Abstract
Objective
To determine the influence of maternal health literacy and child’s age on participation in social welfare programs benefiting children.
Methods
In a longitudinal prospective cohort study of 560 Medicaid-eligible mother-infant dyads recruited in Philadelphia, maternal health literacy was assessed using the Test of Functional Health Literacy in Adults (short version). Participation in social welfare programs (Temporary Assistance to Needy Families [TANF], Supplemental Nutrition Assistance Program [SNAP], Special Supplemental Nutrition Program for Women, Infants, and Children [WIC], child care subsidy, and public housing) was self-reported at child’s birth, and at the 6, 12, 18, 24 month follow-up interviews. Generalized estimating equations quantified the strength of maternal health literacy as an estimator of program participation.
Results
The mothers were primarily African-Americans (83%), single (87%), with multiple children (62%). Nearly 24% of the mothers had inadequate or marginal health literacy. Children whose mothers had inadequate health literacy were less likely to receive child care subsidy (adjusted OR= 0.54, 95% CI: 0.34–0.85) than children whose mothers had adequate health literacy. Health literacy was not a significant predictor for TANF, SNAP, WIC or housing assistance. The predicted probability for participation in all programs decreased from birth to 24 months. Most notably, predicted WIC participation declined rapidly after age one.
Conclusions
During the first 24 months, mothers with inadequate health literacy could benefit from simplified or facilitated child care subsidy application processes. Targeted outreach and enrollment efforts conducted by social welfare programs need to take into account the changing needs of families as children age.
Keywords: health literacy, enrollment, social welfare programs
Introduction
Federally funded social welfare programs such as Medicaid, the Supplemental Nutrition Assistance Program (SNAP, formerly known as Food Stamps), and housing assistance have been found to mitigate the effects of poverty and improve health outcomes for children in low-income families (1–4). However, a significant group of eligible children are still not enrolled in these social welfare programs (5–7). Studies have found that complicated application and renewal processes lowered retention rates for Medicaid and the Children’s Health Insurance Program (CHIP) (8, 9). The application processes for other social welfare programs often follow the Medicaid application format and are often as complex (10–12). To navigate the healthcare system and social welfare programs, parents need to be health literate, which is defined as ‘the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions (13).’ Parents with limited health literacy have trouble entering names and birth dates on health insurance forms and are more likely to have a child without health insurance (14). Thus, limited parental health literacy likely leads to inadequate engagement in these social welfare programs, and, ultimately, poor child health outcomes.
The influence of parental health literacy on participation in social welfare programs remains relatively unexplored. The first study to look at parental health literacy and participation in social welfare programs found that mothers with inadequate health literacy were less likely to receive Temporary Assistance for Needy Families (TANF) than were mothers with adequate and marginal health literacy when the infants reached 6 months of age (15). In addition, programs with streamlined institutionalized enrollment protocols, such as the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), appear to have much higher enrollment rates than those programs with more complex and fragmented procedures (15).
The aim of this study is to extend our understanding of the relationship between maternal health literacy and social welfare program participation beyond the first 6 months of life. We hypothesize that the influence of maternal health literacy becomes less important for participation in these social welfare programs after initial enrollment at birth. These findings have direct relevance for the development and implementation of enrollment and eligibility, enrollment, and renewal processes for public assistance programs designed to support needy families.
Methods
Study design and data source
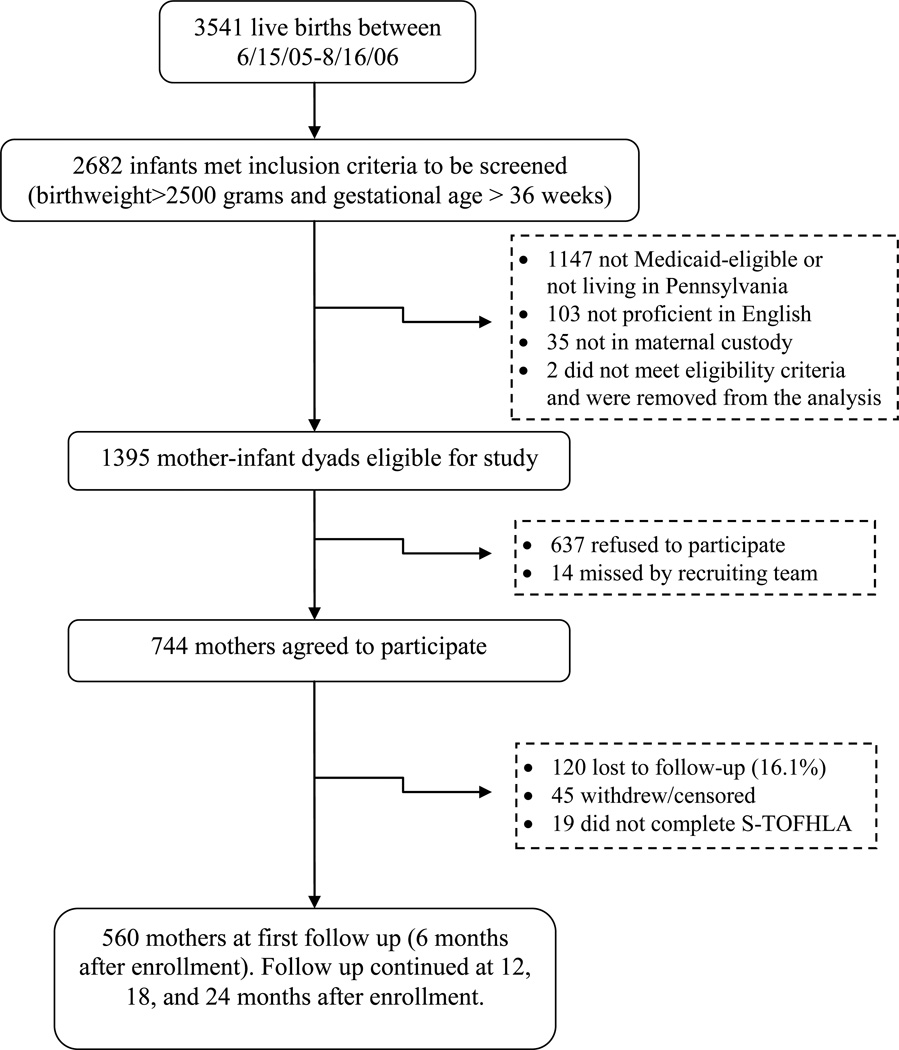
The data source for these secondary analyses was the Health Insurance Improvement Project (HIP), a longitudinal prospective cohort study of maternal and child patterns of Medicaid enrollment (15, 16). Mother-infant dyads were recruited from the post-partum wards of a large Philadelphia hospital between June 15, 2005 and August 6, 2006. Mothers who were: 1) enrolled and/or eligible for Medicaid as recorded in the hospital medical record; and 2) spoke proficient English based on the gestalt impression of the research assistant doing the assessment were further screened for eligibility to participate in the study. Infants who had gestational age less than 36 weeks, birth weight less than 2500 grams, or who were not in the well-baby nursery after delivery were excluded. Infants entering foster care or adoption at birth or immediately thereafter were also excluded. The study was approved by the IRB at the Children’s Hospital of Philadelphia and Stony Brook University.
Out of 1395 eligible mother-infant dyads, 744 agreed to participate in the primary study (Appendix A) (15). Although African Americans were less likely than other racial/ethnic groups to participate and students were more likely to participate than other groups, no significant differences in maternal age, education or infant birth weight between participants and non-participants were found (Appendix B). The analytic sample for this study included 560 (75.3%) mother-infant dyads who completed the 6 month follow-up survey and were followed for the remainder of the study period. Unlike the previously published paper using HIP study data for 499 mother-infant dyads from birth through age 6 months, we did not exclude mothers receiving Supplemental Security Income (SSI) in this analysis. African American mothers, mothers with more than a high school education, and US born mothers were more likely than other groups to complete the 6 month follow-up and have health literacy data (Appendix C).
Measures
The primary outcome of interest was self-reported participation in the following social welfare programs: TANF; SNAP, WIC, child care subsidies, and public housing. Surveys were administered by research assistants at birth in-person and then every 6 months via telephone for the remainder of the study period (i.e. 6, 12, 18, 24 months of age). Notably, the actual age of the child at the time of the follow-up interview (e.g., 7 months if the interview was completed at that time) was used in the analyses. Survey items were adapted from the National Health Interview Survey, questions relevant to this study are included in Appendix D (17).
Maternal health literacy and age of child were the primary predictors of interest. Maternal health literacy was assessed using the short form Test of Functional Health Literacy in Adults (S-TOFHLA). The S-TOFHLA is a well-validated measure of functional health literacy that uses specific health related examples to assess reading comprehension (18, 19). The scores for completing the fill-in-the-blanks in the two passages of medical instructions range from 0 to 36: ≤16 limited; 17–22 marginal; and ≥ 23 adequate health literacy (18, 19).
The following covariates were included because these are known to influence participation in public health insurance and social welfare programs (20–28): race/ethnicity, maternal marital status (single, married, divorced), number of children in household, maternal education (less than high school, high school, or beyond high school), maternal employment status, household income, and whether the mother received supplemental security income (SSI).
Statistical analyses
The main goal of these statistical analyses was to assess whether maternal health literacy and child’s age impacted social welfare program participation. We compared baseline characteristics among the health literacy groups using chi-square tests for categorical variables (race/ethnicity, marital status, and employment status) and the Kruskal-Wallis test for ordinal variables (number of children, income, and, maternal education). Descriptively, the participation rate in each social welfare program was also compared between the health literacy groups using chi-square tests at birth, 6 months, 12 months, 18 months and 24 months of age.
We used generalized estimating equations (GEE), with a logit link function, to obtain our best estimate of the relationship between maternal health literacy and participation in each social welfare program, and included the five evaluation time points over two years, six months apart (29). All variables significantly associated with program participation in single variable relationships (p < 0.05) were included in the GEE models for each of the five programs. Child’s age was included as a continuous variable in months. As the association between child’s age and program participation was non-linear for some of the programs, we included a squared (centered at 12 months) age term in the same model. Race, marital status, maternal education, and health literacy were used as fixed variables in the model process. Employment status, income, housing situation, number of children, and SSI status were included as time-varying factors in the models. For the purpose of GEE analyses, the lower endpoint of each income category was used to transform income into a continuous variable. For instance, income for participants in the lowest income category was entered in the model as 1. Participants in second lowest category was entered in the model as 251, the next category was entered as 501, followed by 1001, 1501, 2001, 2501, and 3001. The final model for each program was selected using a best variable subsets approach which is based on choosing the model with the lowest quasi-likelihood information criterion (QIC) statistic from all possible models. Taking a conservative approach, a Bonferroni correction (p < 0.01 for the 5 public programs of interest) was used to declare significance of each of the variables in the final best variables subset models. The GEE model assumes missing at random, i.e., that missing the interview and not having a data point was not associated with program participation. We also used the Marascuilo procedure to compare employment status across health literacy levels because this association could influence the relationship between maternal health literacy and program participation.
All analyses were conducted using SAS® software, version 9.2.
Results
Sample description
Table 1 shows the characteristics of the study population at birth, grouped by maternal literacy level. Nearly 24% of mothers had inadequate (n=58) or marginal (n=74) health literacy. Most mothers were African-Americans (83%), single (87%), and had more than one child (62%). No significant differences in employment status and income among the three health literacy groups were found; however, education was strongly associated with maternal health literacy. Among those mothers with adequate literacy, a higher proportion of participants completed education beyond high school than among those mothers with inadequate or marginal literacy, as expected.
Table 1.
Population characteristics at birth (N= 560)
| Characteristic | Inadequat e Literacy n (%) |
Marginal Literacy n (%) |
Adequate Literacy n (%) |
Total n (%) |
p- value1 |
|
|---|---|---|---|---|---|---|
| Sample Size | 58 | 74 | 428 | 560 | ||
| Maternal race/ethnicity | 0.68 | |||||
| African-American | 46 (79) | 63 (85) | 355 (83) | 464 (83) | ||
| Non-African-American | 12 (21) | 11 (15) | 73 (17) | 96 (17) | ||
| Maternal marital status | 0.15 | |||||
| Single | 52 (90) | 69 (93) | 366 (86) | 487 (87) | ||
| Married/Widowed/Divorced | 6 (10) | 5 (7) | 62 (14) | 73 (13) | ||
| Number of children2 | 0.083 | |||||
| 1 | 26 (45) | 34 (46) | 152 (36) | 212 (38) | ||
| 2 | 11 (19) | 21 (28) | 114 (27) | 146 (26) | ||
| 3 or more | 21 (36) | 19 (26) | 162 (38) | 202 (36) | ||
| Maternal Education | 0.001 | |||||
| Less than High School | 20 (34) | 32 (43) | 119 (28) | 171 (31) | ||
| High School/GED | 15 (26) | 23 (31) | 97 (23) | 135 (24) | ||
| Beyond High School | 23 (40) | 19 (26) | 212 (50) | 254 (45) | ||
| Employment Status3 | 0.47 | |||||
| Student | 21 (39) | 22 (39) | 141 (40) | 184 (39) | ||
| Employed, Full Time | 16 (30) | 16 (29) | 133 (37) | 165 (35) | ||
| Unemployed, looking for employment | 10 (19) | 10 (18) | 38 (11) | 58 (12) | ||
| Unemployed, not looking for employment | 7 (13) | 8 (14) | 45 (13) | 60 (13) | ||
| Income4 | 0.33 | |||||
| Under $250/month | 14 (27) | 22 (35) | 95 (23) | 131 (25) | ||
| $251 – $500/month | 16 (31) | 18 (29) | 113 (28) | 147 (28) | ||
| $501 – $1000/month | 12 (23) | 16 (25) | 92 (23) | 120 (23) | ||
| $1,001 – $1,500/month | 5 (10) | 3 (5) | 49 (12) | 57 (11) | ||
| ≥$1501/month | 5 (10) | 4 (6) | 58 (14) | 67 (13) | ||
P-value is for the chi-square test for race/ethnicity, marital status, and employment status, and Kruskal-Wallis test for number of children, income, and, maternal education.
Number of children is categorized as 1, 2, 3–10 in this table because of the small number of families with more than 3 children.
Missing 93 (16.6% of sample). The health literacy distribution of those missing employment data is not statistically different from those who reported their employment status.
Missing 38 (6.8% of sample). A higher proportion of mothers who reported their income have adequate health literacy than those with missing income (p<0.05). The two groups are not significantly different for the other two levels of health literacy.
Program participation trends during the first 24 months
In Table 2, we present trends in social welfare program participation with child’s age across the entire cohort. Slightly more than half of these Medicaid-eligible families participated in TANF at birth and at six months. Successive decreases in participation occurred at each follow-up such that only 37% of families were receiving TANF at 24 months. For SNAP, participation rates were consistently in the range of 65–73% during the 24 month study period whereas WIC participation varied more widely. Participation in WIC increased more than 20% between birth and 6 months followed by a decrease of 34% between 12 months and 24 months of age. Twelve percent of the families received child care subsidy at birth and that proportion tripled over the 24 month period, while the proportion of families with housing assistance decreased from 59% at birth to 37% at 24 months.
Table 2.
Maternal Health Literacy and Participation in Social Welfare Programs, unadjusted
| TANF | SNAP | WIC | Child Care subsidy |
Housing assistance |
||
|---|---|---|---|---|---|---|
| Birth | ||||||
| Number of mother-infant dyads | 558 | 560 | 560 | 557 | 560 | |
| Overall participation (%) | 51 | 65 | 69 | 12 | 59 | |
| Health Literacy (N, %) | ||||||
| Inadequate | 19 (33) | 32 (55) | 43 (74) | 7 (12) | 35 (60) | |
| Marginal | 39 (53) | 48 (65) | 51 (69) | 4 (6) | 51 (69) | |
| Adequate | 224 (53) | 286 (67) | 295 (69) | 54 (13) | 242 (57) | |
| P-value1 | 0.017 | 0.22 | 0.72 | 0.22 | 0.13 | |
| 6 month follow-up | ||||||
| Number of mother-infant dyads | 552 | 560 | 560 | 558 | 551 | |
| Overall participation (%) | 56 | 73 | 93 | 29 | 49 | |
| Health Literacy (N, %) | ||||||
| Inadequate | 23 (43) | 37 (64) | 57 (98) | 13 (22) | 30 (53) | |
| Marginal | 46 (63) | 53 (72) | 70 (95) | 25 (34) | 39 (54) | |
| Adequate | 238 (56) | 317 (74) | 395 (93) | 126 (30) | 200 (47) | |
| P-value1 | 0.069 | 0.25 | 0.21 | 0.33 | 0.47 | |
| 12 month follow-up | ||||||
| Number of mother-infant dyads | 476 | 478 | 477 | 475 | 475 | |
| Overall participation (%) | 47 | 71 | 87 | 37 | 48 | |
| Health Literacy (N, %) | ||||||
| Inadequate | 25 (43) | 42 (78) | 48 (89) | 14 (26) | 25 (46) | |
| Marginal | 36 (57) | 45 (71) | 56 (89) | 22 (35) | 36 (59) | |
| Adequate | 164 (46) | 254 (70) | 313 (87) | 141 (39) | 165 (46) | |
| P-value1 | 0.24 | 0.53 | 0.86 | 0.19 | 0.16 | |
| 18 month follow-up | ||||||
| Number of mother-infant dyads | 393 | 395 | 396 | 395 | 394 | |
| Overall participation (%) | 38 | 68 | 65 | 39 | 46 | |
| Health Literacy (N, %) | ||||||
| Inadequate | 17 (39) | 32 (73) | 29 (66) | 11 (25) | 24 (55) | |
| Marginal | 25 (45) | 38 (69) | 46 (84) | 22 (40) | 27 (49) | |
| Adequate | 106 (36) | 200 (68) | 183 (62) | 122 (41) | 130 (44) | |
| P-value1 | 0.41 | 0.78 | 0.007 | 0.12 | 0.38 | |
| 24 month follow-up | ||||||
| Number of mother-infant dyads | 416 | 418 | 415 | 417 | 414 | |
| Overall participation (%) | 37 | 69 | 53 | 36 | 37 | |
| Health Literacy (N, %) | ||||||
| Inadequate | 20 (43) | 30 (65) | 24 (52) | 10 (22) | 24 (53) | |
| Marginal | 28 (47) | 44 (75) | 39 (67) | 18 (31) | 29 (50) | |
| Adequate | 105 (34) | 214 (68) | 155 (50) | 123 (39) | 102 (33) | |
| P-value1 | 0.082 | 0.54 | 0.051 | 0.041 | 0.003 | |
P-value for the χ2 test of association between maternal health literacy and participation in social welfare programs. P < 0.01 is used as threshold for significance, as denoted in bold.
Table 2 also presents the participation rates in each program by health literacy group over time. In this study inclusive of mothers receiving SSI and using a conservative approach for the significance threshold (i.e. Bonferroni correction for five programs, p<0.01), none of the program participation rates at birth, 6 months, and 12 months follow-ups were significantly different between mothers at different levels of health literacy. Although there are two statistically significant results in this table (WIC at 18 months and housing subsidy at 24 months), no pattern that was either consistent within a specific program across time or associated with most programs at a particular time point was found.
Results from multivariable analyses
The results of our multivariable analysis from birth through 24 months of age using GEE models are presented in Table 3. The table displays results for the final model for each program produced by the best variable subsets model fitting approach. In these adjusted models, children with mothers who had inadequate health literacy were less likely to receive child care subsidy (OR=0.54, 95% CI 0.34–0.85, p = 0.008) than children with mothers who had adequate health literacy. Health literacy was not a significant predictor for TANF, SNAP, WIC, or housing assistance participation. To further explore why mothers with inadequate health literacy were less likely to receive a child care subsidy than those mothers with adequate health literacy during the first 24 months of life, we examined employment status (collapsed to three categories: student, employed, and unemployed) across health literacy levels and found that unemployment rate was not significantly associated with maternal health literacy levels (Appendix E).
Table 3.
The influence of maternal health literacy on public program participation from birth through 24 months, adjusted
| TANF | SNAP | WIC | Child Care subsidy | Housing assistance | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| QIC: 2371.10 | QIC: 1904.94 | QIC: 2077.18 | QIC: 2505.29 | QIC: 1616.97 | |||||||
| Number of dyads: 557 | Number of dyads: 551 | Number of dyads: 556 | Number of dyads: 559 | Number of dyads: 559 | |||||||
| Variable | Adjusted Odds Ratio (95% CI) |
P-value | Adjusted Odds Ratio (95% CI) |
P-value | Adjusted Odds Ratio (95% CI) |
P-value | Adjusted Odds Ratio (95% CI) |
P-value | Adjusted Odds Ratio (95% CI) |
P-value | |
| Maternal Health Literacy | |||||||||||
| Inadequate | 0.59 (0.38 –0.93) | 0.022 | 0.70 (0.44–1.12) | 0.135 | 1.10 (0.72–1.68) | 0.659 | 0.54 (0.34–0.85) | 0.008 | 0.71 (0.38–1.33) | 0.283 | |
| Marginal | 1.04 (0.69–1.57) | 0.839 | 1.02 (0.67–1.54) | 0.935 | 1.54 (0.98–2.42) | 0.058 | 0.82 (0.56–1.19) | 0.287 | 1.01 (0.60–1.72) | 0.960 | |
| Adequate | Reference | -- | -- | -- | -- | -- | Reference | -- | -- | -- | |
| Child’s age1 | |||||||||||
| Age (months) | 0.97 (0.96–0.98) | <0.0001 | 1.00 (0.99–1.01) | 0.621 | 0.96 (0.95–0.97) | <0.0001 | 1.07 (1.05–1.08) | <0.0001 | 0.985 (0.973–0.997) | 0.013 | |
| Age squared (centered, months sq) | 0.999 (0.998–1.000) | 0.031 | 0.998 (0.996–1.000) | 0.009 | 0.991 (0.990–0.992) | <0.0001 | 0.994 (0.993–0.996) | <0.0001 | 1.000 (0.998–1.001) | 0.548 | |
| Employment2 | |||||||||||
| In school | 2.99 (2.23–4.01) | <0.0001 | 1.20 (0.88–1.64) | 0.252 | 1.55 (1.11–2.17) | 0.011 | 1.25 (0.94–1.66) | 0.118 | 1.17 (0.83–1.64) | 0.381 | |
| Employed, part time | 1.62 (1.19–2.21) | 0.002 | 1.11 (0.79–1.54) | 0.552 | 1.71 (1.23–2.38) | 0.001 | 0.98 (0.74–1.30) | 0.906 | 1.29 (0.88–1.87) | 0.188 | |
| Unemployed, looking for employment | 3.40 (2.59–4.46) | <0.0001 | 1.49 (1.07–2.08) | 0.019 | 1.48 (1.10–2.00) | 0.010 | 0.47 (0.35–0.62) | <0.0001 | 1.22 (0.89–1.67) | 0.225 | |
| Unemployed, not looking for employment | 2.87 (2.12–3.89) | <0.0001 | 1.29 (0.86–1.93) | 0.212 | 1.91 (1.29–2.82) | 0.001 | 0.28 (0.18–0.44) | <0.0001 | 1.60 (1.08–2.37) | 0.020 | |
| Employed, full time | Reference | -- | -- | -- | Reference | -- | Reference | -- | -- | -- | |
| Marital status | |||||||||||
| Married/widowed/divorced | 0.44 (0.27–0.71) | 0.001 | 0.37 (0.23–0.59) | <0.0001 | -- | -- | 0.46 (0.28–0.75) | 0.002 | -- | -- | |
| Single | Reference | -- | Reference | -- | -- | -- | Reference | -- | -- | -- | |
| Number of children1,2 | |||||||||||
| 1.30 (1.17–1.45) | <0.0001 | 1.83 (1.59–2.11) | <0.0001 | 0.92 (0.83–1.01) | 0.079 | -- | -- | 1.14 (1.00–1.29) | 0.043 | ||
| Income2 | |||||||||||
| Dollars per month | 0.9995 (.9993–.9997) | <0.0001 | 0.9994 (.9992–.9995) | <0.0001 | -- | -- | -- | -- | -- | -- | |
| Supplemental Security Income2 | |||||||||||
| Yes | -- | -- | 1.78 (1.19–2.66) | 0.005 | -- | -- | 1.61 (1.01–2.56) | 0.045 | -- | -- | |
| No | -- | -- | Reference | -- | -- | -- | Reference | -- | -- | -- | |
| Housing situation2 | |||||||||||
| Other living situation | -- | -- | 0.72 (0.57–0.91) | 0.006 | 1.49 (1.16–1.91) | 0.002 | -- | -- | 0.56 (0.42–0.76) | 0.0002 | |
| Living alone | -- | -- | Reference | -- | Reference | -- | -- | -- | Reference | -- | |
| Race | |||||||||||
| Non-African-American | -- | -- | 0.61 (0.42–0.89) | 0.011 | -- | -- | 0.61 (0.42–0.88) | 0.008 | -- | -- | |
| African-American | -- | -- | Reference | -- | -- | -- | Reference | -- | -- | -- | |
| Education | |||||||||||
| Less than High School | 1.97 (1.42–2.73) | <0.0001 | -- | -- | -- | -- | -- | -- | -- | -- | |
| High School degree | 1.75 (1.25–2.47) | 0.001 | -- | -- | -- | -- | -- | -- | -- | -- | |
| More than High School | Reference | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
Note: Bold denotes p-value < 0.01. Only results from final models obtained from best subsets approach (the lowest quasi-likelihood information criterion [QIC] statistic) are presented in this table.
Child’s age, income, and number of children were analyzed as continuous variables. Child’s age was centered at the child turning one year old. For each income category, the lower endpoint of the category was used.
Employment, housing situation, income, number of children, and Supplemental Security Income (SSI) were included as time varying covariates in the models.
Child’s age was significantly associated with participation in four of the five programs examined. For each one month increase in the child’s age, mothers were significantly less likely to be enrolled in TANF (OR=0.97, 95% CI 0.96–0.98) and WIC (OR=0.96, 95% CI 0.95–0.97). For SNAP, a one month increase in the child’s age resulted in a steeper decrease in odds of participation than for TANF or WIC because only the squared age term demonstrated statistical significance. In contrast, for each one month increase in the child’s age, mothers were significantly more likely to be enrolled in child care subsidy (OR=1.07, 95% CI 1.05–1.08).
In this study, mother’s employment status was strongly associated with TANF and child care subsidy receipt. As expected, compared to mothers employed full time, children whose mothers were in school, employed part time or unemployed were more likely to receive TANF. Similarly, unemployed mothers, whether looking for employment or not, were significantly less likely have children in subsidized child care than mothers employed full time. Other factors related to family structure (i.e., marital status, number of children) and socioeconomic status (i.e. housing situation, monthly income, SSI receipt) were not consistently related to participation across the five public benefit programs. Child care subsidy was the only program where race was significantly associated with participation in this predominantly African-American cohort. Similar to previously published results among infants through age 6 months, mothers with less than high school education were nearly twice as likely to receive TANF as those mothers with more than a high school education.
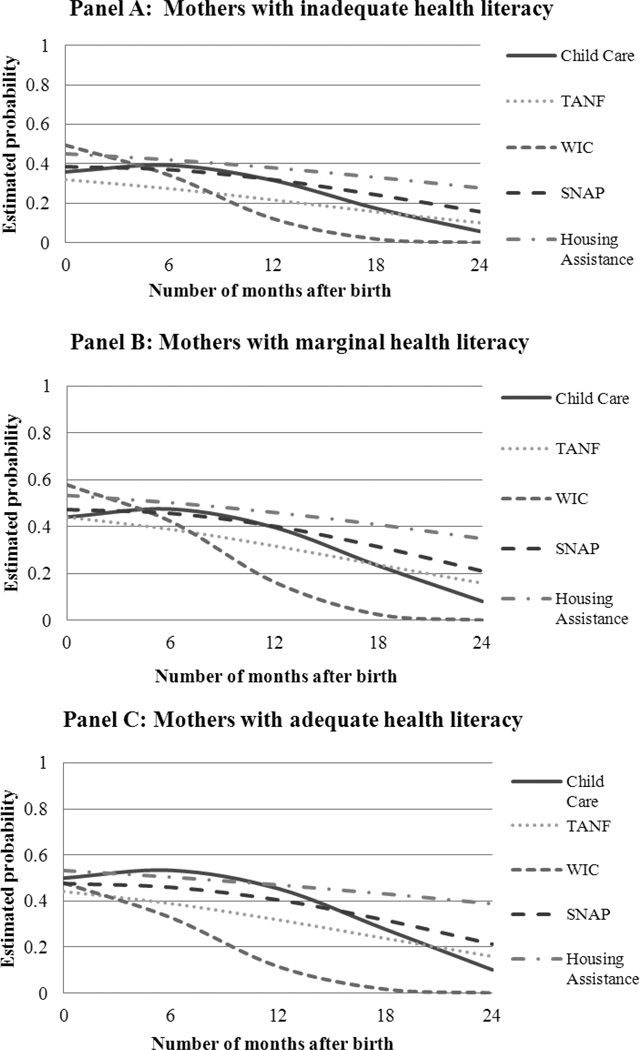
Estimated probability of program participation during the first 24 months
In order to illustrate the relationship between child’s age and program participation, we created graphs of the estimated probability of program participation by child’s age (in months after birth) and by health literacy levels (Figure 1). Consistent with results in Table 3, the participation rates for TANF, SNAP, and housing assistance declined steadily as the child aged. The WIC participation rates also declined but the drop was much steeper than the other programs, and reached zero by 24 months of age. Child care subsidy participation increased slightly at 6 months, and then declined to fairly low levels by age 24 months. Notably, consistent with results presented in Table 3, child care subsidy is the only program where there are visible differences in program participation between mothers with different health literacy levels; specifically, children whose mothers had inadequate health literacy were less likely to participate in child care subsidy than those children whose mothers had adequate health literacy.
Figure 1. Estimated probability for participation in public programs by maternal health literacy.
Note: The graph presents estimated program participation based on the best fitting GEE model for single, African-American mothers with one child who are employed full time with $1000 monthly income, have more than high school education, are living alone, and do not receive SSI.
Discussion
In this study following mother-infant dyads for the first 24 months of life, maternal health literacy is significantly associated with participation in the subsidized child care program but not in TANF, SNAP, WIC or housing assistance. On the other hand, as the infant’s age increased, mothers were more likely to participate in child care subsidy while less likely to participate in TANF, WIC and housing assistance. These findings are consistent with our hypothesis that the influence of maternal health literacy wanes after the initial enrollment in social welfare programs and the needs of low-income families change as the child grows older.
Across the nation, only one-third or fewer of eligible families use child care subsidies (31). Previous studies on child care subsidy use found that lack of a childcare subsidy is a significant barrier to work (32–34). As discussed in the results, our finding that mothers with inadequate health literacy are less likely to receive child care subsidy than those mothers with adequate health literacy cannot be explained by differences in unemployment rates and consequent need (or lack thereof) for child care. On the other hand, these results do support the notion that social welfare programs with complex application process have lower enrollment rates, especially among low literacy populations because the child care subsidy application process in Philadelphia is one of the most difficult. In Philadelphia, non-TANF families apply for child care subsidies in a separate office from TANF families, must provide proof of work in-person, and complete an interview (35). As reported by others, the hassle and restriction of the application process is a major barrier for parents applying for child care subsidies (35). Policies to simplify this application process, especially for low literacy populations, may assist families in realizing economic security.
The changing estimated probability for participation for each program further suggests that family needs change as the child grows older, thus the need for the social programs vary over time. In addition, income eligibility thresholds for TANF, WIC, SNAP, and housing assistance generally become more stringent as children age. Therefore, families’ perceptions about potential benefits and burdens of applying for various types of assistance are likely contributors to differences in program participation. Whereas prior findings showed that mothers with inadequate health literacy were less likely to receive TANF at child’s birth and at six months than mothers with marginal and adequate health literacy (15), we did not find that this association persists through the first 24 months of life. Specific to TANF, federal guidelines dictate that families receive proportionately less TANF money as family income increases. In addition, TANF has a cumulative lifetime limit on assistance receipt (36). Therefore, most families exit TANF as soon as employable adults in the household are able to find work (37). One possible explanation for our finding that WIC participation rate was the highest at birth is that opportunities for enrollment occur prenatally and in the hospital during the immediate post-partum period whereas opportunities for other programs enrollment do not. Subsequently, WIC participation may drop substantially after birth because, once infant formula is no longer needed, families decide that the ongoing burdens of WIC documentation requirements (e.g., in-person appointments, laboratory tests for hemoglobin/hematocrit) outweigh the benefits of receiving food packages.
There are some caveats to this study. First, health literacy is a complex concept and none of the currently available health literacy measures fully assesses a person’s ability to obtain, process, and understand health information (38). Our study only used S-TOFHLA because of its high reliability and ease of administration. Solely relying on this instrument may be problematic in that the S-TOFHLA is not meant to be a comprehensive assessment of an individual's capacities; rather, this tool measures selected domains that are thought to be markers for an individual's overall capacity (39). A review of 19 health literacy indices, however, demonstrated that the TOFHLA (and the REALM-S) demonstrated the strongest psychometric properties of all the instruments examined (38), making it an appropriate choice for our study. Second, the study population was primarily African-American recruited from an urban setting thus generalizable mostly to this population. Specifically, we did not have enough limited English proficiency families in our sample to explore social welfare program participation in a non-English proficient group. Third, eligibility criteria and application processes vary for each social welfare program; in this secondary data analysis, we did not have the information to verify income, household size, or citizenship to determine each mother-infant dyad’s eligibility for different social welfare programs. However, the focus of our study is to determine how low-income families utilize social welfare programs, thus using Medicaid eligibility as a proxy for selecting low-income families who are potentially eligible for these social welfare programs is a reasonable approach that has been used by others (40, 41). Fourth, self-reported data about social welfare program participation are subject to recall bias and other work has shown that recall bias would most likely result in underestimation of true participation rates (42). Lastly, there may be selection bias as only 53% of eligible mothers agreed to participate in the parent study. However, the participants and non-participants had only minor differences in race/ethnicity and employment status such that the main findings are unlikely to be affected by this bias.
In summary, we found that mothers with inadequate health literacy were less likely to receive child care subsidy than those mothers with adequate health literacy during the first 24 months. Mothers with poor health literacy could benefit from simplified or facilitated child care subsidy application processes. In addition, our findings suggest that a family’s need for assistance from different social welfare programs changes over the first two years of the child’s life. Consequently, the application processes for these social welfare programs should be simplified to facilitate enrollment among needy families when they need assistance the most.
Acknowledgement
We thank Kathy Fisher, Director, Family Economics Security, Public Citizens for Children and Youth for sharing her perspective about public program enrollment and renewal policies.
Abbreviations
- TANF
Temporary Assistance to Needy Families
- WIC
Women, Infant, Children program
- SSI
supplemental security income
- S-TOFHLA
short form Test of Functional Health Literacy in Adults
Appendix A. Study enrollment protocol
Appendix B. Population Characteristics for Participants and Non-participants
| Participant (N=744) |
Non- Participant (N=637) |
P- value2 |
||
|---|---|---|---|---|
| Race, n (%) | <.0001 | |||
| Black | 604 (81) | 566 (89) | ||
| Other | 140 (19) | 71 (11) | ||
| Education, n (%) | 0.20 | |||
| Less than high school | 243 (33) | 182 (29) | ||
| High school | 182 (24) | 176 (28) | ||
| More than high school | 319 (43) | 279 (44) | ||
| Employment, n (%) | 0.02 | |||
| Student | 233 (31) | 164 (26) | ||
| Employed | 224 (30) | 219 (34) | ||
| Unemployed (looking for work) | 78 (10) | 48 (8) | ||
| Unemployed (not looking for work) | 84 (11) | 73 (11) | ||
| Missing | 125 (17) | 133 (21) | ||
| Maternal Age (years old), n (%) | 0.24 | |||
| > 20 | 184 (25) | 152 (24) | ||
| 20 – 24 | 300 (40) | 234 (37) | ||
| 25 – 29 | 159 (21) | 158 (25) | ||
| 30 – 34 | 72 (10) | 57 (9) | ||
| > 34 | 29 (4) | 36 (6) | ||
| Country, n (%)1 | 0.20 | |||
| US born | 685 (92) | 554 (90) | ||
| Non-US born | 59 (8) | 61 (10) | ||
| Baby Weight (g), mean (IQR) | 3282 (2970 – 3553) | 3289 (2950 – 3590) | 0.06 | |
| Maternal Age (years old), mean (IQR) | 23 (20 – 26) | 24 (20 – 27) | 0.08 | |
22 subjects missing data for this variable.
P-value determined using chi square test.
Appendix C: Population characteristics for analytic sample vs. subjects with incomplete data
| No Six Month or Health Literacy Data (N=184) |
Analytic Sample (N=560) |
P- value1 |
||
|---|---|---|---|---|
| Race, n (%) | 0.04 | |||
| Black | 140 (76) | 464 (83) | ||
| Other | 44 (24) | 94 (17) | ||
| Education, n (%) | 0.03 | |||
| Less than high school | 72 (39) | 171 (31) | ||
| High school | 47 (26) | 135 (24) | ||
| More than high school | 65 (35) | 254 (45) | ||
| Employment, n (%) | 0.89 | |||
| Student | 46 (28) | 233 (31) | ||
| Employed | 50 (31) | 224 (30) | ||
| Unemployed (looking for work) | 20 (12) | 78 (11) | ||
| Unemployed (no looking for work) | 21 (13) | 84 (11) | ||
| Missing | 27 (16) | 125 (17) | ||
| Maternal Age (years old), n (%)1 | 0.49 | |||
| < 20 | 40 (22) | 145(26) | ||
| 20 – 24 | 72 (39) | 227 (41) | ||
| 25 – 29 | 42 (23) | 117 (21) | ||
| 30 – 34 | 19 (10) | 51 (9) | ||
| > 34 | 11 (6) | 20 (4) | ||
| Maternal Health Literacy, n (%)2 | 0.06 | |||
| Inadequate/Marginal | 26 (17) | 132 (24) | ||
| Adequate | 130 (83) | 428 (76) | ||
| Country, n (%)3 | 0.01 | |||
| US born | 162 (88) | 523 (93) | ||
| Non-US born | 22 (12) | 37 (7) | ||
| Baby Weight (g), mean (IQR) | 3265.5 (2950– 3550) | 3287.7 (2972.5 – 3552.5) | 0.50 | |
| Maternal Age (years old), mean (IQR) | 24 (20 – 27) | 23.31 (19 – 26) | 0.15 | |
Note: Numbers do not add to 100% due to rounding
P-value determined for the chi-square test.
Only 716 from the enrolled category completed the S-TOFHLA.
There are 22 with missing data for this item.
Appendix D: Selected portions of the follow-up survey
HEALTH CARE ACCESS: MATERNAL, CHILD AND POLICY FACTORS
Section 4: Maternal Demographic Information
- What is your marital status?
- Single
- Married
- Widowed
- Don’t know
- No response
- What is your current living situation?
- Living in own housing
- Living with relatives or friends
- Living in a shelter
- Other (specify)
- Don’t know
- No response
-
How many other people (like family or friends) are currently living with you or staying in your home?
_____ people
-
How many other children do you have?
____ children
-
How many of them are living with you?
____ children
- What is your current employment status?
- Working full-time
- Working part-time
- Unemployed, looking for work
- Unemployed, not looking for work
- Student
- DK
- NR
- What is your current monthly household income:
- Under $250 per month (under $3,000 per year)
- $251–$500 per month ($3,012–$6,000 per year)
- $501–$999 per month ($6,012–$11,988 per year)
- $1,000–$1,499 per month ($12,000–$17,988 per year)
- $1,500–$1,999 per month ($18,000–$23,988 per year)
- $2,000–$2,499 per month ($24,000–$29,988 per year)
- $2,500–$2,999 per month ($30,000–$35,988 per year)
- $3,000 or above per month ($36,000 or above per year)
- DK
- NR
Section 7: Family TANF Status and Other Benefits
- Are there any other benefits that you or your family receive?*
- Medical assistance Yes No
- Cash assistance Yes No
- Child care benefits Yes No
- WIC Yes No
- Housing benefits Yes No
- SSI Yes No
- Have you ever enrolled a child in medical assistance/Medicaid?
- Yes
- No
- DK
- NR
- Has anyone you know, like a friend or family member, had experience registering a child for medical assistance?
- Yes (specify person)
- No
- DK
- NR
- How many of your children are enrolled in medical assistance?
- All of them
- Some of them
- One of them
- None
- DK
- NR
* When the survey was administered in person with a laptop, a pop-up window with an explanation of the program will appear for this question as below. When the survey was administered over the phone, the research assistants explained the programs to the mother if they don’t know what that program is.
Medical assistance (Medicaid)
Medical assistance in Pennsylvania provides payment for health care services on behalf of eligible people. Payments are made directly to the health care providers.
Cash Assistance
Pennsylvania offers cash assistance to any person or family, based on rules and standards established by the Department of Public Welfare. There are two major categories of cash assistance. They are:
Temporary Assistance for Needy Families (TANF): provides money for children and their parents or other relatives with whom they live, and for pregnant women.
General Assistance (GA): provides money for persons who do not meet the requirements for TANF. Most GA recipients are individuals or couples with no children, who have temporary or permanent disabilities that prevent their employment.
Food Stamps
Food stamp benefits are used to buy food and help eligible households obtain more nutritious diets.
WIC
WIC provides nutritious foods, nutrition counseling, and referrals to health and other social services to participants at no charge. WIC serves eligible women, infants and children up to age 5.
Child Care benefits
In Pennsylvania, Child Care Works helps eligible families pay for child care.
Housing Assistance
For example, Public Housing, Low-Rent Housing, or Housing Choice Vouchers (formerly called "Section 8").
Public Housing is apartments for eligible people, operated by local housing agencies.
Low-rent housing: The government provides funds directly to apartment owners, who lower the rents they charge tenants.
Housing Choice Vouchers (formerly called “Section 8”) let you find your own place to rent, using the voucher to pay for all or part of the rent.
SSI
Supplemental Security Income (SSI) is a Federal income supplement program funded by general tax revenues (not Social Security taxes).
It is designed to help aged, blind, and disabled people, who have little or no income; and
It provides cash to meet basic needs for food, clothing, and shelter.
Appendix E: Comparison of unemployment rates across health literacy levels by the Marascillo procedure
| Birth | |||
| Expression for Test Statistic | Test-Statistic | Critical Value | Significance |
| |p1-p2| | 0.050 | 0.191 | No |
| |p1-p3| | 0.099 | 0.151 | No |
| |p2-p3| | 0.049 | 0.131 | No |
| 6-month follow-up | |||
| Expression for Test Statistic | Test-Statistic | Critical Value | Significance |
| |p1-p2| | 0.071 | 0.214 | No |
| |p1-p3| | 0.045 | 0.171 | No |
| |p2-p3| | 0.026 | 0.153 | No |
| 12-month follow-up | |||
| Expression for Test Statistic | Test-Statistic | Critical Value | Significance |
| |p1-p2| | 0.021 | 0.203 | No |
| |p1-p3| | 0.008 | 0.163 | No |
| |p2-p3| | 0.012 | 0.144 | No |
| 18-month follow-up | |||
| Expression for Test Statistic | Test-Statistic | Critical Value | Significance |
| |p1-p2| | 0.078 | 0.147 | No |
| |p1-p3| | 0.016 | 0.129 | No |
| |p2-p3| | 0.062 | 0.094 | No |
| 24-month follow-up | |||
| Expression for Test Statistic | Test-Statistic | Critical Value | Significance |
| |p1-p2| | 0.051 | 0.203 | No |
| |p1-p3| | 0.117 | 0.163 | No |
| |p2-p3| | 0.066 | 0.141 | No |
p1: proportion of mothers with inadequate health literacy that are unemployed
p2: proportion of mothers with marginal health literacy that are unemployed
p3: proportion of mothers with adequate health literacy that are unemployed
Footnotes
Financial conflict(s) of interest: None to disclose
Author contributions
S. Pati conceived and led the study and obtained study funding. B. Siewert and R.E. Calixte performed the analyses while A. Cnaan participated in the study design and directed the analyses. A.T. Wong led the writing. S.K. Bhatt assisted with the drafting of the manuscript and interpretation of the analyses. All authors approved the final version of this manuscript.
Contributor Information
Elizabeth Siewert, Email: stats.speaking@gmail.com.
Angie T. Wong, Email: angie.wong@stonybrook.edu.
Suraj K. Bhatt, Email: skbhatt@gwmail.gwu.edu.
Rose E. Calixte, Email: rose.calixte@stonybrook.edu.
Avital Cnaan, Email: ACnaan@childrensnational.org.
References
- 1.Devaney BL, Ellwood MR, Love JM. Programs that mitigate the effects of poverty on children. Future Child. 1997;7(2):88–112. [PubMed] [Google Scholar]
- 2.McKernan S, Ratcliffe C. The Effect of Specific Welfare Policies on Poverty. Washington, DC: The Urban Institute; 2006. [Google Scholar]
- 3.McCartney K, Dearing E, Taylor BA, et al. Quality Child Care Supports the Achievement of Low-Income Children: Direct and Indirect Pathways Through Caregiving and the Home Environment. J. Appl. Dev. Psychol. 2007;28(5–6):411–426. doi: 10.1016/j.appdev.2007.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee BJ, Mackey-Bilaver L. Effects of WIC and Food Stamp Program participation on child outcomes. Children and Youth Services Review. 2007;29(4):501–517. [Google Scholar]
- 5.Haley JM, Kenney GM. Why Aren't More Uninsured Children Enrolled in Medicaid or SCHIP? Washington, D.C: Urban Institute; 2001. Contract No.: B-35. [Google Scholar]
- 6.Wolkwitz K. Trends in Food Stamp Program Participation Rates: 2000 to 2006. Washington, DC: Mathematica Policy Research, Inc; 2008. [Google Scholar]
- 7.Office of the Assistant Secretary for Planning and Evaluation. Indicators of Welfare Dependence, Annual Report to Congress, 2009–2013. Washington, DC: US Department of Health and Human Services; [Google Scholar]
- 8.Sommers BD. The impact of program structure on children's disenrollment from Medicaid and SCHIP. Health Aff. (Millwood) 2005;24(6):1611–1618. doi: 10.1377/hlthaff.24.6.1611. [DOI] [PubMed] [Google Scholar]
- 9.Lake Research Partners, Perry M. Reducing Enrollee Churning in Medicaid, Child Health Plus, and Family Health Plus. Findings from Eight Focus Groups with Recently Disenrolled Individuals. New York, NY: NYS Health Foundation; 2009. Feb, [Google Scholar]
- 10.Pati S, Kavanagh JE, Bhatt SK, et al. Reading level of medicaid renewal applications. Acad. Pediatr. 2012;12(4):297–301. doi: 10.1016/j.acap.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 11.Pati S, Romero D, Chavkin W. Changesin use of health insurance and food assistance programs in medically underserved communities in the era of welfare reform: an urban study. Am. J. Public Health. 2002;92(9):1441–1445. doi: 10.2105/ajph.92.9.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dion MR, Pavetti L. Access to and Participation in Medicaid and the Food Stamp Program: A review of the recent literature. Washington, DC: Mathematica Policy Research, Inc; 2000. [Google Scholar]
- 13.U.S. Department of Health and Human Services. Healthy People 2010. Washington, DC: Office of Disease Prevention and Health Promotion; [Google Scholar]
- 14.Yin HS, Johnson M, Mendelsohn A, et al. The Health Literacy of Parents in the United States: A Nationally Representative Study. Pediatrics. 2009;124:S289–S298. doi: 10.1542/peds.2009-1162E. [DOI] [PubMed] [Google Scholar]
- 15.Pati S, Mohamad Z, Cnaan A, et al. Influence of maternal health literacy on child participation in social welfare programs: the Philadelphia experience. Am. J. Public Health. 2010;100(9):1662–1665. doi: 10.2105/AJPH.2009.172742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pati S, Feemster KA, Mohamad Z, et al. Maternal health literacy and late initiation of immunizations among an inner-city birth cohort. Matern Child Health J. 2011;15(3):386–394. doi: 10.1007/s10995-010-0580-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. National Health Interview Survey. Atlanta, GA: [Accessed December 4 2012]. http://www.cdc.gov/nchs/nhis.htm. [Google Scholar]
- 18.Nurss JR, Parker R, Willams M, et al. TOFHLA: Test of Functional Health Literacy in Adults. Second ed. Snow Camp, NC: Peppercorn Books & Press; 2001. [Google Scholar]
- 19.Parker RM, Baker DW, Williams MV, et al. The test of functional health literacy in adults: a new instrument for measuring patients' literacy skills. J. Gen. Intern. Med. 1995;10(10):537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 20.Office of Child Care. FY 2010 Child Care and Development Fund Data Tables. Washington, D.C: 2013. [Google Scholar]
- 21.Office of Family Assistance. Characteristics and Financial Circumstances of TANF Recipients FY. Washington, D.C: 2010. [Google Scholar]
- 22.Martinez-Schiferl M, Zedlewski S, Giannarelli L. National and State-Level Estimates of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Eligibles and Program Reach, 2010. Alexandria, VA: United States Department of Agriculture Food and Nutrition Service, Office of Research and Analysis; 2013. [Google Scholar]
- 23.Mabli J, Tordella S, Castner L, et al. Dynamics of Supplemental Nutrition Assistance Program Participation in the Mid-2000s. Alexandria, VA: US Department of Agriculture Food and Nutrition Service, Office of Research and Analysis; 2011. [Google Scholar]
- 24.Bethell CD, Kogan MD, Strickland BB, et al. A national and state profile of leading health problems and health care quality for US children: key insurance disparities and across-state variations. Acad. Pediatr. 2011;11(3 Suppl):S22–S33. doi: 10.1016/j.acap.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 25.Kogan MD, Newacheck PW, Blumberg SJ, et al. Underinsurance among children in the United States. N. Engl. J. Med. 2010;363(9):841–851. doi: 10.1056/NEJMsa0909994. [DOI] [PubMed] [Google Scholar]
- 26.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(2):e286–e298. doi: 10.1542/peds.2007-1243. [DOI] [PubMed] [Google Scholar]
- 27.Durfee A, Meyers MK. Who gets what from government? Distributional consequences of child-care assistance policies. Journal of Marriage and Family. 2006;68(3):733–748. [Google Scholar]
- 28.Flores G, Bauchner H, Feinstein AR, et al. The impact of ethnicity, family income, and parental education on children's health and use of health services. Am Journal of Public Health. 1999;89(7):1066–1071. doi: 10.2105/ajph.89.7.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diggle PJ, Heagerty PJ, Liang K, et al. Analysis of longitudinal data. USA: Oxford University Press; 2002. [Google Scholar]
- 30.Maarascuilo LA. Large-sample multiple comparisons. Psychol. Bull. 1966;65:280–290. doi: 10.1037/h0023189. [DOI] [PubMed] [Google Scholar]
- 31.U.S. Government Accountability Office. Child Care: Multiple Factors could have contributed to the Recent Decline in the Number of Children Whose Families Receive Subsidies. Washington, D.C.: 2010. p. 60. [Google Scholar]
- 32.Meyers MK, Heintze T, Wolf DA. Child care subsidies and the employment of welfare recipients. Demography. 2002;39(1):165–179. doi: 10.1353/dem.2002.0008. [DOI] [PubMed] [Google Scholar]
- 33.Danziger SK, Ananat EO, Browning KG. Childcare Subsidies and the Transition from Welfare to Work. Family Relations. 2004;53(2):219–228. [Google Scholar]
- 34.Baum II CL. A Dynamic Analysis of the Effect of Child Care Costs on the Work Decisions of Low-Income Mothers with Infants. Demography. 2002;39(1):139–164. doi: 10.1353/dem.2002.0002. [DOI] [PubMed] [Google Scholar]
- 35.Shlay AB, Weinraub M, Harmon M, et al. Barriers to subsidies: why low-income families do not use child care subsidies. Soc. Sci. Res. 2004;33(1):134–157. [Google Scholar]
- 36.Office of Income Maintenance. [Accessed November 1 2012];Cash Assistance Application. http://services.dpw.state.pa.us/oimpolicymanuals/manuals/bop/ca/104/Table%20of%20Contents.htm#P-1_0.
- 37.Acs G, Loprest PJ. Final Synthesis Report of Findings from ASPE'S 'Leavers' Grants. Washington, D.C.: Urban Institute; 2001. [Google Scholar]
- 38.Jordan JE, Osborne RH, Buchbinder R. Critical appraisal of health literacy indices revealed variable underlying constructs, narrow content and psychometric weaknesses. J. Clin. Epidemiol. 2011;64(4):366–379. doi: 10.1016/j.jclinepi.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 39.Baker DW. The meaning and the measure of health literacy. J. Gen. Intern. Med. 2006;21(8):878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stuber J, Kronebusch K. Stigma and other determinants of participation in TANF and Medicaid. J. Policy Anal. Manage. 2004;23(3):509–530. doi: 10.1002/pam.20024. [DOI] [PubMed] [Google Scholar]
- 41.Bartlett S, Bobronnikov E, Mendelson M. WIC Participation and Program Characteristics 2006. Alexandria, VA: US Department of Agriculture, Food and Nutrition Service, Office of Analysis Nutrition and Evaluation; 2007. [Google Scholar]
- 42.Bollinger CR, David MH. Modeling Food Stamp Participation in the Presence of Reporting Errors. Madison, WI: University of Wisconsin at Madison; 1993. [Google Scholar]