Abstract
Aims
The Systematic COronary Risk Evaluation (SCORE) scale assesses 10 year risk of fatal atherosclerotic cardiovascular disease (CVD), based on conventional risk factors. The high-risk SCORE version is recommended for Central and Eastern Europe and former Soviet Union (CEE/FSU), but its performance has never been systematically assessed in the region. We evaluated SCORE performance in two sets of population-based CEE/FSU cohorts.
Methods and results
The cohorts based on the World Health Organization MONitoring of trends and determinants in CArdiovascular disease (MONICA) surveys in the Czech Republic, Poland (Warsaw and Tarnobrzeg), Lithuania (Kaunas), and Russia (Novosibirsk) were followed from the mid-1980s. The Health, Alcohol, and Psychosocial factors in Eastern Europe (HAPIEE) study follows Czech, Polish (Krakow), and Russian (Novosibirsk) cohorts from 2002–05. In Cox regression analyses, the high-risk SCORE ≥5% at baseline significantly predicted CVD mortality in both MONICA [n = 15 027; hazard ratios (HR), 1.7–6.3] and HAPIEE (n = 20 517; HR, 2.6–10.5) samples. While SCORE calibration was good in most MONICA samples (predicted and observed mortality were close), the risk was underestimated in Russia. In HAPIEE, the high-risk SCORE overpredicted the estimated 10 year mortality for Czech and Polish samples and adequately predicted it for Russia. SCORE discrimination was satisfactory in both MONICA and HAPIEE.
Conclusion
The high-risk SCORE underestimated the fatal CVD risk in Russian MONICA but performed well in most MONICA samples and Russian HAPIEE. This SCORE version might overestimate the risk in contemporary Czech and Polish populations.
Keywords: Cardiovascular mortality, Cardiovascular risk factors, SCORE risk function, Risk prediction, Central and Eastern Europe, Former Soviet Union
See page 537 for the editorial comment on this article (doi:10.1093/eurheartj/eht286)
Introduction
Cardiovascular disease (CVD) is the world's leading cause of mortality, morbidity, and disability.1,2 Numerous algorithms use combinations of conventional risk factors to identify individuals at higher risk of CVD, who are most likely to benefit from preventive measures.2,3 The existing risk scores were mostly derived from Western European and North American cohorts, and their prognostic accuracy might differ in other populations.4,5 The most widely used instruments are the Framingham risk model6 and the Systematic COronary Risk Evaluation (SCORE) scale.7 The latter, based on prospective data from 12 European cohorts, estimates 10 year risk of fatal CVD and uses age, sex, blood lipids, blood pressure, and smoking as risk predictors. One component of the SCORE model defines the shape of the baseline survival function, separately for men and women, while the other calculates relative risks for each risk factor. The effects of risk factors are considered to be similar in both genders, across countries, and over time.7 Two SCORE versions were created for high- and low-risk European countries.
While CVD mortality has recently declined in most Central and Eastern European (CEE) countries, it is still high in almost all of the former Soviet Union (FSU).8 The latest guidelines by the European Society of Cardiology (ESC) acknowledge the heterogeneity of the background CVD risk in this region but still provide only one version of the high-risk SCORE, recommended for use in all CEE/FSU populations.5 It is unclear how well SCORE performs in CEE/FSU, as it was derived without reference to the local data5 and has never been properly recalibrated for this area.
Our study aimed to assess the prognostic performance of the high-risk SCORE in CEE/FSU, using two sets of population-based cohorts from four countries in the region.
Methods
Study population and samples
We used the data from two international studies: the World Health Organization (WHO) MONitoring of trends and determinants in CVD (MONICA) Project9,10 and the Health, Alcohol, and Psychosocial factors in Eastern Europe (HAPIEE) study.11
The WHO MONICA Project monitored the trends in CVD rates and risk factors in 38 populations from the mid-1980s to at least the mid-1990s.9,10 Risk factors were assessed in random population samples of men and women aged 35–64; some of these samples were followed for mortality. We obtained the baseline data and the data on the subsequent 10 year mortality from the following MONICA samples: the Czech sample from six country districts, examined in 1992; Polish Warsaw and Tarnobrzeg samples screened in 1983–84 and 1987–89; Lithuanian Kaunas samples examined in 1983–85, 1986–87, and 1992–93; and Russian Novosibirsk samples screened in 1985–86, 1988–89, and 1994–95. Numbers of subjects and response rates are presented in Table 1. At baseline, participants completed a questionnaire survey, underwent a clinical examination, and provided a blood sample. The mortality follow-up used the data from national and local mortality registers.9
Table 1.
Sample selection and follow-up length
| MONICA |
HAPIEE |
|||||||
|---|---|---|---|---|---|---|---|---|
| CZ | PL-W | PL-T | LT | RU | CZ | PL-K | RU | |
| Baseline, year (response rate, %) | 1992 (65) | 1983–84 (74), 1988–89 (70) | 1983–84 (82), 1987–88 (73) | 1983–85 (70), 1986–87 (70), 1992–93 (59) | 1985–86 (72), 1988–89 (73), 1994–95 (72) | 2002–05 (55) | 2002–05 (61) | 2002–05 (61) |
| Recruited, n | 3273 | 4079 | 4033 | 5968 | 9835 | 8856 | 10 728 | 9363 |
| Within the study age range, n | 1977 | 3396 | 3274 | 4596 | 6062 | 8781 | 10 728 | 9352 |
| No pre-existing CVD, n | 1861 | 2437 | 2782 | 3806 | 5669 | 7633 | 8316 | 7316 |
| No missing SCORE values, n | 1340 | 2404 | 2729 | 3301 | 5253 | 6018 | 7209 | 7290 |
| Median follow-up (interquartile range), years | 10.0 (10.0–10.0) | 10.0 (10.0–10.0) | 10.0 (10.0–10.0) | 10.0 (10.0–10.0) | 10.0 (10.0–10.0) | 6.2 (5.8–6.9) | 5.1 (4.9–5.8) | 4.6 (3.9–5.1) |
CZ, Czech Republic; LT, Lithuania; PL-K, Poland (Krakow); PL-T, Poland (Tarnobrzeg); PL-W, Poland (Warsaw); RU, Russia.
HAPIEE is a multi-centre study of CVD and other chronic conditions in CEE/FSU.11 It follows random population samples of men and women, aged 45–69 at baseline (2002–05), from the Czech Republic (Havířov/Karviná, Hradec Králové, Jihlava, Kroměříž, Liberec, and Ústí nad Labem), Poland (Krakow), Russia (Novosibirsk), and Lithuania (Kaunas). The four cohorts have been followed for cause-specific mortality and non-fatal CVD. As the Lithuanian cohort entered the study later and had fewer CVD deaths, we analysed only Czech, Polish, and Russian data. The baseline data collection included a questionnaire survey and a physical examination, with a fasting venous blood sample collection. Mortality data for the median follow-up period of 4.6–6.2 years (Table 1) come from national (the Czech Republic) and local (Poland and Russia) registers.11
As SCORE predicts the risk of cardiovascular mortality in individuals over 40 and without pre-existing atherosclerotic CVD,5,7 we excluded subjects with a self-reported history or medical evidence of myocardial infarction, angina, or stroke and those aged <40 years at baseline. We also excluded individuals with missing values of the risk factors, which are incorporated in SCORE. In Czech and Polish HAPIEE samples, the study questionnaire was completed at home, prior to medical examination in a clinic. This explains the smaller proportion of Czech and Polish participants with non-missing values of SCORE components. The sizes of our analytical samples (15 027 MONICA and 20 517 HAPIEE participants) are presented in Table 1.
The MONICA study protocol was approved by the local ethics committees in each participating country.9 The HAPIEE study protocol was approved by the UCL/UCLH ethics committee and by the local ethics committees at each study centre.11 All participants provided informed consent.
Measurements
The SCORE risk predictors include age, sex, smoking status, total cholesterol (TC), and systolic blood pressure (SBP). In MONICA and HAPIEE, the data on self-reported smoking status came from the baseline standard questionnaire.9–11 In line with the SCORE criteria,7 participants currently and regularly smoking at least one cigarette per day were regarded as current smokers; never and ex-smokers were considered non-smokers. SBP measurement was performed after a 5 min rest, in a quiet room with comfortable temperature, in a sitting position, on the right arm, with a 2 min interval between measurements, using a standard mercury sphygmomanometer (MONICA) or a digital blood pressure monitor Omron M5-I (HAPIEE).9,11 TC concentration in fasting venous blood was measured with a direct Liebermann-Burchard method in Polish and Russian MONICA and with an enzymatic method in all other samples.9,11 All assay methods were calibrated, and all laboratories were subjected to extensive quality control. In agreement with SCORE end-points,7 the study outcome was coronary or non-coronary atherosclerotic cardiovascular death.
Statistical analyses
The high-risk version of SCORE, recommended by the ESC for CEE/FSU populations,5 was used to predict the risk of fatal atherosclerotic CVD in all MONICA and HAPIEE samples, as the recently introduced Czech and Polish SCORE versions lack a detailed description of their development and recalibration.12,13 For comparison, the performance of the low-risk SCORE was also investigated.
The prognostic performance of risk prediction scales, such as SCORE, could be assessed via calibration and discrimination.14,15 Calibration reflects how close predicted and observed risks are, with a predicted-to-observed (P/O) risk ratio of 1.0 indicating perfect calibration. In our samples, particularly in female ones, a substantial proportion of individuals had the same, relatively low risk levels; therefore, we focused on P/O ratios as the preferred calibration measure. Discrimination is the model's ability to separate participants who will experience events (such as fatal CVD) during the follow-up from those who will remain event-free. The typically used threshold measures of discrimination include sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for a particular risk cut-off (5% for SCORE). Summary measures of discrimination include the area under the receiver operating characteristic curve (AUROC) and its equivalent for survival models, Harrell's C-statistic.16 AUROC plots the model's sensitivity against ‘1—specificity’ across all consecutive cut-offs. AUROC/C-statistic values of 0.5 and 1.0 indicate minimal and ideal discrimination, respectively.
Our analyses of SCORE prognostic ability were performed separately for men and women in each MONICA and HAPIEE sample and included the following steps. First, we investigated the role of SCORE as a fatal CVD predictor, using Cox regression models. Second, we assessed SCORE calibration, calculating P/O risk ratios for MONICA. For HAPIEE, we estimated 10 year levels of atherosclerotic CVD mortality and compared SCORE levels to these estimates, in order to approximate the 10 year SCORE calibration. Finally, we assessed SCORE discrimination by calculating its sensitivity, specificity, PPV, NPV, and Harrell's C.
The use of Cox proportional hazards regression models was justified by the high P-values in Schoenfeld's test across all the samples. The data from all MONICA waves were pooled within samples, because the SCORE-fatal CVD association showed no evidence of confounding by or statistical interaction with the study wave. The estimation of 10 year CVD mortality for HAPIEE was based on the mortality patterns in MONICA samples from respective countries. We assumed that the ratio between the death numbers registered at a pre-specified cut-off point (the follow-up time in complete years: six, five, and four years for Czech, Polish, and Russian HAPIEE, respectively) and the death numbers observed during the 10 year follow-up would be similar for MONICA and HAPIEE subjects from the same country. These ratios were separately calculated for Czech, Polish (Warsaw), and Russian MONICA men and women and projected onto the currently observed numbers of cardiovascular deaths in HAPIEE samples, in order to provide estimates of the 10 year CVD mortality. These estimates were then used for the analyses of the expected 10 year SCORE calibration in HAPIEE. Two-sided P-values <0.05 were used to indicate statistical significance. All statistical analyses were performed using Stata/IC 11.0 (StataCorp LP, Texas, USA).
Results
Baseline sample characteristics are presented in Table 2. The mean age of MONICA participants was close to 52 years, compared with 57 years in HAPIEE. In both studies, the sizes of the five-year age groups were relatively similar. Smoking prevalence was high in both studies, with the exception of MONICA women from Tarnobrzeg, Kaunas, and Novosibirsk. Czech and Polish HAPIEE men smoked less than their MONICA peers. In contrast, among Russian women, smoking prevalence was higher in HAPIEE than in MONICA. In both studies, mean TC levels were close to 6 mmol/L and tended to be slightly higher in women. The highest mean SBP levels, exceeding 140 mm Hg, were observed for MONICA participants from Warsaw and Czech HAPIEE men.
Table 2.
Sample characteristics
| Categories | MONICA men |
HAPIEE men |
||||||
|---|---|---|---|---|---|---|---|---|
| CZ | PL-W | PL-T | LT | RU | CZ | PL-K | RU | |
| N | 636 | 1253 | 1267 | 1651 | 2576 | 2659 | 3456 | 3246 |
| Mean age (SD), years | 50.8 (7.1) | 51.9 (7.0) | 52.5 (6.8) | 51.3 (7.1) | 52.3 (6.8) | 58.0 (7.1) | 57.2 (7.0) | 57.5 (7.0) |
| Age groups, % | ||||||||
| 40–44 | 27.0 | 21.6 | 17.4 | 23.8 | 17.7 | — | — | — |
| 45–49 | 22.5 | 20.8 | 20.8 | 19.3 | 22.6 | 17.3 | 20.4 | 18.9 |
| 50–54 | 21.1 | 20.0 | 21.6 | 18.1 | 20.8 | 19.6 | 21.7 | 21.3 |
| 55–59 | 15.9 | 22.5 | 23.2 | 22.9 | 23.1 | 20.7 | 21.4 | 21.6 |
| 60–64 | 13.5 | 15.1 | 17.0 | 15.9 | 15.8 | 21.6 | 18.3 | 18.2 |
| 65+ | — | — | — | — | — | 20.8 | 18.2 | 20.0 |
| Current smoking, % | 40.3 | 52.5 | 56.3 | 35.1 | 53.1 | 26.6 | 32.9 | 51.0 |
| Mean TC (SD), mmol/L | 6.2 (1.3) | 5.6 (1.0) | 5.5 (1.0) | 6.0 (1.2) | 5.5 (1.2) | 5.7 (1.0) | 5.8 (1.1) | 6.0 (1.2) |
| Mean SBP (SD), mm Hg | 139.0 (20.7) | 142.2 (23.8) | 136.6 (21.2) | 137.3 (20.0) | 136.3 (20.2) | 143.8 (18.4) | 141.6 (20.2) | 141.6 (22.7) |
|
MONICA women |
HAPIEE women |
|||||||
| CZ | PL-W | PL-T | LT | RU | CZ | PL-K | RU | |
| N | 704 | 1151 | 1462 | 1650 | 2677 | 3359 | 3753 | 4044 |
| Mean age (SD), years | 51.2 (7.2) | 51.8 (7.0) | 52.4 (6.9) | 50.9 (7.1) | 52.2 (7.0) | 57.4 (7.1) | 56.6 (6.9) | 57.3 (7.1) |
| Age groups, % | ||||||||
| 40–44 | 24.0 | 21.8 | 18.3 | 24.6 | 19.4 | — | — | — |
| 45–49 | 24.9 | 21.6 | 21.6 | 21.0 | 22.0 | 19.6 | 22.8 | 20.6 |
| 50–54 | 17.6 | 20.4 | 21.4 | 19.6 | 20.8 | 21.2 | 23.4 | 20.8 |
| 55–59 | 18.2 | 20.9 | 21.1 | 19.3 | 20.5 | 18.2 | 20.6 | 21.8 |
| 60–64 | 15.3 | 15.3 | 17.6 | 15.5 | 17.3 | 23.7 | 17.7 | 17.2 |
| 65+ | — | — | — | — | — | 17.3 | 15.5 | 19.6 |
| Current smoking, % | 20.6 | 31.2 | 7.5 | 4.2 | 3.4 | 21.0 | 25.1 | 10.1 |
| Mean TC (SD), mmol/L | 6.3 (1.3) | 5.7 (1.0) | 5.7 (1.1) | 6.3 (1.2) | 5.9 (1.3) | 5.9 (1.0) | 5.9 (1.1) | 6.5 (1.3) |
| Mean SBP (SD), mm Hg | 137.7 (21.7) | 142.6 (25.1) | 141.6 (24.3) | 137.3 (22.7) | 138.5 (22.6) | 134.2 (19.4) | 133.2 (20.8) | 141.6 (25.7) |
CZ, Czech Republic; LT, Lithuania; PL-K, Poland (Krakow); PL-T, Poland (Tarnobrzeg); PL-W, Poland (Warsaw); RU, Russia. SBP, systolic blood pressure; SD, standard deviation; TC, total cholesterol.
SCORE as a CVD mortality predictor
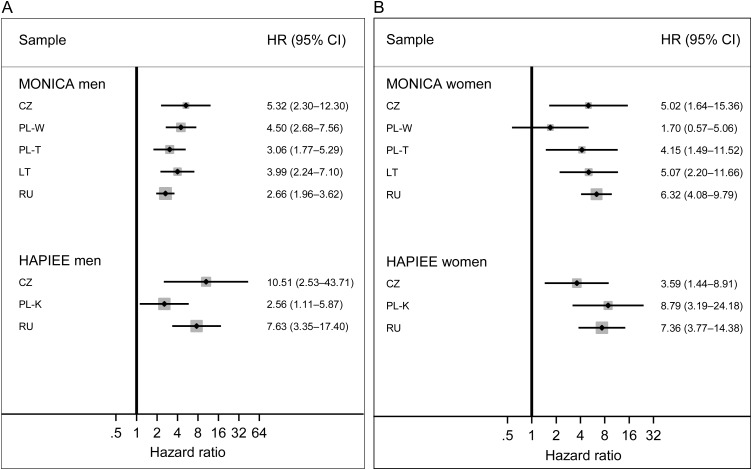
In most MONICA samples, the high-risk SCORE ≥5% at baseline was significantly associated with the 10 year risk of atherosclerotic CVD mortality (Figure 1). The hazard ratios (HR) varied from 1.7 in Warsaw women to 6.3 in women from Novosibirsk. In HAPIEE, the baseline SCORE was a significant predictor of fatal CVD over the subsequent 4.5–6 years (HR, 2.6–10.5).
Figure 1.
The high-risk SCORE (≥5 vs. <5%) and atherosclerotic cardiovascular mortality in MONICA and HAPIEE men (A) and women (B) hazard ratios (HR) and 95% confidence intervals (CI). CZ, Czech Republic; LT, Lithuania; PL-K, Poland (Krakow); PL-T, Poland (Tarnobrzeg); PL-W, Poland (Warsaw); RU, Russia.
SCORE calibration
In all male MONICA samples, mean SCORE-predicted risk levels were relatively high (≥5%); for women, predicted risk was considerably lower and approached 2% (Table 3). Among MONICA men, the percentage of atherosclerotic CVD deaths registered over 10 years was highest in Novosibirsk and lowest in Kaunas. In women, the observed risk of fatal CVD was half of that in men from the respective samples. While most ratios of predicted and observed (P/O) CVD mortality were close to 1.0, the risk was markedly underestimated for Russian men and women.
Table 3.
Prognostic performance of the high-risk SCORE (≥5 vs. <5%)
| MONICA men |
HAPIEE men |
|||||||
|---|---|---|---|---|---|---|---|---|
| CZ | PL-W | PL-T | LT | RU | CZ | PL-K | RU | |
| Predicted (P) deaths, N (%) | 33.5 (5.26) | 72.4 (5.78) | 69.0 (5.43) | 83.1 (5.03) | 138.1 (5.36) | 199.7 (7.51) | 254.7 (7.37) | 294.4 (9.07) |
| Observed (O) deaths, N (%) | 32 (5.03) | 86 (6.68) | 62 (4.89) | 58 (3.51) | 181 (7.03) | 37 (1.39) | 34 (0.98) | 105 (3.23) |
| P/O ratio | 1.05 | 0.87 | 1.11 | 1.43 | 0.76 | 5.40 | 7.52 | 2.81 |
| Estimated (E) deaths, N (%)* | — | — | — | — | — | 74.0 (2.78) | 94.2 (2.73) | 279.3 (8.60) |
| P/E ratio | — | — | — | — | — | 2.70 | 2.70 | 1.06 |
| Sensitivity | 0.78 | 0.79 | 0.71 | 0.72 | 0.65 | 0.95 | 0.79 | 0.94 |
| Specificity | 0.59 | 0.54 | 0.56 | 0.60 | 0.58 | 0.37 | 0.39 | 0.33 |
| PPV | 0.09 | 0.11 | 0.08 | 0.06 | 0.11 | 0.02 | 0.01 | 0.05 |
| NPV | 0.98 | 0.97 | 0.97 | 0.98 | 0.96 | 0.99 | 0.99 | 0.99 |
| Harrell's C | 0.69 | 0.67 | 0.63 | 0.67 | 0.62 | 0.66 | 0.60 | 0.63 |
|
MONICA women |
HAPIEE women |
|||||||
| CZ | PL-W | PL-T | LT | RU | CZ | PL-K | RU | |
| Predicted (P) deaths, N (%) | 12.5 (1.78) | 22.6 (1.96) | 24.6 (1.68) | 26.4 (1.60) | 44.7 (1.67) | 85.0 (2.53) | 92.0 (2.45) | 124.6 (3.08) |
| Observed (O) deaths, N (%) | 13 (1.85) | 21 (1.82) | 19 (1.30) | 26 (1.58) | 86 (3.21) | 19 (0.57) | 16 (0.43) | 42 (1.04) |
| P/O ratio | 0.96 | 1.08 | 1.29 | 1.01 | 0.52 | 4.44 | 5.70 | 2.96 |
| Estimated (E) deaths, N (%)* | — | — | — | — | — | 41.2 (1.23) | 37.3 (0.99) | 139.0 (3.44) |
| P/E ratio | — | — | — | — | — | 2.06 | 2.48 | 0.90 |
| Sensitivity | 0.39 | 0.19 | 0.26 | 0.31 | 0.37 | 0.42 | 0.63 | 0.71 |
| Specificity | 0.89 | 0.88 | 0.92 | 0.92 | 0.92 | 0.83 | 0.84 | 0.76 |
| PPV | 0.06 | 0.03 | 0.04 | 0.06 | 0.13 | 0.01 | 0.02 | 0.03 |
| NPV | 0.99 | 0.98 | 0.99 | 0.99 | 0.98 | 0.99 | 0.99 | 0.99 |
| Harrell's C | 0.64 | 0.54 | 0.59 | 0.61 | 0.64 | 0.63 | 0.74 | 0.74 |
CZ, Czech Republic; LT, Lithuania; PL-K, Poland (Krakow); PL-T, Poland (Tarnobrzeg); PL-W, Poland (Warsaw); RU, Russia. CI, confidence interval; HR, hazard ratio; NNP, negative predictive value; PPV, positive predictive value.
*MONICA-based estimations of 10 year CVD mortality in HAPPIEE.
In each male HAPIEE sample, mean predicted levels of 10 year fatal CVD exceeded 5%; in women, the predicted risk was three times lower. The percentage of CVD deaths registered in Russian men was two to three times higher than among their Czech and Polish peers; the observed cardiovascular mortality levels in women were lower but reflected the same ranking. For the currently available data on fatal CVD, all P/O ratios exceeded 1.0, while the magnitude of risk overprediction was smaller for Russian vs. Czech and Polish HAPIEE.
As SCORE predicts the 10 year risk of atherosclerotic cardiovascular mortality, we estimated the expected 10 year levels of fatal CVD, in order to assess SCORE calibration in HAPIEE. The estimated percentage of deaths for Czech and Polish HAPIEE was noticeably lower than the 10 year mortality levels for the respective MONICA samples. In contrast, the estimated percentage for Russian HAPIEE was slightly higher than the fatal CVD levels in Russian MONICA (Table 3). This difference possibly reflects the heterogeneous CVD trends across CEE/FSU in the last two decades.8 In agreement with the current discrepancies between Russian vs. Czech and Polish national mortality rates,8 our fatal CVD estimates were at least three times higher in Russian HAPIEE participants than in their Czech and Polish peers. Based on the ratios of predicted-to-estimated (P/E) mortality (Table 3), the high-risk SCORE demonstrated at least a two-fold overprediction of the estimated mortality for Czech and Polish HAPIEE, while the agreement between the predicted and estimated risk was good for Russian HAPIEE. The low-risk SCORE version also overpredicted 10 year estimated mortality in Czech and Polish HAPIEE (respective P/E ratios 1.2–1.4; see Supplementary material online, Table), but to a lesser extent than the high-risk SCORE. Among Russian participants, the low-risk SCORE predicted only one-half of the estimated mortality (P/E ratios 0.5–0.6; see Supplementary material online, Table).
SCORE discrimination
Sensitivity of the high-risk SCORE was relatively high in all male MONICA and HAPIEE samples, whereas its specificity was somewhat lower; the opposite was true for MONICA and HAPIEE women (Table 3). Due to the low outcome frequency, PPV values were also low across all the samples; in contrast, NPV values exceeded 0.9. All Harrell's C-values were over 0.50 and were highest for Czech men and Russian women in MONICA and for Czech men and Polish women in HAPIEE. A direct comparison of SCORE discrimination in MONICA vs. HAPIEE was not possible, due to the current difference in the follow-up length. However, SCORE sensitivity appeared higher and specificity lower for most HAPIEE samples, compared with respective MONICA samples.
Discussion
To the best of our knowledge, this is the first attempt to assess the SCORE prognostic performance in CEE/FSU. As expected, the high-risk SCORE was a significant risk predictor in both MONICA and HAPIEE samples, which are the best available approximations of the national levels of cardiovascular risk factors and fatal CVD for the 1980s to 2000s. SCORE calibration was good in MONICA, with the exception of Russia where fatal CVD was substantially underpredicted. This primarily reflects the very high baseline risk: Russia is now regarded by the ESC as a ‘very-high-risk country’, although no relevant SCORE version has yet been provided.5 It is also possible that the very high mortality risk in Russian MONICA was partly influenced by the recent mortality fluctuations.8 In HAPIEE, the comparison between the estimated 10 year CVD mortality and the SCORE predictions demonstrated that better calibration was achieved by the high-risk SCORE for Russian samples and the low-risk SCORE for Czech and Polish samples. The high-risk SCORE discrimination was satisfactory in MONICA and HAPIEE.
Strengths and limitations
Several methodological issues need to be considered when interpreting our findings. First, we used the data from two separate studies, which covered different historical periods. As CVD trends in CEE/FSU have diverged after 1990, and Russian cardiovascular mortality levels have shown large temporal fluctuations, the cohort study estimates of a longer-term mortality risk may be an imperfect approximation of national rates. Second, while the participating cohorts are not nationally representative, they are the best available sources of data, and their ranking by fatal CVD levels reflects between-country differences in cardiovascular mortality. Third, due to a shorter follow-up, the 10 year risk of CVD death in HAPIEE was estimated. We compared two estimation approaches—one based on the MONICA patterns of cardiovascular mortality and the other based on the exponential survival model17 (not shown)—which produced similar results. Fourth, the comparability of MONICA and HAPIEE data was high, as the protocols of baseline survey, physical examination, and mortality follow-up were similar. Fifth, as in most studies, MONICA and HAPIEE participants were likely to be healthier than non-responders. This potential discrepancy could be enhanced by the complete case analyses and dilute the association of interest. The available multiple imputation methods employ the assumption of data missing (completely) at random,18,19 which was not the case for our samples. Moreover, the Cox regression results across the samples with the highest SCORE missingness were similar for complete and multiply-imputed data (not presented). Sixth, some context-specific misclassification of outcomes within the broad category of atherosclerotic CVD deaths might occur, but it was unlikely to affect the associations of interest. Finally, SCORE, like most other risk scales, provides risk point estimates without confidence intervals and does not account for SBP and TC regression to the mean or for CVD treatment effects. However, this single-estimate approach is user-friendly and clinically applicable.
Consistency with other studies
The validity of our results, despite the above-mentioned potential limitations, is supported by the fact that the levels of major risk factors and CVD mortality in MONICA and HAPIEE samples were consistent with the respective national cross-sectional estimates and trends, presented in the WHO Global InfoBase20 and WHO systematic reviews.21,22 The association between baseline SCORE and fatal CVD was statistically significant in both MONICA and HAPIEE. To the best of our knowledge, only two other studies have reported the magnitude of the SCORE–CVD association. For middle-aged Austrians, the strength of a significant link between continuous SCORE and 10 year CVD mortality was reported only after adjustment for several covariates.23 Among adults participating in the Greek ATTICA study, HellenicSCORE levels were significantly associated with the five-year risk of incident CVD.24 While the direct comparison of these results is problematic, the reported HR values23,24 are close to the estimates for high-risk continuous SCORE in MONICA and HAPIEE (not presented).
It is difficult to compare our findings on SCORE calibration to other CEE/FSU data, due to the above-mentioned lack of similar local studies. However, our results are consistent with the evidence from Western studies, which suggest that original and recalibrated SCORE versions tend to overpredict risk in populations with declining CVD rates.23,25–27 Our data on SCORE discrimination also agree with the results for Western populations. In particular, similar to the findings for MONICA and HAPIEE men, SCORE sensitivity was higher than its specificity across the high-risk SCORE Project cohorts7 and among middle-aged Belgians.28 In agreement with our results for MONICA and HAPIEE women, lower sensitivity and higher specificity of SCORE were demonstrated for the low-risk SCORE Project cohorts7 and in middle-aged adults from Finland,29 Iceland,25 Spain,30 and Austria.23 Low SCORE PPVs were observed not only in MONICA and HAPIEE but also in middle-aged Spaniards30 and Austrians.23 The Harrell's C-values in MONICA and HAPIEE were close to AUROC values reported for the high- and low-risk SCORE Project cohorts7 and middle-aged adults from Norway,26 Iceland,25 and Austria.23 However, only in two of our samples (Polish and Russian HAPIEE women), Harrell's C-values exceeded 0.70, which suggests only moderate discrimination.
To summarize, the high-risk SCORE was a significant predictor of fatal atherosclerotic CVD in MONICA and HAPIEE, but it underpredicted the risk in Russian MONICA and could overestimate the risk in Czech and Polish HAPIEE. These findings have several implications. First, the high-risk SCORE can be still used for populations with high cardiovascular mortality levels, such as Russia. For countries where fatal CVD is declining, such as the Czech Republic and Poland, the low-risk SCORE might be preferable. A longer-term solution is SCORE recalibration for specific CEE/FSU populations, using local levels of CVD mortality and risk factors. Second, SCORE performance might benefit from the model's extension by additional risk determinants,31–33 such as socioeconomic parameters or hazardous drinking characteristics. Third, our study has reemphasized the importance of conventional risk factors for CVD prediction and prevention. Controlling these factors in higher-risk groups and individuals and across whole populations will reduce the burden of CVD in CEE/FSU and prevent the reversal of declining CVD rates elsewhere.3,5,34 Finally, as demonstrated by a steady decline in cardiovascular mortality across most Western populations over the last 50 years and, more recently, by the positive dynamic of Czech and Polish CVD trends,8 the task of reducing CVD burden in CEE and particularly FSU is challenging but nonetheless feasible.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
The WHO MONICA Project in the Czech Republic, Poland, Lithuania, and Russia was supported by Czech and Polish Ministries of Health, Polish National Committee for Scientific Research, Lithuanian Ministry of Education and Science, and Russian Academy of Medical Sciences. The HAPIEE study has been supported by the Wellcome Trust (grant numbers 064947/Z/01/Z, 081081/Z/06/Z); the National Institute of Aging (1R01 AG23522); and the MacArthur Foundation (71208).
Conflict of interest: None declared.
Supplementary Material
Acknowledgements
We thank study participants and local collaborators in the Czech Republic, Poland, Lithuania, and Russia.
References
- 1.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organisation. Prevention of Cardiovascular Disease: Guidelines for Assessment and Management of Total Cardiovascular Risk. Geneva: WHO; 2007. [Google Scholar]
- 3.Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30:427–432. doi: 10.1093/ije/30.3.427. [DOI] [PubMed] [Google Scholar]
- 4.Brindle P, Beswick A, Fahey T, Ebrahim S. Accuracy and impact of risk assessment in the primary prevention of cardiovascular disease: a systematic review. Heart. 2006;92:1752–1759. doi: 10.1136/hrt.2006.087932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvanne M, Scholte Op Reimer WJ, Vrints C, Wood D, Zamorano JL, Zannad F. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur Heart J. 2012;33:1635–1701. doi: 10.1093/eurheartj/ehs092. [DOI] [PubMed] [Google Scholar]
- 6.Anderson KM, Wilson PW, Odell PM, Kannel WB. An updated coronary risk profile. A statement for health professionals. Circulation. 1991;83:356–362. doi: 10.1161/01.cir.83.1.356. [DOI] [PubMed] [Google Scholar]
- 7.Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, Ducimetiere P, Jousilahti P, Keil U, Njolstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organisation. Health for All database http://data.euro.who.int/hfamdb (30 November 2012)
- 9.Tunstall-Pedoe Hugh, editor. World Health Organisation MONICA Project. MONICA Monograph and Multimedia Sourcebook: World's Largest Study of Heart Disease, Stroke, Risk Factors and Population Trends 1979–2002. Geneva: 2003. WHO MONICA Project. [Google Scholar]
- 10.Kuulasmaa K, Tunstall-Pedoe H, Dobson A, Fortmann S, Sans S, Tolonen H, Evans A, Ferrario M, Tuomilehto J. Estimation of contribution of changes in classic risk factors to trends in coronary-event rates across the WHO MONICA Project populations. Lancet. 2000;355:675–687. doi: 10.1016/s0140-6736(99)11180-2. [DOI] [PubMed] [Google Scholar]
- 11.Peasey A, Bobak M, Kubinova R, Malyutina S, Pajak A, Tamosiunas A, Pikhart H, Nicholson A, Marmot M. Determinants of cardiovascular disease and other non-communicable diseases in Central and Eastern Europe: rationale and design of the HAPIEE study. BMC Public Health. 2006;6:255. doi: 10.1186/1471-2458-6-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cifkova R, Byma S, Ceska R, Horky K, Karen I, Kunesova M, Kralikov E, Rosolova H, Roztocil K, Soska V, Skhra J. Prevence kardiovaskularnich onemocneni v dospelem veku. Spolecne doporuceni ceskych odbornych spolecnosti. Supplementum Cor Vasa. 2005;47:3–14. [Google Scholar]
- 13.Podolec P, Kopec G, Pajak A, Undas A, Kozek E, Tykarski A, Naruszewicz M, Stanczyk J, Opala G, Godycki-Cwirko M, Rynkiewicz A, Torbicki A, Musial J. Polish forum for prevention guidelines on cardiovascular risk assessment. Kardiol Pol. 2007;65:100–104. [PubMed] [Google Scholar]
- 14.Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, Elkind MS, Go AS, Harrell FE, Jr, Hong Y, Howard BV, Howard VJ, Hsue PY, Kramer CM, McConnell JP, Normand SL, O'Donnell CJ, Smith SC, Jr, Wilson PW. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119:2408–2416. doi: 10.1161/CIRCULATIONAHA.109.192278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Royston P, Moons KG, Altman DG, Vergouwe Y. Prognosis and prognostic research: developing a prognostic model. BMJ. 2009;338:b604. doi: 10.1136/bmj.b604. [DOI] [PubMed] [Google Scholar]
- 16.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 17.Lee ET, Go OT. Survival analysis in public health research. Annu Rev Public Health. 1997;18:105–134. doi: 10.1146/annurev.publhealth.18.1.105. [DOI] [PubMed] [Google Scholar]
- 18.Donders AR, van der Heijden GJ, Stijnen T, Moons KG. Review: a gentle introduction to imputation of missing values. J Clin Epidemiol. 2006;59:1087–1091. doi: 10.1016/j.jclinepi.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 19.Rubin DB. Multiple imputation after 18+ Years. J Am Stat Assoc. 1996;91:473–489. [Google Scholar]
- 20.World Health Organisation. Global InfoBase https://apps.who.int/infobase/Index.aspx (30 November 2012)
- 21.Farzadfar F, Finucane MM, Danaei G, Pelizzari PM, Cowan MJ, Paciorek CJ, Singh GM, Lin JK, Stevens GA, Riley LM, Ezzati M. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3.0 million participants. Lancet. 2011;377:578–586. doi: 10.1016/S0140-6736(10)62038-7. [DOI] [PubMed] [Google Scholar]
- 22.Danaei G, Finucane MM, Lin JK, Singh GM, Paciorek CJ, Cowan MJ, Farzadfar F, Stevens GA, Lim SS, Riley LM, Ezzati M. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5.4 million participants. Lancet. 2011;377:568–577. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 23.Ulmer H, Kollerits B, Kelleher C, Diem G, Concin H. Predictive accuracy of the SCORE risk function for cardiovascular disease in clinical practice: a prospective evaluation of 44 649 Austrian men and women. Eur J Cardiovasc Prev Rehabil. 2005;12:433–441. doi: 10.1097/01.hjr.0000174791.47059.80. [DOI] [PubMed] [Google Scholar]
- 24.Vlismas K, Panagiotakos DB, Pitsavos C, Chrysohoou C, Skoumas Y, Stavrinos V, Stefanadis C. The role of dietary and socioeconomic status assessment on the predictive ability of the HellenicSCORE. Hellenic J Cardiol. 2011;52:391–398. [PubMed] [Google Scholar]
- 25.Aspelund T, Thorgeirsson G, Sigurdsson G, Gudnason V. Estimation of 10-year risk of fatal cardiovascular disease and coronary heart disease in Iceland with results comparable with those of the Systematic Coronary Risk Evaluation project. Eur J Cardiovasc Prev Rehabil. 2007;14:761–768. doi: 10.1097/HJR.0b013e32825fea6d. [DOI] [PubMed] [Google Scholar]
- 26.Lindman AS, Veierod MB, Pedersen JI, Tverdal A, Njolstad I, Selmer R. The ability of the SCORE high-risk model to predict 10-year cardiovascular disease mortality in Norway. Eur J Cardiovasc Prev Rehabil. 2007;14:501–507. doi: 10.1097/HJR.0b013e328011490a. [DOI] [PubMed] [Google Scholar]
- 27.van Dis I, Kromhout D, Geleijnse JM, Boer JM, Verschuren WM. Evaluation of cardiovascular risk predicted by different SCORE equations: the Netherlands as an example. Eur J Cardiovasc Prev Rehabil. 2010;17:244–249. doi: 10.1097/HJR.0b013e328337cca2. [DOI] [PubMed] [Google Scholar]
- 28.De Bacquer D, De Backer G. Predictive ability of the SCORE Belgium risk chart for cardiovascular mortality. Int J Cardiol. 2010;143:385–390. doi: 10.1016/j.ijcard.2009.03.101. [DOI] [PubMed] [Google Scholar]
- 29.Ketola E, Laatikainen T, Vartiainen E. Evaluating risk for cardiovascular diseases—vain or value? How do different cardiovascular risk scores act in real life. Eur J Public Health. 2009;20:107–112. doi: 10.1093/eurpub/ckp070. [DOI] [PubMed] [Google Scholar]
- 30.Comin E, Solanas P, Cabezas C, Subirana I, Ramos R, Gene-Badia J, Cordon F, Grau M, Cabre-Vila JJ, Marrugat J. Estimating cardiovascular risk in Spain using different algorithms. Rev Esp Cardiol. 2007;60:693–702. [PubMed] [Google Scholar]
- 31.Cooney MT, Dudina A, De Bacquer D, Fitzgerald A, Conroy R, Sans S, Menotti A, De Backer G, Jousilahti P, Keil U, Thomsen T, Whincup P, Graham I. How much does HDL cholesterol add to risk estimation? A report from the SCORE investigators. Eur J Cardiovasc Prev Rehabil. 2009;16:304–314. doi: 10.1097/HJR.0b013e3283213140. [DOI] [PubMed] [Google Scholar]
- 32.Cooney MT, Vartiainen E, Laatikainen T, Joulevi A, Dudina A, Graham I. Simplifying cardiovascular risk estimation using resting heart rate. Eur Heart J. 2010;31:2141–2147. doi: 10.1093/eurheartj/ehq164. [DOI] [PubMed] [Google Scholar]
- 33.Sehestedt T, Jeppesen J, Hansen TW, Wachtell K, Ibsen H, Torp-Pedersen C, Hildebrandt P, Olsen MH. Risk prediction is improved by adding markers of subclinical organ damage to SCORE. Eur Heart J. 2010;31:883–891. doi: 10.1093/eurheartj/ehp546. [DOI] [PubMed] [Google Scholar]
- 34.Mendis S, Lindholm LH, Anderson SG, Alwan A, Koju R, Onwubere BJ, Kayani AM, Abeysinghe N, Duneas A, Tabagari S, Fan W, Sarraf-Zadegan N, Nordet P, Whitworth J, Heagerty A. Total cardiovascular risk approach to improve efficiency of cardiovascular prevention in resource constrain settings. J Clin Epidemiol. 2011;64:1451–1462. doi: 10.1016/j.jclinepi.2011.02.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.