Abstract
Objective
Granulomatous mastitis is a benign disorder which closely mimics malignancy clinico-radiologically. A simple and cost effective modality like fine needle aspiration cytology (FNAC) can help in prompt diagnosis and avoid unnecessary surgery.
Material and Methods
A retrospective study where data were collected for granulomatous lesions of the breast diagnosed by histopathology in a five year period and review of FNAC slides. Cases positive for Mycobacterium tuberculosis either on ZN stain or Polymerase chain reaction (PCR) and fungus were excluded. A total of 8 cases were included in our study for analysis.
Results
All the cases showed the presence of granuloma composed of epithelioid histiocytes against a background of giant cells, polymorphs with absence of necrosis.
Conclusion
Cytological diagnosis of granulomatous mastitis is difficult as it overlaps with other etiologies like tuberculosis which is prevalent in this part of the world. However, with the use of ancillary techniques like PCR and negative microbiological investigations, a definitive diagnosis can be made.
Keywords: Granulomatous mastitis, fine needle aspiration cytology (FNAC)
Özet
Amaç
Granülomatöz mastit klinik ve radyolojik olarak kanseri taklit edebilen iyi huylu bir hastalıktır. Basit ve ucuz bir yöntem olan ince iğne aspirasyon sitolojisi (İİAS) gereksiz cerrahileri önlemede ve kesin tanı koymada etkin bir yoldur.
Gereç ve Yöntemler
Bu retrospektif çalışma dataları 5 yıllık süre ile histopatolojik olarak granulomatöz lezyon tanısı konan hastaların İİAS lamları ve kayıtları gözden geçirelerek toplanmıştır. ZN boyama veya PCR ile tanısı konmuş olan tüberküloz vakaları ve mantar enfeksiyonu olanlar çalışmaya alınmamıştır. toplam çalışmaya uygun 8 vaka incelenmiştir.
Bulgular
Tüm olgular epiteloid histiositler ve tabanda dev hücreler ve nekrozsuz polimorfmlar göstermiştir.
Sonuç
Granulomatoz mastitin sitolojik tanısı özellikle dünyanın bu bölgesinde olduğu gibi yaygın görülen tüberküloz varlığında oldukça zor konulur. Ancak PCR ve negatif mikrobiolojik araştırmalar sayesinde ayırıcı tanıya kolayca gidilir.
Introduction
Idiopathic granulomatous mastitis is a rare benign breast disease, first described by Kessler and Wallooch (1) in 1972. In the literature, only a few large series have been reported, emphasizing the histological (2–5), imaging (6–8) and cytological (9–11) aspects, with series sizes ranging from 6–16 cases. The histological features of granulomatous mastitis have been well described as consisting of non-caseating granulomas within the breast parenchyma and lobulitis with or without neutrophilic micro abscesses (12, 13). However, cytological features have not been widely discussed.
The clinical and radiological presentation mimics carcinoma, often resulting in unnecessary radical surgery. Therefore, in our study we present eight cases of granulomatous mastitis with special emphasis on their cytological features.
With the increasing use of fine needle aspiration and cytology (FNAC) as the initial investigation for breast lesions, there is a need for an increased awareness of this disease entity so that prompt and correct line of management can be selected.
Material and Methods
The histopathology records of a tertiary care hospital were collected for cases of granulomatous lesion reported between July 2004 and July 2009. The histopathology slides and all the case histories of these patients were retrieved and re-analyzed. A total of 19 cases of granulomatous lesions of breast were diagnosed on histopathology during this period. Of these, FNAC slides of 14 patients could be retrieved. Among the latter, acid fast bacilli (AFB) were detected in Ziehl Neelsen (ZN) stained smear in one case only in which a straightforward diagnosis of tuberculosis of breast was made. In the remaining 13 cases, Polymerase chain reaction (PCR) was performed for the IS6110 sequence of mycobacterium tuberculosis either on material obtained on cytology or from paraffin-wax embedded material. PCR gave positive results in 5 cases and negative in the 8 cases. These PCR-negative cases gave negative results on Periodic Acid Schiff (PAS) and Grocott’s Methanamine Silver staining and culture in Lowenstein-Jensen (LJ) media. These cases are included in our report of Idiopathic Granulomatous Mastitis.
(The FNAC were performed by trained and experienced pathologists using 10ml syringes fitted to a FNAC gun and using 22 to 23 gauge needles. The aspirated material was used to make direct smears for May Grunwald Giemsa (MGG) stain and alcohol-fixed smears for Haematoxylin and Eosin stain and/or Papanicolaou stains.
In all the cases, the following cytological parameters were evaluated
Presence or absence of granulomas
Relative proportions of other cells like epithelioid histiocytes, lymphocytes, plasma cells and polymorphs.
Presence or absence of background necrosis
Multinucleated giant cells- proportion and morphology
Ductal cells- normal or atypical.
All the histopathological slides were reviewed and the diagnosis confirmed.
Results
All the patients were women and the mean age was 34.8 years. In 6 cases, the lesion was located on the left side and in the other 2 on the right (Table 1). At least 4 smears were prepared from each case and were stained with H& E and/or Papanicolaou stain, MGG, PAS and Grocott’s Methanamine Silver stains.
Table 1.
Clinicopathological profile of patients included in the study
| Case Number | Age | Sex | Clinical Features | Radiology | FNAC diagnosis | Histopathological diagnosis |
|---|---|---|---|---|---|---|
| 1 | 30 | F | Lump in left upper outer quadrant breast with axillary lymphadenopathy | Mass with angulated and spiculated margins surrounded by echogenic fibrous tissue ? Carcinoma | Granulomatous Mastitis | Idiopathic Granulomatous Mastitis |
| 2 | 28 | F | Lump in right upper inner quadrant breast | Not Done | Granulomatous Mastitis | Idiopathic Granulomatous Mastitis |
| 3 | 25 | F | Lump in left breast involving three-fourth of breast with sinus formation and few enlarged axillary lymph nodes | Increased soft tissue thickening and edema with multiple focal heterogenous area. ? Inflammatory | Granulomatous Mastitis | Idiopathic Granulomatous Mastitis |
| 4 | 61 | F | Right breast lump and nipple discharge | Not Done | Granulomatous Mastitis | Idiopathic Granulomatous Mastitis |
| 5 | 35 | F | Left breast lump | Not Done | Granulomatous Mastitis | Idiopathic Granulomatous Mastitis |
| 6 | 36 | F | Pain and ill defined lump in right breast | Benign breast disease | Granulomatous Mastitis | Idiopathic Granulomatous Mastitis |
| 7 | 32 | F | Lump in left breast with sinus formation | heterogeneous, with a thin rim of subcapsular radiolucent fat | Granulomatous Mastitis | Idiopathic Granulomatous Mastitis |
| 8 | 32 | F | Lump in left breast | spiculated margins with separate anterior focal asymmetry ? Carcinoma | Granulomatous Mastitis | Idiopathic Granulomatous Mastitis |
All the 8 cases showed the presence of granulomas and giant cells in the smears (Fig. 1). The granulomas (Fig. 2) were composed of epithelioid histiocytes with abundant cytoplasm, oval to reniform nuclei, dispersed chromatin and conspicuous nucleoli. Background of all the smears showed epithelioid histiocytes with morphology similar to those seen constituting the granulomas. Polymorphs accounted for most of the inflammatory cells in all the cases. Three cases showed lymphocytes, while plasma cells were present in only one case. Caseous necrosis was absent in all the cases. The giant cells were both foreign body type and Langhan’s type morphologically.
Figure 1.
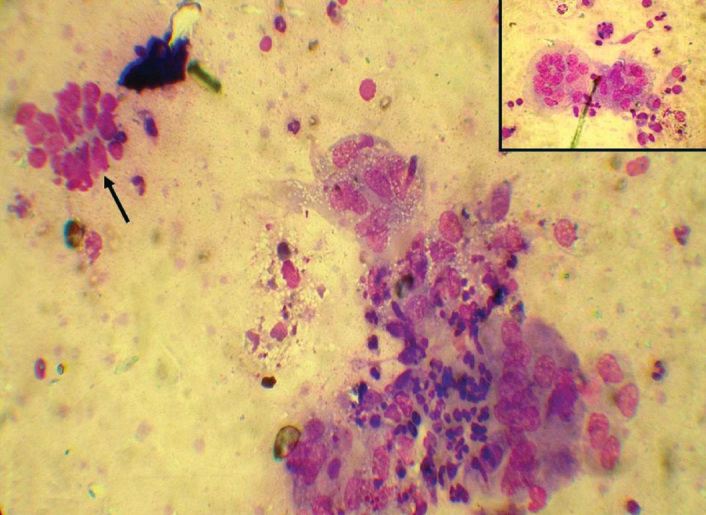
Collection of histiocytes, arrow (↑) showing benign ductal epithelial cells, inset showing giant cells. MGG, × 40
Figure 2.
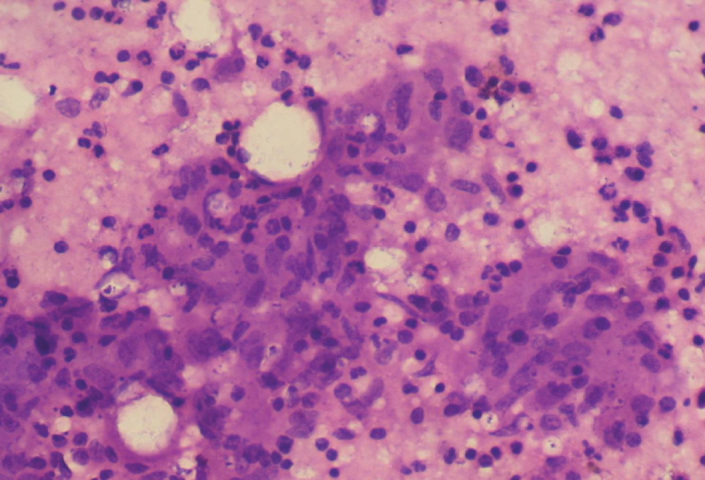
Granuloma comprising of epithelioid histiocytes with polymorphs in the background. H&E, × 40
All the slides were negative for fungus on PAS stain and Grocott’s Methanamine Silver stain. Culture did not yield any growth in any of the 8 cases. For all the cases, ZN stain staining for acid fast bacilli was non-contributory and Mycobacterium Tuberculosis DNA was not detected by PCR in the specimens (Fig. 3).
Figure 3.
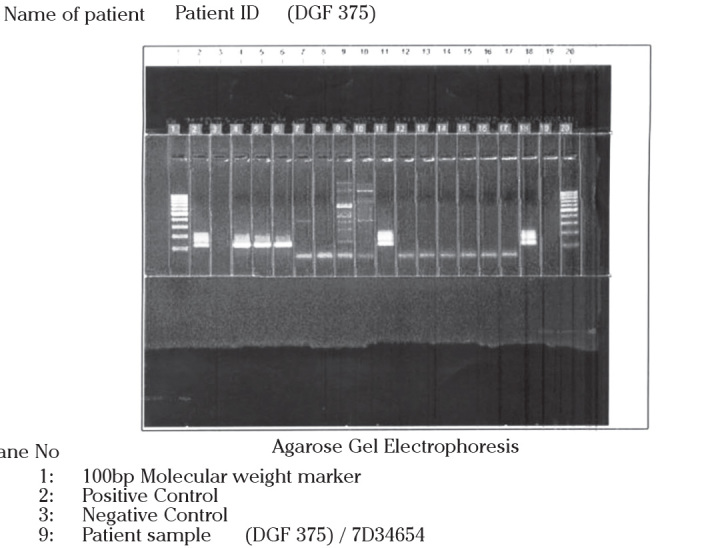
Photograph of agarose gel electrophoresis showing negative result for the sequence of Mycobacterium tuberculosis
Histological review of all the cases confirmed the diagnosis of granulomatous mastitis (Fig. 4).
Figure 4.
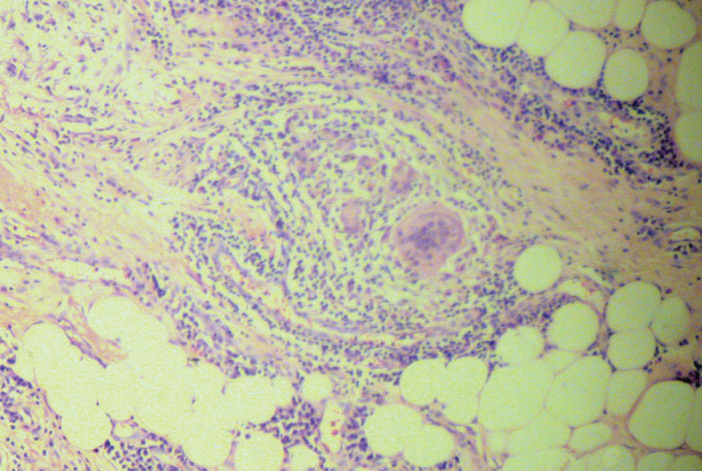
Histopathology section showing granuloma, giant cells & polymorphs involving breast lobule. H&E, × 40
Discussion
Granulomatous mastitis is an uncommon breast lesion that is well known for its worrisome clinical presentation, particularly in younger women (14). In our study, however, one patient was aged 61 years. Clinically and radiologically, granulomatous mastitis is difficult to distinguish from breast carcinoma (14). In our study, the radiological diagnoses of cases 1 and 7 were that of breast carcinoma and both patients had to undergo unnecessary mastectomy. This could have been avoided by performing core biopsy before mastectomy (15).
The etiology of idiopathic granulomatous mastitis is still unknown. Kessler and Wallooch proposed an autoimmune pathogenesis (1). In a recently reported case, immunohistochemical staining showed that the lesion contained predominantly stromal T lymphocytes (16). However, there has been no evidence of systemic immune abnormalities such as the formation of autoantibodies or antigen-antibody complexes.
Among the only three large series describing the FNAC features of granulomatous mastitis in the literature, the usefulness of FNAC in granulomatous mastitis has been debated, with some authors confirming the useful role of FNAC (10, 11), whereas others have concluded that the various causes of granulomatous inflammation cannot be confidently differentiated by FNAC (9).
The presence of epithelioid histiocytes appears to be a common feature, having been reported in all cases of granulomatous mastitis in the literature (9–11, 14, 16, 17). In our study, all the cases showed epithelioid histiocytes whether single or in the form of granulomas.
The number of single epithelioid histiocytes was directly proportional to the number of granulomas in the smears. Our series showed the predominance of neutrophils over lymphocytes, similar to that of another study of nine cases, which demonstrated moderate to abundant numbers of neutrophils in the FNAC preparation. Most other reports have described a mixed inflammatory cell infiltrate. Another characteristic feature was the absence of caseous necrosis, which favors a diagnosis of granulomatous mastitis over an infective cause of granulomatous inflammation.
The single most important differential diagnosis of granulomatous mastitis in our part of the world is tuberculosis. The predominant presence of neutrophils in the background and the lack of caseous necrosis favor a diagnosis of granulomatous mastitis rather than tuberculosis (14). Granulomatous mastitis should also be distinguished from other chronic inflammatory breast diseases such as mammary duct ectasia, Wegener’s granulomatosis, sarcoidosis and histoplasmosis (17). A diagnosis of granulomatous mastitis should also be considered when high numbers of epithelioid histiocytes are seen in smears, even in the absence of granulomas.
Footnotes
Conflict of interest
None declared.
References
- 1.Kessler E, Wallooch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol. 1972;58:642–6. doi: 10.1093/ajcp/58.6.642. [DOI] [PubMed] [Google Scholar]
- 2.Fletcher A, Magrath IM, Riddell RH, Talbot IC. Granulomatous mastitis : a report of seven cases. J Clin Pathol. 1982;35:941–5. doi: 10.1136/jcp.35.9.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Going JJ, Anderson TJ, Wilkinson S, Chetty U. Granulomatous lobular mastitis. J Clin Pathol. 1987;40:535–40. doi: 10.1136/jcp.40.5.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galea MH, Robertson JF, Ellis IO, Elston CW, Blamey RW. Granulomatous lobular mastitis. Aust N Z J Surg. 1989;59:547–50. doi: 10.1111/j.1445-2197.1989.tb01629.x. [DOI] [PubMed] [Google Scholar]
- 5.Bhaskaran CS, Prasad KR, Rao G, Kameshwari R, Saheb DA, Aruna CA. Chronic granulomatous mastitis:review of 26 cases with special reference to chronic lobular mastitis. Indian J Pathol Microbiol. 1992;35:38–43. [PubMed] [Google Scholar]
- 6.Engin G, Acunas G, Acunas B. Granulomatous mastitis: gray scale and color Doppler sonographic findings. J Clin Ultrasound. 1999;27:101–6. doi: 10.1002/(sici)1097-0096(199903/04)27:3<101::aid-jcu1>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 7.Han BK, Choe YH, Park JM, Moon WK, Ko YH, Yang JH, et al. Granulomatous mastitis : mammographic and sonographic appearances. Am J Roentgenol. 1999;173:317–20. doi: 10.2214/ajr.173.2.10430126. [DOI] [PubMed] [Google Scholar]
- 8.Yilmaz E, Lebe B, Usal C, Balci P. Mammographic and sonographic findings in the diagnosis of idiopathic granulomatous mastitis. Eur Radiol. 2001;11:2236–40. doi: 10.1007/s003300100965. [DOI] [PubMed] [Google Scholar]
- 9.Martinez-Parra D, Nevado-Santos M, Melendez-Guerrero B, García-Solano J, Hierro-Guilmain CC, Pérez-Guillermo M. Utility of fine-needle aspiration in the diagnosis of granulomatous lesions of the breast. Diagn Cytopathol. 1997;17:108–14. doi: 10.1002/(sici)1097-0339(199708)17:2<108::aid-dc5>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 10.Kumarasinghe MP. Cytology of granulomatous mastitis. Acta Cytol. 1997;41:727–30. doi: 10.1159/000332694. [DOI] [PubMed] [Google Scholar]
- 11.Yip CH, Jayaram G, Swain M. The value of cytology in granulomatous mastitis: a report of 16 cases from Malayasia. Aust N Z J Surg. 2000;70:103–5. doi: 10.1046/j.1440-1622.2000.01764.x. [DOI] [PubMed] [Google Scholar]
- 12.Page DL, Anderson TJ. Diagnostic histopathology of the breast. Edinburgh: Churchill Livingstone; 1987. [Google Scholar]
- 13.Ellis IO, Elston CW, Goulding H. Inflammatory conditions. In: Elston CW, Ellis IO, editors. Systemic Pathology. 3rd ed. Vol. 13. Edinburgh: Churchill Livingstone; 2000. pp. 192–5. The Breast. [Google Scholar]
- 14.Tse GMK, Poon CSP, Law BKB, Pang LM, Chu WCW, Ma TKF. Fine needle aspiration cytology of granulomatous mastitis. J Clin Pathol. 2003;56:519–21. doi: 10.1136/jcp.56.7.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hirata S, Saito T, Kiyanagi K, Kitada M, Yamazaki K, Sasajima T, et al. Granulomatous mastitis diagnosed by core-needle biopsy and successfully treated with corticosteroid therapy: a case report. Breast Cancer. 2003;10:378–81. doi: 10.1007/BF02967662. [DOI] [PubMed] [Google Scholar]
- 16.Miliauskas JR, Pieterse AS, Williams RS. Granulomatous lobular Mastitis. Aust NZ J Surg. 1995;65:139–41. doi: 10.1111/j.1445-2197.1995.tb07281.x. [DOI] [PubMed] [Google Scholar]
- 17.Imoto S, Kitaya T, Kodama T, Hasebe T, Mukai K. Idiopathic Granulomatous Mastitis: Case Report and Review of the Literature. Japanese Journal of Clinical Oncology. 1997;27:274–7. doi: 10.1093/jjco/27.4.274. [DOI] [PubMed] [Google Scholar]


