Abstract
OBJECTIVE
To compare breastfeeding duration in postpartum mothers randomized to a behavioral educational intervention versus enhanced usual care.
STUDY DESIGN
Randomized trial. Self-identified black and Latina early postpartum mothers were randomized to receive a behavioral educational intervention or enhanced usual care. The two-step intervention aimed to prepare and educate mothers about postpartum symptoms and experiences (including tips on breastfeeding and breast/nipple pain), bolster social support and self-management skills. Enhanced usual care participants received a list of community resources and received a 2-week control call. Intention-to-treat analyses examined breastfeeding duration (measured in weeks) for up to six-months of follow-up. This study is registered with clinicaltrial.gov (NCT01312883).
RESULTS
Five hundred forty mothers were randomized to the intervention (n=270) versus controls (n=270). Mean age was 28 (range 18–46); 62% were Latina and 38% were black. Baseline sociodemographic, clinical, psycho-social, and breastfeeding characteristics were similar among intervention versus controls. Mothers in the intervention arm breastfed for longer duration than controls (median of 12.0 weeks versus 6.5 weeks, respectively, p =.02) Mothers in the intervention arm were less likely to quit breastfeeding over the first six-months postpartum (hazard ratio of 0.79; 95% CI 0.65–0.97).
CONCLUSION
A behavioral educational intervention increased breastfeeding duration among low-income, self-identified black and Latina mothers during the six-month postpartum period.
Keywords: breastfeeding, intervention, minority, postpartum, randomized trial
Breastfeeding provides substantial health benefits for children and mothers and the American Academy of Pediatrics strongly recommends breastfeeding for the first year of life.1,2 The health benefits of breastfeeding are consequential including reduced infection rates, obesity, and postneonatal mortality among children, and a lower risk of breast and ovarian cancer among mothers.1,2 Each additional week of breastfeeding confers benefit.3
Unfortunately, significant racial/ethnic disparities in breastfeeding initiation and duration exist in the US with black women having lower rates of both as compared with white women.4 While national data suggest that Latino women have breastfeeding rates similar to those of whites, significantly different patterns of breastfeeding continuation rates exist among certain low-income subgroups of Latinos.5,6 Culturally sensitive interventions targeting groups with the worst breastfeeding outcomes are needed.6 We report results of a randomized trial testing a behavioral educational intervention with the secondary aim of increasing breastfeeding duration among minority mothers.
MATERIALS AND METHODS
The primary aim of this randomized controlled trial tested whether a 2-step behavioral educational intervention reduced postpartum depressive symptoms among minority mothers and details have been published elsewhere.7 Here we report results on the secondary aim of this trial which was to examine whether this 2-step intervention extended duration of breastfeeding during the six-month postpartum period.
Eligibility
We enrolled 540 self-identified black and Latina postpartum women who delivered at a large tertiary hospital located in New York City between April 2009 and March 2010. The Icahn School of Medicine at Mount Sinai Program for Protection of Human Subjects approved this study. The patient sample was identified through an electronic documentation system for the labor and delivery unit. Eligible participants were black/African American or Latina/Hispanic, ≥18 years, had infants with birth weights >2500 grams and 5-minute Apgar scores ≥7. Maternal race/ethnicity, maternal age, infant Apgar scores, and infant birth weight are contained in the electronic system. Bilingual clinical research coordinators asked additional questions related to race and ethnicity. Mothers who self-identified black/African American or Latina/Hispanic, spoke English or Spanish, and had a working telephone were eligible. Mothers were recruited during their postpartum hospital stay, consented, underwent a baseline interview, and then were randomized to intervention versus control.
Intervention and Control
The behavioral educational intervention aimed to prepare and educate mothers about postpartum symptoms and experiences (including tips on breastfeeding and breast/nipple pain), bolster social support and self-management skills, and included an in-hospital educational session with a social worker, educational materials, and a 2-week follow-up call. Mothers randomized to the intervention arm, were given a two-step intervention. The first step occurred in the hospital when a masters-trained bilingual social worker reviewed an education pamphlet and partner summary sheet with each mother. Education materials included information on breastfeeding, breast/nipple pain, c-section site pain, episiotomy site pain, urinary incontinence, back pain, headaches, hair loss, hemorrhoids, infant colic, and depressive symptoms. Additional information was provided on social support. A partner summary sheet spelled out the typical pattern of experience for mothers postpartum in an effort to normalize the experience. During the second step, the 2-week post-delivery call, the social worker assessed patients’ symptoms, skills in symptom management and other needs. Patients and social worker created action plans to address current needs including accessing community resources. Enhanced usual care participants received a list of community resources and received a 2-week control call.7
The intervention was culturally tailored. The intervention was revised based on the results of a pilot-test with 50 diverse postpartum mothers and review with obstetricians, psychiatrists, and social workers. The intervention was further revised based on feedback from focus groups with black and Latina postpartum mothers and our community action board. All materials were translated into Spanish and back-translated for accuracy and consistency of meaning. Content, pictures, wording, and length were revised according to these sources.7
Assessments
Data were collected in-person at baseline and by telephone during follow-up interviews by bilingual clinical research coordinators blinded to intervention status. Interviews occurred by phone at 3-weeks (mean days = 27.6, SD 5.8), 3-months (mean days = 83.5, SD 7.8) and 6-months (mean days = 175.6, SD 8.9) postpartum. Mothers were asked a series of questions about breastfeeding, including importance of breastfeeding and breastfeeding support, physical and emotional symptoms, social support, and healthcare factors. The dependent variable, breastfeeding duration, was ascertained by asking mothers how long they breastfed their infants (in weeks). At each interview mothers were asked if they were currently breastfeeding their infant. If they answered no, they were asked how long they breastfed their infant postpartum. Variables that were selected for inclusion in our analyses were: maternal socio-demographic characteristics (age, race/ethnicity, nativity, language, educational attainment, insurance coverage, marital status, and work status), maternal health and clinical characteristics (parity, delivery type, presence of comorbid conditions, and antepartum complications), maternal psycho-social characteristics (social support, partner support, and past history of depression), and breastfeeding characteristics (perceived importance of breastfeeding and breastfeeding support).
Maternal depressive symptoms were measured with the Edinburgh Postnatal Depression Scale (EPDS), a 10-item self-report scale. The EPDS is a validated, widely used postpartum depression screening instrument.8,9 We used an EPDS score ≥10 as indicating possible depression. Although a number of cut-off points have been used, it is recommended that to minimize the failed detection of depressive cases, a cut-off score of 9/10 be used.8,9 The Generalized Anxiety Disorder, seven-item scale (GAD-7), was used to assess generalized anxiety disorder.10 A cut-point of 10, which has been found to measure moderate anxiety, was used. General social support was assessed by taking the mean of three items which measured emotional support, instrumental support with the baby, and instrumental support with the household, responses (cronbach α = 0.701), responses ranged from 0 to 4.11,12 The partner support scale was constructed by taking the mean of the two items (cronbach α = 0.693) and had a range of 0 to 4.11,12
Women’s breastfeeding characteristics were assessed by four questions. First, respondents were asked “How important is breastfeeding?” Responses were coded as (1) “extremely” or “quite a bit” and (0) “moderately”, “a little bit” or “not at all”. Subjects were also asked if they received breastfeeding support from health care providers, partners, and family or friends. Each response was coded (1) “yes” and (0) “no”. In addition, each mother was asked whether her infant received breastmilk only, formula only, or both at the six-month assessment.
Statistical Analyses
Randomization procedures and sample size calculations have been reported.7 All statistical analyses were done using PC SAS version 9.2 (SAS Institute Inc., Cary, NC). Intervention status was the key independent variable in the current analyses. Bivariate analyses were conducted using chi square tests and t-tests to assess the association between sociodemographic, clinical, and breastfeeding characteristics with intervention status. Intention-to-treat analyses examined breastfeeding duration (measured in weeks). Twenty-six women, who indicated that they were breastfeeding at baseline, were missing breastfeeding duration data at all three follow-up time points and were assigned the midpoint value of two weeks for breastfeeding duration. This represented the midpoint between the time from their baseline interview and the next scheduled follow-up assessment (mean of 27.6 days for trial participants). Kaplan Meier analysis was used to test the effect of the intervention on breastfeeding duration for up to six months of follow-up. Kaplan Meier curves were compared using the log rank test. Cox regression analysis was used to calculate hazard ratios (HRs) with 95% confidence intervals. Additional analyses examined breastfeeding duration among the 451 mothers who initiated breastfeeding. Results were similar and we therefore present only intention to treat results.
RESULTS
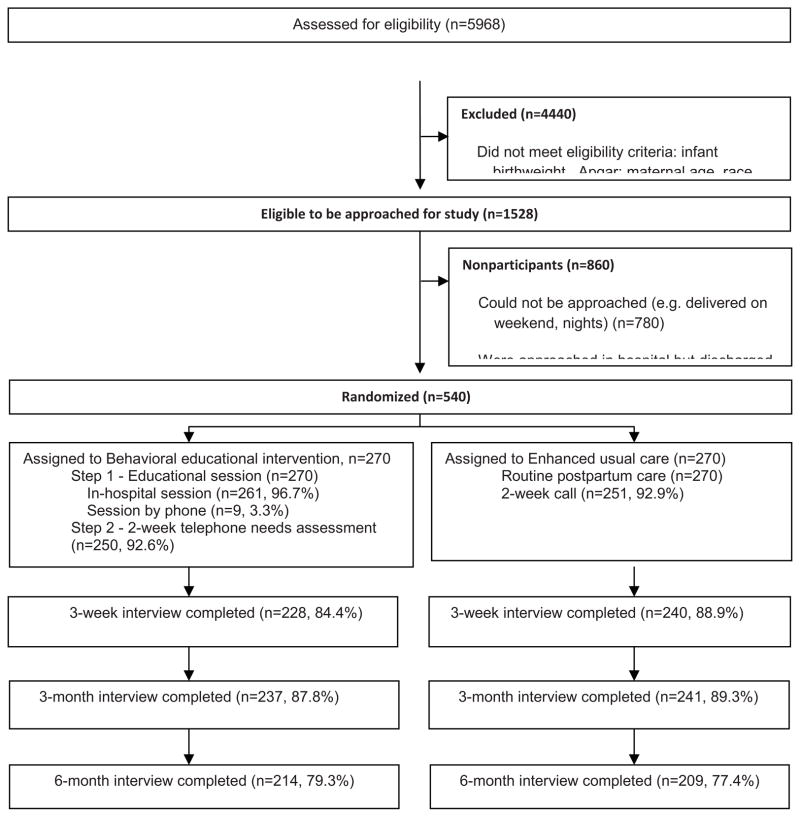
The refusal rate was 19%.7 Among the 540 mothers enrolled, rates for follow-up interviews were 87% at 3-weeks, and 89% at 3 months and 78% at 6 months.(Figure 1). Table 1 shows the baseline characteristics of the sample. The overall mean age of enrolled participants was 28 (range 18–46); 38% were black and 62% were Latina. Thirty-six percent of participants were foreign born, 21% were primarily Spanish speaking and 63% had Medicaid insurance. There were no clinically important differences between intervention and control groups in baseline sociodemographic, clinical, and psychosocial characteristics except that comorbid conditions were more prevalent among the controls than intervention (27% vs. 20%, p=.05). There was no difference in prevalence rates of returning to work between intervention and controls. In addition there was no statistically significant difference by race in positive depression screens or positive screens for anxiety (results not shown).
Figure 1.
Participants’ flow through study*
*Howell EA, Balbierz A, Wang J, Parides M, Zlotnick C, Leventhal H. Reducing postpartum depressive symptoms among black and Latina mothers: a randomized controlled trial. Obstet Gynecol. May 2012;119(5):942–949.
Table 1.
Demographic, Clinical, and Breastfeeding Characteristics of Study Participants. (N=540)
| Total (N= 540) | Intervention (N=270) | Control (N=270) | p-value | |
|---|---|---|---|---|
| Sociodemographic Characteristics | ||||
| Age (range 18–46) | 27.79 (6.00) | 28.21 (5.84) | 27.37 (6.13) | 0.10 |
| Race | 0.44 | |||
| Black/African American | 203 (38) | 97 (36) | 106 (39) | |
| Hispanic/Latina | 337 (62) | 173 (64) | 164 (61) | |
| Foreign Born | 193 (36) | 101 (37) | 92 (34) | 0.41 |
| Primarily Spanish speaking | 113 (21) | 60 (22) | 53 (20) | 0.45 |
| High School or Less | 248 (46) | 117 (43) | 131 (49) | 0.23 |
| Medicaid/Medicaid Managed Care | 339 (63) | 168 (62) | 171 (63) | 0.78 |
| Single/Separated/Divorced/Widowed | 206 (38) | 102 (38) | 104 (39) | 0.85 |
| Returned to work at 1m postpartum | 0 (0) | 0 (0) | 0 (0) | - |
| Returned to work at 3m postpartum | 126 (23) | 59 (22) | 67 (25) | 0.42 |
| Returned to work at 6m postpartum | 178 (33) | 90 (33) | 88 (33) | 0.85 |
| Clinical and Characteristics | ||||
| Primiparous | 220 (41) | 107 (40) | 113 (42) | 0.70 |
| Delivered by C-Section | 208 (39) | 105 (39) | 103 (38) | 0.83 |
| Comorbid Condition | 125 (23) | 53 (20) | 72 (23) | 0.05 |
| Antepartum Complication | 124 (23) | 65 (24) | 59 (22) | 0.52 |
| Psycho-Social Characteristics | ||||
| Screened positive for depression at baseline (Edinburgh Postpartum Depression Scale) | 82 (15) | 37 (14) | 45 (17) | 0.34 |
| Screened positive for anxiety (Generalized Anxiety Disorder-7 item scale) | 99 (18) | 49 (18) | 50 (19) | 0.91 |
| General Social Support Scale (0–4) | 3.24 (0.91) | 3.28 (0.92) | 3.21 (0.89) | 0.37 |
| General Partner Support Scale (0–4) | 2.87 (1.07) | 2.82 (1.12) | 2.92 (1.02) | 0.29 |
| Breastfeeding Characteristics | ||||
| Initiated breastfeeding | 451 (84) | 231 (86) | 220 (81) | 0.20 |
| Perceived Breastfeeding as Important | 443 (82) | 220 (82) | 223 (83) | 0.74 |
| Received breastfeeding support by healthcare provider | 339 (63) | 162 (60) | 177 (66) | 0.18 |
| Received breastfeeding support by partner | 324 (60) | 159 (59) | 165 (61) | 0.60 |
| Received breastfeeding support by family/friend | 357 (66) | 177 (66) | 180 (67) | 0.79 |
Values are numbers (%) unless otherwise specified. Mean and (SD) for continuous variables.
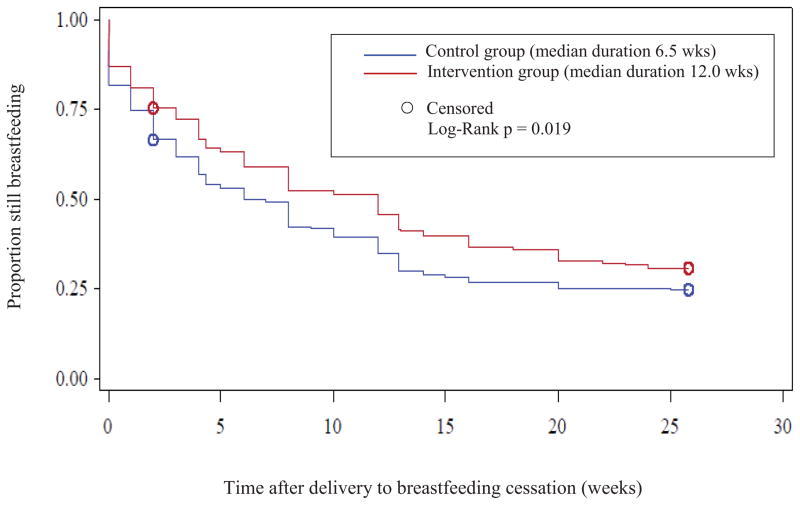
Eighty-four percent of participants initiated breastfeeding (in both trial arms) and the majority of participants perceived breastfeeding as important and received breastfeeding support from partners, family and healthcare providers. Kaplan Meier analysis revealed a statistically significant difference in time to cessation between the intervention and control group (log rank test, p=0.019) over the six month postpartum period (Fig. 2). Median breastfeeding duration was 12.0 weeks for the intervention group and 6.5 weeks for women in the control group. Mothers in the intervention group were less likely to quit breastfeeding over the six-month period (hazard ratio of 0.79; 95% CI 0.65–0.97). There was no statistically significant difference in exclusive breastfeeding at six-months postpartum between the intervention group versus the control group (7% versus 4%, respectively).
Figure 2.
Breastfeeding duration for intervention versus control.
COMMENT
The results of this trial suggest that a behaviorally focused, educational intervention, delivered in the postpartum inpatient setting, has the potential to increase the duration of breastfeeding among black and Latina mothers. Our intervention, designed to educate and prepare mothers for the postpartum experience was successful in our primary aim of reducing postpartum depressive symptoms among black and Latina mothers.7 The current results demonstrate that this behaviorally focused, educational intervention was also successful in extending duration of breastfeeding among a predominantly low-income group of black and Latina mothers. Our intervention is one of few successful interventions to improve breastfeeding rates among minority women.6
The results of our trial are consistent with published literature suggesting that support and education are important factors associated with breastfeeding status.13–16 Our intervention addressed situational factors correlated with postpartum depression and included education on physical symptoms, breast/nipple pain, breastfeeding problems, and social support.7 Studies suggest that women cite nipple pain as a major reason for stopping, and that higher levels of support increase breastfeeding.13,17–19
Our intervention was conducted after the completion of the baseline survey and was not expected to impact breastfeeding initiation rates. The fact that rates of initiation, importance of breastfeeding, and breastfeeding support were similar among the intervention versus control groups suggests that our randomization was successful. This is important as each of these factors is correlated with breastfeeding duration. As with all randomized trials, women who consented to participate may be different than women who chose not to and thus may limit the generalizability of our findings. However, our refusal rate was very low.7 Recall bias may have affected a mother’s answers to duration of breastfeeding, however, mothers were asked this question several times over the first six months postpartum.
A behavioral educational intervention extended breastfeeding duration among black and Latina mothers. The public health implications of this promising intervention are significant as improving breastfeeding rates is included in Healthy People 2020 goals and interventions to improve breastfeeding among those with the lowest rates are particularly needed.6 Future research should be directed at evaluating dissemination efforts of successful interventions to increase breastfeeding among at risk populations.
Acknowledgments
This work was supported by the National Institute on Minority Health and Health Disparities (5P60MD000270-10) and the National Institute of Mental Health (5R01MH77683-2). The authors report no conflict of interest.
Footnotes
This research was presented as a poster at the Academy Health Annual Meeting, Baltimore, MD June 23, 2013.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Singh GK, Kogan MD, Dee DL. Nativity/immigrant status, race/ethnicity, and socioeconomic determinants of breastfeeding initiation and duration in the United States, 2003. Pediatrics. 2007 Feb;119 (Suppl 1):S38–46. doi: 10.1542/peds.2006-2089G. [DOI] [PubMed] [Google Scholar]
- 2.Gartner LM, Morton J, Lawrence RA, et al. Breastfeeding and the use of human milk. Pediatrics. 2005 Feb;115(2):496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- 3.Pettigrew MM, Khodaee M, Gillespie B, Schwartz K, Bobo JK, Foxman B. Duration of breastfeeding, daycare, and physician visits among infants 6 months and younger. Ann Epidemiol. 2003 Jul;13(6):431–435. doi: 10.1016/s1047-2797(02)00463-5. [DOI] [PubMed] [Google Scholar]
- 4.Racial and ethnic differences in breastfeeding initiation and duration by state - National Immunization Survey, United States, 2004–2008. MMWR Morb Mortal Wkly Rep. 2010 Mar 26;59(11):327–334. [PubMed] [Google Scholar]
- 5.Chapman DJ, Damio G, Young S, Perez-Escamilla R. Effectiveness of breastfeeding peer counseling in a low-income, predominantly Latina population: a randomized controlled trial. Arch Pediatr Adolesc Med. 2004 Sep;158(9):897–902. doi: 10.1001/archpedi.158.9.897. [DOI] [PubMed] [Google Scholar]
- 6.Chapman DJ, Perez-Escamilla R. Breastfeeding among minority women: moving from risk factors to interventions. Adv Nutr. 2012 Jan;3(1):95–104. doi: 10.3945/an.111.001016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howell EA, Balbierz A, Wang J, Parides M, Zlotnick C, Leventhal H. Reducing postpartum depressive symptoms among black and latina mothers: a randomized controlled trial. Obstet Gynecol. 2012 May;119(5):942–949. doi: 10.1097/AOG.0b013e318250ba48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cox AD, Puckering C, Pound A, Mills M. The impact of maternal depression in young children. J Child Psychol Psychiatry. 1987 Nov;28(6):917–928. doi: 10.1111/j.1469-7610.1987.tb00679.x. [DOI] [PubMed] [Google Scholar]
- 9.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987 Jun;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 10.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006 May 22;166(10):1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 11.Howell EA, Mora PA, Horowitz CR, Leventhal H. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstet Gynecol. 2005 Jun;105(6):1442–1450. doi: 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howell EA, Mora PA, DiBonaventura MD, Leventhal H. Modifiable factors associated with changes in postpartum depressive symptoms. Arch Womens Ment Health. 2009 Apr;12(2):113–120. doi: 10.1007/s00737-009-0056-7. [DOI] [PubMed] [Google Scholar]
- 13.Milligan RA, Pugh LC, Bronner YL, Spatz DL, Brown LP. Breastfeeding duration among low income women. J Midwifery Womens Health. 2000 May-Jun;45(3):246–252. doi: 10.1016/s1526-9523(00)00018-0. [DOI] [PubMed] [Google Scholar]
- 14.Anderson AK, Damio G, Young S, Chapman DJ, Perez-Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Arch Pediatr Adolesc Med. 2005 Sep;159(9):836–841. doi: 10.1001/archpedi.159.9.836. [DOI] [PubMed] [Google Scholar]
- 15.Bentley ME, Caulfield LE, Gross SM, et al. Sources of influence on intention to breastfeed among African-American women at entry to WIC. J Hum Lact. 1999 Mar;15(1):27–34. doi: 10.1177/089033449901500109. [DOI] [PubMed] [Google Scholar]
- 16.Bonuck KA, Trombley M, Freeman K, McKee D. Randomized, controlled trial of a prenatal and postnatal lactation consultant intervention on duration and intensity of breastfeeding up to 12 months. Pediatrics. 2005 Dec;116(6):1413–1426. doi: 10.1542/peds.2005-0435. [DOI] [PubMed] [Google Scholar]
- 17.Pugh LC, Milligan RA, Frick KD, Spatz D, Bronner Y. Breastfeeding duration, costs, and benefits of a support program for low-income breastfeeding women. Birth. 2002 Jun;29(2):95–100. doi: 10.1046/j.1523-536x.2002.00169.x. [DOI] [PubMed] [Google Scholar]
- 18.Grossman LK, Fitzsimmons SM, Larsen-Alexander JB, Sachs L, Harter C. The infant feeding decision in low and upper income women. Clin Pediatr (Phila) 1990 Jan;29(1):30–37. doi: 10.1177/000992289002900105. [DOI] [PubMed] [Google Scholar]
- 19.Feinstein JM, Berkelhamer JE, Gruszka ME, Wong CA, Carey AE. Factors related to early termination of breast-feeding in an urban population. Pediatrics. 1986 Aug;78(2):210–215. [PubMed] [Google Scholar]