuro-2012-0027 [DOI] [PubMed] [Google Scholar]
- 35. Rouleau I, Decary A, Chicoine AJ, Montplaisir J (2002) Procedural skill learning in obstructive sleep apnea syndrome. Sleep 25 (4): 401–411. [PubMed] [Google Scholar]
- 36. Kennedy KM, Raz N (2005) Age, sex and regional brain volumes predict perceptual-motor skill acquisition. Cortex; a journal devoted to the study of the nervous system and behavior 41 (4): 560–569. [DOI] [PubMed] [Google Scholar]
- 37.Oken BS (1997) Endogenous Event-Related Potentials. In: Chiappa KH, editor. Evoked Potentials in Clinical Medicine, 3rd edn. Lippincott Williams & Wilkins, Philadelphia-New York, 529–563. [Google Scholar]